Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7147
Peer-review started: January 11, 2022
First decision: March 15, 2022
Revised: March 27, 2022
Accepted: May 28, 2022
Article in press: May 28, 2022
Published online: July 16, 2022
Processing time: 174 Days and 10.4 Hours
Primary cutaneous amyloidosis (PCA) is a chronic metabolic skin disease that has a detrimental impact on physical and mental health. It appears as mossy papules and severe itching, which is long-term and recurrent. Traditional treatments are unsatisfactory, especially for refractory cases. Fire needle therapy, which is widely used in China, has shown good clinical efficacy, as well as advantages concerning safety and cost. Clinical reports about fire needle treatment of this disease are few at present.
We report two older men who had developed maculopapules with itchiness on the trunk and arms for more than 10-15 years. Due to the dermatopathological findings, PCA was our primary consideration. They received topical halometa
Topical halometasone cream and pretreatment with fire needle could be a fast, safe, and economic treatment for PCA.
Core Tip: We explored a combination therapy for primary cutaneous amyloidosis, which is fast and noninvasive with low recurrence. The effects of topical drugs could be more pronounced after fire needle intervention. Topical halometasone cream plus fire needle pre-treatment could shorten the course of treatment and reduce recurrence.
- Citation: Su YQ, Liu ZY, Wei G, Zhang CM. Topical halometasone cream combined with fire needle pre-treatment for treatment of primary cutaneous amyloidosis: Two case reports. World J Clin Cases 2022; 10(20): 7147-7152
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7147.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7147
Primary cutaneous amyloidosis (PCA) is a chronic metabolic skin disease that results from deposition of amyloid in the dermal papillary layer with no involvement of other organs, which has a detrimental impact on physical and mental health. Currently, topical corticosteroids are one of the effective methods for treatment of PCA. However, long-term use of corticosteroids can cause adverse reactions such as angiotelectasis of the skin. Fire needle is a form of acupuncture therapy. The acupuncture needle pierces the lesion quickly after being burned red on an alcohol lamp. It has been reported that fire needle can be used for treatment of itchy, painful, inflammatory, and pigmented diseases[1-5], and has achieved a good therapeutic effect as an adjuvant therapy. Here, we report two cases of PCA that received fire needle pre-treatment and topical halometasone cream (Bright Future Pharmaceuticals Factory, Hong Kong), who achieved significant improvement.
Case 1: Brown papules with itchiness on the back and limbs for > 10 years.
Case 2: Mossy maculopapules with itchiness on the back and both upper arms for > 15 years.
Case 1: At first, the skin on the patient’s back and limbs developed itching. Numerous brown papules formed after repeated scratching. During this period, although corticosteroid cream and moisturizers were used topically many times, the effect was poor and the lesions increased gradually.
Case 2: The patient had used varieties of topical hormones and the cupping, but the effects were not obvious.
Case 1: The patient had been exposed to sunlight for a long time.
Case 2: The patient reported no notable past illness.
Cases 1 and 2: No notable personal or family medical history.
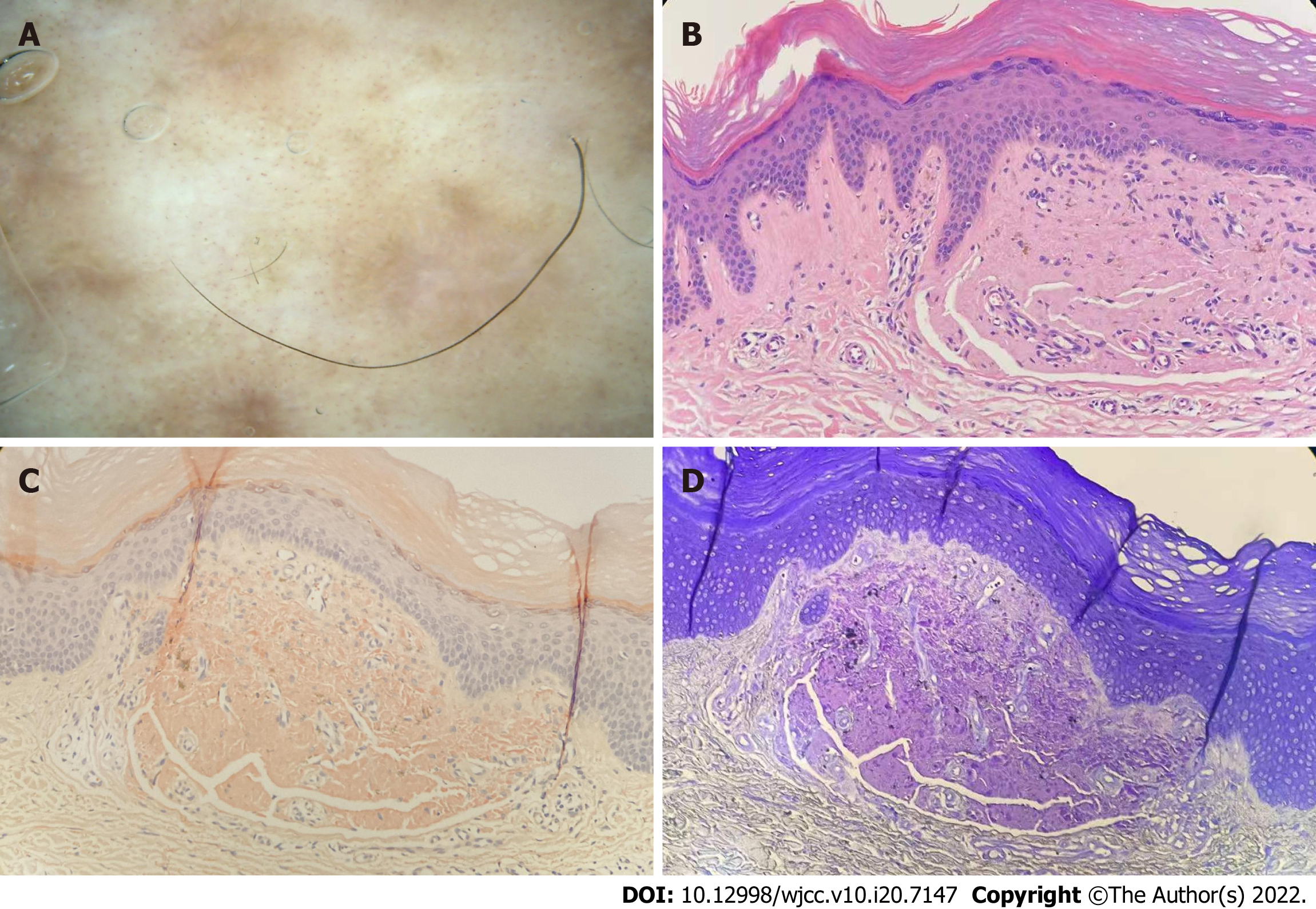
Case 1: The back and shanks were symmetrically distributed with dense, hard, and rough brown papules. There was almost no normal skin between the papules. Lesions were more pronounced on the shanks. Due to excessive scratching, a small number of gray scales and blood scabs were attached to some of the papules (Figure 1A).
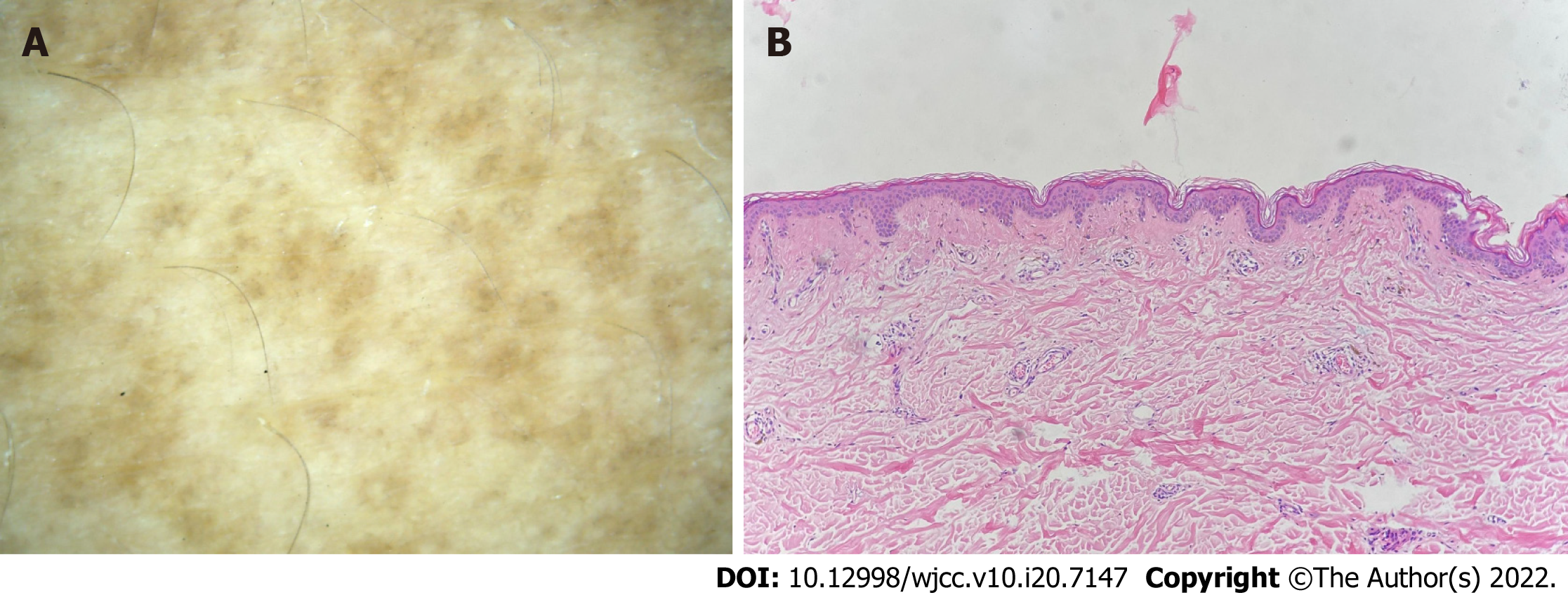
Case 2: Polygonal mossy maculopapules were widely distributed in the dorsal scapular region and on both upper arms, with well-defined boundaries and numerous scratches. Lesions were more pronounced in the middle than in the surrounding area. The skin of the dorsal interscapular area was normal (Figure 2A).
Case 1: The epidermis was hyperkeratinized. There were homogeneous red-stained amorphous substances in the superficial dermis and pigment incontinence in the stratum basale. Lymphocytes were scattered around the blood vessels (Figure 3A). Amyloid deposited within the dermal papillary layer was stained orange by Congo red (Figure 3B) and purple by crystal violet (Figure 3C).
Case 2: In the dermal papillary layer, there was a reddish mass of amorphous matter and pigment incontinence in the superficial dermis, as well as a small amount of lymphocyte infiltration around the blood vessels (Figure 4A).
Case 1: On dermatoscopy, the lesions were evenly distributed, and the central area was light white or light red without structure. The pigment was radially distributed around them, and the dotted blood vessels were densely distributed around most of the lesions (Figure 3D).
Case 2: On dermatoscopy, the central hub had white or brown structure surrounded by irregular pigmentation (Figure 4B).
In both cases, based on the findings, the final diagnosis was PCA.
Initially, a fire needle was used to scatter the lesions locally. The acupuncture needle was burned red on the alcohol lamp and pierced the targeted lesions. The spacing was 5-10 mm and the depth of penetration was approximately 5 mm. This treatment was performed every 2 wk for four times. Topical halometasone cream was applied to the surface of the lesions and the lesions were covered with clean plastic wrap for 20-30 min. This was performed twice daily for 4 wk.
The treatment method was the same as that for case 1, except that halometasone cream was applied for 4 wk.
After 1 wk of the treatments, itching was significantly reduced. After 4 wk, the lesions were thinner and the surface was smoother (Figure 1B). After 8 wk, the lesions gradually disappeared, and left some pigmentation (Figure 1C). Itching was completely relieved. After telephone follow-up at 2 years, there was no recurrence.
After 4 wk of the treatments, the original lesions became flat with light brown pigmentation, and the itching sensation disappeared (Figure 2B). At the 3-year telephone follow-up visit, the lesions had not subsided completely, but the itching had not recurred.
We report two older male patients with a long-term and stubborn history of scratching. The average course of disease was 12.5 years. Patient 1 had a history of UV exposure, which is consistent with the description of the disease. Both patients took multiple hormones topically, and patient 2 also had cupping therapy. Their effects were not obvious.
PCA is a chronic metabolic disease mainly involving the skin, with a predilection for the shins, calves, ankles, and dorsa of the feet and thighs[1]. Typical lesions are mossy papules forming brown patches, accompanied by stubborn itching and obvious pigmentation. The characteristic pathological feature is amyloid deposition in the dermal papillary layer. Common dermatoscopic findings are the presence of a white or brown structure, or scarring in the central area, with a variety of pigmented structures and bright white streaks[2]. PCA is related to scratching, UV exposure, genetic susceptibility, race, and environment. There is no difference between men and women. It has been reported that all eight patients with PCA in a Pakistani family were female[3]. It has also been reported that the disease mostly occurs in housewives, but the gender difference is not significant[4].
The common treatment methods for PCA mainly include topical and systemic drugs such as retinoids, phototherapy, laser therapy, and surgical interventions, but the results are often not satisfactory[1]. Fire needle has the advantages of both conventional acupuncture and moxibustion, due to needle and thermal stimulation. It can promote microcirculation, accelerate metabolism, and restore damaged tissues in the lesional area through the regulation of cutaneous nerves, which in turn can eliminate or attenuate pathological features such as edema, hyperemia, exudation, adhesion, calcification, contractures, and ischemia[5]. Fire needle also can stimulate vascular dilatation and local edema of the lesion, which promotes transdermal absorption and maximizes the efficacy of the topical agents[6].
The adverse effects of fire needle, such as mild burning, stinging, and itching, and slight redness and swelling of the skin, are temporary and not regarded as severe, because these effects disappear within 30-60 min[7]. Therefore, fire needle is a viable treatment option for PCA, and packet therapy can increase drug hydration, promoting the transdermal absorption of halometasone cream and maximizing its efficacy. Therefore, it is believed that the effect of halometasone cream is more significant after fire needle and packet therapy.
We report two patients with PCA treated with topical halometasone cream and pretreatment with fire needle. The lesions in patient 1 improved significantly after 8 wk, and the lesions in patient 2 were basically flattened after 4 wk. Neither patient had recurrence after 2-3 years of follow-up. This method reduced severe itching significantly and removed lesions more effectively. It is believed that this combination therapy could be an effective, safe, and economic alternative therapy for PCA. The number of reported cases of this method is small, and there was no blank control, so further exploration is needed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sarici IS, Turkey; Zhang CH, China S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Chen Z, Zhou D, Wang Y, Lan H, Duan X, Li B, Zhao J, Li W, Liu Z, Di T, Guo X, Zhang J, Feng S, Li P. Fire needle acupuncture or moxibustion for chronic plaque psoriasis: study protocol for a randomized controlled trial. Trials. 2019;20:674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Luo Y, Kuai L, Song N, Ding X, Sun X, Luo Y, Ru Y, Hong S, Xing M, Zhou M, Li B, Li X. Efficacy and Safety of Fire Needle Therapy for Nodular Prurigo: A Quantitative Study. Evid Based Complement Alternat Med. 2019;2019:8797056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Wang JX, Zhao WX, Zeng JC, Liu K, Li QJ, She YL, Lin GH. [Systematic review and sequential analysis on treatment of herpes zoster pain mainly by fire needle therapy]. Zhen Ci Yan Jiu. 2019;44:677-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Xing M, Yan X, Sun X, Wang S, Zhou M, Zhu B, Kuai L, Liu L, Luo Y, Li X, Li B. Fire needle therapy for moderate-severe acne: A PRISMA systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2019;44:253-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Luo Y, Qian W, Dai T, Ru Y, Sun X, Kuai L, Liu L, Xing M, Zheng Q, Zhang Y, Chen X, Zhao H, Li B, Li X. A New Therapy for Vitiligo Using Fire Needles: A Systematic Review of Evidence from 3618 Subjects. Evid Based Complement Alternat Med. 2020;2020:8492097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Weidner T, Illing T, Elsner P. Primary Localized Cutaneous Amyloidosis: A Systematic Treatment Review. Am J Clin Dermatol. 2017;18:629-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 7. | Żychowska M, Pięta K, Rudy I, Skubisz A, Reich A. Dermoscopic Features of Lichen Amyloidosis in Caucasians-A Case Series and Literature Review. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |