Published online Aug 16, 2022. doi: 10.12998/wjcc.v10.i23.8367
Peer-review started: March 17, 2022
First decision: May 12, 2022
Revised: May 20, 2022
Accepted: July 11, 2022
Article in press: July 11, 2022
Published online: August 16, 2022
Processing time: 137 Days and 0.6 Hours
Fused teeth usually involve several complications, such as the development of caries in the groove between fused crowns, tooth impaction, diastemas, aesthetic and periodontal problems, and pulpal pathosis, due to the complex anatomical structure of fused teeth. A thorough diagnosis is paramount to forming an acc
This report details the diagnosis and endodontic treatment of a rare case involving a fused maxillary second molar and two paramolars with apical periodontitis. The patient experienced pain upon biting and cold sensitivity in the area of the maxillary left molar. No caries or other defects were identified in these teeth, and a normal response to a pulp electric viability test was observed. With the aid of CBCT and digital model technology, we initially suspected that the infection originated from the isthmus between the maxillary second molar and two paramolars. Therefore, we only treated the isthmus by an endodontic approach and did not destroy the original tooth structure; furthermore, the vital pulp was retained, and good treatment outcomes were observed at the 24-month follow-up.
This finding may provide new insights and perspectives on the diagnosis and treatment of fused teeth.
Core Tip: Fused teeth usually involve several complications due to their complex anatomical structure. A thorough diagnosis is of vital importance. With the aid of cone-beam computed tomography (CBCT) and digital model technology, accurate 3-dimensional images of teeth can be obtained; thus, CBCT provides a minimally invasive approach to acquiring detailed diagnostic information. In this report, we utilized CBCT data to generate a digital model of a fused tooth and only treated the infected isthmus by an endodontic approach. Good treatment outcomes were observed at the 24-month follow-up. This finding provides new perspectives on the diagnosis and treatment of fused teeth.
- Citation: Mei XH, Liu J, Wang W, Zhang QX, Hong T, Bai SZ, Cheng XG, Tian Y, Jiang WK. Endodontic management of a fused left maxillary second molar and two paramolars using cone beam computed tomography: A case report. World J Clin Cases 2022; 10(23): 8367-8374
- URL: https://www.wjgnet.com/2307-8960/full/v10/i23/8367.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i23.8367
During endodontic treatments, obtaining a thorough diagnosis is paramount for preparing an accurate treatment plan that results in a favourable prognosis. However, complex anatomical structures often introduce challenges to forming diagnoses and performing treatments. The incidence of fusion is approximately 0.1% in permanent dentition and 0.5% in primary dentition[1]. During tooth deve
Clinically, fused teeth may cause several complications, such as the development of caries in the groove between the fused crowns, tooth impaction, diastemas, aesthetic and periodontal problems, and pulpal pathosis. Many of these complications necessitate a multidisciplinary approach, and the treatment depends on the type and position of the supernumerary tooth as well as its relation to the adjacent teeth[7]. In endodontics, periapical X-ray (PAX) is mandatory for diagnosis, treatment, and follow-up. However, such images provide a limited 2-dimensional view of the true 3-dimensional (3D) anatomy. With the advent of cone-beam computed tomography (CBCT), accurate 3D images of teeth and their surrounding dentoalveolar structures can be readily obtained[8], and the technology can accurately provide a minimally invasive approach to acquire detailed diagnostic information[9].
In this study, a rare case of fusion between a maxillary second molar and two paramolars is described. 3D images were obtained to visualize the relationship of the supernumerary to its counterpart. The low-density transmission image was extended along the isthmus pathway to the apical area, and it was clearly observed that the roots of the two supernumerary teeth were fused with the mesial buccal roots of the second molar and that the root canal systems of the two supernumerary teeth intersected in the middle 1/3 of the root and the apical area; moreover, no communication was observed between the canal systems of the teeth. To determine if normal pulp was present, electric pulp testing was adopted; this test was also utilized to gain confidence in performing more accurate and conservative treatment methods. With the goal of preserving the vitality of the unaffected counterpart, this patient underwent endodontic treatment of the isthmus pathway, thereby eliminating periapical tissue inflammation.
A 24-year-old male presented to the Department of Operative Dentistry and Endodontics of the Fourth Military Medical University with complaints of pain upon biting and cold sensitivity on his maxillary left molar; notably, these symptoms had occurred for approximately 1 month.
For approximately one month, the patient felt pain in his maxillary left molar while chewing, and the tooth was sensitive to cold. Before this time, the tooth did not exhibit spontaneous pain.
The patient did not have a relevant medical history. He did not report any history of drug allergies or systemic diseases and exhibited no apparent dental treatment contraindications.
The patient did not report any personal and family history.
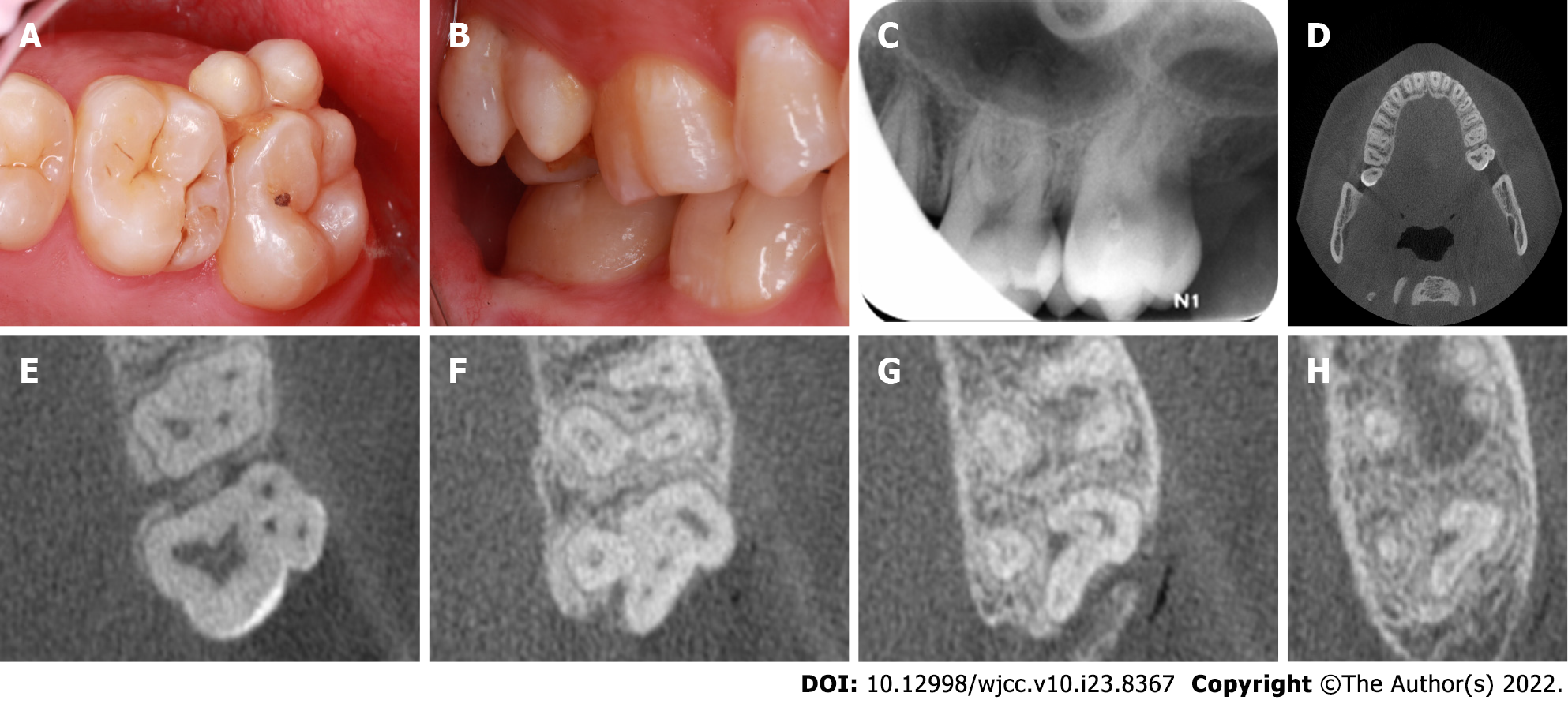
Clinical analyses revealed the presence of two extra teeth on the buccal aspect of the maxillary left second molar (#15); however, these teeth were separated by distinct developmental grooves (Figure 1A and B). Long-term impaction of food caused gingival recession in this region, but no caries or other obvious defects were detected. Decay in the intersecting groove was evident. Pain was evident in response to percussion, but responses were normal for the adjacent and contralateral teeth. The visual analogue scale (VAS) score of the #15 tooth was 3.5. The readings of the pulp viability test of the #15 and #2 teeth were 21 and 20, respectively. A pulp electric viability test yielded normal responses, which were identical to those of the control teeth. The periodontal probing depth of the #15 tooth was < 3.0 mm. No mobility or swelling was evident. The Oral Hygiene Index-Simplified (OHI-S) and Decayed Missing Filled-Index (DMF-Index) scores are shown in Tables 1 and 2.
| Oral hygiene index-simplified | Labial (Buccal) surface | Lingual surface | Total score | ||||
| #3 | #8 | #14 | #24 | #19 | #30 | ||
| Debris index-simplified | 1 | 0 | 1 | 0 | 1 | 0 | 5 |
| Calculus index-simplified | 0 | 0 | 1 | 0 | 1 | 0 | |
| Decayed missing filled-index | ||
| D (Decayed) | 1 | #18 occlusal caries |
| M (Missing) | 4 | #1, #16, #17, #32 missing |
| Filled (Filled) | 0 | 0 |
This case did not have any laboratory examinations.
Digital periapical radiography was performed preoperatively, and the results did not provide sufficient information (Figure 1C). Tooth fusion was suspected; therefore, CBCT was considered to be appropriate. After obtaining informed consent from the patient, CBCT imaging was performed to assess the root canal systems of the fused left maxillary second molar and supernumerary teeth via 3D technology (New Tom VG10048S; Quantitative Radiologys.r.l, Verona, Italy). The axial, sagittal, and coronal sections confirmed that the maxillary left second molar and two paramolars were fused, and no such abnormalities were evident on the other side (Figure 1D). Three slightly curved and patent root canals were present in the maxillary second molar, and each of the fused paramolers contained a single similar canal. The apex area of the irregular bending isthmus was observed in the periapical transmission image (Figure 1E-H).
Based on the subjective, objective, and radiographic findings, this tooth was diagnosed as a fused tooth with periodontal apical periodontitis.
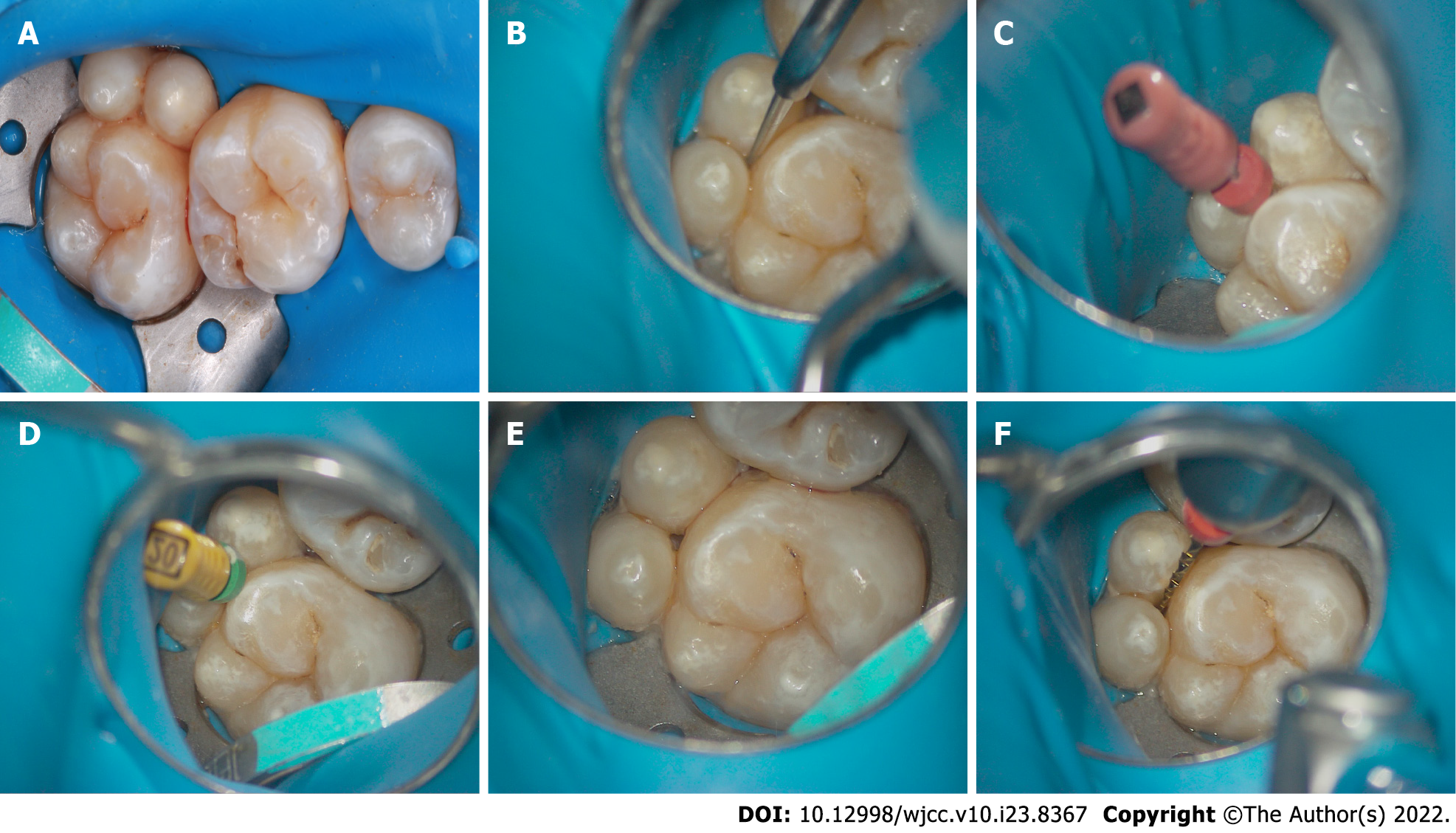
The patient provided informed consent to undergo a planned endodontic treatment of the isthmus that was formed at the fusion joint. A rubber dam was properly positioned (Figure 2A), and a ball drill (ET BD) and ET 20 ultrasonic equipment (P5 Newtron; ACTEON Satelec, Merignac, France) were used to remove the decay under a microscope (Figure 2B). The working lengths were determined with an electronic apex locator (EAL) and a #6K file (Figure 2C), and filing was performed until reaching a #20 size (Figure 2D and E). Next, the isthmus was cleaned and shaped via a crown-down approach using Waveone Gold Ni-Ti rotary instruments (Dentsply Sirona, Switzerland) with considerable 3% NaOCl and 17% EDTA irrigation (Figure 2F). Strong electrolytic water and ultrasonication (P5 Newtron) were used for a final irrigation, and the canals were dried with paper points. Then a calcium hydroxide [Ca(OH)2] paste was applied to the canals, and the access cavity was sealed using Cavit™av.
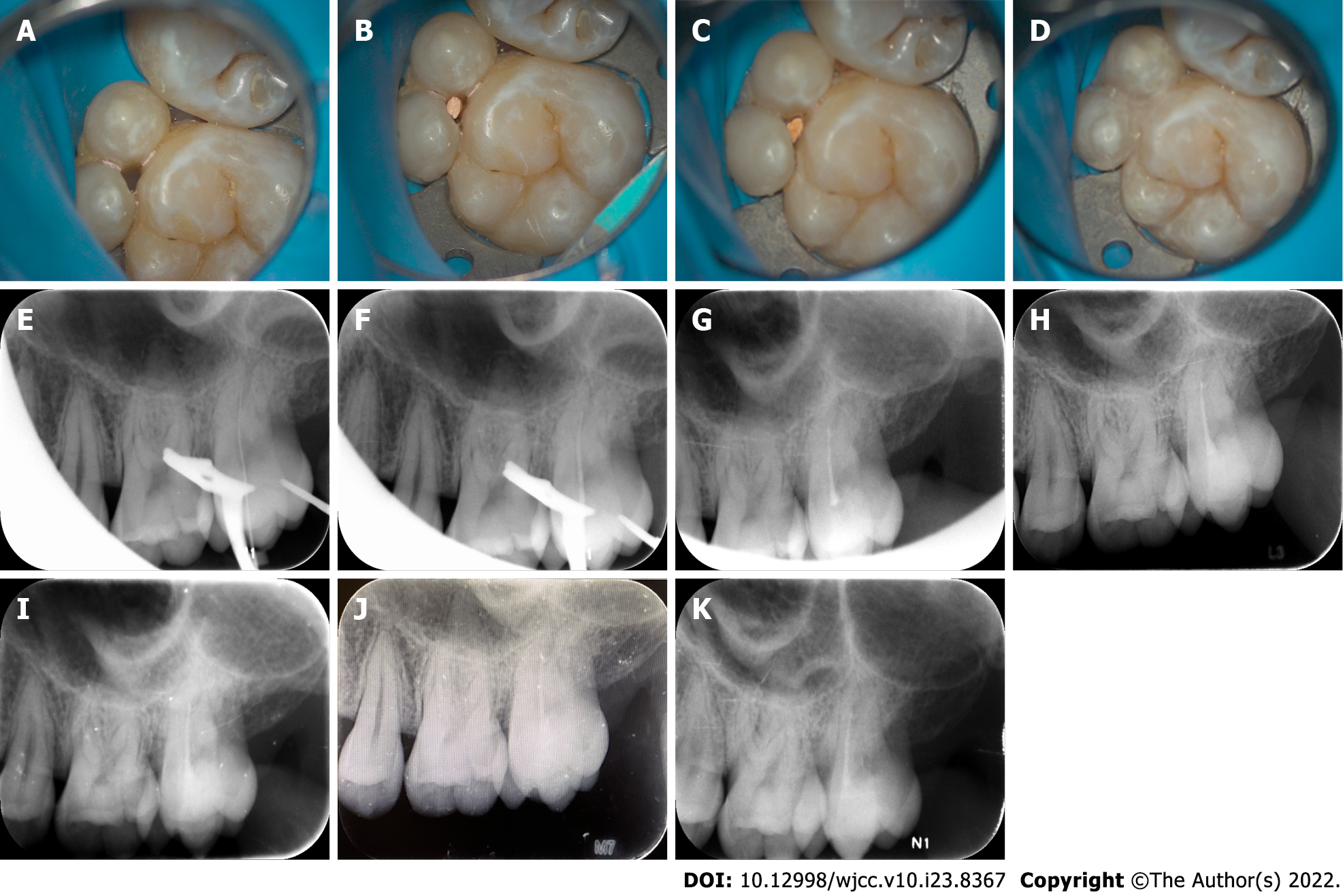
At 10 d post-operation, the patient experienced no pain upon percussion or cold stimulation. The VAS score of the #15 tooth was 0. Complete canal obturation was achieved through the single cone technique (Figure 3A-C) with IROOT SP (Innovative BioCreamix Inc, Vancouver, BC, Canada), and the access cavity was then sealed with flow and nanoresin (3M Dental Products, MN, United States) (Figure 3D). A final digital PAX was taken at this time, in which well-obturated canals were observed (Figure 3G).
The patient reported no symptoms throughout the 6 month, 12 month, 18 month, and 24 month follow-up periods. The VAS score of the #15 tooth was 0. Additionally, the treatment success was confirmed via X-ray examinations (Figure 3H-K).
Tooth fusion is thought to affect 0.5%-2.5% of the primary dentition and affects permanent teeth with an even lower frequency[4]. Fusion can result in significant changes in dental and periodontal anatomy, and these changes contribute to plaque retention, a higher risk of caries formation, and associated periodontal problems. Intraorally, fused teeth may present a range of phenotypes and can occur in any region, although they most commonly involve the anterior teeth and are unilateral in nature[10]. Additionally, fusion can occur between two teeth, between normal and supernumerary teeth, or between a tooth and an unerupted crown[11]. In a rare process known as concrescence, two fully formed adjacent teeth fuse only in the cementum. This process is most often observed with maxillary molars. More specifically, concrescence most often involves the maxillary third molar and a supernumerary tooth. Supernumerary molars are denoted as either paramolars or distomolars based on their location; paramolar are supernumerary teeth on the mesiobuccal side of molars and distomolars are supernumerary teeth on the distal side of the third molar[12]. The aetiological basis for such fusion is not well understood, and the fusion is thought to be associated with dental arch crowding, caries-related chronic irritation, trauma, and/or rapid orthodontic movement, which result in the resorption of interdental alveolar bone between fully formed teeth. Subsequently, fusion can occur due to cementum deposition[5,13]. In the present case report, two paramolars were fused on the mesiobuccal side of the upper left second molar, and fusion of the enamel at the crown was observed; in addition, cementum was fused at the roots of these teeth, and dentin was likely involved.
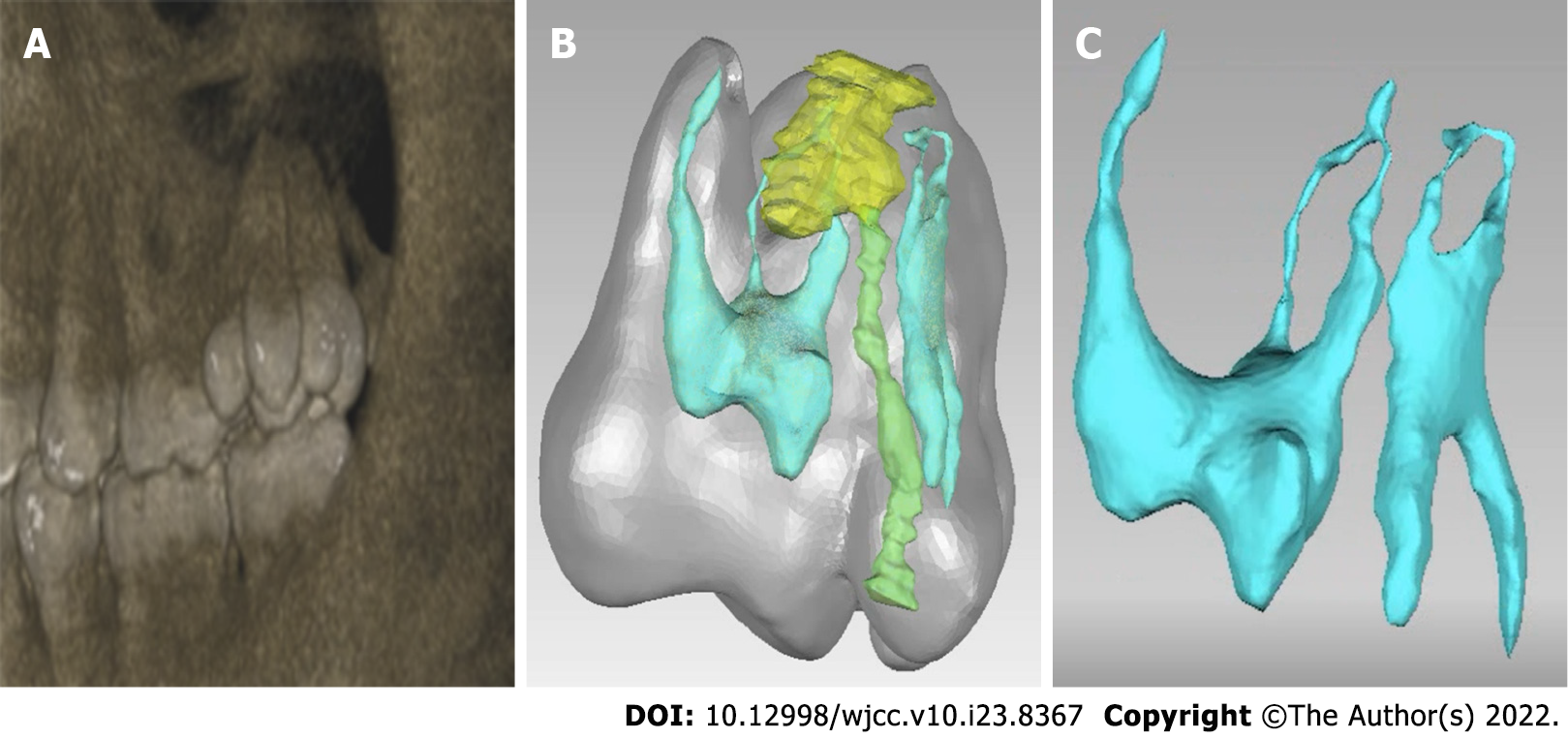
Successful treatment is dependent upon accurately evaluating the sources of any pain and accurately establishing the pulp status. In the present case, the patient exhibited percussion pain and temperature sensitivity. The pulp vitality tests yielded normal results, and no caries were observed. Conventionally, intraoral periapical radiographic imaging cannot reveal any obvious abnormality and only yields two-dimensional superimposed images that have the potential to magnify 3D structures or provide inaccurate angulation information[14]. Therefore, it can be challenging to obtain an accurate diagnosis. Here, we used CBCT images to construct a digital model of the local anatomy (Figure 4), and this model provided more intuitive information than that of previous models. Specifically, the low-density transmission image was extended along the isthmus pathway to the apical area, but the apex was not involved, and the roots of the two supernumerary teeth were fused with the mesial buccal roots of the second molar. The images also showed that the root canal systems of the two supernumerary teeth intersected in the middle 1/3 of the root and the apical area while an independent root canal system was retained in the second molar. Considering these findings, we suspected that the infection arose from the central isthmus of the fused tooth. Thus, we were able to speculate that the patient's primary complaint was associated with partial bone loss in the apical area, and this bone loss was caused by periapical periodontitis and gingival recession as a result of long-term food impaction. Exposure of the dentin in the dental cervix led to temperature sensitivity. Therefore, we provided the patient with two treatment options, either complete resection of the paramolars or retention of the paramolars, while only endodontic treatment was provided for the isthmus pathway. Although the paramolars and the second molar have independent root canal systems, performing a complete resection of the paramolars from the second molar necessitates a traumatic periodontal flap. Additionally, after the paramolars undergo a hemisection, the procedure may cause buccal dentin and cementum to become exposed, which may aggravate temperature sensitivity and even cause pulpitis. Because the fused tooth was in the area of the posterior teeth, the patient did not need to consider aesthetics. In addition, the patient has a good awareness of oral hygiene. Therefore, after negotiating the treatment plan with the patient, the patient preferred the conservative treatment to resolve the existing symptoms.
In such cases, the large buccal-lingual dimensions and the complexities of this isthmus pathway can further complicate the treatment process. First, it can be challenging to place the rubber dam clamp during endodontic procedures and achieve effective isolation. Therefore, we utilized a bow method to position the rubber dam so that the clip could be placed under a direct view. Additionally, cleaning and shaping the isthmus pathway was difficult. Compared to the inner wall of conventional root canals, the walls of the path around the enamel and cementum were harder because the isthmus exhibited an irregularly curved path. We used ultrasonic instruments to remove carious tissues and part of the coronal tooth structure to enhance straight-line access. In general, the canal curvature can better be followed with smaller files owing to their flexibility; therefore, smaller files should be utilized to gently negotiate the canal prior to utilizing larger files. Next, we used reciprocating Ni-Ti files to clean and shape the canals. These procedures seemed to enhance path negotiation, allowing for faster and more efficient instrumentation. However, owing to the irregular shape of this pathway, we were unable to determine whether the pathway walls were composed of dentin or cementum following treatment. Even so, effectively isolating the tooth and performing cleaning, irrigation, disinfection, and sealing during endodontic treatment can effectively eliminate inflammation and reinfection, thereby alleviating patient discomfort and achieving a successful outcome[4,15,16].
The 6 month, 12 month, 18 month, and 24 month follow-ups showed that the treatment was effective. The limitation of this treatment was that it did not restore the normal shape of the maxillary second molar. However, the fused tooth was in the posterior teeth area, and the patient had low aesthetic requirements. Therefore, the patient preferred a conservative treatment to preserve vital pulpal tissue. Additionally, the tooth was located at the distal end of the dental arch close to the buccal aspect, which is not conducive to daily cleaning. Consequently, we emphasized the importance of correct oral hygiene maintenance and long-term follow-up to the patient; thus, we anticipate a good prognosis.
In summary, we described a rare case that involved the fusion of the maxillary second molar and two paramolars. It is often challenging to clinically detect fused teeth. The underlying abnormal tooth structures may limit the ability of obtaining an appropriate diagnosis with traditional radiographic imaging, which yield insufficient information for diagnoses and treatments. We herein utilized CBCT data to generate a digital model of the affected region in this patient, and this model enabled us to better plan the management of his case. In addition, with the resultant models, we could better view the underlying complex morphology. The models provided 3D morphological insights and supported the accurate detection of pulp electrical vitality to ensure that the endodontic diagnosis was successful.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elshazly NEAB, Egypt; Rakhshan V, Iran; Suzuki EY, Thailand S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Tortora C, Meazzini MC, Garattini G, Brusati R. Prevalence of abnormalities in dental structure, position, and eruption pattern in a population of unilateral and bilateral cleft lip and palate patients. Cleft Palate Craniofac J. 2008;45:154-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Chen F, Wang S, Bai N, Li X, Wang L, Xia X, Liu J, Tan F. Management of Fused Anterior Teeth: Review and Clinical Report. J Prosthodont. 2022;31:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Garattini G, Crozzoli P, Brenna F. Bilateral dental fusion of the upper central incisors: a multidisciplinary approach. J Esthet Dent. 1999;11:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Açıkel H, İbiş S, Şen Tunç E. Primary Fused Teeth and Findings in Permanent Dentition. Med Princ Pract. 2018;27:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Sato M, Garcia-Sanchez A, Sanchez S, Chen IP. Use of 3-dimensional-Printed Guide in Hemisection and Autotransplantation of a Fusion Tooth: A Case Report. J Endod. 2021;47:526-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Rani A K, Metgud S, Yakub SS, Pai U, Toshniwal NG, Bawaskar N. Endodontic and esthetic management of maxillary lateral incisor fused to a supernumerary tooth associated with a talon cusp by using spiral computed tomography as a diagnostic aid: a case report. J Endod. 2010;36:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Aydın H. Relationship between crown and root canal anatomy of four-rooted maxillary molar teeth. Aust Endod J. 2021;47:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Katheria BC, Kau CH, Tate R, Chen JW, English J, Bouquot J. Effectiveness of impacted and supernumerary tooth diagnosis from traditional radiography versus cone beam computed tomography. Pediatr Dent. 2010;32:304-309. [PubMed] |
| 9. | Shim YS, Kim AH, Choi JE, An SY. Use of three-dimensional computed tomography images in dental care of children and adolescents in Korea. Technol Health Care. 2014;22:333-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Nunes E, de Moraes IG, de Novaes PM, de Sousa SM. Bilateral fusion of mandibular second molars with supernumerary teeth: case report. Braz Dent J. 2002;13:137-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Sugiyama M, Ogawa I, Suei Y, Tohmori H, Higashikawa K, Kamata N. Concrescence of teeth: cemental union between the crown of an impacted tooth and the roots of an erupted tooth. J Oral Pathol Med. 2007;36:60-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Nangia D, Dinkar S, Nawal RR, Talwar S. Endodontic management of mandibular second molar fused to odontome with 12-month follow-up using cone beam computed tomography: A case report. Aust Endod J. 2021;47:350-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | El Backly RM, Kotry GS, Moussa H. Multidisciplinary management of a fused maxillary incisor: Case report with 5-year follow-up. Clin Case Rep. 2021;9:775-786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Silva MA, Wolf U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone-beam computed tomography for routine orthodontic treatment planning: a radiation dose evaluation. Am J Orthod Dentofacial Orthop. 2008;133:640.e1-640.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 209] [Article Influence: 12.3] [Reference Citation Analysis (1)] |
| 15. | Ray S. Esthetic management of fused incisors with ceramic veneers. J Prosthet Dent. 2019;121:217-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Ben Salem M, Chouchene F, Masmoudi F, Baaziz A, Maatouk F, Ghedira H. Fusion or Gemination? Case Rep Dent. 2021;2021:6661776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |