Published online Aug 18, 2025. doi: 10.5312/wjo.v16.i8.109904
Revised: June 16, 2025
Accepted: July 15, 2025
Published online: August 18, 2025
Processing time: 75 Days and 12.8 Hours
This is a retrospective study on endoscopic treatment of cervical spinal radiculopathy (CSR) conducted at a single academic institution. Conventional full-spine endoscopy is performed in a single portal which has certain limitations of high technical requirements, steep learning curve, and narrow indications. Although unilateral biportal endoscopy (UBE) technique has a gentle learning curve and is gradually applied to treat CSR, all procedures were performed in the uniportal working channel that potentially increase the surgical risk and time in the treatment of complex cases. It is worthy to delve novel technique for more working channels in the treatment of complex CSR.
To propose a hybrid technique (HT) that utilizes spine endoscopy in UBE to treatment of CSR.
A total of 81 patients with single-segment CSR who underwent uniportal endoscopic surgery (UES), UBE, or HT at a single institution between September 2019 and August 2021 were retrospectively studied. Perioperative patient data were compared between the groups. The pre-operative and post-operative images were compared to confirm adequate decompression of the nerve root canal. Patients' visual analogue scale (VAS) scores and neck disability index (NDI) were recorded before surgery, and three days, three months and six months after surgery.
The UBE and HT groups had a significantly shorter operation duration than the UES group. Data for bleeding and length of hospital stay were significantly higher in the UBE group than in the UES and HT groups. The hospitalization cost was lowest in the UES group and highest in the HT group. Soft tissue edema reaction bands on post-operative day 3 were larger in the UBE and HT groups than in the UES group. Post-operative VAS and NDI scores were significantly lower in all three groups than the pre-operative levels. On post-operative day 3, the VAS score for neck pain was significantly higher in the UBE and HT groups than that in the UES group. However, there were no significant differences in the VAS scores for arm pain or NDI between the three groups. The post-operative 3-month and 6-month neck pain VAS, arm pain VAS, NDI, and modified Macnab success rates did not differ statistically between the three groups.
The HT for CSR treatment has the advantage of double working channels to facilitate decompression and hemostasis, improving the surgical efficiency and clinical outcomes of CSR.
Core Tip: This study proposed a hybrid technique (HT) that utilizes spine endoscopy in unilateral biportal endoscopy to obtain another working channel to treat the cervical spondylotic radiculopathy. The HT has the advantage of double working channels to facilitate decompression and hemostasis, improving the surgical efficiency and clinical outcomes.
- Citation: Yan MJ, Zhang BT, Tang GK, Liu YB, Liao WB, Guo S, Fu Q. Novel endoscopic hybrid technique in the treatment of cervical spondylotic radiculopathy. World J Orthop 2025; 16(8): 109904
- URL: https://www.wjgnet.com/2218-5836/full/v16/i8/109904.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i8.109904
The incidence of cervical spondylotic radiculopathy (CSR) has increased annually due to the aging population and new living habits in today’s society. It causes significant disability due to nerve root dysfunction, severely affecting the quality of life of patients and posing a significant financial burden to the patients and society[1]. Moreover, anterior cervical discectomy and fusion has been the gold standard treatment for directly removing herniated nucleus pulposus tissue, decompressing nerve roots, and fusing pathological segments[2]. Despite its curative effect, several complications remain to be addressed, including dysphagia, pseudoarthrosis, and adjacent segment degeneration[3,4]. Minimally invasive spine technique has become increasingly popular for its proposed advantages. Ruetten et al[5] first performed posterior cervical foraminoplasty (PCF) using a 6.9 mm endoscope to treat cervical disc herniation, which resulted in good clinical outcome[5]. PCF under a full endoscope has more advantages compared with the anterior approach, such as avoiding damage to the anterior vital structures and preserving the motion segment[6].
Conventional full-endoscopic PCF is generally performed using uniportal endoscopy. However, uniportal endoscopic surgery (UES) has certain limitations, such as high technical requirements, steep learning curve, and limited indications[7]. Hence, UES is suitable only for cervical disc herniation. Additionally, excessive perfusion pressure on the UES can potentially damage the dural sac. To resolve these disadvantages, the unilateral biportal endoscopy (UBE) technique has emerged, which has a working channel and an observation channel. Considering that the instruments and endoscopes are independent of each other, we can obtain a larger surgical field of view, and the operation is more identical to that of an open surgery than a UES[8]. Therefore, the UBE technique has a gentle learning curve and is gradually applied in the treatment of cervical radiculopathy, especially in patients with spinal stenosis. According to Park et al[9], PCF treated with the UBE technique yielded a satisfactory clinical outcome and could serve as a good alternative to the uniportal endoscopic technique. A study by Kim et al[10] compared the imaging and mid-term efficacy of minimally invasive PCF with uniportal endoscopy, the UBE, and a microscope. Their findings highlighted that all three techniques achieved good clinical effectiveness and sufficient decompression of the intervertebral foramen[10].
In our experience, both the UES and UBE techniques have only one working channel, increasing the surgical risk and time in the treatment of complex cases, particularly when pulling the nerve root or spinal cord to expose the herniated nucleus pulposus for decompression. Additionally, arthroscopic radiofrequency with high energy is employed in the UBE technique, and its working interface is planar, increasing the risk of nerve injury when performing intraspinal hemostasis[11,12]. To attain enough decompression and reduce surgical risk, Zhu et al[13] suggested to add a third channel to compensate for the shortage of a single working channel. However, it increased surgical trauma in these patients. Taking this into account, this study proposes a hybrid technique (HT) that combines UBE and full spinal endoscopy techniques to increase one more working channel and delve deeper into the application potential of the HT in the treatment of cervical radiculopathy.
In the context of treating CSR, this study retrospectively analyzed patients who underwent one of the 3 types of endoscopic PCF between September 2019 and August 2021 at a single center.
The study was approved by the Ethics Committee of Shanghai General Hospital (No. 2019SQ378), and the study was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent.
Two experienced spine surgeons, who had at least 5 years of experience in uniportal endoscopic and biportal endoscopic surgery at the time of this study, performed all the procedures. Moreover, the operative procedures were determined according to the surgeons’ experience and preferences.
All the included patients met the following criteria: (1) Age within the range of 30 to 65 years; (2) There was no improvement in symptoms after > 3 months of conservative treatment; (3) Imaging examination confirmed a single-segment cervical disc herniation, with the lesion segment ranging from C4/5 to C6/7; and (4) Clear symptoms of radiculopathic pain are observed in the upper limbs.
The exclusion criteria were as follows: (1) Concomitant myelopathy of cervical spondylosis; (2) Imaging shows that the cervical spine is unstable; (3) Previous surgical history of lesions, tumors, infections, and other diseases; and (4) Pre-operative clear contraindications to surgery.
According to the above criteria, 81 patients were included and divided into UES, UBE, and HT groups according to the surgical methods used. As shown in Table 1, there were 15 males and 13 females in the UES group, aged 44.21 ± 9.84 years, with 11 cases of C4/5, 12 of C5/6, and 5 of C6/7. Moreover, there were 13 males and 13 females in the UBE group, aged 45.03 ± 10.96 years, with 8 cases of C4/5, 10 of C5/6, and 8 of C6/7. There were 13 males and 14 females in the HT group, aged 47.78 ± 11.19 years old, with 9 cases of C4/5, 12 of C5/6, and 6 of C6/7. No significant differences in age, sex, or surgical segment data were found between the three groups (P > 0.05).
| Item | UES | UBE | HT | ||||
| Gender | Male | Female | Male | Female | Male | Female | |
| 15 | 13 | 13 | 13 | 13 | 14 | ||
| Age | 44.21 ± 9.84 | 45.03 ± 10.96 | 47.78 ± 11.19 | ||||
| Segment | C4/5 | 11 | 8 | 9 | |||
| C5/6 | 12 | 10 | 12 | ||||
| C6/7 | 5 | 8 | 6 | ||||
UES group: Under general anesthesia, patients were positioned in the standard prone position on a carbon bed with protection of the face and bilateral eyes on a face cradle pad, following routine disinfection and draping. C-arm fluoroscopy was used to localize the responsible segment. Then, an 8 mm-long skin incision was made approximately 1.5 cm ipsilateral to the middle line at the level of the target interlaminar space. Next, a Kirschner (K) wire was inserted at the lesion level under fluoroscopic guidance. Serial dilators were inserted through the K-wire and docked at the medial border of the facet joint. Subsequently, an endoscopic system was used. Laminotomy and foraminotomy were performed using a 3.0 or 3.5 mm endoscopic drill and endoscopic punches, respectively, after soft tissue removal by coagulation with the radiofrequency probe. Following resection of the ligamentum flavum using a basket punch and endoscopic Kerrison punch, the nerve root was exposed, and herniated nucleus pulposus tissue was removed with endoscopic pituitary forceps. After adequate nerve root decompression was confirmed with a fine dissector, annuloplasty was performed around the perforated disk hole using a radiofrequency probe. Full intra- and extraspinal hemostasis was confirmed to complete the operation.
UBE group: The patient’s position and landmark localization were the same as above. A transversal 8 mm long skin incision was made approximately 1.5 cm ipsilateral to the spinous process line at the level of the target interlaminar space. Subsequently, a similar incision was made 2–3 cm below the first incision. The cranial and caudal approaches were utilized for viewing and working portals, respectively. The usual biportal endoscopic system (Coblation) with a 4.0 mm diameter, using a zero-degree optic view angle endoscope, was placed through the viewing portal. The medial border of the facet joint was the initially focused area, and soft tissues were removed using a radiofrequency probe. The same laminotomy and foraminotomy procedures were carried out using an endoscopic drill and a 1.0 or 2.0 mm Kerrison punch. After removing the ligamentum flavum with a regular Kerrison punch, the herniated nucleus pulposus was extracted using regular pituitary forceps to decompress the nerve root. Finally, hemostasis was achieved using a radiofrequency probe, and a drainage tube was placed.
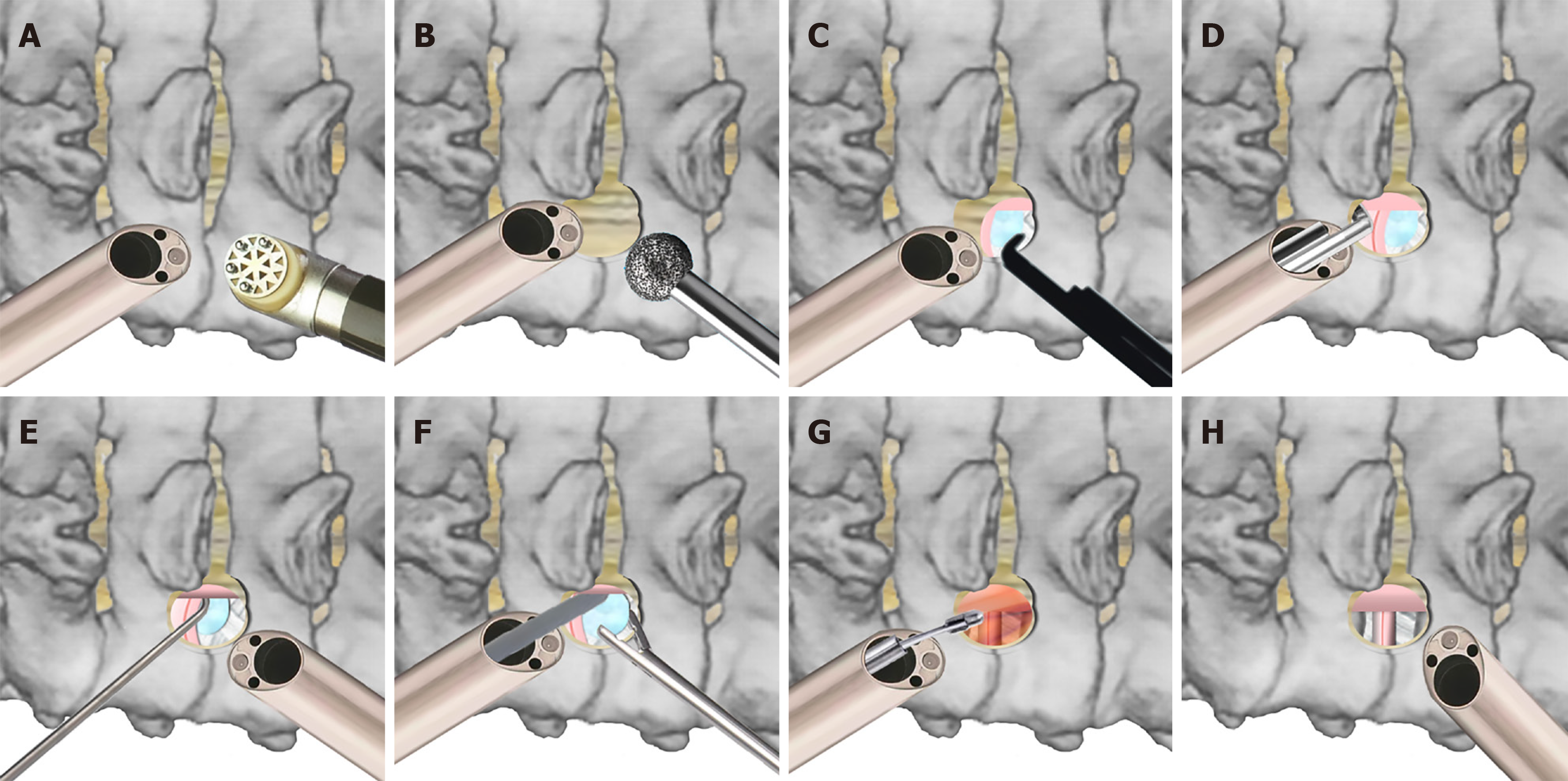
HT group: The preparation procedures were the same as those in the above two groups. An 8-mm long longitudinal incision was made approximately 1 cm ipsilateral to the midline at the lesion level. A second incision was made 2 cm below the first incision. The cranial approach for the viewing portal and the caudal approach for the working portal were placed. Different from the UBE group, full-spine endoscopy was performed instead of UBE arthroscopy. Both endoscopic and regular cervical surgical instruments were used for laminotomy and foraminotomy, respectively. A high-energy radiofrequency probe was used for extraspinal soft tissue exfoliation and hemostasis. Laminotomy procedures were conducted using an endoscopic drill. The ligamentum flavum was removed by an endoscopic and regular punch. Intraspinal hemostasis was achieved using a low-energy radiofrequency probe. The herniated nucleus pulposus was then removed by pituitary forceps in original working portal after slight traction of nerve root by stripper in endoscopic working portal, which was different from the above two groups. Furthermore, the viewing and working portals could be exchanged to enlarge the surgical field as much as possible. Hemostasis was confirmed before closure (Figure 1).
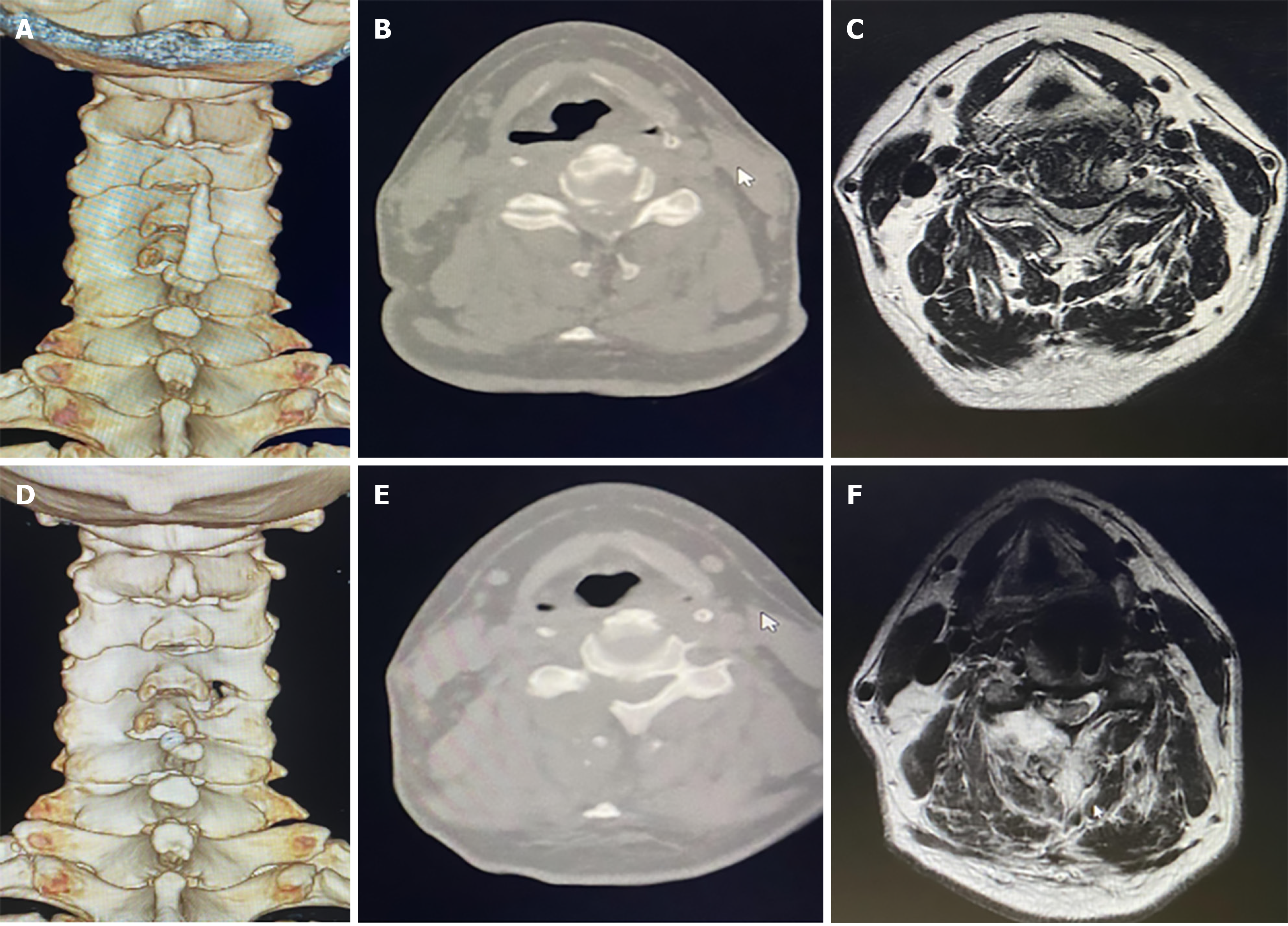
We recorded the patient's basic information, duration of the operation, intraoperative bleeding coefficient (colorimetric method was used to obtain the coefficient after correction by standard samples), percentage of bleeding time (endoscopic bleeding time/total time), length of hospitalization, cost, and visual analogue scale (VAS) score for neck and upper limb pain. Additionally, the neck disability index (NDI) and improved Macnab score of patients before surgery, as well as the data 3 days, 3 months, and 6 months postoperatively, were recorded, and the outcome of the surgery and the patient’s recovery were evaluated. Computed tomography (CT) and magnetic resonance imaging (MRI) images of the patients pre-operatively and 6 months post-operatively were compared to confirm adequate decompression. post-operative soft tissue response bands on MRI were also documented. All postoperative evaluations (including VAS, NDI, and imaging analyses) were performed by an independent orthopedic specialist blinded to the surgical grouping.
The SPSS 20.0 software was used for the statistical analysis. Normally distributed measurement data are represented by the mean ± SD, and the comparison between the measurement data groups utilized a one-way analysis of one-way analysis of variance and a two-to-two comparison between the groups. The comparison between the counting data was made using the χ2 test. Statistical significance was set at P < 0.05.
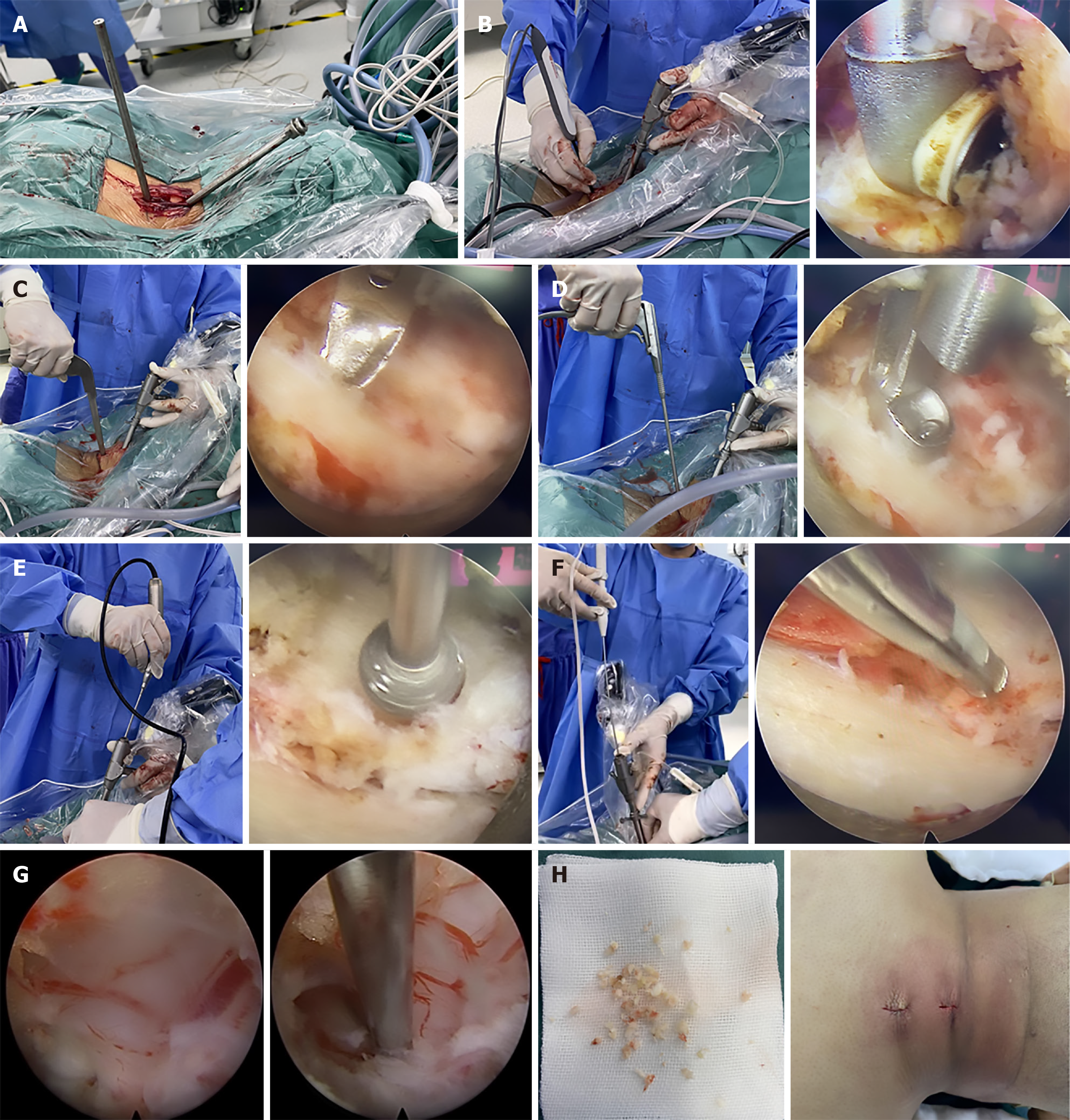
All three groups successfully completed the surgical procedures and follow-ups. See the specific procedure details in Figure 2. All outcome metrics were collected and analyzed under blinded conditions as described in the Methods section, minimizing observer bias. Table 2 shows a comparison of the perioperative period indicators. In the inter-group comparison, the operation time of both the UBE group and the hybrid group was significantly lower than that of the uniportal endoscopy group, and the difference was statistically significant (P < 0.05). In addition, the intraoperative bleeding coefficient and percentage of endoscopic bleeding time were significantly higher in the UBE group than in the uniportal endoscopic and hybrid groups, and the difference was statistically significant (P < 0.05). The length of hospital stay in the UBE group was higher than in the uniportal endoscopy and hybrid groups, and the difference was statistically significant (P < 0.05). Furthermore, hospitalization costs were the lowest in the uniportal endoscopy group and the highest in the hybrid endoscopy group, and statistical differences were observed between the three groups (P < 0.05).
| Item | UES | UBE | HT |
| Duration of operation (minute) | 72.46 ± 8.41a | 59.27 ± 5.16 | 64.15 ± 7.55 |
| Bleeding index | 1.09 ± 0.15 | 1.49 ± 0.28a | 1.3 ± 0.13 |
| Bleeding duration percentage (%) | 24.59 ± 3.16 | 32.49 ± 4.09a | 26.22 ± 2.8 |
| Length of hospital stay (day) | 4.63 ± 0.61 | 5.8 ± 0.56a | 4.65 ± 0.67 |
| Cost (Thousands, Yuan) | 3.45 ± 0.07a | 4.12 ± 0.08a | 5.06 ± 0.11a |
| Modified Macnab criteria (excellent + good) | 0.86 | 0.92 | 0.96 |
| Post-operative soft tissue edema (cm2) | 5.21 ± 0.46a | 7.29 ± 0.78 | 7.02 ± 0.53 |
There were no significant differences in the post-operative clinical outcomes between the three groups. Compared with the pre-operative values, significantly lower post-operative VAS and NDI scores were found in all three groups (P < 0.05). There was no statistical difference in the success rates among the three groups according to the modified Macnab criteria (P > 0.05). Soft tissue reaction bands at three days post-surgery were larger in the UBE and hybrid groups than in the uniportal endoscopic group, and the difference was statistically significant (P < 0.05). Additional details are presented in Table 3 and a typical case of pre- and post-operative images were shown in Figure 3.
| VAS of neck pain | VAS of upper limb pain | NDI | ||
| UES | Pre-operation | 6.29 ± 0.69 | 7.43 ± 0.83 | 42.19 ± 3.08 |
| 3 days after surgery | 2.81 ± 0.72b | 3.1 ± 0.51b | 17.57 ± 3.24b | |
| 3 months after surgery | 2.14 ± 0.62b | 2.57 ± 0.49b | 8.43 ± 1.22b | |
| 6 months after surgery | 2.29 ± 0.54b | 2.43 ± 0.5b | 7.95 ± 1.21b | |
| UBE | Pre-operation | 6.12 ± 0.85 | 7.46 ± 0.99 | 42.89 ± 3.74 |
| 3 days after surgery | 3.89 ± 0.97a,b | 2.89 ± 0.64b | 22.05 ± 2.74b | |
| 3 months after surgery | 2.37 ± 0.67b | 2.37 ± 0.48b | 8.32 ± 1.45b | |
| 6 months after surgery | 2.32 ± 0.46b | 2.26 ± 0.44b | 8.16 ± 1.04b | |
| HT | Pre-operation | 6.26 ± 0.91 | 7.44 ± 0.94 | 43.04 ± 3.22 |
| 3 days after surgery | 3.89 ± 0.69a,b | 2.93 ± 0.6b | 22 ± 3.16b | |
| 3 months after surgery | 2.46 ± 0.72b | 2.63 ± 0.58b | 8.26 ± 1.56b | |
| 6 months after surgery | 2.25 ± 0.81b | 2.44 ± 0.49b | 8.09 ± 1.33b | |
In the UBE technique, arthroscopy is used as the monitoring channel with a conventional surgical instrument channel to expand the range of the surgical approach. Decompression of the spinal canal and release of the nerve root can be completed while preserving the paravertebral muscles. Therefore, being minimally invasive, the UBE technique is also highly practical[14,15] with three main characteristics: (1) Compared with the full endoscopic technique, the advantages of the UBE technique lie in the two channels without interference, specifically endoscopy and work channels, which can be tilted and moved freely to enhance the convenience of the operation. The working vision will not be obstructed by the instruments throughout the operation, which substantially increases the flexibility of the surgery; (2) Unilateral partial laminectomy or hemilaminectomy can be performed using the UBE technique since it is a translaminar approach. Comprehensive decompression of the spinal canal, including ossification of the ligamentum flavum and hyperplasia of the articular process, can be performed to maintain effective release of the nerve root; and (3) Various traditional and endoscopic instruments can be used in the UBE technique to improve decompression efficiency and reduce operation time[16].
However, we found that the uniportal full endoscope or UBE technique has only one working channel. This increases the surgical risk and reduces the effectiveness when dealing with complex cervical radiculopathy cases in which the nucleus pulposus tissue is hidden behind the nerve root.
Additionally, failure of hemostasis in the UBE technique may blur the visual field to increase the operative time and even cause major complications such as dural tears or nerve root injuries. Lee et al[17] retrospectively analyzed the UBE technique in the treatment of lumbar spinal stenosis and presented seven cases of dural injurie. They suggested that dural tears were associated with inadequate intraoperative hemostasis and blurred visual fields.
The use of arthroscopic radiofrequency with a planar working interface increases the risk of nerve injury during intraspinal hemostasis. We propose using a hybrid technique based on the unilateral biportal technique and full spinal endoscopic technique for the treatment of CSR. It aims to increase the working channel of endoscopic surgery and achieve accurate spinal canal hemostasis. Moreover, spinal endoscopy was used in this hybrid technique with two working channels. The monitoring and working channels can be switched with each other, further improving surgical efficiency and achieving better decompression and hemostasis.
The present study found that the symptoms in all three groups significantly improved after surgery. Nevertheless, a more thorough decompression was observed in both the UBE and hybrid groups due to the flexible operation and the absence of instrument interference in both groups. Kim et al[10] showed that a more adequate foraminal decompression could be achieved in the UBE group than in the uniportal endoscopic group. Additionally, the operation time in the UBE and hybrid groups was significantly shorter than in the uniportal endoscopy group. This is linked to the expansion of the surgical field and working channel in the first two groups, providing favorable conditions for effective decompression operation and accurate hemostasis during the entire operation. However, in a comparative study of PCF surgery, Kim et al[10] concluded that longer operation time was required in the UBE group than in the uniportal full endoscopy group. They believed that multiple layers of muscle and thick fascia comprise the cervical paraspinal muscular structures. Two portals in different directions in the UBE technique should be established through the multilayered fascia. Moreover, the working portal is frequently obstructed by flapping pieces of fascia to prolong the operation time.
To obtain a broader field of view, the UBE and hybrid groups require more soft tissue dissection, thereby causing more blood loss and a wider range of soft tissue injury zones. Guo et al[18] substantiated the risk of hidden blood loss during UBE surgery; thus, drainage was routinely required afterward. Additionally, the post-operative bed rest and hospital stay were longer in the UBE and hybrid groups than in the uniportal endoscopic technique group. As shown previously, more soft tissue and bone resections are required during decompression in the UBE and hybrid groups, especially in elderly patients with severe spinal stenosis. The bed rest and hospital stay were correspondingly extended to prevent nerve root edema and mild instability after the procedure.
In terms of blood loss, we also found that it was superior in the hybrid group than in the UBE group. This verifies the higher hemostatic efficiency of the former than of the latter. The use of arthroscopic radiofrequency in the UBE group may damage the spinal nerve due to its large working surface and high energy. Conversely, both arthroscopic and spinal radiofrequency were used in the hybrid technique group. Using spinal Elliquence radiofrequency with a low-energy and point-working surface can minimize the risk of nerve injury and ensure accurate intraspinal hemostasis, thereby reducing the incidence of post-operative intraspinal hematoma[19].
The combined use of high and low energy radiofrequency increased the effectiveness of intraspinal hemostasis during surgery in the hybrid group. Although conventional instruments can be used in the UBE technique, the risk of nerve injury is significantly increased when high-speed drilling is used for decompression due to the interference of soft tissue and the lack of a protective sleeve[20]. Unlike the UBE technique, endoscopic drilling can be used in the hybrid group, which has greater precision and stability because of the effective protection provided by uniportal endoscopy. Finally, the nerve can be mildly pulled and exposed using the nerve root retractor through another working channel when dealing with a deeply hidden protrusion. In addition, the two working channels can be exchanged with each other. However, the hospitalization cost is relatively high because of an increase in spinal elliquence radiofrequency.
There are some limitations in this study. It primarily focuses on single-segment CSR and lacks multi-segment CSR and other types of cervical spondylotic disease. Since this was a retrospective study with a small number of cases that may lead to selection bias, a large sample and multi-center prospective randomized study must be performed. Long-term clinical outcomes, including the impact on spinal stability and symptom recurrence, are required for further evaluation.
The use of a hybrid technique can significantly boost surgical efficiency, maintain and improve satisfactory clinical outcomes, and reduce trauma during the treatment of CSR.
| 1. | Safaee MM, Nichols NM, Yerneni K, Zhang Y, Riew KD, Tan LA. Safety and efficacy of direct nerve root decompression via anterior cervical discectomy and fusion with uncinectomy for cervical radiculopathy. J Spine Surg. 2020;6:205-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Liu WJ, Hu L, Chou PH, Wang JW, Kan WS. Comparison of Anterior Cervical Discectomy and Fusion versus Posterior Cervical Foraminotomy in the Treatment of Cervical Radiculopathy: A Systematic Review. Orthop Surg. 2016;8:425-431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 3. | Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien). 1989;99:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 217] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H, Tsianaka E, Vagkopoulos K, Paterakis K, Fountas KN. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. 2017;3:444-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 5. | Ruetten S, Komp M, Merk H, Godolias G. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg. 2007;50:219-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 128] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:940-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 247] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 7. | Wu PH, Kim HS, Lee YJ, Kim DH, Lee JH, Yang KH, Raorane HD, Jang IT. Posterior endoscopic cervical foramiotomy and discectomy: clinical and radiological computer tomography evaluation on the bony effect of decompression with 2 years follow-up. Eur Spine J. 2021;30:534-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Jung SB, Kim N. Biportal endoscopic spine surgery for cervical disk herniation: A technical notes and preliminary report. Medicine (Baltimore). 2022;101:e29751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Park JH, Jun SG, Jung JT, Lee SJ. Posterior Percutaneous Endoscopic Cervical Foraminotomy and Diskectomy With Unilateral Biportal Endoscopy. Orthopedics. 2017;40:e779-e783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Kim JY, Hong HJ, Lee DC, Kim TH, Hwang JS, Park CK. Comparative Analysis of 3 Types of Minimally Invasive Posterior Cervical Foraminotomy for Foraminal Stenosis, Uniportal-, Biportal Endoscopy, and Microsurgery: Radiologic and Midterm Clinical Outcomes. Neurospine. 2022;19:212-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 11. | Jiang HW, Chen CD, Zhan BS, Wang YL, Tang P, Jiang XS. Unilateral biportal endoscopic discectomy versus percutaneous endoscopic lumbar discectomy in the treatment of lumbar disc herniation: a retrospective study. J Orthop Surg Res. 2022;17:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 87] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 12. | Li L, An J, Guo L, Shan X, Sun Y, Li J, Zhang F, Zhang W. Comparison of percutaneous endoscopic lumbar discectomy (PELD) and unilateral biportal endoscopic (UBE) discectomy in the treatment of far lateral lumbar disc herniation (FLLDH): a retrospective study. J Orthop Surg Res. 2025;20:510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Zhu C, Cheng W, Wang D, Pan H, Zhang W. A Helpful Third Portal for Unilateral Biportal Endoscopic Decompression in Patients with Cervical Spondylotic Myelopathy: A Technical Note. World Neurosurg. 2022;161:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Zheng B, Xu S, Guo C, Jin L, Liu C, Liu H. Efficacy and safety of unilateral biportal endoscopy versus other spine surgery: A systematic review and meta-analysis. Front Surg. 2022;9:911914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 15. | Chu PL, Wang T, Zheng JL, Xu CQ, Yan YJ, Ma QS, Meng-Chen Y, Da-Sheng T. Global and Current Research Trends of Unilateral Biportal Endoscopy/Biportal Endoscopic Spinal Surgery in the Treatment of Lumbar Degenerative Diseases: A Bibliometric and Visualization Study. Orthop Surg. 2022;14:635-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 75] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 16. | Kang MS, Heo DH, Kim HB, Chung HT. Biportal Endoscopic Technique for Transforaminal Lumbar Interbody Fusion: Review of Current Research. Int J Spine Surg. 2021;15:S84-S92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 17. | Lee HG, Kang MS, Kim SY, Cho KC, Na YC, Cho JM, Jin BH. Dural Injury in Unilateral Biportal Endoscopic Spinal Surgery. Global Spine J. 2021;11:845-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Guo S, Tan H, Meng H, Li X, Su N, Yu L, Lin J, An N, Yang Y, Fei Q. Risk factors for hidden blood loss in unilateral biportal endoscopic lumbar spine surgery. Front Surg. 2022;9:966197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 19. | Beyaz SG, İnanmaz ME, Zengin EŞ, Ülgen AM. Combined Use of High Radiofrequency Disk Ablation, Annulus Modulation, and Manual Nucleotomy in a Patient with Extruded Disk Herniation. Pain Pract. 2016;16:E74-E80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | An JW, Lee CW. Surgical Treatment of Extraforaminal Gas-Containing Pseudocyst Compressing L5 Nerve Root by Using Unilateral Biportal Endoscopy. World Neurosurg. 2019;124:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |