Published online Feb 16, 2017. doi: 10.12998/wjcc.v5.i2.35
Peer-review started: July 3, 2016
First decision: September 5, 2016
Revised: November 19, 2016
Accepted: December 27, 2016
Article in press: December 28, 2016
Published online: February 16, 2017
Processing time: 230 Days and 11.9 Hours
Kikuchi-Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is an uncommon condition, typically characterized by lymphadenopathy and fevers. It usually has a benign course; however, it may progress to fatality in extremely rare occasions. The diagnosis is made via lymph node biopsy and histopathology. Our patient was a young female who presented with shortness of breath, fever, and malaise. Physical examination revealed significant cervical and axillary lymphadenopathy. Chest X-ray displayed multilobar pneumonia. She required intubation and mechanical ventilation for progressive respiratory distress. Histopathology of lymph nodes demonstrated variable involvement of patchy areas of necrosis within the paracortex composed of karyorrhectic debris with abundant histiocytes consistent with KFD. After initial stabilization, the patient’s condition quickly deteriorated with acute anemia, thrombocytopenia and elevated prothrombin time, partial prothrombin time, and D-dimer levels. Disseminated intravascular coagulopathy (DIC) ensued resulting in the patient’s fatality. DIC in KFD is not well understood, but it is an important cause of mortality in patients with aggressive disease.
Core tip: Kikuchi-Fujimoto disease (KFD), or histiocytic necrotizing lymphadenitis, is an uncommon condition, typically characterized by lymphadenopathy and fevers. KFD is an extremely rare disease. With this case we wish to highlight that KFD carries a risk of mortality in the setting of acute, aggressive disease, which is in contrast to the benign, self-limiting condition that has been classically documented in literature. The patient emphasizes the importance of recognizing this as we present the fourth case of disseminated intravascular coagulopathy as a cause of fatality in these patients.
- Citation: Barbat B, Jhaj R, Khurram D. Fatality in Kikuchi-Fujimoto disease: A rare phenomenon. World J Clin Cases 2017; 5(2): 35-39
- URL: https://www.wjgnet.com/2307-8960/full/v5/i2/35.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i2.35
Kikuchi-Fujimoto disease (KFD), or histiocytic necrotizing lymphadenitis, is a rare, self-limiting condition characterized by regional lymphadenopathy, fevers, night sweats, and upper respiratory symptoms. Although a viral or autoimmune pathogenesis has been suggested, the etiology continues to remain unknown. Diagnosis is based on histologic features noted on excisional biopsy. A majority of cases have a benign course; rarely does KFD result in death. After performing a wide literature search, we only found three other documented cases that resulted in death from disseminated intravascular coagulopathy (DIC). This disease was initially thought to have a predilection for Asian women between the ages of 20 and 35 years. However, new cases of KFD have also been described in non-Asian ethnicity and young age groups in the United States[1]. Recognition of KFD is essential because it can easily be mistaken for lymphoma, tuberculosis, or carcinoma[2]. Here we report a case of a patient with KFD who died secondary to DIC.
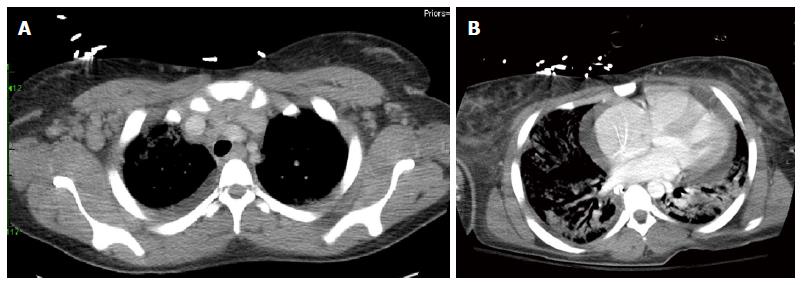
The patient was a previously healthy, 21-year-old female who presented with a two-day history of dyspnea, fever, and malaise. Initial set of vitals revealed a blood pressure of 109/57 mmHg, temperature of 38.2 °C, heart rate of 118 bpm, respiratory rate of 24 breaths/min, and oxygen saturation of 78% on room air. On 4 liters of nasal cannula, her oxygen saturation improved to 97%. A chest X-ray demonstrated multifocal pneumonia. Treatment for community-acquired pneumonia was initiated with ceftriaxone and azithromycin. On physical examination, she was noted to have significant axillary, cervical and inguinal lymphadenopathy. Her respiratory status continued to decline despite supplemental oxygen therapy and antibiotics, requiring emergent endotracheal intubation with mechanical ventilation. A computerized tomography (CT) chest, abdomen, and pelvis was performed, which revealed significant cervical and axillary lymphadenopathy, bilateral lung consolidation, and a moderate pericardial effusion (Figure 1).
As the patient’s presentation was very severe, a comprehensive differential was considered. Among the entire laboratory data that was performed HIV, streptococcus pneumonia, legionella, histoplasma, brucella, aspergillus, tuberculosis, influenza, respiratory syncytial virus were negative. There was a mild elevation in mycoplasma IgM and chlamydia antibody titer. The patient’s antibiotic therapy was tailored to include a broader spectrum of organisms. Bronchoscopy with bronchoalveolar lavage was performed given the above CT findings. There was no evidence of mucus plugs, active bleeding, endobronchial lesions or anatomical abnormalities. Pathology of the fluid revealed presence of acute inflammatory cells. A transthoracic echocardiogram revealed normal systolic function with a moderate pericardial effusion without tamponade physiology.
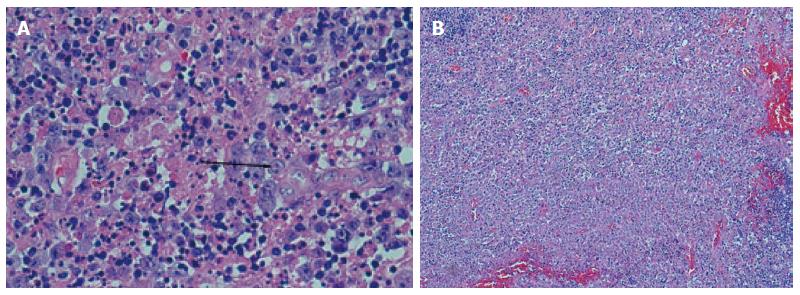
Due to the significant lymphadenopathy, pericardial effusion, and an elevated LDH of 2319 unit/L, a concern for lymphoma was raised. Therefore, a cervical lymph node biopsy was performed. Histopathology demonstrated variable involvement of patchy small to large areas of necrosis within the paracortex. The necrotic areas were composed of karyorrhectic debris with abundant histiocytes consistent with KFD (Figure 2).
Septic work up consisting of blood, sputum and urine cultures remained negative throughout her admission. Despite aggressive antibiotic therapy, high dose steroids, and supportive care, the patient’s condition continued to decline. She required increasing pressure support to maintain oxygenation. Intravenous immune globulin (IVIG) was given without any improvement in the patient’s symptoms. The hemoglobin level began to precipitately decrease without any active sites of bleeding. A hemolytic work up was initiated, which revealed a haptogobin < 10 mg/dL and schistocytes on peripheral smear. She then developed significant thrombocytopenia with platelet level recorded as low as 26 K/mcL. Partial thromboplastin time, prothrombin time levels and D-dimer levels started to rise. Fresh frozen plasma was transfused for impending DIC. The patient’s clinical condition and laboratory parameters continued to deteriorate despite resuscitative efforts in the intensive care unit. Unfortunately, she expired secondary to development of DIC.
KFD, or histiocytic necrotizing lymphadenitis, is rare and usually has a benign self-limiting course. The etiology of this disease has not been established yet, but there are viral origins including HHV-6, HHV-8, and EBV that have been theorized[3]. One study found that apoptotic cell death plays a role in the pathogenesis of KFD[4]. The most common symptoms include, but are not limited to lymphadenopathy, fatigue, fevers, night sweats and weight loss.
There are no specific laboratory values that are pathognomonic for this disease. A case review of 244 patients with KFD revealed laboratory values that were unremarkable except for an elevated ESR, mild neutropenia, and lymphocytosis in some cases[5]. Imaging can aid in limiting the differential diagnosis. CT and magnetic resonance imaging can be useful for evaluating patients with cervical lymphadenopathy. CT features may mimic those of lymphoma; however, lymph nodes in KFD are not as large as those in lymphoma[6].
A definite diagnosis of KFD is made by biopsy, typically excisional, but fine needle aspiration has also been used. There are some characteristic histologic features of KFD including patchy necrotizing areas primarily in the paracortical regions that contain fibrinous material with karyorrhexis. A distinctive mottled appearance may be noted, as immunoblasts tend to border necrotic zones[7]. Early diagnosis is important as the clinical and laboratory presentations can imitate situations needing time-consuming and expensive interventions[5]. KFD can be easily misdiagnosed; literature estimates as high as 40% of the time with lymphoma being the most commonly mistaken diagnosis[8].
Once the diagnosis is made, symptomatic and supportive treatment is usually adequate. When symptomatology requires treatment, a short course of corticosteroids is preferred. Currently, there are no recommendations on exact dosage or route of administration[9]. In severe cases, high dose intravenous steroids have been shown to be effective and aid in symptom reduction[10]. IVIG has been shown to be successful in several, critical cases. Once again, no formal recommendations on dosing and duration exist. IVIG has been routinely implemented as empiric therapy in autoimmune and inflammatory processes secondary to its immunomodulatory properties[11]. In individuals with a benign hospital course, it is important to have adequate follow up as patients have an increased risk of relapse. One study showed that hydroxychloroquine could be used in the treatment of relapsed KFD[12]. On rare instances, despite these treatment modalities, KFD may progress to mortality such as the patient we presented.
Our patient is unique as she had an extremely progressive course of Kikuchi lymphadenitis with subsequent multiorgan failure and death from DIC. In our review of literature, we found three other documented cases of death in KFD as a result of DIC (Table 1)[13,14]. Other causes of death included hemophagocytic syndrome and severe infection[15], pulmonary hemorrhage[16] and acute heart failure[17].
| Ref. | Presentation | Presence of autoantibodies | Cause of death |
| Uslu et al[13], 2014 | A 32-year-old female with fever, fatigue, chest and abdominal pain for 15 d | Not mentioned | DIC |
| Sharma et al[14], 2015 | A 57-year-old fever with fever and UTI | Yes: ANA, anti- La, anti-RNP | Septic shock and DIC |
| Sharma et al[14], 2015 | A 55-year-old female with fever, dizziness, loss of balance, decreased hearing, diarrhea, vomiting and a non-blanching rash over the upper arms and thighs | Yes: Anti-Ro and anti-La | DIC |
The precise mechanism of DIC in KFD is unknown. A proposed mechanism involves a massive cytokine release during the acute phase of the disease, mainly consisting of tumor necrosis factor-alpha, interleukin-1, and interleukin-6. These cytokines result in significant endothelial damage and activation of the thrombosis and anticoagulation cascade pathognomonic for DIC[13]. In our patient, all other potential causes of DIC including sepsis and acute myeloid leukemia were negative, supporting the association of DIC and KFD.
KFD is an extremely rare disease. With this case we wish to highlight that KFD carries a risk of mortality in the setting of acute, aggressive disease, which is in contrast to the benign, self-limiting condition that has classically been documented in literature. Our patient emphasizes the importance of recognizing this fact as we present the fourth case of DIC as a cause of fatality in these patients.
The patient is a 21-year-old female who presented with symptoms of malaise and fevers.
The main clinical findings included cervical and axillary lymphadenopathy.
Differential diagnosis included lymphoma, viral syndrome and bacterial infections. Computerized tomography scan findings confirmed the lymphadenopathy as well as bilateral lung consolidation, and a moderate pericardial effusion. Histopathology of the lymph node biopsy revealed findings consistent with Kikuchi-Fujimoto disease (KFD).
In most cases, supportive treatment is adequate. In severe cases and relapsing cases, intravenous immune globulin and hydroxychloroquine have been used, respectively.
Unfortunately, our patient expired secondary to disseminated intravascular coagulopathy (DIC). The exact mechanism of how DIC occurs in KFD is unknown; however, it has been proposed that cytokine release plays a role. With this case we wish to highlight that KFD carries a risk of mortality in the setting of acute, aggressive disease, which is in contrast to the benign, self-limiting condition that has classically been documented in literature.
KFD: Kikuchi-Fujimoto disease.
KFD is an extremely rare disease. The authors highlighted that KFD carries a risk of mortality in the setting of acute, aggressive disease, which is in contrast to the benign, self-limiting condition that has been classically documented in literature. This set of cases emphasizes the importance of recognizing the fact of DIC as a cause of fatality in these patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Gac P, Li YZ, Razek AAKA S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Deaver D, Horna P, Cualing H, Sokol L. Pathogenesis, diagnosis, and management of Kikuchi-Fujimoto disease. Cancer Control. 2014;21:313-321. [PubMed] |
| 2. | Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol. 2004;122:141-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 120] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Ifeacho S, Aung T, Akinsola M. Kikuchi-Fujimoto Disease: A case report and review of the literature. Cases J. 2008;1:187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Iguchi H, Sunami K, Yamane H, Konishi K, Takayama M, Nakai Y, Nakagawa T, Shibata S, Nishimura K. Apoptotic cell death in Kikuchi’s disease: a TEM study. Acta Otolaryngol Suppl. 1998;538:250-253. [PubMed] |
| 5. | Kucukardali Y, Solmazgul E, Kunter E, Oncul O, Yildirim S, Kaplan M. Kikuchi-Fujimoto Disease: analysis of 244 cases. Clin Rheumatol. 2007;26:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 243] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 6. | Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY. CT findings in Kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol. 2004;25:1099-1102. [PubMed] |
| 7. | Silva AF, Focaccia R, Oliveira AC, Sementilli A, Reis GF. Kikuchi-Fujimoto disease: an unusual association with acute renal failure. Braz J Infect Dis. 2010;14:621-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Ramirez AL, Johnson J, Murr AH. Kikuchi-Fujimoto’s disease: an easily misdiagnosed clinical entity. Otolaryngol Head Neck Surg. 2001;125:651-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Dumas G, Prendki V, Haroche J, Amoura Z, Cacoub P, Galicier L, Meyer O, Rapp C, Deligny C, Godeau B. Kikuchi-Fujimoto disease: retrospective study of 91 cases and review of the literature. Medicine (Baltimore). 2014;93:372-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Jang YJ, Park KH, Seok HJ. Management of Kikuchi’s disease using glucocorticoid. J Laryngol Otol. 2000;114:709-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 82] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Noursadeghi M, Aqel N, Gibson P, Pasvol G. Successful treatment of severe Kikuchi’s disease with intravenous immunoglobulin. Rheumatology (Oxford). 2006;45:235-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Rezai K, Kuchipudi S, Chundi V, Ariga R, Loew J, Sha BE. Kikuchi-Fujimoto disease: hydroxychloroquine as a treatment. Clin Infect Dis. 2004;39:e124-e126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Uslu E, Gurbuz S, Erden A, Aykas F, Karagoz H, Karahan S, Karaman H, Cetinkaya A, Avci D. Disseminated intravascular coagulopathy caused by Kikuchi-Fujimoto disease resulting in death: first case report in Turkey. Int Med Case Rep J. 2014;7:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Sharma V, Rankin R. Fatal Kikuchi-like lymphadenitis associated with connective tissue disease: a report of two cases and review of the literature. Springerplus. 2015;4:167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Kampitak T. Fatal Kikuchi-Fujimoto disease associated with SLE and hemophagocytic syndrome: a case report. Clin Rheumatol. 2008;27:1073-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Wong CY, Law GT, Shum TT, Wong KY, Li YK. Pulmonary haemorrhage in a patient with Kikuchi disease. Monaldi Arch Chest Dis. 2001;56:118-120. [PubMed] |
| 17. | Chan JK, Wong KC, Ng CS. A fatal case of multicentric Kikuchi’s histiocytic necrotizing lymphadenitis. Cancer. 1989;63:1856-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |