Published online Jul 6, 2019. doi: 10.12998/wjcc.v7.i13.1623
Peer-review started: February 27, 2019
First decision: March 27, 2019
Revised: April 17, 2019
Accepted: May 2, 2019
Article in press: May 3, 2019
Published online: July 6, 2019
Processing time: 129 Days and 19.2 Hours
Current research has identified several risk factors for refractory benign esophageal strictures (RBES), but research is scarce on the prediction of RBES in benign esophageal strictures patients. Meanwhile, the long-term outcomes of RBES remain unclear. The aim of this study was to develop and validate a model to determine the progression of RBES in patients with benign esophageal strictures. And we also explored the long-term outcomes and safety in patients with RBES.
To develop and validate a model to determine the progression of RBES in patients with benign esophageal strictures, based on the demographic data and endoscopic findings.
A total of 507 benign esophageal stricture patients treated by dilation alone or in combination with stenting were retrospectively enrolled between January 2009 and February 2018. The primary outcome was to establish a risk-scoring model predicting RBES in benign esophageal strictures. The secondary outcome was to explore the clinical effectiveness and adverse events in patients with RBES.
In the study, age, etiology, and number and length of strictures were the independent risk factors for the refractory performance of benign esophageal strictures. According to risk factors of benign esophageal strictures, a risk-scoring model for predicting RBES in benign esophageal strictures was established: The risk score ranged from 0 to 8 points, and the risk scores were divided into low risk (0-2 points), intermediate risk (3-5 points), and high risk (6-8 points). The proportions of RBES in the corresponding risk categories were 1.0%, 12.2%, and 76.0%, respectively. Among 507 patients, 57 had RBES (39 males; median age, 60 years). The success rate of dilation treatment (51.2%, 21/41) was higher than that of stent placement (37.5%, 6/16).
In this study, 11.3% (57/507) patients had RBES at our hospital. The risk-scoring model predicting RBES in benign esophageal strictures could predict the long-term outcome of patients with strictures ahead.
Core tip: We developed and validated a model to determine the progression of refractory benign esophageal strictures in patients with benign esophageal strictures. The risk-scoring model could predict the long-term outcome of patients with strictures ahead. The endoscopic therapy was the standard treatment for all benign stenosis patients. Our findings may have an impact on daily practice. The presence of a bad score may means surgical indication and refractoriness to endoscopic therapy.
- Citation: Lu Q, Lei TT, Wang YL, Yan HL, Lin B, Zhu LL, Ma HS, Yang JL. Development and validation of a model to determine risk of refractory benign esophageal strictures. World J Clin Cases 2019; 7(13): 1623-1633
- URL: https://www.wjgnet.com/2307-8960/full/v7/i13/1623.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i13.1623
Benign strictures of the esophagus include peptic esophageal strictures, caustic esophageal strictures, post-surgical esophageal strictures, post-endoscopic submucosal dissection (ESD) esophageal strictures, esophageal strictures caused by local radiotherapy and tuberculosis, and others[1,2]. The goals of therapy for benign esophageal strictures are relieving dysphagia and the prevention of stricture recurrence[3]. Dilation with bougie or balloon is the classic treatment. In the majority of patients, this can be accomplished with esophageal dilation, but in cases of refractoriness to dilation, additional therapy may be required during long-term follow-up[4,5]. Kochman et al[6] defined refractory benign esophageal strictures (RBES) as more than 3-5 dilations having been performed without clinical response or when it is impossible to achieve a 14 mm lumen over 3-5 dilation sessions[6,7]. Current research has identified several risk factors for RBES, but research is scarce on the prediction of RBES in benign esophageal strictures patients. Meanwhile, the long-term outcomes of RBES remain unclear. The aim of this study was to develop and validate a model to determine the progression of RBES in patients with benign esophageal strictures, based on the demographic data and endoscopic findings. And we also explored the long-term outcomes and safety in patients with RBES.
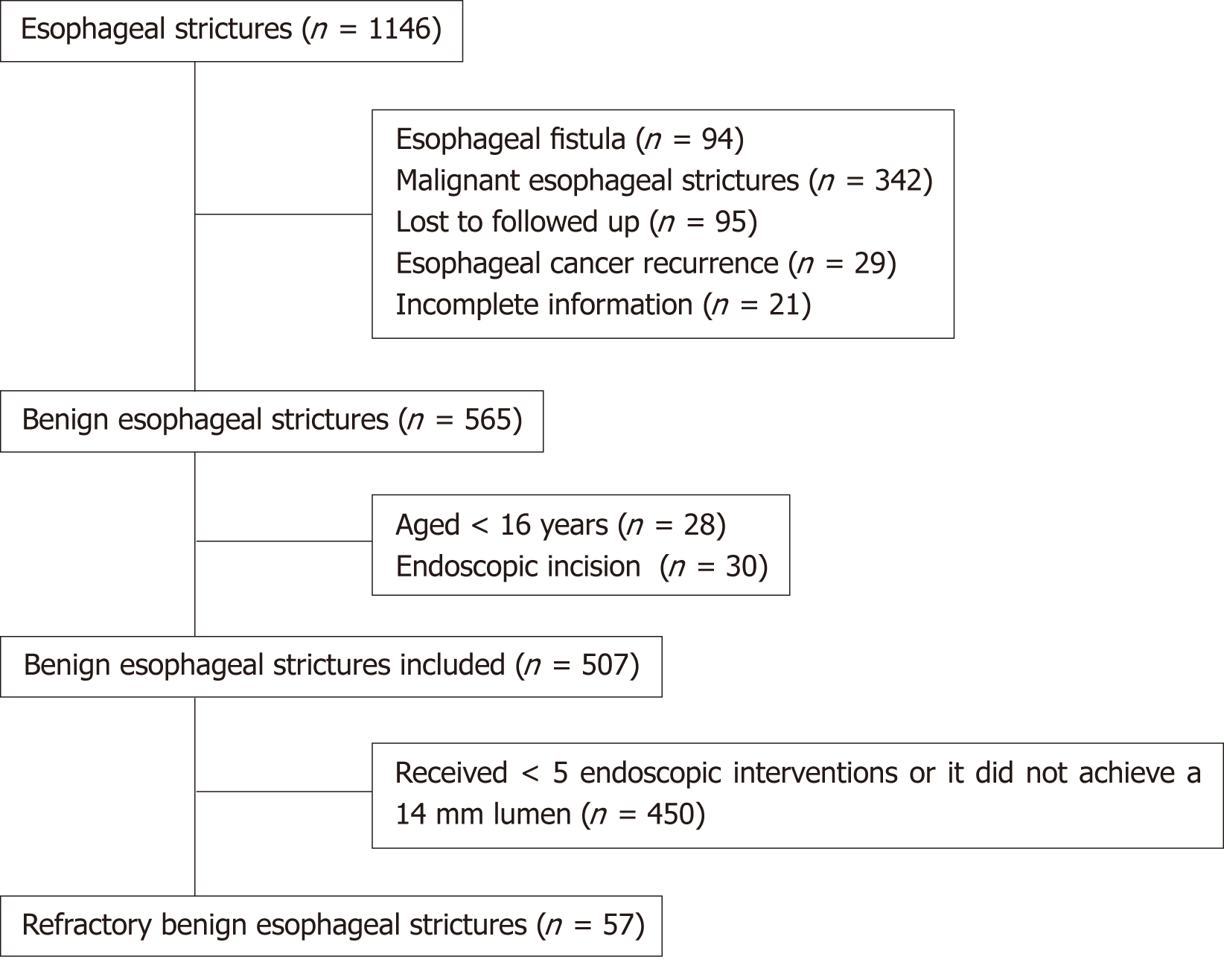
This is a single-center retrospective study. A total of 1146 patients with esophageal strictures were treated by dilation alone or in combination with stenting between January 2009 and February 2018 at our hospital. All medical records were retro-spectively reviewed. Overall, 507 patients were included in the study. The inclusion criteria were: (1) They had been diagnosed with esophageal benign stricture according to the clinical manifestation, gastroscopy, and pathology; (2) They had complete medical records and follow-up information, including gender, age at first therapy, etiology, number, location, length and diameter of structures, endoscopic therapy, and adverse events; and (3) They were more than 16 years old. Patients were excluded if they: (1) Had been diagnosed with congenital esophageal strictures, malignant esophageal strictures, or esophageal fistula; (2) Were diagnosed with recurrence of esophageal cancer; (3) Were lost to follow-up, or had incomplete data; (4) Were less than 16 years old; and (5) Had a history of endoscopic incision after stenosis. The inclusion criteria for RBES were: (1) Satisfying the inclusion criteria for benign esophageal stenosis; and (2) Esophageal endoscopic treatment (including esophageal dilation treatment and esophageal stent placement) performed five times or more, and benign esophageal strictures remained with dysphagia or it did not achieve a 14 mm lumen (Figure 1). This study was approved by the Ethics Committee of West China Hospital of Sichuan University.
Gastroscopes (JIF - Q260 or JIF - Q260J, Olympus Medical Systems, Tokyo, Japan) were used according to the stricture characteristics and type of treatment. Each physician had over 10 years of experience in endoscopy. Written consent for endoscopic dilation and stenting was obtained before the operations. All patients received the standard dilation, with balloon and bougie or fully covered self-expandable metal stents (SEMSs) (MTN-SE C-membrane; 60-140 m; 20 mm; MicroTech, Nanjing, China). The dilation procedures were performed with a through-the-scope balloon (Type 5842; 3 ATM-12 mm, 4.5 ATM-13.5 mm, 8 ATM-15 mm; Boston Scientific Corp; Marlborough, United States) and Savary bougie system (Savary-Gilliard Dilator set, type SGD-70-1; length: 70 cm, diameters: 5, 7, 9, 11, 12.8, 14, and 15 mm; Wilson-Cook Medical, United States). Dilation was the standard treatment for all patients, with other alternatives, such as stents placed on a case-by-case basis at the discretion of the endoscopist performing the procedure, after an appropriate discussion with surgeons and a dietician, as needed. In our study, the stent removal was performed 6-8 wk after insertion to allow the remodeling of the scar tissue.
The primary outcome was to establish a risk-scoring model predicting RBES in patients having benign esophageal strictures. The secondary outcome was to explore the endoscopic therapy effectiveness, ineffectiveness, and adverse events in patients with RBES. Endoscopic therapy success was defined as no need for any other interventions, lasting at least 6 mo[8]. Treatment failure was defined as the need for any endoscopic intervention, including surgery[9], during the follow-up period. Adverse events included esophageal fistula, bleeding, stent dysfunction (stent overgrowth, stent migration, and food impaction), and intolerable chest pain. Early and late adverse events were defined as those occurring within 7 d and later than 7 d after stenting, respectively. All patients were followed via telephone contact, from the first therapy session until study termination or patient death to assess symptom resolution.
Descriptive statistics are reported as the median or mean and range for continuous variables. The χ2 test and the Fisher’s exact test were used for categorical variables, and the t-test was used for continuous variables. To create and validate a risk model for the progression of RBES in benign esophageal strictures patients, we used a split-sample strategy. Using a random number from the uniform (0, 1) distribution, we labeled those with values < 0.3 as a validation cohort and > 0.3 as a development cohort, and this gave us a 70/30 split. This strategy has been used in multiple models[10,11]. In the development cohort (70%), we tested candidate variables and retained the statistical significance in multivariate binary logistic regression analysis. In addition, multivariate binary logistic regression analysis, with the corresponding odds ratios (OR) and 95% confidence intervals (CI) reported, was performed to identify the independent risk factors for RBES. A scoring model was established to calculate the probabilities of RBES in benign esophageal strictures patients on the basis of the retaining candidate variables. The independent risk factors were chosen as scoring items. Meanwhile, each risk factor score was weighted based on the beta coefficient obtained from the logistic regression analysis. In order to keep the scoring model simple, the respective beta coefficient was rounded to the nearest whole number. The total score represented the sum of scores for each risk factor. Using these scores, we derived three groups of risk: Low (points 0-2), intermediate (3-5), and high (6-8). Probabilities of RBES with 95%CI in each group, stratified by the risk factor, were calculated. In the validation cohort (30%), the model discrimination was tested with the receiver operating characteristic (ROC) curve and area under the ROC curve (AUROC). An AUROC of 1.0 indicated perfect concordance, whereas an AUROC of 0.5 indicated no relationship. External validation of the scoring model was performed by measuring the discriminatory ability with AUROC. To test calibration, we used a Hosmer-Lemeshow (H-L) test along with reporting the calibration slope and intercept. To evaluate the relationship between various clinical characteristics in RBES patients, univariate analyses were performed using the χ2 test and t-test. Statistical analyses were performed using SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, United States). P-values less than 0.05 were considered statistically significant.
Patient characteristics are shown in Table 1. In total, 507 patients with benign esophageal strictures were included (178 males; median age, 58 years). Among these patients, esophageal strictures were caused by esophagectomy in 246 (48.5%) patients, ESD in 78 (15.4%), achalasia in 148 (29.2%), caustic injury in 13 (2.6%), mixed etiology in 2 (0.4%), and others in 20 (3.9%). Among the 507 cases, esophageal strictures were located in the cervical esophagus in 40 (7.9%), thoracic esophagus in 315 (62.1%), and ventral esophagus in 152 (30.0%). A single stricture was observed in 477 (94.1%) patients, 24 (4.7%) patients had two strictures, and 6 (1.2%) patients had three or more strictures. The median stricture length was 0.5 cm (range, 0.5-10.0 cm). All 507 patients received endoscopic dilations. A total of 299 (59.0%) patients underwent one dilation session, 85 (16.8%) underwent 2, 42 (8.3%) underwent 3, 24 (4.7%) underwent 4, and 57 (11.2%) had RBES. The median number of dilation session was 5 (range, 3-21) during a mean follow-up period of 31 months (range, 6-106 mo). The SEMSs were placed in 55 (10.8%) patients. A mean of 1.9 (range, 1-6) SEMSs were placed in 20 (26.7%) patients. The mean time of stent placement was 29 d (range, 7-67 d).
| Category | N (%) / M (range) n = 507 | |
| Sex | Female | 178 (35.1) |
| Male | 329 (64.9) | |
| Age (yr) | - | 58 (16-88) |
| Etiology1 | Post-ESD/ESTD | 78 (15.4) |
| Achalasia | 148 (29.2) | |
| Caustic | 13 (2.6) | |
| Postoperative | 246 (48.5) | |
| Peptic | 3 (0.6) | |
| Trauma | 2 (0.4) | |
| Mixed | 2 (0.4) | |
| Post-radiation | 1 (0.2) | |
| Iatrogenic | 14 (2.8) | |
| Location of strictures1 | Cervical | 40 (7.9) |
| Thoracic | 315 (62.1) | |
| Ventral | 152 (30.0) | |
| Number of strictures | One | 477 (94.1) |
| Two | 24 (4.7) | |
| Three or more | 6 (1.2) | |
| Length of strictures (cm) | - | 0.5 (0.5, 10) |
| Times | One | 299 (59.0) |
| Two | 85 (16.8) | |
| Three | 42 (8.3) | |
| Four | 24 (4.7) | |
| Five or more | 57 (11.2) | |
| Endoscopic therapy | Stenting + dilation | 55 (10.8) |
| Dilation only | 452 (89.2) |
The clinical features of the 507 benign esophageal strictures are summarized in Table 2. The incidence of RBES was 11.2% (57/507) in benign esophageal strictures. Significant associations between the incidence of RBES and etiology, location, number and length of strictures, and endoscopic therapy were revealed in the univariate analyses (Table 2). There was a significant association between the incidence of RBES and age, etiology, number and length of strictures, and endoscopic therapy in the multivariate analyses (Table 2).
| Category | Non-RBES n (%) / M (range) n = 450 | RBES n (%) / M (range) n = 57 | P1 | P2 | OR (95%CI) | |
| Sex | Female | 160 (89.9) | 18 (10.1) | 0.553 | 0.665 | 0.916 (0.617-1.361) |
| Male | 290 (88.1) | 39 (11.9) | 0.665 | 1.091 (0.735-1.620) | ||
| Age (yr) | - | 58 (16, 88) | 60 (16, 75) | 0.548 | 0.034 | 0.968 (0.939-0.998) |
| Etiology | Post-ESD/ESTD | 55 (70.5) | 23 (29.5) | < 0.001 | 0.007 | 5.874 (1.623-21.255) |
| Postoperative | 223 (90.7) | 23 (9.3) | 0.009 | 3.333 (1.358-8.182) | ||
| Achalasia | 147 (99.3) | 1 (0.3) | 0.013 | 0.084 (0.012-0.597) | ||
| Caustic | 5 (38.5) | 8 (61.5) | 0.320 | 1.512 (0.67-3.413) | ||
| Other | 20 (90.9) | 2 (9.1) | 0.208 | 0.404 (0.099-1.653) | ||
| Location of strictures | Cervical | 30 (75.0) | 10 (25.0) | < 0.001 | 0.603 | 1.250 (0.539-2.901) |
| Thoracic | 271 (86.0) | 44 (14.0) | 0.671 | 0.869 (0.454-1.663) | ||
| Ventral | 149 (98.0) | 3 (2.0) | 0.884 | 0.921 (0.303-2.794) | ||
| Length of strictures (cm) | 0.5 (0.5, 8) | 2 (0.5, 10) | < 0.001 | 0.001 | 1.344 (1.135-1.591) | |
| Number of strictures | One | 436 (91.4) | 41 (8.6) | < 0.001 | 0.049 | 0.615 (0.370-1.023) |
| Two or more | 14 (46.7) | 16 (53.3) | 0.049 | 1.625 (0.977-2.704) | ||
| Endoscopic therapy | Dilation only | 411 (90.9) | 41 (9.1) | < 0.001 | 0.009 | 0.582 (0.388-0.874) |
| Stenting + dilation | 39 (70.9) | 16 (29.1) | 0.009 | 1.718 (1.145-2.577) |
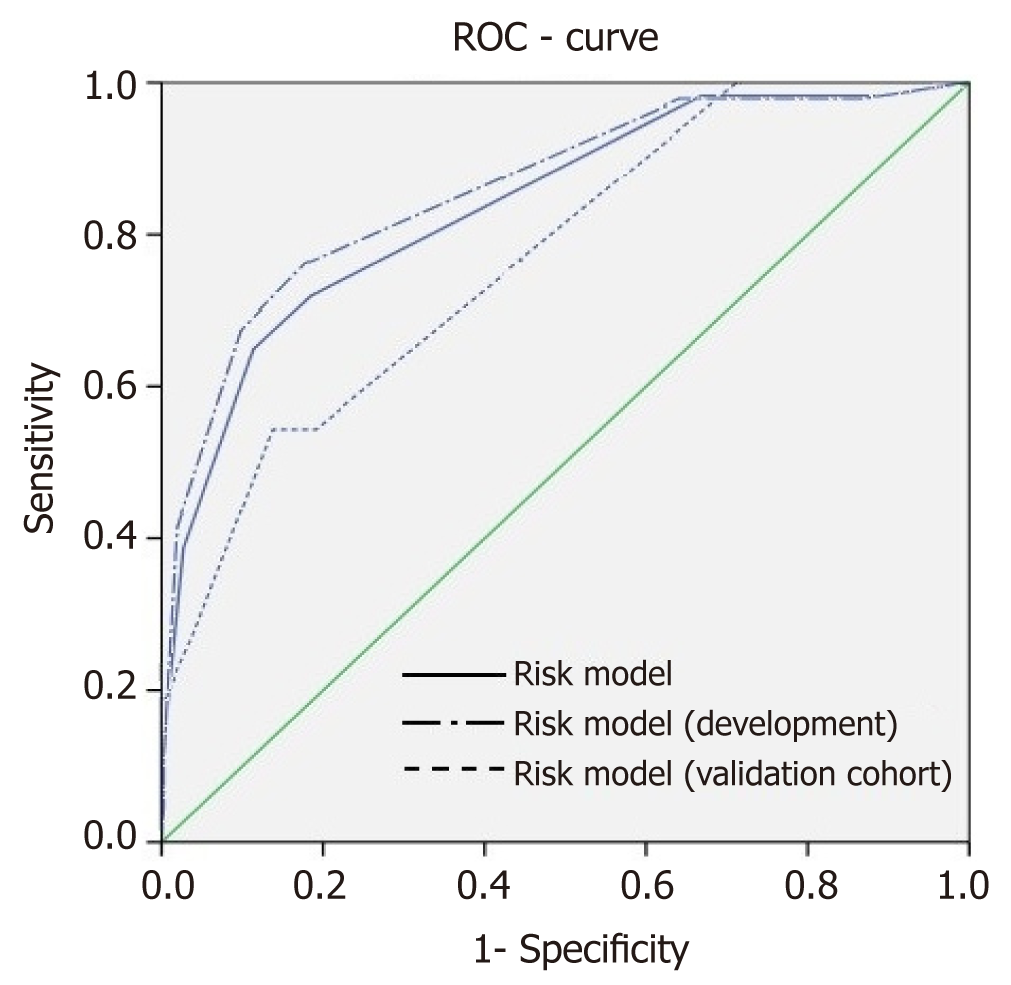
We initially included 7 candidate predictors (Tables 2 and 3) in our analysis. Multivariate binary logistic regression analysis revealed that age, etiology, number, length of strictures, and endoscopic therapy were the independent risk factors for RBES. In reality, stenting was one of the treatment approaches for strictures after multiple dilations with bougie or balloon. We noticed that the stent placement was mostly chosen in patients with RBES, so we excluded endoscopic therapy from candidate predictors. Ultimately, the final model contained only four variables: Age, etiology, and number and length of strictures. Beta coefficients of the four independent risk factors identified in the multivariate analysis are shown in Table 4, and the scores of selected predictors were assigned an integer score based on the Beta coefficient. Based on the scores in each predictor for the development dataset of 345 cases (age, etiology, and number and length of strictures), an 8-point risk-scoring model was built to predict the stratified RBES risk (Table 5). With the scoring model, the percentage of RBES ranged from 0.0 to 100% in the order of calculated risk scores in the development cohort (Table 5). The risk trend of low to high scores presented a significant linear increase (P < 0.001, Cochran-Armitage trend test). A ROC curve of the risk-scoring model for RBES was plotted using the development cohort, and the AUROC of the model for the prediction of RBES was 0.858 (Figure 2). The percentage of RBES for each calculated score and the AUROC were also examined in the validation dataset of 162 cases (Table 5 and Figure 2). The percentage increased from 0.0% to 25% as the score increased, and the AUROC was 0.768. H-L test showed that the P-value was 0.813 in the validation dataset. We divided the cohorts into three risk groups: low, intermediate, and high-risk groups based on point scoring system and the probability of progression to RBES (Table 5). The total risk of progression, at the end of study period, of RBES in each of the three risk categories is provided in Table 5: Low risk: 1.0%, intermediate risk: 12.2%, and high risk: 76.0%.
| Category | Development cohort (n = 345) | Validation cohort (n = 162) | All (n = 507) |
| Sex | |||
| Female | 119 | 59 | 178 |
| Male | 226 | 103 | 329 |
| Age (yr) | |||
| 50 ≤ n < 70 | 197 | 83 | 280 |
| <50 | 103 | 55 | 158 |
| ≥70 | 45 | 24 | 69 |
| Etiology | |||
| Achalasia | 103 | 45 | 148 |
| Post-ESD/ESTD | 58 | 20 | 78 |
| Postoperative | 170 | 76 | 246 |
| Caustic | 6 | 7 | 13 |
| Other | 8 | 14 | 22 |
| Location of strictures | |||
| Cervical | 26 | 14 | 40 |
| Thoracic | 208 | 107 | 315 |
| Ventral | 111 | 41 | 152 |
| Length of strictures (cm) | |||
| <2 cm | 282 | 135 | 417 |
| ≥2 cm | 63 | 27 | 90 |
| Number of strictures | |||
| One | 325 | 152 | 477 |
| Two or more | 20 | 10 | 30 |
| Factor | P | OR | Beta coefficient | Score |
| Age (yr) | ||||
| 50 ≤ n < 70 | 0.066 | 1 (Ref.) | 0 | 0 |
| <50 | 0.021 | 1.2-8.6 | 1.2 | 1 |
| ≥70 | 0.776 | 0.4-3.2 | 0.1 | 0 |
| Etiology | ||||
| Achalasia | 0.037 | 1 (Ref.) | 0 | 0 |
| Post-ESD/ESTD | 0.004 | 25.8 (2.9-230.5) | 3.3 | 3 |
| Caustic | 0.009 | 52.3 (2.7-1027.8) | 4.0 | 4 |
| Postoperative | 0.006 | 19.2 (2.3-161.2) | 3.0 | 3 |
| Other | 0.216 | 6.7 (0.3-136.6) | 1.9 | 2 |
| Number of strictures | ||||
| One | 0.042 | 1 (Ref.) | 0 | 0 |
| Two or more | 0.042 | 3.5 (1.1-11.5) | 1.2 | 1 |
| Length of strictures (cm) | ||||
| < 2 cm | < 0.001 | 1 (Ref.) | 0 | 0 |
| ≥ 2 cm | < 0.001 | 6.4 (2.7-15.2) | 1.9 | 2 |
| Risk score | Rate of RBES (n = 345) | Rate of RBES (n = 162) | Risk | Point | Development cohort Rate of RBES | Validation cohort Rate of RBES |
| 0 | 2.6% (1/38) | 0% (0/11) | Low | 0-2 | 1.0% (1/107) | 0% (0/43) |
| 1 | 0% (0/67) | 0% (0/28) | Intermediate | 3-5 | 12.2% (26/213) | 7.3% (8/110) |
| 2 | 0% (0/2) | 0% (0/4) | High | 6-8 | 76.0% (19/25) | 33.3% (3/9) |
| 3 | 6.7% (10/149) | 6% (5/84) | ||||
| 4 | 14.3% (4/28) | 0% (0/8) | ||||
| 5 | 33.3% (12/36) | 16.7% (3/18) | ||||
| 6 | 73.7% (14/19) | 14.3% (1/7) | ||||
| 7 | 100% (3/3) | 100% (1/1) | ||||
| 8 | 66.7% (2/3) | 100% (1/1) |
Endoscopic therapy success was achieved in 27 (47.4%) patients. The success rate was higher in patients treated by dilation (77.8%, 21/27) than in those treated with stents (22.2%, 6/27). Endoscopic treatment failure was observed in 30 (52.6%) patients. One patient was treated by surgery, and another patient was treated with endoscopic gastrostomy feeding tubes. Fourteen patients had adverse events after endoscopic therapy. Six patients experienced esophageal fistula. One patient experienced intolerable chest pain, and one patient experienced bleeding. Ten patients experienced stent dysfunction, including stent overgrowth in 2, stent migration in 5, and food impaction in 3 (Table 6). There was a significant relationship between endoscopic treatment success and etiology (P = 0.003) and endoscopic therapy (P = 0.043) in univariate analysis (Table 7). Comparing bougie to balloon dilation showed no difference in terms of clinical resolution (P = 0.949).
| Early, n = 3 | Late, n = 11 | |
| Stent overgrowth | 0 | 2 |
| Stent migration | 0 | 5 |
| Food impaction | 0 | 3 |
| Fistula | 1 | 5 |
| Bleeding | 1 | 0 |
| Intolerable chest pain | 1 | 0 |
| Category | N (%) / M (range) | Success (n = 27) | Failure (n = 30) | P |
| Sex | ||||
| Female | 18 (31.5%) | 9 | 9 | 0.787 |
| Male | 39 (68.5%) | 18 | 21 | |
| Age (yr) | 60 (16-75) | 58 (16-75) | 60.5 (16-74) | 0.472 |
| Etiology | ||||
| Post-ESD/ESTD | 23 (40.4%) | 11 | 12 | 0.003 |
| Postoperative | 23 (40.4%) | 7 | 16 | |
| Caustic | 8 (14%) | 8 | 0 | |
| Other* | 3 (5.2%) | 1 | 2 | |
| Location of strictures | ||||
| Cervical | 10 (17.5%) | 5 | 5 | 0.135 |
| Thoracic | 44 (77.2%) | 22 | 22 | |
| Ventral | 3 (5.3%) | 0 | 3 | |
| Number of strictures | ||||
| 1 | 41 (71.9%) | 16 | 25 | 0.351 |
| 2 | 11 (19.3%) | 7 | 4 | |
| 3 and more | 5 (8.8%) | 4 | 1 | |
| Length of strictures (cm) | 2 (0.5-10) | 3 (0.5-10) | 2 (0.5-10) | 0.105 |
| Diameter of strictures (mm) | 4 (1-8.5) | 4 (1-8.5) | 4 (0.5-8.5) | 0.240 |
| Times | 7 (5-28) | 6 (5-19) | 7.5 (5-28) | 0.129 |
| Endoscopic therapy | ||||
| Stenting + dilation | 16 (28%) | 6 | 10 | 0.043 |
| Dilation only | 41 (72%) | 21 | 20 |
A total of 507 patients with benign esophageal strictures met the inclusion criteria. Surgery was the main cause of stenosis, accounting for 48.5% (246/507). Multivariate analysis suggested that post-ESD/endoscopic submucosal tunnel dissection strictures, post-surgery strictures, multiple esophageal strictures, and long segment strictures may lead to RBES. Our results are consistent with the previous research results. Lew et al considered that the short, straight, and not angulated strictures could positively respond to endoscopic dilation as simple strictures. And those complex strictures that are angulated, long (>2 cm), and irregular were often refractory to dilation. Another study showed that longer strictures had a high risk of being refractory to treatment[12]. Patients undergoing esophageal surgery, especially esophagectomies, may develop stenosis, due to developing local ischemia. Patients usually require three to five sessions for the resolution of dysphagia. Esophageal strictures are one of the common complications of post-ESD strictures. The majority of the patients needed to experience several dilations to achieve the relief of symptoms, especially those refractory to dilation, and could accept dilation every around 15 d in our study.
Patients with benign esophageal strictures were stratified according to the risk factors. In our study, we considered that caustic strictures were the high-risk predictive factor, and the finding is consistent with the previous research results. Caustic strictures frequently are a difficult type of strictures associated with a greater need for subsequent dilatations, due to the corrosion resulting in widespread esophageal mucosa damage, and a long-lasting local inflammatory process[13]. Because the mucosal injury often involves an extended segment of the esophagus, the destructed structure frequently is complex, with angulations, narrow lumens, greater length, and severe fibrosis than simple strictures[14]. Caustic strictures often require multiple dilations and are treated for prolonged periods of time. The caustic strictures can be extremely refractory despite repeated dilations, and an esophagectomy may be required to alleviate dysphagia. But the alternatives of surgical reconstruction or feeding tube frequently are unsatisfactory. In our analysis, most refractory caustic strictures had a clinical resolution.
We built the RBES risk assessment model, and the total risk score ranged from 0 to 8 points, based on which the risk was divided into low (0-2), medium (3-5 points), and high (6-8). The refractory benign esophageal stenosis rates in the low, medium, and categories were 1.0%, 12.2%, and 76.0%, respectively, and the low-risk to high-risk population trend increased linearly and significantly. According to the risk assessment model, we could judge the long-term results of stenosis patients in advance. The study examined a large number of subjects and revealed detailed data on RBES risk stratified by risk factors. RBES risk differed considerably according to the status of the risk factors. These results could be useful in determining the management of patients with benign esophageal strictures. For the high risk RBES, it is desirable to perform gastrectomy and choose other interventions, such as surgery.
Our study patients were long-term followed and evaluated after at least 5 therapy sessions, to assess the long-term outcomes, safety, and therapeutic success of endoscopic therapy in patients with RBES. We defined the endoscopic therapy success as no need for any other interventions, lasting at least 6 months. The endoscopic therapy success had an inconsistent standard. So, in our study, the dysphagia-free period was a proxy for survival quality. Once over 6 months, it indicated good quality of life.
In most studies, apparently, the most promising alternative endoscopic stenting can affect the long-term endoscopic therapy outcome. In fact, in our study, the rate of successful outcome appeared to be worse in the subgroup with stents as compared with those without. So, we observed that the stent therapy did not reduce the frequency of dilation. Immediate and postponed complications after dilation occur in 0.5% to 1.2%[15], and excess bleeding may occur in less than 0.5% of the cases[15].
This study has some limitations. First, our study had a potential selection bias, which inherently decreased the statistical power of the study. Second, our study was a retrospective single-center design. A large proportion of our patients were referred, so the incidence of RBES may be overestimated. To best identify the factors that predict RBES and endoscopic therapy efficacy, adverse events, and dysphagia-free period, a large, prospective, and randomized controlled study is needed. Third, although external validation of the scoring model was performed in this study by examining more benign esophageal stricture cases at the same institution with the development set, more external validation in other institutions is still necessary for the future studies.
Overall, 11.3% (57/507) of patients were with RBES in our hospital. The 8-point risk-scoring model predicted RBES in benign esophageal strictures based on age, etiology, and number and length of strictures. The risk scores were divided into low (0-2 points), intermediate (3-5 points), and high risk (6-8 points). And the proportions of RBES in the corresponding risk categories were 1.0%, 12.2%, and 76.0%, respectively. Meanwhile, it could predict the long-term outcome of patients with strictures ahead and might enable more individualized care for patients with benign esophageal strictures.
Current research has identified several risk factors for refractory benign esophageal strictures (RBES), but research is scarce on the prediction of RBES in benign esophageal strictures patients. Meanwhile, the long-term outcomes of RBES remain unclear. The aim of this study was to develop and validate a model to determine the progression of RBES in patients with benign esophageal strictures. And we also explored the long-term outcomes and safety in patients with RBES.
To our knowledge, the present study is the largest sample research of benign esophageal strictures, and our observation indicators are complete, the follow-up period is long, the results are credible, and there is strong reference significance in clinical work.
The aim of this study was to develop and validate a model to determine the progression of RBES in patients with benign esophageal strictures.
A total of 507 benign esophageal stricture patients treated by dilation alone or in combination with stenting were retrospectively enrolled.
Among 507 patients, 57 were with RBES (39 males; median age, 60 years). The age, etiology, and number and length of strictures were the independent risk factors for the refractory performance of benign esophageal strictures. According to risk factors of benign esophageal strictures, a risk-scoring model for predicting RBES in benign esophageal strictures was established; the risk score ranged from 0 to 8 points, and the risk scores were divided into low (0-2 points), intermediate (3-5 points), and high risk (6-8 points). The proportions of RBES in the corresponding risk categories were 1.0%, 12.2%, and 76.0%, respectively.
The risk-scoring model predicting RBES in benign esophageal strictures could predict the long-term outcome of patients with strictures ahead.
The present study is a retrospective study to develop and validate a model to determine the progression of RBES in patients with benign esophageal strictures. Future case-control studies and prospective studies are required to confirm our findings.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jarcuska P, Konishi H, Lima M S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Spechler SJ. American gastroenterological association medical position statement on treatment of patients with dysphagia caused by benign disorders of the distal esophagus. Gastroenterology. 1999;117:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 59] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Kobayashi S, Kanai N, Ohki T, Takagi R, Yamaguchi N, Isomoto H, Kasai Y, Hosoi T, Nakao K, Eguchi S, Yamamoto M, Yamato M, Okano T. Prevention of esophageal strictures after endoscopic submucosal dissection. World J Gastroenterol. 2014;20:15098-15109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Standards of Practice Committee; Egan JV, Baron TH, Adler DG, Davila R, Faigel DO, Gan SL, Hirota WK, Leighton JA, Lichtenstein D, Qureshi WA, Rajan E, Shen B, Zuckerman MJ, VanGuilder T, Fanelli RD. Esophageal dilation. Gastrointest Endosc. 2006;63:755-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Patterson DJ, Graham DY, Smith JL, Schwartz JT, Alpert E, Lanza FL, Cain GD. Natural history of benign esophageal stricture treated by dilatation. Gastroenterology. 1983;85:346-350. [PubMed] |
| 5. | de Wijkerslooth LR, Vleggaar FP, Siersema PD. Endoscopic management of difficult or recurrent esophageal strictures. Am J Gastroenterol. 2011;106:2080-91; quiz 2092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Kochman ML, McClave SA, Boyce HW. The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc. 2005;62:474-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 191] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Spaander MC, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell À, Garcia-Pagán JC, Dumonceau JM, Conio M, de Ceglie A, Skowronek J, Nordsmark M, Seufferlein T, Van Gossum A, Hassan C, Repici A, Bruno MJ. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:939-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 208] [Article Influence: 23.1] [Reference Citation Analysis (1)] |
| 8. | Fuccio L, Hassan C, Frazzoni L, Miglio R, Repici A. Clinical outcomes following stent placement in refractory benign esophageal stricture: a systematic review and meta-analysis. Endoscopy. 2016;48:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Young MM, Deschamps C, Trastek VF, Allen MS, Miller DL, Schleck CD, Pairolero PC. Esophageal reconstruction for benign disease: early morbidity, mortality, and functional results. Ann Thorac Surg. 2000;70:1651-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Rao SV, McCoy LA, Spertus JA, Krone RJ, Singh M, Fitzgerald S, Peterson ED. An updated bleeding model to predict the risk of post-procedure bleeding among patients undergoing percutaneous coronary intervention: a report using an expanded bleeding definition from the National Cardiovascular Data Registry CathPCI Registry. JACC Cardiovasc Interv. 2013;6:897-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 216] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 11. | McNamara RL, Kennedy KF, Cohen DJ, Diercks DB, Moscucci M, Ramee S, Wang TY, Connolly T, Spertus JA. Predicting In-Hospital Mortality in Patients With Acute Myocardial Infarction. J Am Coll Cardiol. 2016;68:626-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 183] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 12. | Andreevski V, Deriban G, Isahi U, Mishevski J, Dimitrova M, Caloska V, Joksimovic N, Popova R, Serafimovski V. Four Year Results of Conservative Treatment of Benign Strictures of the Esophagus with Savary Gilliard Technique of Bougienage: Cross-Sectional Study Representing First Experiences in Republic of Macedonia. Pril (Makedon Akad Nauk Umet Odd Med Nauki). 2018;39:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Gumaste VV, Dave PB. Ingestion of corrosive substances by adults. Am J Gastroenterol. 1992;87:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 14. | Lew RJ, Kochman ML. A review of endoscopic methods of esophageal dilation. J Clin Gastroenterol. 2002;35:117-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 172] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Nostrant TT, Nandi PS. Esophageal dilation. Gastroenterologist. 1998;6:5-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |