Copyright
©The Author(s) 2017.
World J Radiol. Apr 28, 2017; 9(4): 155-177
Published online Apr 28, 2017. doi: 10.4329/wjr.v9.i4.155
Published online Apr 28, 2017. doi: 10.4329/wjr.v9.i4.155
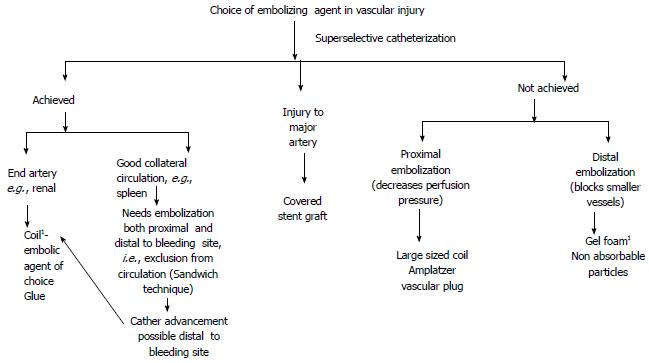
Figure 1 Choice of embolizing agent in vascular injury.
1Workhorse of IR in trauma. IR: Interventional radiology.
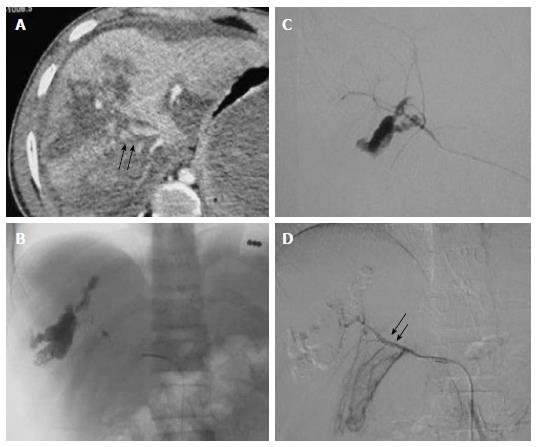
Figure 2 High grade liver injury with active contrast extravasation.
Case of blunt trauma abdomen, FAST positive, hemodynamically stable (A) CECT abdomen showed extensive laceration, intraparenchymal hematoma consistent with Grade V liver injury alongwith diffuse active contrast extravasation (arrow) within the lacerated segment VIII (arrow) of liver with resultant hemoperitoneum (B) Selective hepatic artery angiogram revealed active contrast extravasation from anterior division of right hepatic artery with increased conspicuity in (C) superselective right hepatic artery angiogram which was subsequently embolized by microcoils (D) Post embolization angiogram revealed faint opacification of branches of anterior division of RHA (arrow) with subsidence of extravasation. FAST: Focused assessment with sonography in trauma; RHA: Right hepatic artery; CECT: Contrast enhanced computed tomography.
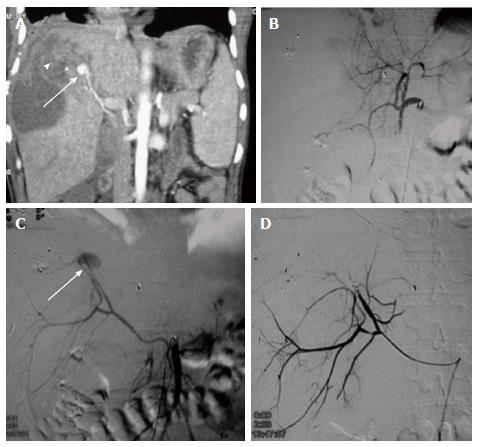
Figure 3 Gun shot injury with hepatic artery pseudoaneurysm.
A 38-year male with gunshot injury presented after a week with falling hematocrit. A: CECT showed a contrast filled outpouching in segment VIII of liver paralleling the attenuation of adjacent hepatic artery branch s/o PsA (arrow) with adjacent subscapular hematoma (arrowhead) subsequently DSA was done; B: Initial hepatic angiogram showed opacification of only branches of left lobe of liver,no opacification of right hepatic artery -s/o variant anatomy; C: SMA angiogram showed replaced right hepatic artery with PsA arising from the terminal end of anterior division (arrow). Due to smaller caliber and spasm, neck of the PsA could not be negotiated, hence, proximal embolization with microcoils was performed; D: Post embolization angiogram showed faint opacification of branches of anterior division of RHA alongwith exclusion of PsA. CECT: Contrast enhanced computed tomography; RHA: Right hepatic artery; PsA: Pseudoaneurysm; SMA: Superior mesentery artery; DSA: Digital subtraction angiography.
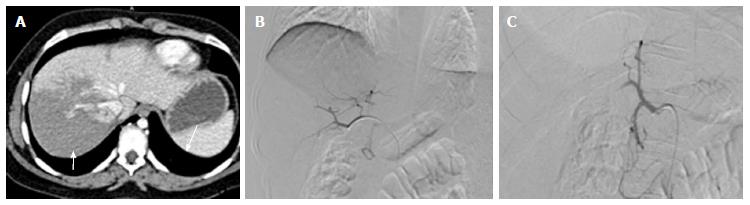
Figure 4 Prophylactic embolization of right hepatic artery in high grade liver injury.
A: CECT abdomen of a 35 years old male, c/o BTA showed extensive deep lacerations and intraparenchymal contusions in the right lobe of liver s/o Grade IV injury. Majority of these lacerations were reaching upto the hepatic surface (arrow) with possible capsular breach. Mild hemoperitoneum was present in pelvis; no active contrast extravasation or pseudoaneurysm; B: In view of high grade injury involving right lobe, prophylactic gelfoam embolization of right hepatic artery was done; C: Post embolization,there was non-opacification of RHA. CECT: Contrast enhanced computed tomography; BTA: Blunt trauma abdomen; RHA: Right hepatic artery.
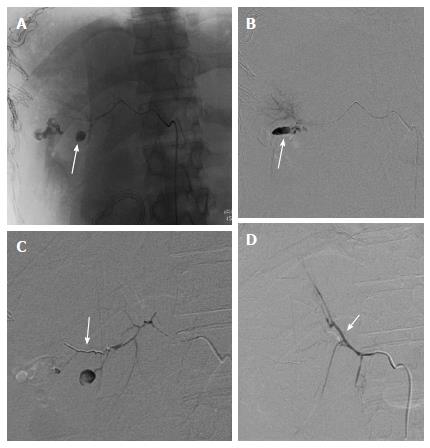
Figure 5 Re-bleed after perihepatic packing.
A 38-year-old male with BTA, hemodynamically unstable and taken directly to OR for perihepatic packing. DSA was contemplated in view of persistent hypotension after perihepatic packing. A and B: Selective right hepatic angiogram showed PsA arising from its posterior division (arrow). Subsequently, guidewire followed by micro catheter manipulation was done across its neck; C: Microcoil was deployed across the neck of PsA from distal to proximal followed by gelfoam embolization; D: Post embolization angiographic run showed faint opacification of posterior branch due to sluggish flow. Note brilliant opacification of anterior branch of RHA (arrow) due to reflux of contrast. OR: Operating room; RHA: Right hepatic artery; BTA: Blunt trauma abdomen; DSA: Digital subtraction angiography.
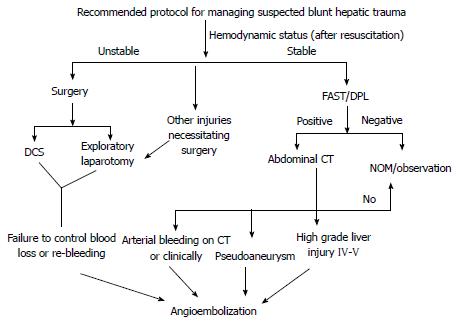
Figure 6 Recommended protocol for managing suspected blunt hepatic trauma.
CT: Computed tomography; DCS: Damage control surgery; FAST: Focused assessment with sonography in trauma; DPL: Diagnostic peritoneal lavage.
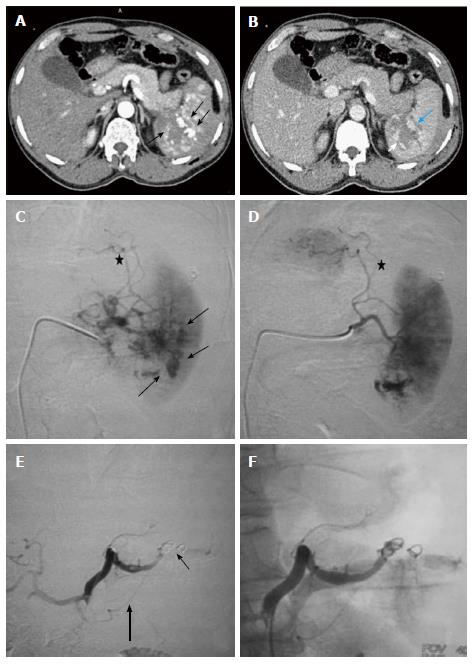
Figure 7 Grade IV splenic injury with active contrast extravasation in a 29-year-old male with blunt trauma abdomen, hemodynamically stable and FAST positive.
Arterial phase image (A) showing blobs of contrast (arrow) marginating the deep splenic laceration. In portovenous phase (B), lacerations are better appreciated, few of which are involving splenic hilum. Also, blobs of contrast in the arterial images has slight increased in size (arrow), nonetheless, remain localised s/o focal active contrast extravasation. DSA was done (C and D), selective splenic artery angiogram showed multiple areas of active contrast extravasation from trabecular arteries of lower pole (arrow) with disruption of parenchymal continuity due to laceration (asterisk). Proximal embolization of splenic artery was done with coil followed by gelfoam instillation (E). Note coils (thin arrow) are deployed distal to the origin of dorsal pancreatic artery (thick arrow). Post embolization angiographic run (F) showed proximal contrast stasis with no opacification distal to embolization site. DSA: Digital subtraction angiography; FAST: Focused assessment with sonography in trauma.
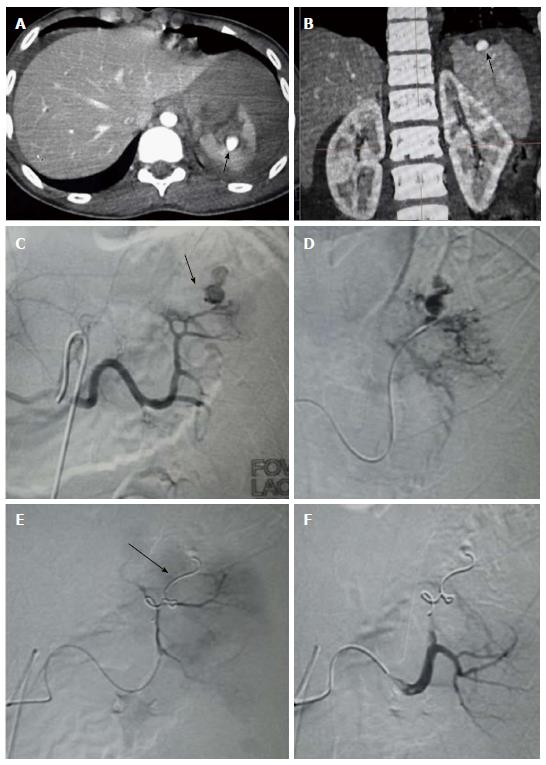
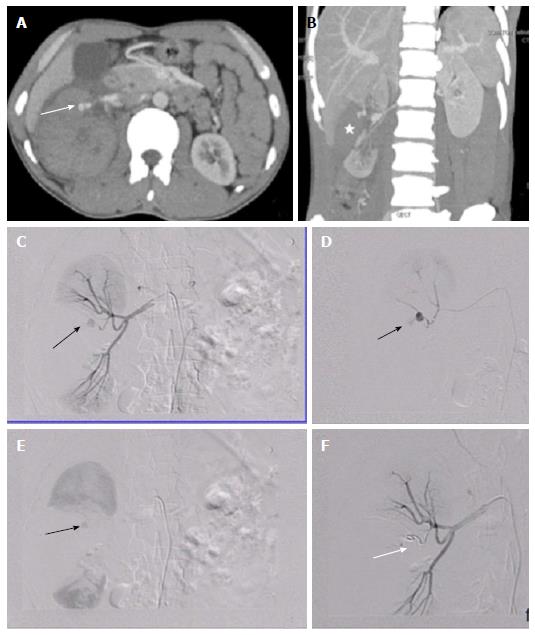
Figure 8 Splenic artery pseudoaneurysm.
Case of 39-year-old female with BTA, FAST positive, hemodynamically stable. CECT revealed (A and B) Extensive lacerations involving spleen with presence of contrast filled intrasplenic outpouching paralleling the aortic attenuation s/o pseudoaneurysm. Splenic artery angiogram showed (C) PsA (arrow) arising from the upper polar branch which on delayed phases showed contrast spillage s/o leaking PsA (D). Subsequently, upper pole branch was selectively catheterised by microcatheter followed by deployment of microcoils (arrow) across the neck of PsA (distal embolization) (E). Post embolization angiography (F) showed no flow distal to coil with exclusion of PsA and good contrast opacification of lower pole branch. CECT: Contrast enhanced computed tomography; BTA: Blunt trauma abdomen; PsA: Pseudoaneurysm; FAST: Focused assessment with sonography in trauma.
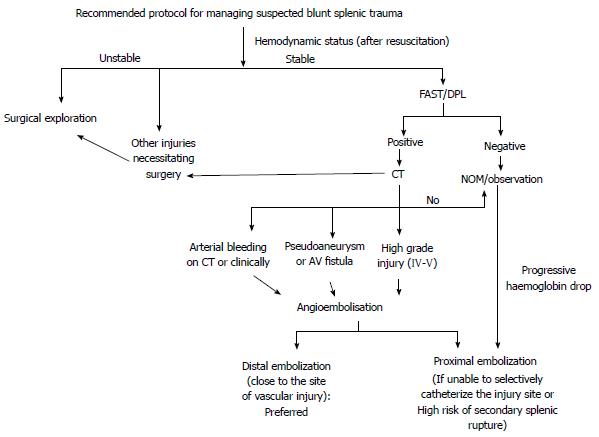
Figure 9 Recommended protocol for managing suspected blunt splenic trauma.
CT: Computed tomography; FAST: Focused assessment with sonography in trauma; DPL: Diagnostic peritoneal lavage; NOM: Non operative management.
Figure 10 Renovascular injury: 35 years old male with blunt trauma abdomen.
A, B: CECT abdomen showed deep lacerations involving the interpole of right kidney extending upto the renal hilum (asterisk). A pseudoaneurysm (arrow) was seen arising from upper polar branch alongwith presence of perinephric hematoma; C, D: DSA with catheterisation of right main renal artery confirmed the presence of pseudoaneurysm (arrow); E: In view of end arterial supply, involved branch was selectively accessed and catheter was subsequently manipulated across the neck of PsA with the help of microwire followed by deployment of coil; F: Post embolization angiography showed non opacification distal to the coil (arrow). CECT: Contrast enhanced computed tomography; PsA: Pseudoaneurysm; DSA: Digital subtraction angiography.
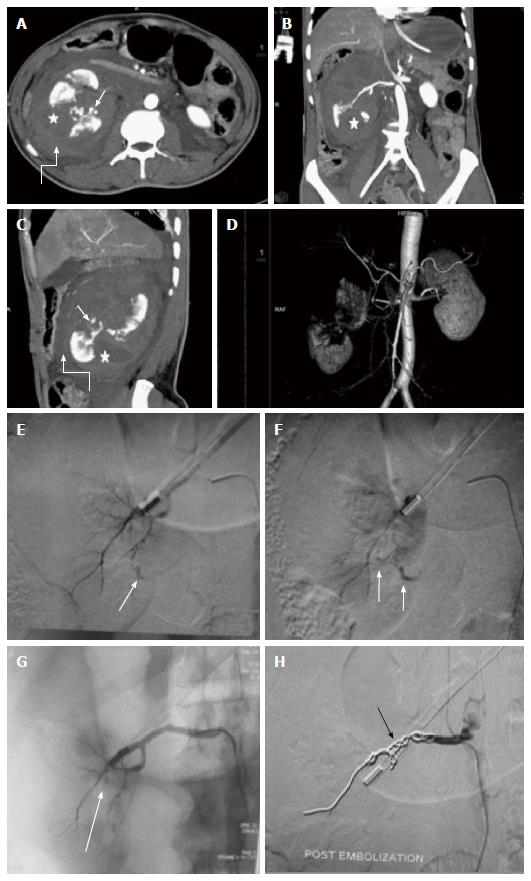
Figure 11 Main renal artery injury.
A-D: CECT in a 22 years old male following road traffic accident revealed multiple deep lacerations (asterisk) involving entire thickness of right kidney resulting in shattered kidney. Few areas of active contrast extravasation (thin arrow) were noted at the edge of laceration alongwith presence of extensive pernephric hematoma (curved arrow). Although, main renal artery was showing good luminal opacification, however, less than 25 % remaining functioning renal parenchyma precluded salvagability. Due to high post operative morbidity, angiography was resorted over nephrectomy; E, F: Selective catheterisation of main renal artery showed multiple areas of active contrast extravasation (arrow); G: Subsequently, in view of potentially life threatening haemorrhage and non-salvagable kidney, coil embolization (arrow) of main renal artery was contemplated; H: Post embolization angiography showed opacification of only proximal stump of renal artery. Following conservative management, patient was then discharged 8 d later. CECT: Contrast enhanced computed tomography.
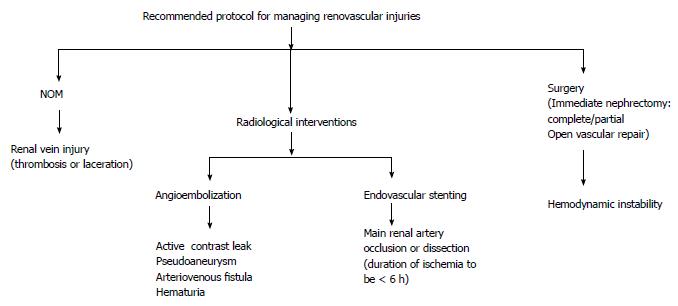
Figure 12 Recommended protocol for managing renovascular injuries.
NOM: Non operative management.
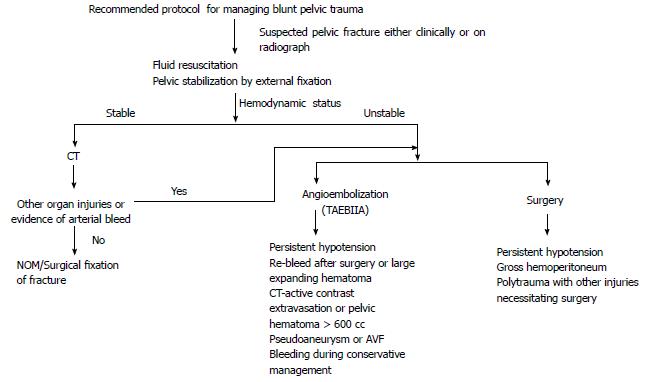
Figure 13 Recommended protocol for managing blunt pelvic trauma.
NOM: Non operative management; TAEBIIA: Transarterial embolization of bilateral iliac artery; CT: Computed tomography; AVF: Arterio-venous fistula.
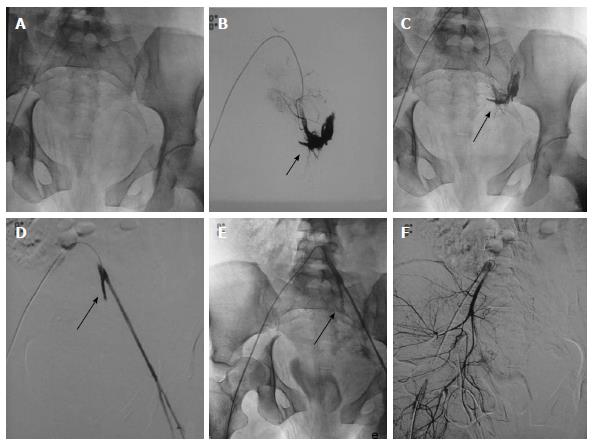
Figure 14 Pelvic fractures with injury of left internal iliac artery.
DSA of 24-year-old hemodynamically unstable patient with extensive pelvic fractures. A-C: Selective catheterization of left common iliac artery showed active contrast extravasation from left internal iliac artery subjacent to the disrupted left sacroiliac articulation which was subsequently embolized with coil; D, E: Angiography post embolization showed non-opacification of internal iliac artery distal to coil (arrow) with complete disappearance of contrast extravasation. Left external iliac artery showed good opacification; F: Subsequently, right common iliac artery was cannulated which revealed no vascular injury. DSA: Digital subtraction angiography.
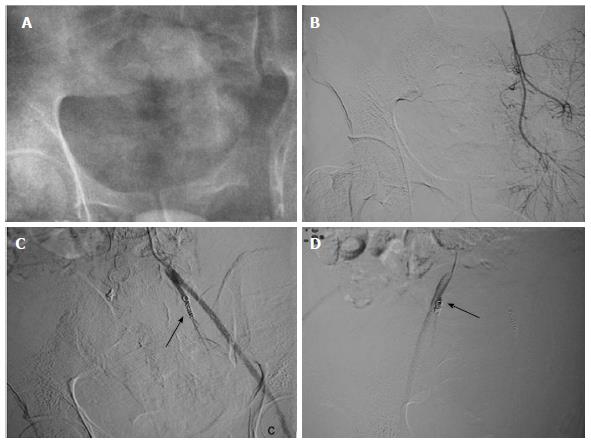
Figure 15 Transarterial embolization of bilateral internal iliac artery: Another case of severe pelvic injury with persistent hypotension.
A-D: Bilateral internal iliac arteries were selectively cannulated, however, no vascular injury present. Prophylactic coil embolization of bilateral internal iliac artery was done (arrow). Few hours later patient became normotensive.
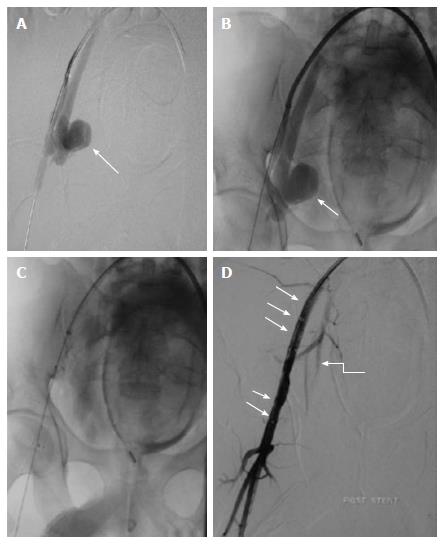
Figure 16 Stent grafting in pseudoaneurysm.
Case of gun shot injury, CECT showed presence of PsA from right internal iliac artery (not shown). A, B: Arterial access was obtained through the left common femoral artery and a long arterial sheath was placed. Angiogram showed a large pseudoaneurysm (arrow) arising from the proximal portion of anterior division of right internal iliac artery with no contrast opacification distally (except for a short stump); C, D: Subsequently, a covered stent graft (arrow) was placed in right external artery. Post procedural angiography showed preservation of flow across the right external iliac artery and branches of right internal iliac artery (curved arrow). CECT: Contrast enhanced computed tomography; PsA: Pseudoaneurysm.
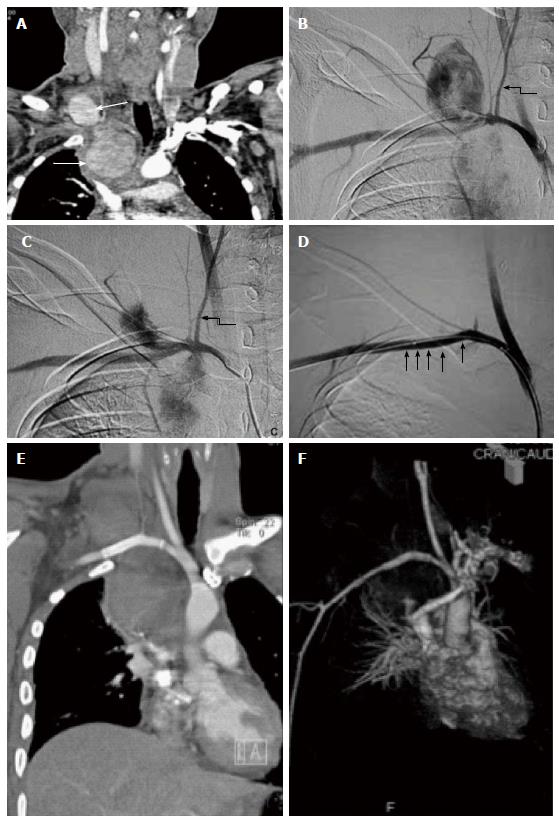
Figure 17 Peripheral vascular injury.
A 56-year-old male with multiple rib fractures and neck swelling following road traffic accident. A: CT angiography showed two distinct pseudoaneurysms arising from the proximal right subclavian artery, one cervical and other intrathoracic (arrow). However, there was good opacification of distal subclavian artery with no disruption in continuity, ruling out transection (curved arrow); B, C: DSA corroborated CT findings and revealed two large pseudoaneurysms arising from the proximal right subclavian artery, lateral to the origin of thyrocervical branch (arrow); D: Subsequently, guidewire was manipulated across the PsA and covered stent graft (arrow) was deployed, excluding the origin of right common carotid artery. Post stenting angiography showed no opacification of pseudoaneurysm with good flow in distal subclavian artery; E, F: Follow up CT angiography done 2 wk later revealed both the pseudoaneurysm to be thrombosed. The stent (arrow) was optimally placed stent (arrow) with preservation of distal flow across it. PsA: Pseudoaneurysm; DSA: Digital subtraction angiography.
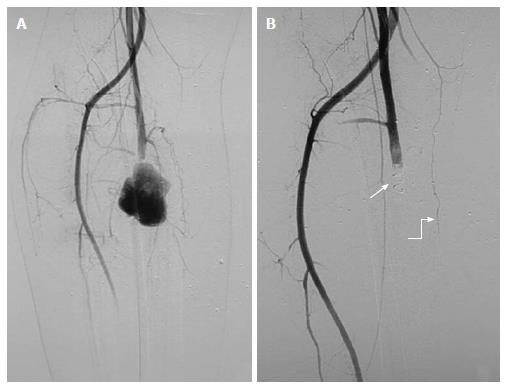
Figure 18 Pseudoaneurysm from right profunda femoris artery: 21-year-old male with stab injury.
A: DSA showed a large PsA arising from right profunda femoris artery with no distal flow, likely vascular transection with pseudoaneurysm of proximal end; B: As guidewire could not be negotiated across the pseudoaneurysm due to possible discontinuity, proximal coil embolization (arrow) was done. Post embolization angiography showed complete exclusion of pseudoaneurysm. Note the presence of collaterals (curved arrow) along the course of profunda femoris artery. PsA: Pseudoaneurysm; DSA: Digital subtraction angiography.
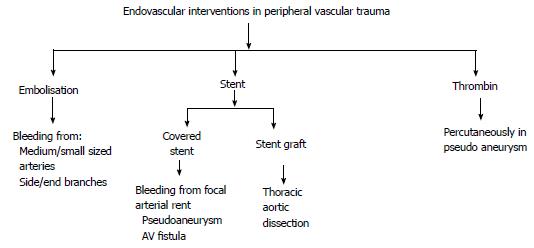
Figure 19 Endovascular interventions in peripheral vascular trauma.
AV: Arterio-venous.
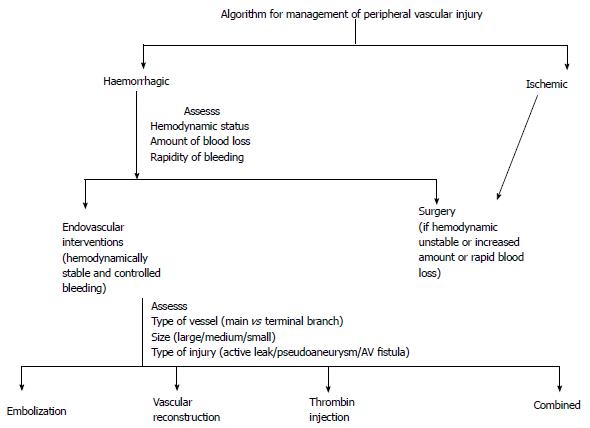
Figure 20 Algorithm for management of peripheral vascular injury.
- Citation: Singh A, Kumar A, Kumar P, Kumar S, Gamanagatti S. “Beyond saving lives”: Current perspectives of interventional radiology in trauma. World J Radiol 2017; 9(4): 155-177
- URL: https://www.wjgnet.com/1949-8470/full/v9/i4/155.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i4.155