Published online Dec 7, 2015. doi: 10.3748/wjg.v21.i45.12981
Peer-review started: June 28, 2015
First decision: July 19, 2015
Revised: August 24, 2015
Accepted: September 30, 2015
Article in press: September 30, 2015
Published online: December 7, 2015
Processing time: 160 Days and 23.7 Hours
The coexistence of hepatocellular carcinoma (HCC) and non-Hodgkin’s lymphoma (NHL) in the liver is rare. Reports show that these patients have cirrhotic livers or hepatitis virus infections before they develop HCC and NHL. We present a patient with hepatitis B virus infection who was transferred to our hospital with a newly detected liver mass; abdominal computed tomography examination showed one hypodense mass of 7 cm in diameter and multiple mesenteric and mediastinal lymph nodes. A liver tumor biopsy showed a hepatoma, and the pathologic findings from an inguinal lymph node excision showed mantle cell lymphoma. An immunohistochemical stain confirmed that the atypical lymphoid cells within the HCC were positive for the CD20, CD5 and cyclin D1 antigens. Taking these findings into account, the hepatic tumor was determined to be a HCC infiltrated by mantle cell lymphoma.
Core tip: The coexistence of hepatocellular carcinoma (HCC) and non-Hodgkin’s lymphoma in the liver is rare. The risk factors include hepatitis virus infection, liver cirrhosis and antineoplastic therapy. This case report presents a rare case of HCC and mantle cell lymphoma in the liver. Only hepatitis B virus infection is identified. “Tumor to tumor metastasis” is noted in the pathologic findings. The literature is also reviewed.
- Citation: Lee MH, Lin YC, Cheng HT, Chuang WY, Huang HC, Kao HW. Coexistence of hepatoma with mantle cell lymphoma in a hepatitis B carrier. World J Gastroenterol 2015; 21(45): 12981-12986
- URL: https://www.wjgnet.com/1007-9327/full/v21/i45/12981.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i45.12981
Hepatocellular carcinoma (HCC) is the most common primary liver tumor, and it is mostly associated with hepatitis B and C virus infection[1]. Liver invasion of non-Hodgkin’s lymphoma (NHL) has been the focus of several clinical investigations. Only a few publications have reported coexistence of HCC and NHL. Major risk factors include liver cirrhosis, hepatitis virus infection and chemotherapy[2-4]. Hepatitis B virus (HBV) is hepatotropic, but there were evidences that peripheral blood mononuclear cells (PBMCs) can also serve as a reservoir of this virus[5]. Therefore, it can be a causative factor of both HCC and lymphoma[6,7]. We present here a rare case of coexistent HCC and lymphoma in a HBV infected patient without liver cirrhosis.
A 52-year-old male patient was referred to our hospital for a newly diagnosed liver tumor of the right lobe. The following symptoms were noted: easy fatigue, poor appetite and progressive weight loss of 10 kg in the past two months. He had no fever or night sweats. He had not received prior chemotherapy. A contrast-enhanced computed tomography (CT) before this referral showed one 7-cm sized hypodense mass located in Couinaud’s segment 7. He was tested positive for HBV infection. A physical examination revealed multiple enlarged lymph nodes in his neck and inguinal region. Anemia, jaundice, leg edema and hepatosplenomegaly were not observed.
On admission, his laboratory tests for alanine aminotransferase (ALT), total bilirubin, albumin, leukocytes, and prothrombin time were all within normal range; but his aspartate aminotransferase was 41 U/L (0-34 U/L), hemoglobin 18.4 g/d, and red blood cell mass 6.49 × 106. His platelets count decreased to 97 × 103/μL (150 × 103-450 × 103/μL), and alpha-fetoprotein (AFP) increased to 49465.6 ng/mL (< 15 ng/mL). Viral serologic tests were negative for anti-hepatitis C virus (HCV) antibody but positive for hepatitis B surface antigen and anti-hepatitis B core antigen. HBV DNA quantitative test showed a low viral load of 0.00305 × 106 IU/mL. Serum β2-microglobulin was elevated to 3370 ng/mL.
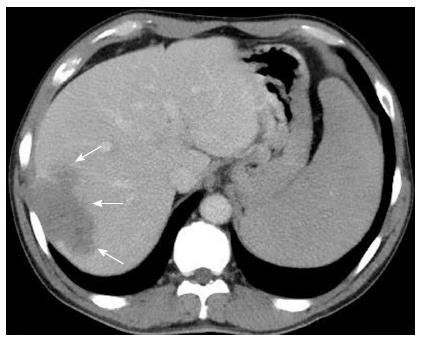
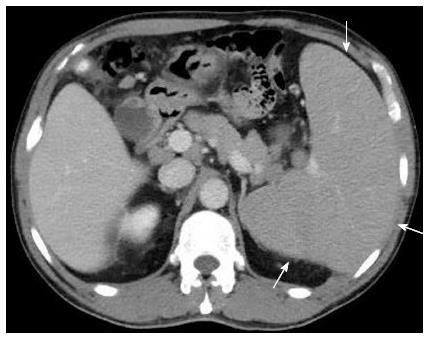
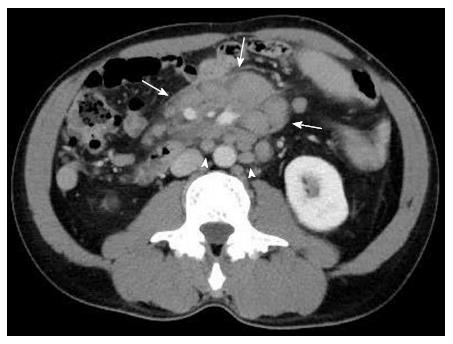
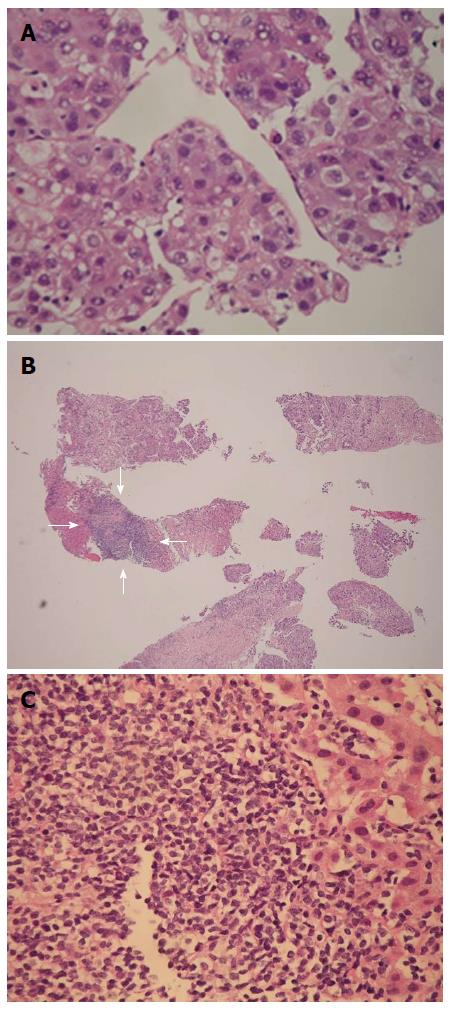
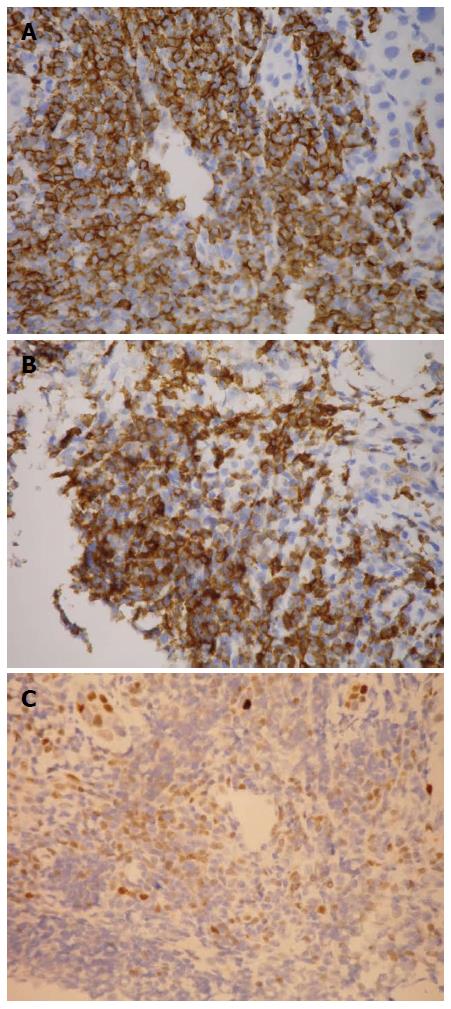
Review of CT by our radiologist revealed a 7-cm in diameter liver mass in S7 with heterogeneous enhancement in the arterial phase and wash out in the delay phase (Figures 1 and 2). It was considered a HCC with internal necrosis. There was no evidence of cirrhosis or portal vein thrombosis. Multiple mediastinal and mesenteric enlarged lymph nodes and splenomegaly were observed (Figures 3 and 4), which was not commonly seen in patients with HCC. An echo-guided core biopsy of the liver tumor was performed, and the initial pathologic finding indicated that it was an HCC (Figure 5A). Immunochemical study using an automated immunostainer BOND-MAX (Leica), however, revealed an aggregate of small to medium-sized lymphoid cells with irregular nuclei in the neighboring portal areas of normal liver tissue and also the tumor tissue (Figure 5B and C). These lymphoid cells were positive for CD20 (L26; Dako; 1:1000), CD5 (4C7; Lieca; 1:200) and cyclin D1 (SP4; Zytomed; 1:25) (Figure 6). This tumor was thus an HCC infiltrated with mantle cell lymphoma. A right inguinal lymph node was excised and the result showed mantle cell lymphoma. Given these findings, this patient was diagnosed as having a coexistent HCC and mantle cell lymphoma. Whole body contrast-enhanced CT before chemotherapy revealed no gastrointestinal tract involvement. Bone marrow biopsy revealed no evidence of lymphmatous involvement. Radiofrequency tumor ablation (RFA) was performed. Chemotherapy with CHOP regimen (cyclophosphamide, hydroxydaunorubicin, oncovin, prednisolone) was initiated. He has been in remission one year after therapy.
Mantle cell lymphoma (MCL) is a rare subgroup of B-cell NHL that occurs in approximately 6% of all NHL patients. MCL cells can enter the lymphatic channels and blood vessels, and they can also spread to other lymph nodes or tissues, such as the bone marrow, liver and gastrointestinal tract. The prognosis of MCL is poor. Although a positive relationship has been reported between HBV infection and NHL[7], only a few reported cases of coexistent MCL and HCC, especially in patients with chronic hepatitis B but no liver cirrhosis[8-10]. Most of the patients had HCV infection and liver cirrhosis[3,11,12].
The association between HBV and HCC is well established. Worldwide, HBV accounts for more than 50% of the HCC[13]. The risk of HCC increases with higher HBV DNA level. Patients infected with HBV also have a higher risk of developing non-Hodgkin lymphoma. Ulcickas Yood et al[7] found that patients with HBV had a 2.8 times higher risk of NHL. However, only few cases of coexistent HCC and NHL in patients with HBV have been reported in the literature. Talamo et al[8] reported the first case of simultaneous primary hepatic lymphoma and HCC in a patient with chronic HBV. Takeshima et al[14] reported another patient with HBV infection developed coexistent hepatic mucosa-associated lymphoid tissue lymphoma and HCC. These two reports described primary hepatic lymphoma that did not involve extra-hepatic lymph nodes or organs. Cavanna et al[9] reported a case of hepatic NHL relapse without extra-hepatic involvement in a patient who had HCC. Shikuwa et al[10] and Monarca et al[15] reported two cases of HCC and malignant lymphoma with extra-hepatic involvement. These cases revealed the rare coexistence of HCC and NHL with or without extrahepatic involvement in hepatitis B carrier, but the role of HBV in HCC and NHL was not addressed. To the best of our knowledge, this is the only published report to date. Other reports include cases of HCV infection and two cases without chronic hepatitis or liver cirrhosis[16,17]. In the present case, this patient had not received any prior chemotherapy. Moreover, there are no clinical or pathologic evidences of HCV infection, cirrhosis or alcohol abuse. Therefore, the only etiology for the two tumor growth is HBV infection. This patient is a rare case of coexistent HCC and mantle cell lymphoma in HBV infection.
Only a few studies on the association between HCC and NHL have been published. Di Stasi et al[2] reported that 4 of the 132 patients with NHL developed HCC and that all four patients had liver cirrhosis. Tanaka et al[3] reported that 9 of the 592 patients with NHL developed HCC during the first 10 years following the diagnosis. Of the nine patients who developed HCC, eight had clinical or histologic evidence of cirrhosis, six were HCV antibody positive, and none had HBV infection. The study also found that patients who received chemotherapy for NHL had a significantly increased risk of HCC. Civardi et al[4] reported 7 cases of HCC among the 414 patients with NHL; all of these cases were HCV antibody positive. Based on these studies, hepatitis virus infection, liver damage and antineoplastic agents may play important roles in the development of concurrent HCC and NHL. A subpopulation of chemotherapy-induced lymphoma cell may selectively invade the liver. Recurrence of HCC may have resulted in the simultaneous co-localization of the two distinct tumors. Another study by Xiong et al[18] found that the Cdc6 G1321A polymorphism lowers the risk of developing both NHL and HCC.
There are accumulated evidences on the associations of HCV and HBV with hematologic malignancies, in particular B-cell NHL. HCV has been the most frequently studied. Chronic viral antigen stimulation that leads to proliferation of B-cells and mutations in tumor suppressor genes has been proposed as two likely pathways of HCV-induced NHL[19,20]. Conversely, the association between NHL and HBV has not been studied. Similar to HCV, HBV may induce NHL formation through the similar mechanism. Two mechanisms have been proposed[21]. In HBV-infected patients, the chronic antigen stimulation from HBV activates B-cells, which in the long term leads to subsequent DNA damage and lymphoma formation. The second mechanism involves synthesis of viral antigen and assembly of viral particles in hepatocytes and lymphocytes. HBV particles can then infect other lymphocytes that are located in lymphoid organs[5,22]. Viral DNA integrats into the host genome; this leads to overexpression of cellular oncogenes or down-regulation of tumor suppressor genes. Further investigations are needed to address these questions.
In the present case, liver tumor biopsy revealed a coexistent HCC and mantle cell lymphoma. The occurrence of one tumor spreading into another tumor, referred to as “tumor-to-tumor metastasis (TTM)”, is rare. The most frequent cancer with metastasis is lung cancer. And the most frequent recipients are renal clear cell carcinomas. To date, NHL has rarely infiltrated other tumors, especially HCC. To our knowledge, only one similar case has been reported[23].
In summary, we have presented a rare case of hepatic co-localization of HCC and mantle cell lymphoma in a patient with HBV infection. The case showed a rare pattern of “tumor-to-tumor metastasis.” This case suggests that although lymph node enlargements are often considered to be reactive or metastatic lymphadenopathy in chronic hepatitis B patients who have HCC, NHL should also be considered as a differential diagnosis. Future large studies are required to establish firm evidence of the relationship between the occurrence of NHL and HCC.
A 52-year-old male with hepatitis B infection presented with easy fatigue, poor appetite and progressive weight loss of 10 kg over the past 2 mo.
Multiple enlarged lymph nodes were found on the neck and in the inguinal region upon physical examination of the patient.
Advanced hepatocellular carcinoma (HCC) with distal lymph node metastases; lymphoma with hepatic involvement.
AST: 41 U/L; Hb: 18.4 g/dL; PLT: 97 × 103 UL; alpha-fetoprotein: 49465.6 ng/mL; metabolic panel was within the normal reference limits.
Contrasted computed tomography showed a 7-cm in diameter liver mass at S7 with heterogeneous enhancement in the arterial phase and wash out in the delay phase. Moreover, splenomegaly and multiple mediastinal and mesenteric enlarged lymph nodes were observed.
Liver biopsy revealed HCC with an aggregate of small to medium-sized lymphoid cells that were CD20, CD5 and cyclin D1 positive.
Radiofrequency ablation of the liver tumor was performed, and cyclophosphamide-hydroxydaunorubicin-oncovin-prednisone chemotherapy was administered to treat the lymphoma.
This report presents a rare case of coexistent HCC and mantle cell lymphoma in a patient with hepatitis B virus infection. The case suggests that although lymph node enlargements are often considered to be reactive or metastatic lymphadenopathy in chronic hepatitis B patients who have HCC, non-Hodgkin’s lymphoma should also be considered as a differential diagnosis.
The submitted manuscript represents a case report about a male patient chronically infected with HBV. The patient had enlarged lymph nodes in the neck and inguinal regions, and a tumor in the Cauinaud’s segment 7. The case report describes an interesting case with lymphoid cells infiltrating the HCC. The authors should clarify or discuss whether there is an evidence of a wider infiltration into the liver tissue or exclusively into the HCC. Also, please state whether there was any evidence for a spread into the gastrointestinal tract and/or bone marrow.
P- Reviewer: Netter HJ S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
| 1. | Schütte K, Bornschein J, Malfertheiner P. Hepatocellular carcinoma--epidemiological trends and risk factors. Dig Dis. 2009;27:80-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 309] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 2. | Di Stasi M, Cavanna L, Fornari F, Civardi G, Rossi S, Sbolli G, Giacani M, Fermi S, Buscarini L. Association of non-Hodgkin’s lymphoma and hepatocellular carcinoma. Oncology. 1990;47:80-83. [PubMed] |
| 3. | Tanaka H, Tsukuma H, Teshima H, Ajiki W, Koyama Y, Kinoshita N, Masaoka T, Oshima A. Second primary cancers following non-Hodgkin’s lymphoma in Japan: increased risk of hepatocellular carcinoma. Jpn J Cancer Res. 1997;88:537-542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Civardi G, Vallisa D, Bertè R, Lazzaro A, Moroni CF, Cavanna L. Focal liver lesions in non-Hodgkin’s lymphoma: investigation of their prevalence, clinical significance and the role of Hepatitis C virus infection. Eur J Cancer. 2002;38:2382-2387. [PubMed] |
| 5. | Pontisso P, Vidalino L, Quarta S, Gatta A. Biological and clinical implications of HBV infection in peripheral blood mononuclear cells. Autoimmun Rev. 2008;8:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Giacomin A, Cazzagon N, Sergio A, Vanin V, Farinati F. Hepatitis B virus-related hepatocellular carcinoma: primary, secondary, and tertiary prevention. Eur J Cancer Prev. 2011;20:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ulcickas Yood M, Quesenberry CP, Guo D, Caldwell C, Wells K, Shan J, Sanders L, Skovron ML, Iloeje U, Manos MM. Incidence of non-Hodgkin’s lymphoma among individuals with chronic hepatitis B virus infection. Hepatology. 2007;46:107-112. [PubMed] |
| 8. | Talamo TS, Dekker A, Gurecki J, Singh G. Primary hepatic malignant lymphoma: its occurrence in a patient with chronic active hepatitis, cirrhosis, and hepatocellular carcinoma associated with hepatitis B viral infection. Cancer. 1980;46:336-339. [PubMed] |
| 9. | Cavanna L, Civardi G, Fornari F, Vallisa D, Berte R, Buscarini E, Sbolli G, Paties C, Foroni R, Di Stasi M. Simultaneous relapse of liver cell carcinoma and non-Hodgkin’s lymphoma in the liver. Report of a case with diagnosis by ultrasonically guided fine needle aspiration biopsy. Acta Cytol. 1994;38:451-454. [PubMed] |
| 10. | Shikuwa S, Ito M, Nakashima M, Hamasaki K, Naito S, Sekine I, Fujii H. Autopsy case of colocalized tumors of hepatocellular carcinoma and malignant lymphoma. J Gastroenterol. 1996;31:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Suriawinata A, Ye MQ, Emre S, Strauchen J, Thung SN. Hepatocellular carcinoma and non-Hodgkin lymphoma in a patient with chronic hepatitis C and cirrhosis. Arch Pathol Lab Med. 2000;124:1532-1534. [PubMed] |
| 12. | Ohtsubo K, Oku E, Imamura R, Seki R, Hashiguchi M, Osaki K, Yakushiji K, Yoshimoto K, Ogata H, Nagamatsu H. Simultaneous hepatic relapse of non-Hodgkin’s lymphoma and hepatocellular carcinoma in a patient with hepatitis C virus-related cirrhosis. Acta Haematol. 2006;116:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1764] [Cited by in RCA: 1843] [Article Influence: 97.0] [Reference Citation Analysis (0)] |
| 14. | Takeshima F, Kunisaki M, Aritomi T, Osabe M, Akama F, Nakasone T, Niino D, Katayama S, Isomoto H, Omagari K. Hepatic mucosa-associated lymphoid tissue lymphoma and hepatocellular carcinoma in a patient with hepatitis B virus infection. J Clin Gastroenterol. 2004;38:823-826. [PubMed] |
| 15. | Monarca R, Montanaro M, Stroffolini T. Simultaneous occurrence of hepatocellular carcinoma and low grade non-Hodgkin’s lymphoma in a chronic hepatitis B surface antigen carrier. Ann Hematol. 1999;78:531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Kataoka TR, Tsukamoto Y, Kanazawa N, Izumi T, Awata N, Nishizawa Y, Ohsawa M, Ishiguro S. Concomitant hepatocellular carcinoma and non-Hodgkin’s lymphoma in a patient with nodular regenerative hyperplasia. Pathol Int. 2006;56:279-282. [PubMed] |
| 17. | Heidecke S, Stippel DL, Hoelscher AH, Wedemeyer I, Dienes HP, Drebber U. Simultaneous occurrence of a hepatocellular carcinoma and a hepatic non-Hodgkin’s lymphoma infiltration. World J Hepatol. 2010;2:246-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Xiong XD, Qiu FE, Fang JH, Shen Y, Liang C, Jiang W, Zhuang SM. Association analysis between the Cdc6 G1321A polymorphism and the risk for non-Hodgkin lymphoma and hepatocellular carcinoma. Mutat Res. 2009;662:10-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Schöllkopf C, Smedby KE, Hjalgrim H, Rostgaard K, Panum I, Vinner L, Chang ET, Glimelius B, Porwit A, Sundström C. Hepatitis C infection and risk of malignant lymphoma. Int J Cancer. 2008;122:1885-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Marcucci F, Mele A. Hepatitis viruses and non-Hodgkin lymphoma: epidemiology, mechanisms of tumorigenesis, and therapeutic opportunities. Blood. 2011;117:1792-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 182] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 21. | Marcucci F, Spada E, Mele A, Caserta CA, Pulsoni A. The association of hepatitis B virus infection with B-cell non-Hodgkin lymphoma - a review. Am J Blood Res. 2012;2:18-28. [PubMed] |
| 22. | Féray C, Zignego AL, Samuel D, Bismuth A, Reynes M, Tiollais P, Bismuth H, Brechot C. Persistent hepatitis B virus infection of mononuclear blood cells without concomitant liver infection. The liver transplantation model. Transplantation. 1990;49:1155-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 132] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Utsunomiya T, Okamoto M, Tsujita E, Yamamoto M, Tsutsui S, Fujihara M, Ishida T. Hepatocellular carcinoma infiltrated with non-Hodgkin’s lymphoma: report of a case. Surg Today. 2009;39:1010-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |