Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.8985
Peer-review started: June 30, 2021
First decision: July 26, 2021
Revised: August 10, 2021
Accepted: August 25, 2021
Article in press: August 25, 2021
Published online: October 26, 2021
Processing time: 112 Days and 23 Hours
Myopia, as one of the common ocular diseases, often occurs in adolescence. In addition to the harm from itself, it may also lead to serious complications. Thus, prevention and control of myopia are attracting more and more attention. Previous research revealed that single-focal glasses and orthokeratology lenses (OK lenses) played an important part in slowing down myopia and preventing high myopia.
To compare the clinical effects of OK lenses and frame glasses against the increase of diopter in adolescent myopia and further explore the mechanism of the OK lens.
Changes in diopter and axial length were collected among 70 adolescent myopia patients (124 eyes) wearing OK lenses for 1 year (group A) and 59 adolescent myopia patients (113 eyes) wearing frame glasses (group B). Refractive states of their retina were inspected through multispectral refraction topography. The obtained hyperopic defocus was analyzed for the mechanism of OK lenses on slowing down the increase of myopic diopter by delaying the increase of ocular axis length and reducing the near hyperopia defocus.
Teenagers in groups A and B were divided into low myopia (0D - -3.00 D) and moderate myopia (-3.25D - -6.00 D), without statistical differences among gender and age. After 1-year treatment, the increase of diopter and axis length and changes of retinal hyperopic defocus amount of group A were significantly less than those of group B. According to the multiple linear analysis, the retinal defocus in the upper, lower, nasal, and temporal directions had almost the same effect on the total defocus. The amount of peripheral retinal defocus (15°-53°) in group A was significantly lower than that in group B.
Multispectral refraction topography is progressive and instructive in clinical prevention and control of myopia.
Core Tip: Nowadays, against the increasingly serious myopia of juveniles, myopia prevention and control methods have attracted more attention. Among them, orthokeratology is highly valued because of its high efficiency and low side effects. In this study, the effect of orthokeratology on reducing diopter growth and eye axis length was proved again. Multispectral refraction topography was used to quantify the defocus state of the retina in the 53° field of view and present the defocus form using a visual topographic map. Thus more accurate and reliable evidence was provided on the association between the peripheral retina and myopia development.
- Citation: Ni NJ, Ma FY, Wu XM, Liu X, Zhang HY, Yu YF, Guo MC, Zhu SY. Novel application of multispectral refraction topography in the observation of myopic control effect by orthokeratology lens in adolescents. World J Clin Cases 2021; 9(30): 8985-8998
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/8985.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.8985
Myopia has become a worldwide health problem. The myopia incidence in China is one of the highest globally and increases year by year[1]. Moreover, complications of high myopia, such as cataracts, glaucoma, retinal detachment, macular hemorrhage, and macular hole, occur frequently[2]. High myopia has become the leading cause of blindness and low vision in China. The World Health Organization has listed the prevention and control of myopia in the Global Blindness Prevention Plan[3].
Orthokeratology lenses (OK lenses), rigid contact lenses with a reverse geometric design, can reduce the refractive power and correct myopia by flattening the center of the cornea and steepening the periphery with the absorption of tear fluid during nights when eyelids are closed[4]. At present, the efficacy and safety of OK lenses in controlling adolescent myopia are generally recognized. Studies support it as a control of myopia, as it can reduce the hyperopic defocus in the periphery of the retina by changing diopter and even reverse the defocus of myopia, delaying the growth of the optic axis length[5-7].
The quantification of hyperopia defocus is the key to correcting myopia and preventing diopter increase in adolescents. The multi-spectral topographic map refers to a topographic map corresponding with values of the actual refractive power of each pixel, calculated and summarized through the in-depth development of computer algorithms. Different wavelengths of single-spectral light collect fundus images in multispectral refraction topography (MRT) sequentially. The lens-compensated multispectral images are analyzed for diopter values. Now Chinese self-developed multispectral fundus imaging system, combined with its honeycomb focusing system, can detect retinal refractive topography and quantify the retinal hyperopic defocus.
This is the first study to apply MRT to research the inhibition of myopia by OK. By comparing the refractive power increases of patients, the myopia increase of patients treated with different methods can be quantified. Based on the speculation about the relationship between total retinal defocus values (TRDV) growth and peripheral retinal hyperopic defocus in recent years, corneal topographic measurements are used to quantify the patient’s axial length growth and TRDV in order to verify the impact of TRDV.
Measurements were performed on adolescent patients treated and regularly reviewed in our hospital’s ophthalmology clinic from June 2019 to July 2020. Patients were divided into group A [70 adolescent myopia patients (124 eyes) wearing OK lenses for 1 year] and group B [59 myopia patients (113 eyes) wearing single-focal frame glasses]. The spherical lens diopter in groups A and B was within 0D - -6.00 D, and their corrected visual acuity of both eyes reached 1.0. Group A was composed of 45 males and 79 females, while group B included 51 males and 62 females (Table 1). The age ranges of both groups were 8-16 years (Table 2). Few statistically significant differences existed in genders and age composition ratio of both groups (gender composition ratio of patients with low myopia: P = 0.860; gender composition ratio of patients with moderate myopia: P = 0.030; age composition ratio between group A and B: P = 0.166; age composition ratio of patients with low myopia: P = 0.105; age composition ratio of patients with moderate myopia: P = 0.096).
| Patients with | Group | Gender | Total | χ2 | P value1 | |
| Male | Female | |||||
| Low myopia | Group A | 16 | 25 | 41 | 0.031 | 0.860 |
| Group B | 22 | 37 | 59 | |||
| Moderate myopia | Group A | 29 | 54 | 83 | 4.718 | 0.030 |
| Group B | 29 | 25 | 54 | |||
Exclusion criteria: Patients whose corneal curvature was less than 40 D or more than 47 D, the corneal thickness was less than 480 um or greater than 600 um, original corneal curvature value was not restored after stopping treating for 1 mo, and whose parents had high heredity myopia, or who had irregular astigmatism, ophthalmological organic diseases, or became myopic due to trauma.
OK lenses were provided by the same brand. All patients wore OK lens for 8-10 h overnight. Then their corneas were stained with fluorescein under the cobalt blue light of a slit lamp. No severe complications were shown in the cornea. The optical zone covered the pupil area; the motion range of the lens was 1-2 mm. The four arc zones were kept clear. Patients whose naked eye vision was 0.8-1.0 during the daytime were conducted follow-up inspections regularly. Patients of group B wore single focus frame glasses during the daytime.
In both eyes, 0.5% compound tropicamide was spotted every 5 min and five times in total for mydriasis. After complete anesthesia of ciliary muscle, the lowest diopter was measured through retinoscopy optometry combined with computer optometry and test strips to calculate the best-corrected visual acuity of the patients. Before their diopter changes (spherical lenses) were determined, patients of both groups received myopia correction for 1 year. Group A patients received mydriatic optometry 1 mo after stopping wearing OK lenses, and the apparent refraction was taken as a diopter.
The length of the eye axis was indicated with the average of three measurements with IOL-Master 500.
MRT was used to measure the retinal refractive values and the retinal hyperopic defocus of two groups after correction for 1 year. Pictures of the fundus were taken in a dark room with a normal pupil and a 53° field of view, from which overexposed or poor-quality ones were removed. Total defocus values, defocus values of 15°/30°/45° (RDV15°/30°/45°) around the macula, and defocus values of the upper, nasal, lower, and temporal quadrants were measured and recorded separately.
All statistical analyses were performed using SPSS 23.0. Normal distribution of data was substantiated through Shapiro-Wilk Test (Univariate Analysis and Normality Test Using SAS, Stata, and SPSS, HM Park, 2015) on raw data. Statistically significant differences were determined by the Student’s test (t-test). Statistically significant differences of datasets, which did not meet the assumptions of normality, were determined by the Mann-Whitney U test. The count data was represented by n (%). Statistically significant differences were determined by the χ2 test. The correlation between the independent and dependent variables of the groups was analyzed using multiple linear regression analysis.
As mentioned above, the effects of OK lens and frame glasses treatment on myopia were evaluated among patients with low or moderate myopia. The gender composition of groups A and B with moderate myopia showed a small difference (P = 0.030), which is expected to be revised in future data collection.
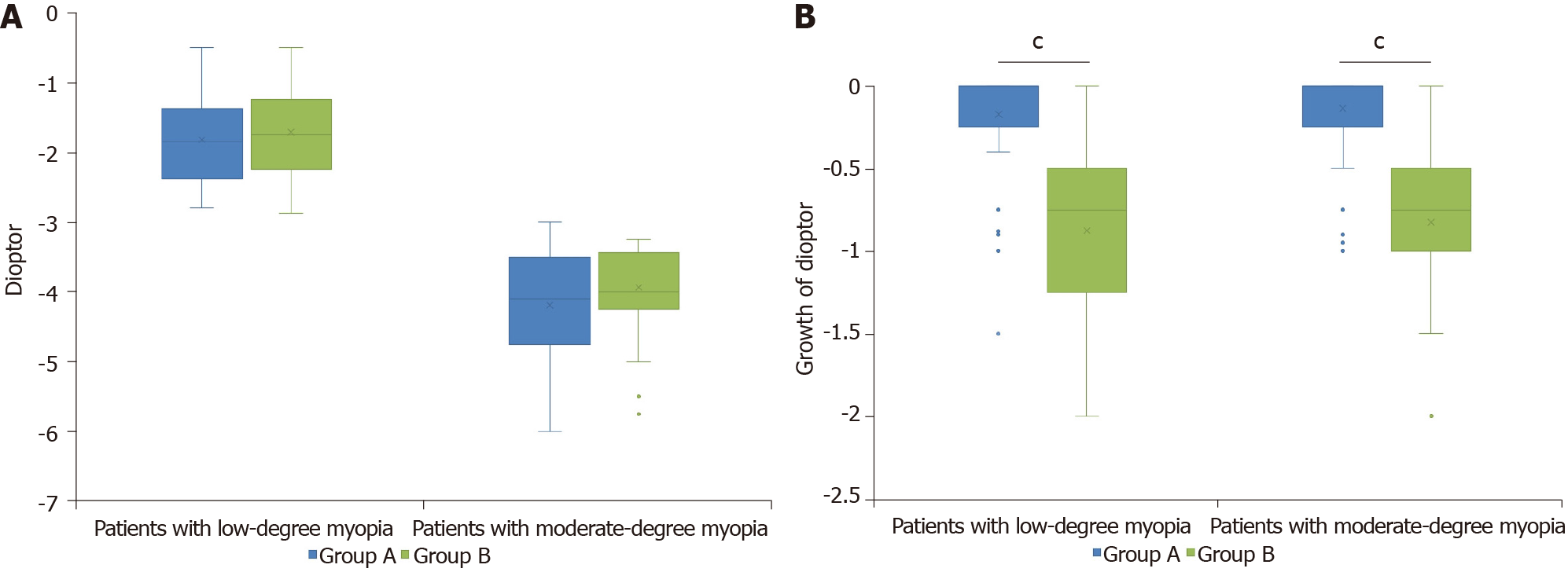
Diopter increase was compared between groups A and B through non-parametric Mann-Whitney U test with non-normal distributed data; no significant difference existed between original diopter values of two groups (low myopia group: Z = -0.949, P = 0.343; moderate myopia group: Z = -1.758, P = 0.079). Among patients with low or moderate myopia, the growth rate of diopter showed significant differences between the two groups. The degree of myopia in patients wearing OK increased significantly, slower than that of patients wearing traditional frame glasses (low myopia group: Z = -7.103, P < 0.001; moderate myopia group: Z = -8.925, P < 0.001), indicating the effect of OK lenses on delaying myopia growth (Figure 1). In addition, no correlation between original diopter values and increase of diopter was observed in both groups; the growth rate of myopia in patients with low and moderate degrees showed no significant differences (group A: Correlation coefficient = 0.032, P = 0.728, Z = -0.395, P = 0.693; group B: Correlation coefficient = -0.071, P = 0.455, Z = -0.522, P = 0.601).
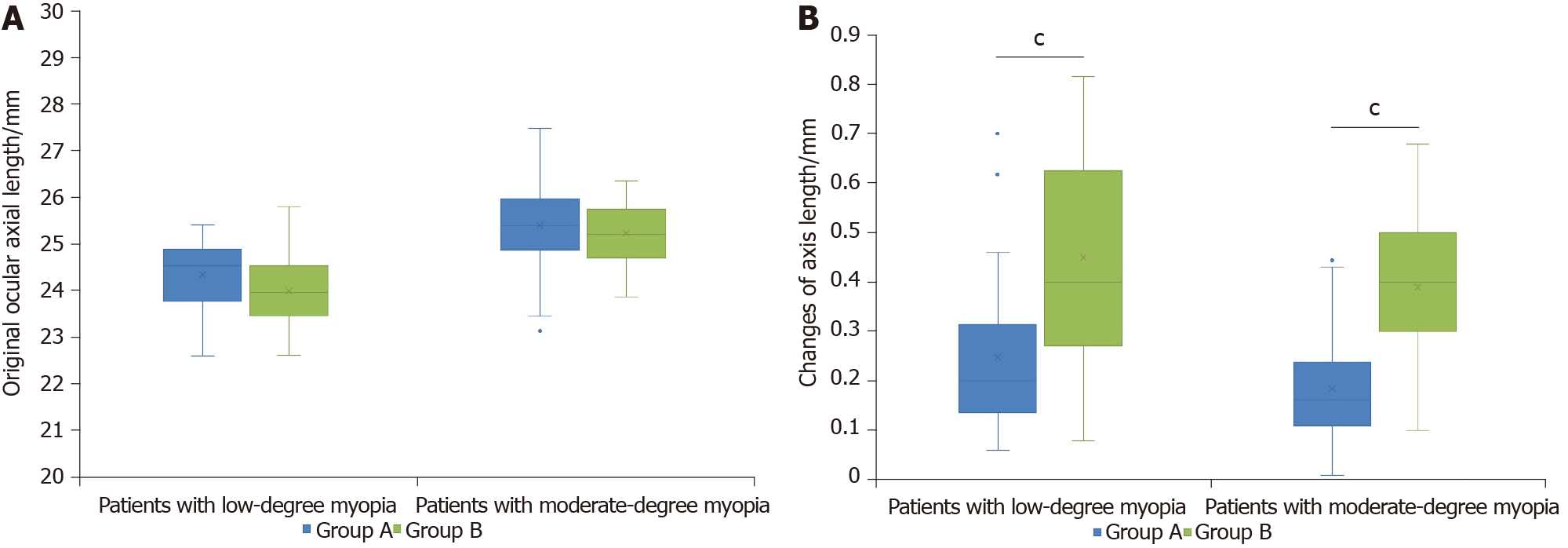
The axis length of groups A and B was measured separately before treatment (2019) and after wearing glasses for 1 year (2020) to identify the differences in axis changes caused by the two treatments. Low and moderate myopia patients were separately analyzed because of the length difference in the original eye axis. Despite no significant difference between the original length of eye axis of groups A and B (low myopia group: F = 0.004, P = 0.061, Figure 2A; moderate myopia group: F = 2.553, P = 0.253, Figure 2B), patients wearing OK showed significantly fewer changes of axis length than those wearing frame glasses (low myopia group: Z = -4.504, P < 0.001, Figure 2; moderate myopia group: Z = -6.625, P < 0.001, Figure 2). Correlation between the original axis length and axis growth was only proved in group A (group A: Correlation coefficient = -0.214, P = 0.040; group B: Correlation coefficient = -0.128, P = 0.200). Similarly, the effect of original defocus values on axis growth was also observed in group A (group A: Z = -2.178, P = 0.029; group B: Z = -1.198, P = 0.231). Surprisingly, the therapeutic effect of OK lenses was more significant in the moderate myopia group; eye axis length changed significantly slower in the group of moderate myopia [low myopia patients in group A: mean ± standard deviation (SD) = 0.25 ± 0.15 (mm); low myopia patients in group B: mean ± SD = 0.45 ± 0.19 (mm); moderate myopia patients in group A: mean ± SD = 0.18 ± 0.11 (mm); moderate myopia patients in group B: mean ± SD = 0.39 ± 0.14 (mm)].
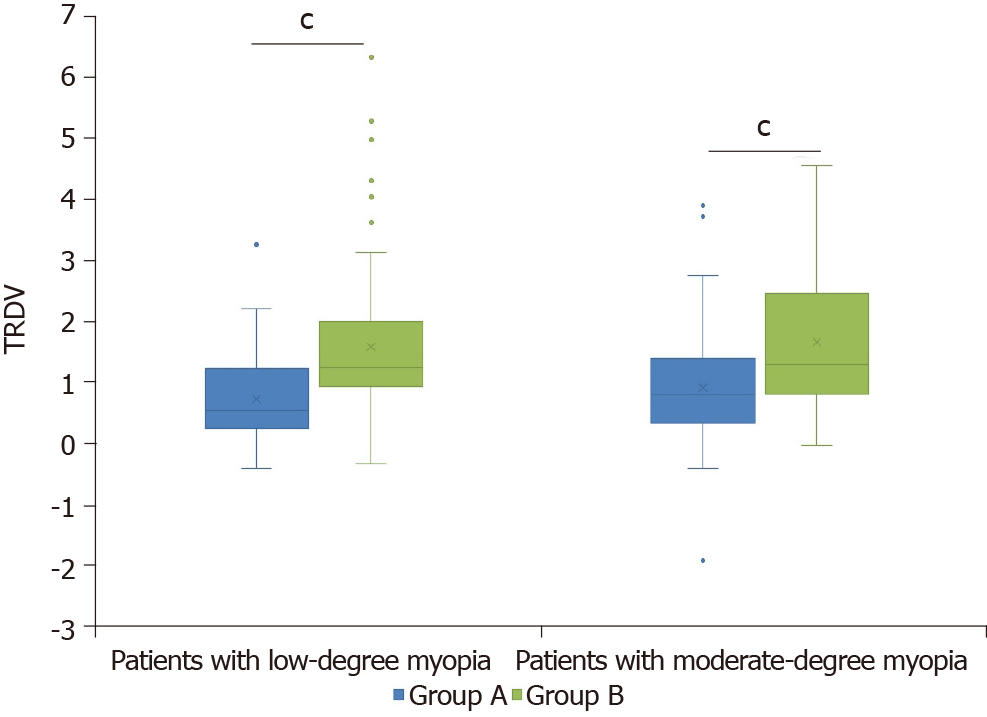
In addition to the increase of diopter and eye axis, OK was also detected to impact the TRDV of these adolescent patients. TRDV was unaffected by original defocus value (group A: Correlation coefficient = -0.008, P = 0.934, Z = -1.439, P = 0.150; group B: Correlation coefficient = -0.010, P = 0.916, Z =-0.463, P = 0.644). Besides, TRDV had a tiny influence on increase of defocus values (group A: Correlation coefficient = 0.064, P = 0.483; group B: Correlation coefficient = -0.166, P = 0.080). In low and moderate myopia groups, TRDV of patients wearing OK lenses was significantly lower than that of patients wearing frame glasses (low myopia group: Z = -3.879, P < 0.001, Figure 3; moderate myopia group: Z = -3.821, P < 0.001, Figure 3). The significantly lower hyperopia defocus value in group A revealed the effect of OK lenses on delaying the eye axis growth and improving eye fundus environment, thereby the myopia growth prevention was verified again.
With previous studies and evidence above, the OK lens delays the progression of myopia by inhibiting the posterior growth of the eye axis and reducing the defocus of the peripheral retinal hyperopia. Although this theory is generally recognized, details of the mechanism are still not clear. For the influence of OK on areas of the peripheral retina, relationships between defocus values of four sides of the peripheral retina and TRDV were analyzed through multiple linear regression.
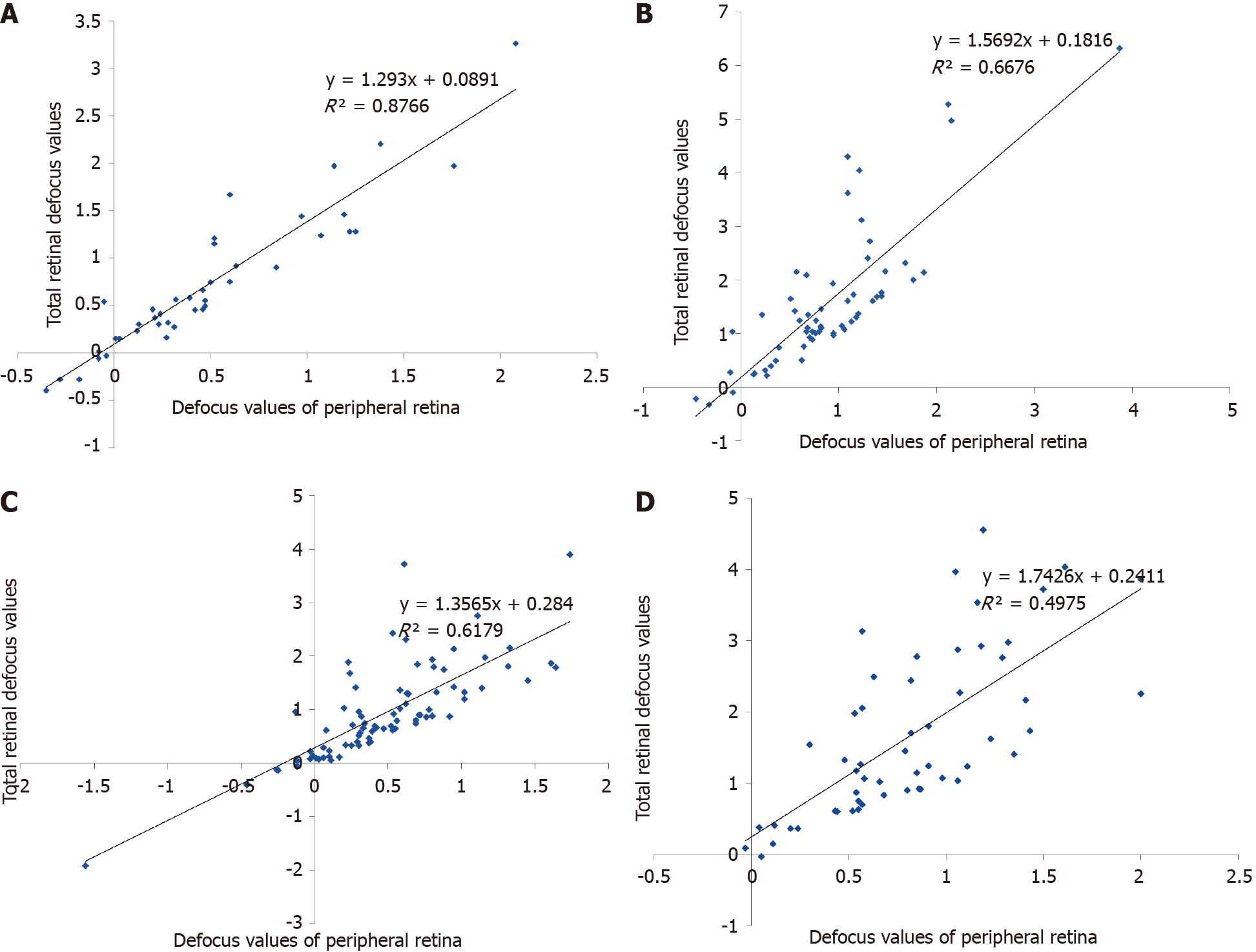
Undoubtedly, peripheral hyperopic defocus (15°-53°) showed a strong correlation with TRDV (patients with low myopia in group A: Correlation coefficient = 0.944, P < 0.001; patients with low myopia in group B: Correlation coefficient = 0.787, P < 0.001; patients with moderate myopia in group A: Correlation coefficient = 0.809, P < 0.001; patients with moderate myopia in group B: Correlation coefficient = 0.745, P < 0.001; correlation test was performed through Spearman test with non-normally distributed data; Figure 4). Peripheral hyperopic defocus (15°-53°) were also affected by treatment with OK lens, significantly lower among patients in group A (patients with low myopia: Z = -3.403, P < 0.001; patients with moderate myopia: Z = -3.905, P < 0.001; correlation test was performed through Mann-Whitney U test with non-normally distributed data).
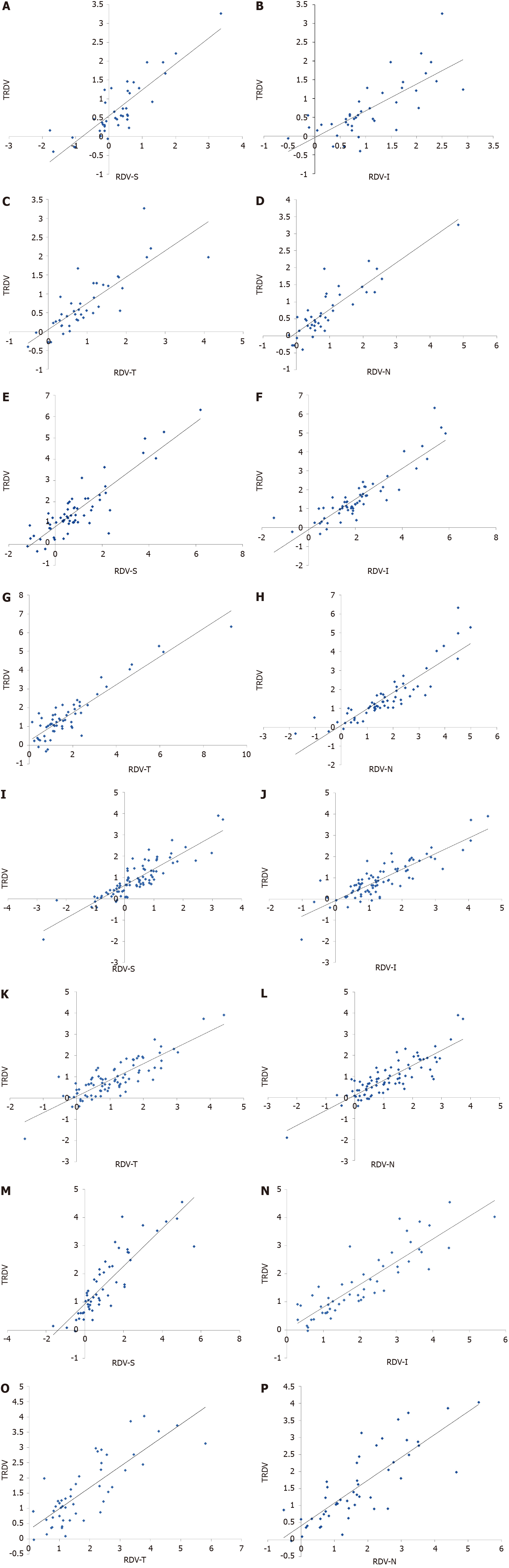
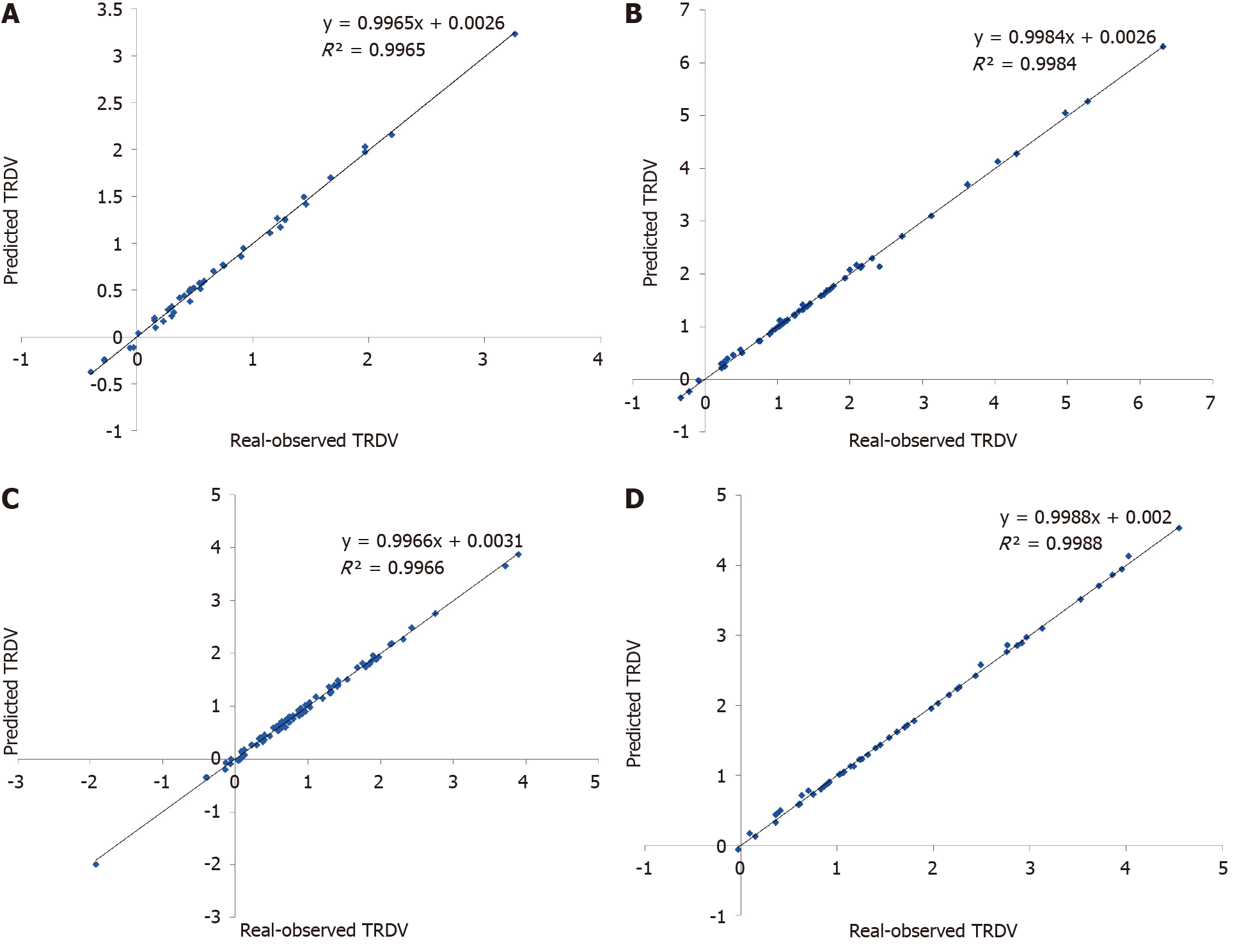
In addition, a certain degree of linearity between TRDV and defocus of the upper, lower, nasal, and temporal sides of the retina (Figure 5) existed for patients with low or moderate myopia treated with OK lenses or single-focal frame glasses. According to the multiple linear regression equation obtained, the predicted TRDV had a good linear relationship with the actual measured value (Regression equation: patients with low myopia in group A: TRDV = 0.265 × N + 0.270 × T + 0.233 × I + 0.237 × S - 0.094, R2 = 0.996; patients with low myopia in group B: TRDV = 0.241 × N + 0.250 × T + 0.256 × I + 0.252 × S - 0.043, R2 = 0.998; patients with moderate myopia in group A: TRDV = 0.262 × N + 0.274 × T + 0.239 × I + 0.224 × S - 0.091, R2 = 0.997; patients with moderate myopia in group B: TRDV = 0.248 × N + 0.250 × T + 0.249 × I + 0.255 × S - 0.046, R2 = 0.999, Figure 6).
To sum up, OK lenses control myopia development, delaying the growth rate of diopter and axis length through improving peripheral retinal defocus. Changes of TRDV appear equally on the four sides peripheral retina.
Myopia is an eye disease resulting from multiple factors, among which genetic and environmental factors play a major role[8]. With heavier study and academic pressure and the popularization of electronic products, the incidence of myopia in adolescents is increasing year by year. Moreover, complications of high myopia such as cataracts, glaucoma, and retinal detachment have increased significantly.
Currently, the most effective myopia prevention and control methods are: (1) Longer outdoor activities time, at least 2 h a day; (2) Effective optical correction, like OK; and (3) Drug treatments, such as low-concentration atropine eye drops[9,10]. Because of the side effects of atropine, the optically corrected OK lens is attracting people’s attention[9,11-13].
Undoubtedly, the current focus is myopia control and high myopia rate reduction. OK is highly valued for its effect on low- and moderate-myopia control. OK lenses are generally recognized to delay myopia growth now. It is reversible to correct myopia by temporary diopter reduction. Big data research shows that OK lenses can slow down the eye axis growth by approximately 0.15 mm/year and control refractive power increase (0.25-0.50 D/year)[14,15]. In a 2-year study by Santodomingo-Rubido et al[16] in patients aged 6-12 years, the axial length of patients wearing OK lenses increased by 0.47 mm, less than 0.69 mm in the group wearing frame glasses. The same conclusion was reached by the teams of Lau et al[17] and Na et al[18].
Currently, different opinions exist about the mechanism of myopia incidence. In recent years, a new concept has been proposed that signals from the periphery of the retina play a significant role in controlling myopia[19]. Smith[20] proved that the eye axis growth was accelerated through induced hyperopia defocus in the peripheral retina of young monkeys. After the removing inducement, the eye axis growth gradually slowed down and even returned to normal levels. Animal model research also revealed that not the central retina but the peripheral retina defocus mainly controlled the myopia progression[19]. Studies have shown that the peripheral retina has a more regulatory effect on the eye axis growth and myopia development than the fovea. Hyperopia defocus can be adjusted in the peripheral retina to delay myopia progression[21,22]. In addition to OK lenses, defocus soft lenses, defocus frame lenses, and multifocal soft lenses also represented their effects on reducing hyperopic defocus around the retina and delaying myopia development[11,23,24].
Depth estimation is a critical field of computer vision research. Generally, depth information is automatically extracted from one or a plurality of images of a scene[25-27]. The design of MRT is based on the depth estimation method of focus distance measurement. Thus, this classic method is creatively applied to the fundus depth estimation and further transformed into the refractive information of human eyes.
In this study, comparing patients of low or moderate myopia wearing OK and frame glasses for 1 year, the former showed significantly slower refractive power and eye axis growth, indicating the efficiency of OK lenses on delaying myopia development.
This study also confirmed that the initial defocus values and axis length could affect the following length growth after wearing OK lenses for 1-year[28,29]. After 1 year of treatment, the retinal hyperopic defocus were measured through MRT. In groups with low or moderate myopia, patients wearing OK lenses showed significantly lower TRDV than those wearing frame glasses. Eyeball growth backward was weakened by OK lenses, corresponding to lower TRD values; thus, the eye axis of those patients grew slower, and their refractive power of myopia increased less.
In addition, the 15°-53° (peripheral) hyperopic defocus values of the retina in the OK lens group were significantly lower than in the frame glasses group. In conclusion, OK lenses can reduce the peripheral retina hyperopia defocus values and delay the eye axis growth, thereby controlling myopia progression. This theory also has guiding significance for other myopia preventing and control methods, such as defocus soft lenses, defocus frame lenses, and multifocal soft lenses[30-32]. In this study, MRT was used to quantify the change in the peripheral retinal defocus, the delay of the eye axis growth, and the refractive power increase in the peripheral retina of the OK lens group. The final results were consistent with many studies at home and abroad[33-36].
With the popularity of electronic products, myopia incidence remains high in adolescents, seriously affecting the physical and mental health of children. Thus, this problem needs close attention.
MRT was used to detect the corneal state to obtain accurate diopter values. It has been proved that, whether wearing frame glasses or OK lenses, patients with moderate myopia showed higher retinal hyperopic defocus than those with low myopia. More samples and study time are necessary to study whether the retinal hyperopic defocus of patients is related to the aspheric shape of the cornea and the eye axis length. So far, MRT is the only advanced instrument to reproduce the amount of retinal defocus accurately. The data is accurate and reliable, having clinical applicability. It is advanced and instructive in clinical myopia prevention and control[37]. MRT can also be used to predict initial eye axis growth and myopia progression.
Myopia is a common eye disease often occurring among adolescents. Although the study-and-play surrounding of teenagers has been greatly improved in recent years, myopia incidence in China and some other developing countries is still quite high. As for myopia pathogenesis, a new hypothesis shows that myopia is controlled by signals from the retina’s periphery. To some extent, it explains how rigid gas-permeable contact lenses, like orthokeratology lens (OK lens) and single-focal glasses, testified effective in myopia control, slow down the growth rate of myopia degree. Based on computer depth estimation, multispectral refraction topography (MRT) technology can provide more accurate data containing more refractive information, especially the peripheral retina counterpart.
This study focused on the theory supporting OK lenses in myopia control. The treatment efficiency comparison between OK lenses and single-focal glasses revealed the effect of OK lenses in delaying diopter development, reducing the growth rate of the eye axis, and controlling total retinal defocus values (TRDV). Meanwhile, the effect of periphery retina on myopia progression was proved on another side. The myopia control mechanism of OK lenses provides guides for technical improvement of OK lenses and new possibilities for more effective myopia control.
In this study, MRT was involved in predicting myopia development and guiding myopia control. It provides more accurate data on myopia progression than traditional optometry methods. It is a new attempt, showing a further use of MRT in myopia prevention and control.
In this study, MRT was creatively combined with myopia treatment to explore the mechanism of OK lenses in preventing myopia growth. MRT was used to accurately quantify the retina hyperopia defocus, confirming that reducing the defocus of peripheral hyperopia can delay the eye axis growth and increase diopter.
Statistically significant differences were detected in diopter increase between patients treated with OK lenses and single-focal glasses. Regardless of low- or moderate myopia in the initial period, OK lenses were more effective than frame glasses. Similarly, when no significant difference existed in the original ocular axial length between the two groups, growth of eye axis was delayed more distinctly in groups wearing OK lenses. OK lenses were also more effective in TRDV control, which was certificated to be linearly associated with hyperopic defocus values of the peripheral retina (15°-53°). Improvement of TRDV occurred evenly on four sides of the retina.
The effects of OK lenses on controlling myopia development, reducing diopter growth rate and ocular axial length, and improving patients’ TRDV were certificated again in this study. More evidence that OK lenses affected myopia development through working on the peripheral retina was given by the strong relationship between TRDV and peripheral hyperopic defocus values. Those data were very valuably detected by MRT with high correctness and accuracy.
This study provided new evidence for old theories and hypotheses and proved the high value of MRT in ocular research, especially myopia-associated ones. Thus, it has been planned to expand the study size for more accurate and reliable data. This data may provide a new angle about how myopia developed and further how to prevent and control myopia.
We thank all medical staff and technicians who agreed to participate in this study.
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ikeda HO, Schuster AK S-Editor: Wang JL L-Editor: Filipodia P-Editor: Liu JH
| 1. | Yuan S, Zhang S, Jiang Y, Li L. Effect of short-term orthokeratology lens or ordinary frame glasses wear on corneal thickness, corneal endothelial cells and vision correction in adolescents with low to moderate myopia. BMC Ophthalmol. 2019;19:242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 711] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 3. | Xiang F, Morgan IG, He M. New perspectives on the prevention of myopia. Eye Sci. 2011;26:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Li SY, Li SM, Zhou YH, Liu LR, Li H, Kang MT, Zhan SY, Wang N, Millodot M. Effect of undercorrection on myopia progression in 12-year-old children. Graefes Arch Clin Exp Ophthalmol. 2015;253:1363-1368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Walline JJ, Lindsley K, Vedula SS, Cotter SA, Mutti DO, Twelker JD. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2011;CD004916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | Zhang Y, Chen Y. Effect of Orthokeratology on Axial Length Elongation in Anisomyopic Children. Optom Vis Sci. 2019;96:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 7. | Yu LH, Jin WQ, Mao XJ, Jiang J. Effect of orthokeratology on axial length elongation in moderate myopic and fellow high myopic eyes of children. Clin Exp Optom. 2021;104:22-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Xu GD. Visual optics and refractration. Beijing: Military Medical Science Press, 2005: 67-70. |
| 9. | Hieda O, Hiraoka T, Fujikado T, Ishiko S, Hasebe S, Torii H, Takahashi H, Nakamura Y, Sotozono C, Oshika T, Morimoto T, Nishida K, Nishikawa N, Song YS, Tokutake T, Nishi Y, Shigeno Y, Kurihara T, Negishi K, Tsubota K, Ono M, Nakai T, Tan D, Tanaka S, Kinoshita S; ATOM-J. Study Group. Efficacy and safety of 0.01% atropine for prevention of childhood myopia in a 2-year randomized placebo-controlled study. Jpn J Ophthalmol. 2021;65:315-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 10. | Jiang J. [Expert Consensus on Myopia Management White Paper (2019)]. Zhonghua Yanshiguangxue Yushijuekexue Zazhi. 2019;21:161-165. [DOI] [Full Text] |
| 11. | Sankaridurg P, Donovan L, Varnas S, Ho A, Chen X, Martinez A, Fisher S, Lin Z, Smith EL 3rd, Ge J, Holden B. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010;87:631-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 180] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 12. | Cheung SW, Boost MV, Cho P. Pre-treatment observation of axial elongation for evidence-based selection of children in Hong Kong for myopia control. Cont Lens Anterior Eye. 2019;42:392-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci. 2019;96:556-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 309] [Article Influence: 61.8] [Reference Citation Analysis (0)] |
| 14. | Huang J, Wen D, Wang Q, McAlinden C, Flitcroft I, Chen H, Saw SM, Bao F, Zhao Y, Hu L, Li X, Gao R, Lu W, Du Y, Jinag Z, Yu A, Lian H, Jiang Q, Yu Y, Qu J. Efficacy Comparison of 16 Interventions for Myopia Control in Children: A Network Meta-analysis. Ophthalmology. 2016;123:697-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 569] [Cited by in RCA: 493] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 15. | Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 294] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 16. | Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060-5065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 235] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 17. | Lau JK, Wan K, Cheung SW, Vincent SJ, Cho P. Weekly Changes in Axial Length and Choroidal Thickness in Children During and Following Orthokeratology Treatment With Different Compression Factors. Transl Vis Sci Technol. 2019;8:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 18. | Na M, Yoo A. The effect of orthokeratology on axial length elongation in children with myopia: Contralateral comparison study. Jpn J Ophthalmol. 2018;62:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965-3972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 353] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 20. | Smith EL 3rd. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88:1029-1044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 159] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 21. | Ho WC, Wong OY, Chan YC, Wong SW, Kee CS, Chan HH. Sign-dependent changes in retinal electrical activity with positive and negative defocus in the human eye. Vision Res. 2012;52:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004;43:447-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 708] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 23. | Leung JT, Brown B. Progression of myopia in Hong Kong Chinese schoolchildren is slowed by wearing progressive lenses. Optom Vis Sci. 1999;76:346-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 104] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Li SM, Kang MT, Wu SS, Meng B, Sun YY, Wei SF, Liu L, Peng X, Chen Z, Zhang F, Wang N. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow myopia progression in school-aged children: a meta-analysis. Ophthalmic Physiol Opt. 2017;37:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 25. | Khan F, Salahuddin S, Javidnia H. Deep Learning-Based Monocular Depth Estimation Methods-A State-of-the-Art Review. Sensors (Basel). 2020;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 26. | Pentland AP. A new sense for depth of field. IEEE Trans Pattern Anal Mach Intell. 1987;9:523-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 753] [Cited by in RCA: 190] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Jiang J, Zhang XS. Depth estimation methods based on computer vision. Guangdian Jishu Yingyong. 2011;26:51-55. [DOI] [Full Text] |
| 28. | Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 406] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 29. | Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53:3913-3919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 327] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 30. | Kang P, Fan Y, Oh K, Trac K, Zhang F, Swarbrick H. Effect of single vision soft contact lenses on peripheral refraction. Optom Vis Sci. 2012;89:1014-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol. 2014;98:40-45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 249] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 32. | Moore KE, Benoit JS, Berntsen DA. Spherical Soft Contact Lens Designs and Peripheral Defocus in Myopic Eyes. Optom Vis Sci. 2017;94:370-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 33. | Kong Q, Guo J, Zhou J, Zhang Y, Dou X. Factors Determining Effective Orthokeratology Treatment for Controlling Juvenile Myopia Progression. Iran J Public Health. 2017;46:1217-1222. [PubMed] |
| 34. | Cho P, Tan Q. Myopia and orthokeratology for myopia control. Clin Exp Optom. 2019;102:364-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 35. | Kang P, Swarbrick H. Time course of the effects of orthokeratology on peripheral refraction and corneal topography. Ophthalmic Physiol Opt. 2013;33:277-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 36. | Tsukiyama J, Miyamoto Y, Higaki S, Fukuda M, Shimomura Y. Changes in the anterior and posterior radii of the corneal curvature and anterior chamber depth by orthokeratology. Eye Contact Lens. 2008;34:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Panthier C, Burgos J, Rouger H, Saad A, Gatinel D. New objective lens density quantification method using swept-source optical coherence tomography technology: Comparison with existing methods. J Cataract Refract Surg. 2017;43:1575-1581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |