Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8186
Peer-review started: May 7, 2021
First decision: June 6, 2021
Revised: June 18, 2021
Accepted: July 19, 2021
Article in press: July 19, 2021
Published online: September 26, 2021
Processing time: 132 Days and 8 Hours
Organophosphorus poisoning (OP) is one of the common critical conditions in emergency departments in China, which is usually caused by suicide by taking oral drugs. Patients with severe OP have disturbance of consciousness, respiratory failure, toxic shock, gastrointestinal dysfunction, and so on. As far as we know, the perforation of the duodenum caused by OP has not been reported yet.
A 33-year-old male patient suffered from acute severe OP, associated with abdominal pain. Multiple computed tomography scans of the upper abdomen showed no evidence of intestinal perforation. However, retrograde digital subtraction angiography, performed via an abdominal drainage tube, revealed duodenal perforation. After conservative treatment, the symptoms eased and the patient was discharged from hospital.
Clinicians should pay close attention to gastrointestinal dysfunction and abdominal signs in patients with severe OP. If clinical manifestation and vital signs cannot be explained by common complications, stress duodenal ulcer or perforation should be highly suspected.
Core Tip: Organophosphorus poisoning is one of the common critical conditions in emergency departments in China and is usually caused by suicide. However, duodenal perforation caused by organophosphorus poisoning has not yet been reported. In this case, organophosphorus poisoning induced duodenal perforation, and the potential mechanism involves drug toxicity, physical injury caused by gastric lavage, or a stress response to acute poisoning, and severe shock.
- Citation: Lu YL, Hu J, Zhang LY, Cen XY, Yang DH, Yu AY. Duodenal perforation after organophosphorus poisoning: A case report. World J Clin Cases 2021; 9(27): 8186-8191
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8186.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8186
Organophosphorus poisoning (OP) is one of the common critical conditions in emergency departments in China, accounting for 49.1% of acute poisonings and 83.6% of poisoning-related deaths. In the vast southwestern regions of China, pesticide use and storage are poorly managed, and thus, people sometimes commit suicide by oral administration of pesticides. Patients with severe OP usually have disturbance of consciousness, respiratory failure, toxic shock, and gastrointestinal dysfunction[1]. However, concurrent duodenal perforation has not been reported in the literature. We treated one case of duodenal perforation secondary to severe acute OP.
A 33-year-old man attempted suicide 4 h ago because of taking an unknown dose of dichlorvos, and was admitted to the emergency department of our hospital.
The patient was hospitalized due to acute severe phosphorus poisoning. He drank before oral dose of unknown dichlorvos and was found foaming at the mouth and sweating, with cyanotic lips and no response to calls. Gastric lavage and atropine treatment were administered at a local hospital. He was later transferred to our hospital.
The patient had a free previous medical history.
The patient had no personal and family history.
On examination, the vital signs showed an unmeasurable body temperature, heart rate of 127/min, blood pressure of 61/39 mmHg, and SPO2 of 82%, invasive ventilator assisted ventilation, slight coma, moist skin and mucous membrane, no light reflection, a garlic smell in the mouth, a thick breathing sound of both lungs, a little damp rale in the left lower lung, a soft and flat abdomen, and normal bowel sounds.
Auxiliary examination showed a cholinesterase level of 0.26 kU/L.
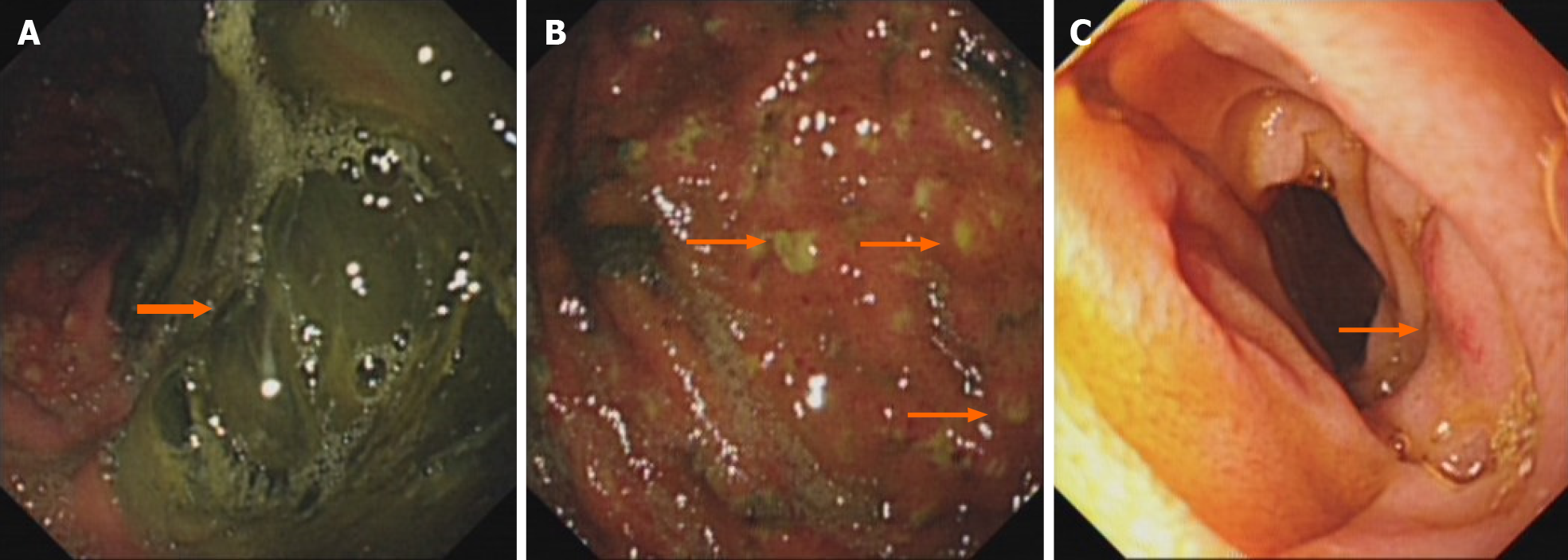
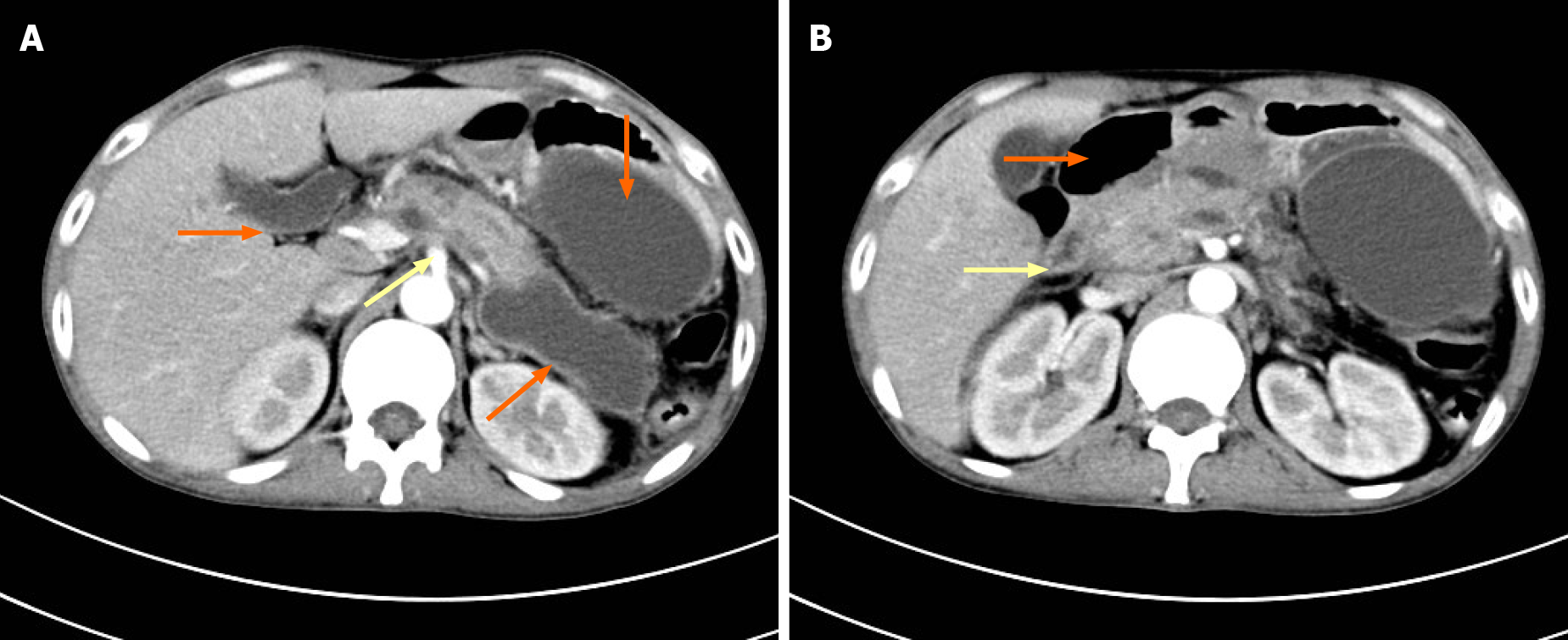
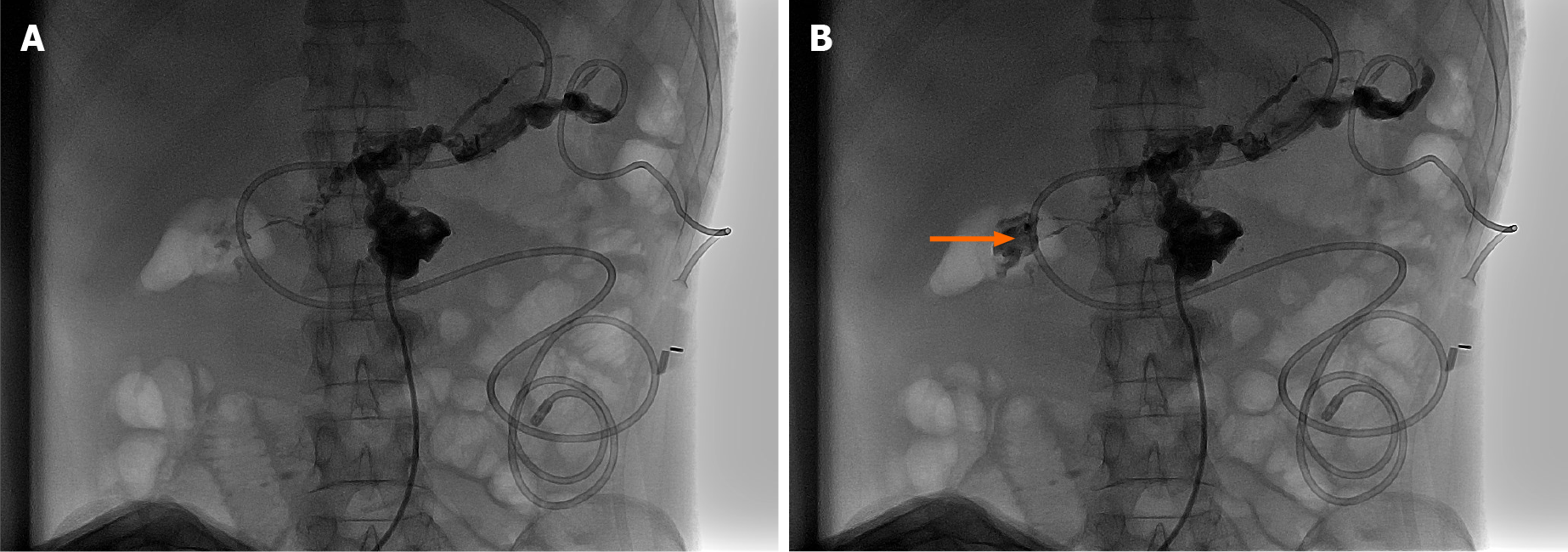
Gastroscopy performed on September 3, 2018 showed that there were a large number of dark green secretions and membranous substances in the stomach cavity (Figure 1A), and there were many bulges in the mucosa of the stomach cavity, purulent secretions at the top, and obvious congestion in the surrounding mucosa (Figure 1B). It also showed congestion and edema in part of the descending duodenum (Figure 1C). Computed tomography (CT) of the upper abdomen performed on September 18, 2018 showed acute pancreatitis and multiple pancreatic pseudocysts (Figure 2A), as well as descending duodenal edema and pneumatosis (Figure 2B). From September 3, 2018 to October 3, 2018, repeated CT of the upper abdomen showed no sign of intestinal perforation. However, digital subtraction angiography (DSA) performed on October 2, 2018 revealed that iohexol, a contrast agent, had been distributed around pancreatic pseudocyst through a drainage tube (Figure 3A) and the descending duodenum (Figure 3B), which confirmed duodenal perforation.
Duodenal fistula was finally diagnosed by retrograde DSA through a drainage tube in the median abdomen.
The patient received gastric lavage, catharsis, a special antidote, blood purification, ventilator-assisted respiration, and vasoactive drugs for boosting blood pressure. The patient was seriously ill, and the above-mentioned rescue measures significantly improved his symptoms. He still presented remarkable abdominal bulging and tenderness in the upper abdomen, accompanied by local muscular tension and weakened bowel sounds. Abdominal CT scanning indicated the possibility of acute pancreatitis. He underwent fasting, enzyme therapy, and acid suppression, as well as jejunal nutrition. Additionally, the traditional Chinese medical prescription Qingyi II was administered to restore normal bowel movement. All symptoms were alleviated, and thus, the tracheal intubation was removed, and vital signs became stable. Four weeks after admission, multiple pseudocysts were observed, peripheral to the pancreas (Figure 2A). CT-guided puncture and drainage were performed, and 300 mL of a light-yellow fluid was drawn from the left upper and median abdomen. Abdominal CT demonstrated that the peripancreatic cysts shrank and their number was reduced. The concentration of amylase was lowered, and abdominal pain was significantly relieved. At 40 d after admission, the patient experienced intensified abdominal pain after oral ingestion of a small amount of a fluid diet, and the volume of the drainage fluid from the median abdomen increased to 500 mL. Retrograde DSA was performed through a drainage tube in the median abdomen (Figure 3), which confirmed duodenal perforation. According to the surgical consultation, since the patient was in a poor general condition and the perforated duodenum was enveloped, there was no indication for surgery. The patient underwent fasting and conservative treatment and then was discharged with a drainage tube.
The patient was discharged with a drainage tube and had a normal diet 5 wk after the jejunal nutrition tube was removed. Angiography of the upper digestive tract showed no abnormalities in the duodenum.
Organophosphorus pesticides are widely used in agriculture in China and are regarded as one of the main sources of poisoning. The poisoning mechanism in humans and animals involves the inhibition of the acetylcholine enzyme and causes the accumulation of acetylcholine, leading to muscarinic and nicotine toxicity and central nervous system dysfunction[2]. Patients with severe OP usually have clinical manifestations including disturbance of consciousness, respiratory failure, toxic shock, and gastrointestinal dysfunction.
Gastrointestinal dysfunction is closely related to the development and aggravation of OP. The mechanism involves the direct damage of the poison to the gastrointestinal mucosa, mucosal atrophy, shortening of villi, and increased vascular permeability. There are few cases of OP complicated with acute pancreatitis in the literature, and there are fewer cases of severe pancreatitis after operation[3], but there are no case of duodenal perforation. Previous research reported yellow phosphorus poisoning, which is one of the raw materials for synthesizing organophosphorus pesticides and could lead to explosive liver failure and duodenal perforation[4]. Duodenal perforation is mainly caused by a duodenal ulcer and diverticulum, traumatic injury, iatrogenic endoscopic injury, a foreign body[5,6], and corrosive drug poisoning[4]. In this case, the difficult and eventful diagnosis and treatment of duodenal perforation after severe, acute OP may be attributed to the following facts: (1) The physical injury, caused by the pesticide and gastric lavage, or a stress reaction, caused by acute poisoning and severe shock, resulted in mucosal injury and gastrointestinal bleeding[7], e.g., an acute gastric lesion shown in Figure 1. Gastroscopy showed that there were many bulges in the mucosa of the stomach cavity, purulent secretions at the top, and obvious congestion in the surrounding mucosa (Figure 1B), and edema in part of the descending duodenum (Figure 1C); (2) Atropine, which was administered against poisoning, inhibited intestinal peristalsis and promoted the absorption of intestinal edema and toxins, further leading to an increased abdominal pressure (maximum: 27 cm H2O) and weakened bowel sounds[8]; (3) Severe poisoning caused serious hemodynamic changes and hypoxia. The concentration of lactic acid was 13.0 mmol/L, and therefore, a high dose of norepinephrine was administered to maintain blood pressure. Key organs were in ischemia and hypoxia[9], and the gastrointestinal tract might have also been impaired. Mahajan et al[7] reported that one patient with severe OP developed multiple perforations in the small intestine after the patient fell in shock; (4) The organs in the abdominal cavity were damaged, and pseudocysts were formed because of pancreatic secretion. The pancreatic fluid corroded the surrounding intestinal wall. Retrograde DSA via a drainage tube on a pseudocyst of the pancreatic head showed that a peripancreatic pseudocyst was connected to the duodenum (Figure 3B); and (5) The patient was in sedation and analgesia for critical care. The perforated part was enveloped, and therefore, no diffuse peritonitis developed. The abdominal symptoms were not thoroughly observed, and gastroscopy and abdominal CT showed no free gas below the diaphragm, leading to the missed diagnosis of duodenal perforation. Due to the aggravated abdominal pain and a sudden increase in abdominal drainage, retrograde angiography was performed via a drainage tube to confirm duodenal perforation. CT of the upper abdomen and gastroscopy are effective for the diagnosis of duodenal perforation. However, abdominal CT is superior to X-ray, with a higher sensitivity and specificity in detecting free gas outside the abdominal cavity and with a better view of the perforated section. In this case, the missed diagnosis of duodenal perforation at an early stage was due to severe toxic symptoms, repeated abdominal pain, and a small perforation and package. No typical signs of peritonitis were observed, which made it difficult to reach a definitive diagnosis. Finally, retrograde angiography confirmed duodenal perforation. Because the patient was in a poor general condition and had low immunity, conservative treatment was provided. Upper gastrointestinal angiography at 4 weeks after discharge showed no duodenal abnormalities. Compared with those undergoing surgical treatment, patients who undergo conservative treatment have fewer complications and a lower mortality.
Duodenal perforation caused by OP has not yet been reported. In the clinic, many factors such as duodenal ulcer and diverticulum, traumatic injury, iatrogenic endoscopic injury, a foreign body, and corrosive drug poisoning can induce duodenal perforation. In patients with severe OP, clinicians should pay close attention to the damage to gastrointestinal function and to abdominal signs. If clinical manifestations and signs go beyond common complications, stress-induced duodenal ulcer and perforation should be highly suspected.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abubakar MS, Ravikanth R S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wu RR
| 1. | Haliga RE, Morarasu BC, Ursaru M, Irimioaia V, Sorodoc L. New insights into the organophosphate-induced intermediate syndrome. Arh Hig Rada Toksikol. 2018;69:191-195. [PubMed] [DOI] [Full Text] |
| 2. | Malinak D, Nepovimova E, Jun D, Musilek K, Kuca K. Novel Group of AChE Reactivators-Synthesis, In Vitro Reactivation and Molecular Docking Study. Molecules. 2018;23. [PubMed] [DOI] [Full Text] |
| 3. | Hou R, Zhang H, Chen H, Zhou Y, Long Y, Liu D. Total pancreatic necrosis after organophosphate intoxication. Front Med. 2019;13:285-288. [PubMed] [DOI] [Full Text] |
| 4. | Ravikanth R, Sandeep S, Philip B. Acute Yellow Phosphorus Poisoning Causing Fulminant Hepatic Failure with Parenchymal Hemorrhages and Contained Duodenal Perforation. Indian J Crit Care Med. 2017;21:238-242. [PubMed] [DOI] [Full Text] |
| 5. | Yang Z, Wu D, Xiong D, Li Y. Gastrointestinal perforation secondary to accidental ingestion of toothpicks: A series case report. Medicine (Baltimore). 2017;96:e9066. [PubMed] [DOI] [Full Text] |
| 6. | Donald KJ, Doherty SR, Shun A. Duodenal perforation: an interesting case report. Emerg Med Australas. 2005;17:46-48. [PubMed] [DOI] [Full Text] |
| 7. | Mahajan RK, Rajan SJ, Peter JV, Suryawanshi MK. Multiple Small Intestine Perforations after Organophosphorous Poisoning: A Case Report. J Clin Diagn Res. 2016;10:GD06-GD07. [PubMed] [DOI] [Full Text] |
| 8. | Mostafazadeh B, Farzaneh E, Paeezi M, Nikkhah F. Toxic megacolon as a rare complication following atropine therapy due to organophosphate poisoning: A case report. Med Leg J. 2017;85:221-223. [PubMed] [DOI] [Full Text] |
| 9. | Yuan S, Gao Y, Ji W, Song J, Mei X. The evaluation of acute physiology and chronic health evaluation II score, poisoning severity score, sequential organ failure assessment score combine with lactate to assess the prognosis of the patients with acute organophosphate pesticide poisoning. Medicine (Baltimore). 2018;97:e10862. [PubMed] [DOI] [Full Text] |