Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11467
Peer-review started: July 31, 2021
First decision: September 4, 2021
Revised: September 17, 2021
Accepted: November 14, 2021
Article in press: November 14, 2021
Published online: December 26, 2021
Processing time: 145 Days and 2.5 Hours
Intramural esophageal dissection (IED) is a rare disease that should be considered in patients with chest pain, dysphagia, and hematemesis. Although it occurs most frequently in older adult women with impaired coagulation or as a sequela of endoscopy, the incidence of spontaneous IED without an obvious causative agent has risen gradually.
This report describes a case of extensive annular IED in a 75-year-old male patient who presented with dysphagia for the past month. Esophageal barium meal radiography revealed slow passage of diluted iohexol through the esophagus after swallowing, prominent luminal dilation, obstruction of the lower segment with only a small amount of contrast medium entering the gastric cavity, and no obvious extravasation. Gastroscopy revealed smooth esophageal mucosa; several esophageal mucosal bridges and webbed mucosa were observed approximately 22 cm from the incisor. The mucosal surface was occasionally rough and uneven, and the length of the esophageal mucosal defect exceeded 10 cm. The anatomy was considered to be annular because the mucosal bridge connecting the proximal and distal tube was not attached to the surrounding myotubes. The final diagnosis was spontaneous extensive annular IED. We treated the patient successfully using endoscopic esophagotomy, which completely relieved the symptoms without complications.
Spontaneous annular IED can be treated successfully by endoscopic resection of the mucosal septum between the true and false lumen.
Core Tip: Intramural esophageal dissection (IED) is a rare entity characterized by mucosal rupture resulting in a false cavity. Herein, we presented a rare case of spontaneous annular IED that was treated successfully by endoscopic resection of the mucosal septum between the true and false lumina without complications, resulting in complete symptomatic relief. Physicians should consider IED, especially in elderly patients, after excluding other thoracic emergencies. This study indicates that endoscopic treatment may be effective in treating annular IED, without complications and aid clinicians in selecting the most suitable treatment, depending on the patient’s condition and type of lesion.
- Citation: Hu JW, Zhao Q, Hu CY, Wu J, Lv XY, Jin XH. Rare spontaneous extensive annular intramural esophageal dissection with endoscopic treatment: A case report. World J Clin Cases 2021; 9(36): 11467-11474
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11467.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11467
Intramural esophageal dissection (IED) is a rare disease characterized by a long tear occurring deep in the esophageal mucosa but without complete perforation. This condition represents an intermediate form of esophageal injury between the Mallory-Weiss tear and Boerhaave syndrome. Boerhaave syndrome occurs after severe vomiting, while IED usually occurs in patients with coagulation disorders, those taking oral anticoagulants, patients with blunt injuries, or eosinophilic esophagitis. Iatrogenic causes such as the insertion of a nasogastric tube or endoscopic examination, and ingestion of irritating food can also result in IED[1-3]. Patients usually present with dysphagia, odynophagia, and retrosternal chest pain; IED may mimic cardiac or thoracic emergencies, such as acute myocardial infarction and aortic dissection[4,5]. The majority of patients respond well to conservative treatment. Interventions such as endoscopic treatment and surgical resection of the diseased esophagus are rarely needed in patients with partial IED. However, the management of annular IED is complex and requires long-term endoscopic treatment and, sometimes, even surgery[2].
A 75-year-old male patient was transferred to our hospital due to dysphagia for the past month.
The patient’s symptoms commenced a month prior and mainly included difficulty in eating, choking, and soreness in the chest and back. There was no history of ingestion of a sharp foreign body, trauma, bleeding, or past endoscopy.
The patient had a history of hypertension and diabetes mellitus.
No obvious personal and family history was found.
No obvious abnormalities were observed on physical examination performed at the time of admission.
No obvious abnormalities were detected on laboratory examination.
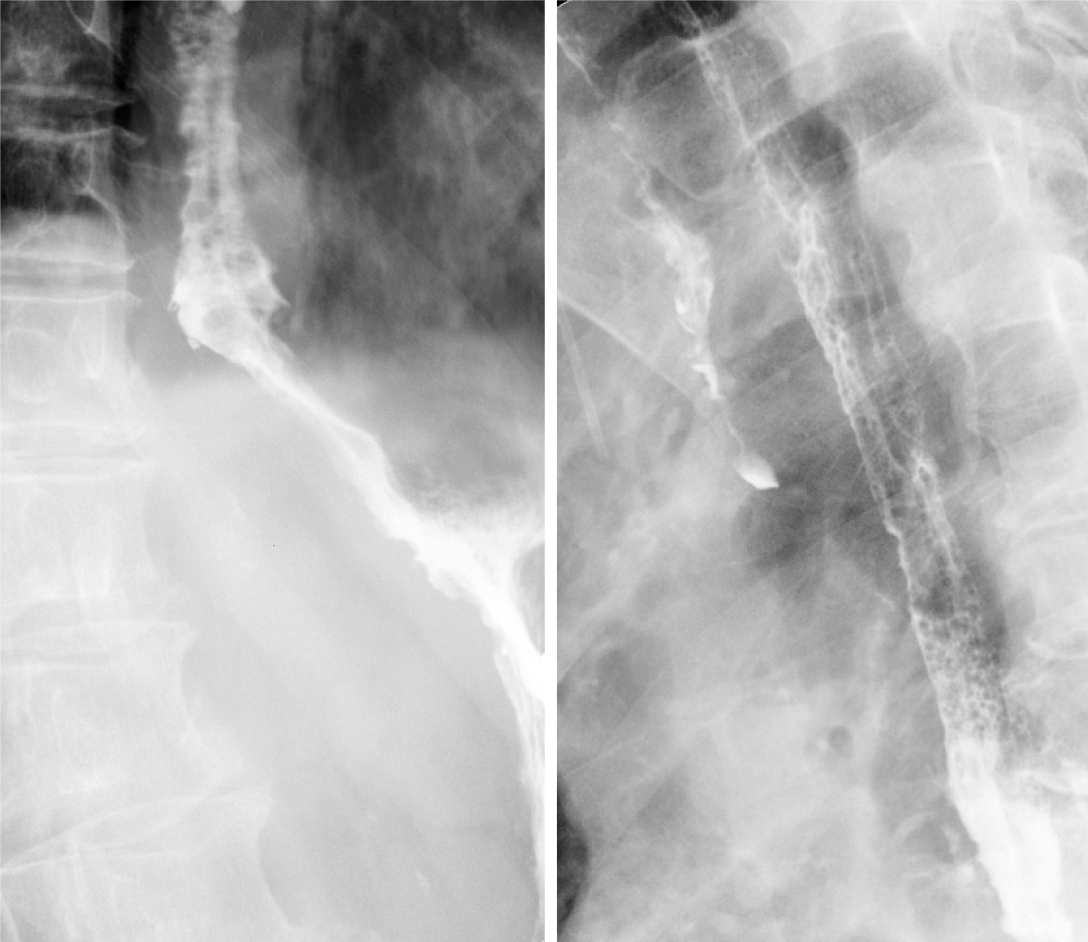
Barium meal radiography of the esophagus revealed the following: slow passage of the diluted iohexol through the esophagus after swallowing, prominent dilation of the lumen, obstruction OF the lower segment with only a small amount of contrast medium entering the gastric cavity, and no obvious extravasation (Figure 1).
Esophageal computed tomography (CT) depicted dilation of the esophageal cavity with an irregular diaphragmatic shadow, linear-enhancement of the mucosa after contrast enhancement, and some segments of the esophagus that were “double-barreled” (Figure 2); there was no mediastinal emphysema or pleural fusion.
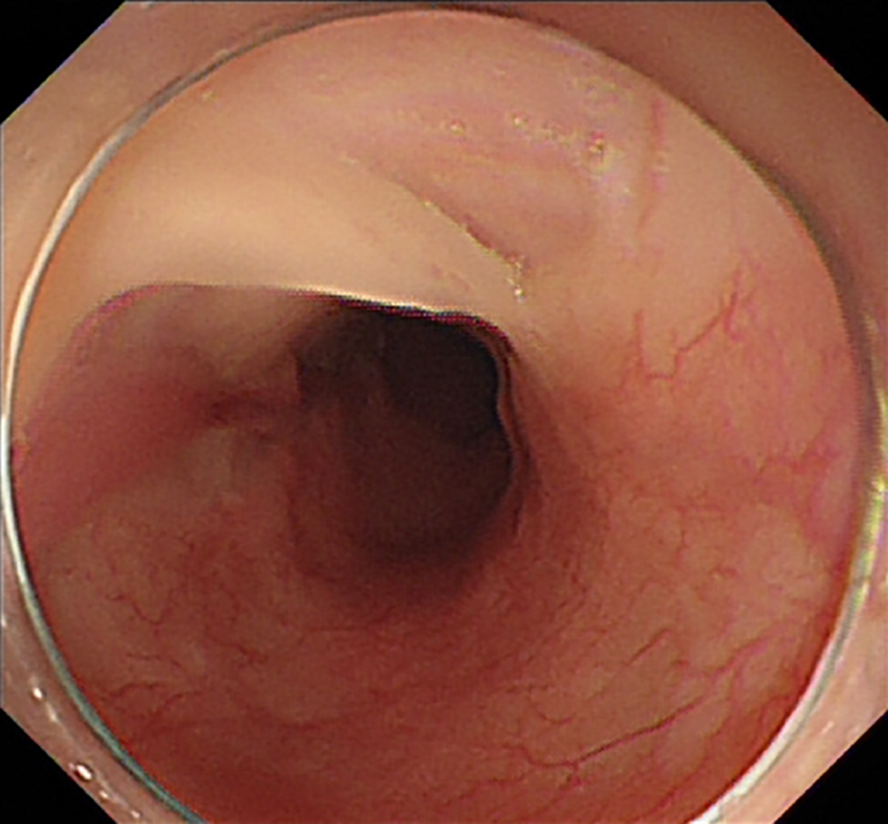
Gastroscopy revealed smooth esophageal mucosa; however, several esophageal mucosal bridges and webbed mucosa were observed approximately 22 cm from the incisor. The mucosal surface was rough and uneven in some places, and the length of the esophageal mucosal defect exceeded 10 cm. The anatomy was considered to be annular because the mucosal bridge connecting the proximal and distal tube was not attached to the surrounding myotubes. The lower end of the distal mucosal duct was collapsed, the endoscope mainly entered the dead sac, and the blind end terminated at about 2 cm above the gastroesophageal junction (Figure 3A and B).
The final diagnosis of the presented case was spontaneous extensive annular IED.
We chose endoscopic esophagotomy for treatment since our patient had an extensive annular IED and extensive mucosal defects. During the procedure, we observed that the esophageal mucosa was completely stripped and dissociated within the esophageal cavity, and the lower end was narrow, which did not permit the passage of the gastroscope. L-H S-E methylene blue solution was injected locally, and the blind end of the mucosa was resected using an L-knife. Subsequently, a disposable polypectomy device was used to remove a segment of the mucosal strip so that the blind end could be unobstructed, after which the gastroscope could be passed through the gastric cavity smoothly, and a gastric tube was finally inserted (Figures 3C-E and 4).
We chose endoscopic esophagotomy for treatment since our patient had an extensive annular IED and extensive mucosal defects. During the procedure, we observed that the esophageal mucosa was completely stripped and dissociated within the esophageal cavity, and the lower end was narrow, which did not permit the passage of the gastroscope. L-H S-E methylene blue solution was injected locally, and the blind end of the mucosa was resected using an L-knife. Subsequently, a disposable polypectomy device was used to remove a segment of the mucosal strip so that the blind end could be unobstructed, after which the gastroscope could be passed through the gastric cavity smoothly, and a gastric tube was finally inserted (Figures 3C-E and 5).
IED is a rare disease with a benign course, good prognosis, and low mortality[6]. It is currently believed that the etiology and pathogenesis of the disease mainly fall into three categories: (1) IED formation secondary to traumatic mucosal injury, including iatrogenic and non-iatrogenic trauma[7,8]. The former includes esophageal dilatation, conventional endoscopic biopsy, and intraesophageal injection of sclerosing agent to stop bleeding; the latter mainly includes swallowing foreign bodies or food incarceration; (2) IED formation secondary to intra-esophageal hemorrhage[9], more common in middle-aged and older adult women and patients with coagulation disorders or oral anticoagulants. Small blood vessels under the mucosa rupture and hemorrhage, forming hematomas. The hematomas can be localized and can also tear the mucosa and muscle layer and cause large-scale intramural dissection; and (3) Idiopathic IEDs are rare, and Cho et al[10] reported the case of a 39-year-old healthy man who had no obvious cause for IED. However, when we continued to inquire about our patient’s medical history we learned that the patient developed chest discomfort after ingesting “ergot” (a hard object) a month prior, and then repeated and increased vomiting. We speculate that this may have caused damage to the esophageal mucosa, and then during vomiting, the pressure in the esophageal cavity increased, secondary tissue tore, and the submucosal wall may have been dissected. The patient's medical history is consistent with the characteristics of IED-related diseases. In addition, histopathology of the esophagus revealed chronic mucosal inflammation with inflammatory granulation tissue formation (non-specific inflammation), and no obvious signs of tumors, diverticula, or other underlying pathological signs. Eosinophilic esophagitis and mycosis were excluded and the patient did not have coagulation dysfunction. He denied use of anticoagulants or antiplatelets or a history of drug use. Therefore, we speculated that the possible cause of this patient's IED was the formation of IED secondary to traumatic mucosal injury. At present, the diagnosis of IED mainly depends on esophagography, endoscopy, and CT findings. Early IED is usually diagnosed using esophagography[11]. In most patients with IED, the esophageal mucosa is breached, and a small amount of contrast medium can flow into the false lumen, while the true lumen is unobstructed. The contrast medium can flow into the stomach through the gastroesophageal junction smoothly, forming the characteristic “barium double-track” sign. However, the possibility of esophageal duplication should be eliminated if this sign is observed. Leakage of contrast medium into the false lumen can also occur in esophageal rupture[12]. In the present case, the defect in the esophageal mucosa was extensive, and the contrast medium could flow into the true and false lumina simultaneously. The false cavity was huge, and a large amount of contrast agent that accumulated within the false cavity compressed the true cavity because the entire thoracic esophagus had an annular dissection. Therefore, radiography only revealed a prominent dilation of the thoracic esophagus, narrowing of the gastroesophageal junction at the lower esophagus, and no typical signs of IED were observed. Endoscopy is also one of the principal methods for the diagnosis of IED[13]. Mucosal rupture and the mucosal space between the true and false cavities can be observed on endoscopy. The presence of a false cavity can confirm the diagnosis of IED, and the length and scope of the dissection can be determined. CT has now become the investigation of choice for detecting this disease, owing to the development of imaging technology. The presence and morphology of the true and false lumina can be observed on transverse and coronal sections of the CT scan. If CT is performed immediately after the intake of the oral contrast agent, the extravasation of the contrast agent can also be observed, which is indicative of esophageal rupture[13,14]. IED is considered a benign disease that is usually treated conservatively. The administration of intravenous fluids, antiemetics, and proton pump inhibitors, and close monitoring may be the appropriate treatment for patients with IED without esophageal perforation. Most case reports have described partial IEDs, which respond to conservative or simple endoscopic treatment. Only a few cases of annular IED have been reported in the literature, and conservative management is usually unsuccessful in these patients[3]. Our patient had an extensive annular IED and large mucosal defects, which necessitated endoscopic treatment or surgery. Endoscopic interventions such as adhesiolysis, distal mucosal incision, and placement of a bougie or stent play an auxiliary role in providing symptomatic relief. The development of endoscopic technology in recent years has resulted in several studies: Shelton et al[7], Kim et al[9], and Cho et al[10], and reports of the use of a needle-shaped papillotomy knife for cutting the mucosal septum between the true and false lumina endoscopically, so that the two lumina could be connected. At the same time, the disease was cured by the strong regenerative ability of the mucosa that covered the surface of the esophageal muscle layer. We performed esophagotomy in our patient. Postoperative barium meal radiography showed a smooth passage of the contrast medium and widening of the lumen; the patient recovered well after surgery. Endoscopic treatment is usually not accomplished after only a single procedure; it may sometimes require a long and complex process[9]. We could also have chosen to insert an endoscopic stent in our patient. However, mucosal stripping started 22 cm from the incisor, the mucosal defect was as long as 10 cm, and the blind sac was enlarged, reaching up to 2 cm above the gastroesophageal junction. The patient would have required a very long stent, the proximal end of which would have been close to the cricopharyngeus. Extensive scarring can occur easily at the site of mucosal defects, making the removal of the stent difficult. In this case, the possibility of failure of endoscopic stent implantation is very high. Therefore, we suggest that if the esophageal mucosal defect is limited and the scope is small, stent placement can be performed, otherwise this approach is not supported and numerous case reports have stated that serious systemic or local infection or esophageal rupture may be present concomitantly when the dissection occurs over a long stretch of the esophagus. Therefore, it is safer and more reliable to surgically remove the diseased esophagus and reconstruct the digestive tract, which is likely to be more beneficial to patients[8,13,15]. Fortunately, our patient achieved satisfactory results in esophagotomy. However, our case report has a few limitations. First, the patient could only be followed up for 2 mo after the procedure, owing to loss to follow-up, which is not sufficient to determine the long-term complications. Second, the surgical risk was high due to our patient’s age and comorbidities. The patient refused esophagectomy, which is an extensive procedure that can lead to poor quality of life; therefore, endoscopic management was selected to treat annular IED.
Only a few studies on IED requiring surgery are available in the literature. A high level of suspicion is conducive to timely diagnosis for patients with typical symptoms, including those with repeated vomiting, recent foreign body ingestion, or a history of upper gastrointestinal endoscopy. Even though endoscopic management is a viable option, the treatment method for IED should be based on the type and severity of the lesion, presence of serious complications such as esophageal rupture, mediastinitis, and stricture, and the patient’s condition.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ding X, Syahputra DA S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Ibáñez-Sanz G, Rodríguez-Alonso L, Romero NM. Spontaneous intramural esophageal dissection: an unusual onset of eosinophilic esophagitis. Rev Esp Enferm Dig. 2016;108:156-157. [PubMed] |
| 2. | Anand S. Circumferential intramural esophageal dissection with large mucosal defect. Clin J Gastroenterol. 2020;13:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Zhu RY, Law TT, Tong D, Tam G, Law S. Spontaneous circumferential intramural esophageal dissection complicated with esophageal perforation and esophageal-pleural fistula: a case report and literature review. Dis Esophagus. 2016;29:872-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Abdi S, Baianati MR, Momtahen M, Mohebbi B. Intramural Esophageal Dissection: A Rare Cause of Acute Chest Pain after Percutaneous Coronary Intervention. J Tehran Heart Cent. 2019;14:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Heitmiller RF. Intramural esophageal dissection with perforation. Gastroenterol Hepatol (N Y). 2008;4:365-366. [PubMed] |
| 6. | Lučenič M, Zsemlye Z, Hlavatý T, Koller T. [Intramural esophageal dissection]. Rozhl Chir. 2013;92:450-454. [PubMed] |
| 7. | Shelton JH, Mallat DB, Spechler SJ. Esophageal obstruction due to extensive intramural esophageal dissection: diagnosis and treatment using an endoscopic 'rendezvous' technique. Dis Esophagus. 2007;20:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Krieg A, Vogt C, Ramp U, Poll LW, Brinkmann MJ, Bölke E, Knoefel WT, Peiper M. Combined esophageal injury complicated by progression to a second perforation: a case report. J Med Case Rep. 2009;3:9213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Kim SH, Lee SO. Circumferential intramural esophageal dissection successfully treated by endoscopic procedure and metal stent insertion. J Gastroenterol. 2005;40:1065-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Cho CM, Ha SS, Tak WY, Kweon YO, Kim SK, Choi YH, Chung JM. Endoscopic incision of a septum in a case of spontaneous intramural dissection of the esophagus. J Clin Gastroenterol. 2002;35:387-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Lowman RM, Goldman R, Stern H. The roentgen aspects of intramural dissection of the esophagus. The mucosal stripe sign. Radiology. 1969;93:1329-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Katabathina VS, Restrepo CS, Martinez-Jimenez S, Riascos RF. Nonvascular, nontraumatic mediastinal emergencies in adults: a comprehensive review of imaging findings. Radiographics. 2011;31:1141-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Cullen SN, McIntyre AS. Dissecting intramural haematoma of the oesophagus. Eur J Gastroenterol Hepatol. 2000;12:1151-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Constantine S. Oesophageal dissection: contrast studies and CT in diagnosis and monitoring. Australas Radiol. 2003;47:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Liguori G, Cortale M, Cimino F, Sozzi M. Circumferential mucosal dissection and esophageal perforation in a patient with eosinophilic esophagitis. World J Gastroenterol. 2008;14:803-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |