Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9954
Peer-review started: June 11, 2021
First decision: July 15, 2021
Revised: August 9, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: November 16, 2021
Processing time: 151 Days and 21.1 Hours
Complex aberration in lung is rare, which may increase risk of vascular injury and cause ligation of wrong pulmonary vein or bronchus by mistake during lung surgery, and result in sever complication like pulmonary congestion or atelectasis.
A 44-year-old female was admitted for a ground glass nodule (24 mm in diameter) in her right upper lobe. Video-assisted thoracoscopic (VATS) right upper lobectomy with lymph nodes dissection was performed. During operation, we simultaneously identified extremely rare aberrations of right preeparterial bronchus, right upper lobe vein behind pulmonary artery and right middle lobe vein drained into left atrium in this patient. The patient was well recovered and discharged at the postoperative-day 4.
Preoperatively, three-dimensional reconstruction can help to identify incon
Core Tip: Complex aberration in lung is rare but inappropriate management of aberration may result in severe complications. In this case, we presented an extremely rare aberrations of right preeparterial bronchus, right upper lobe vein behind pulmonary artery and right middle lobe vein drained into left atrium simultaneously identified in one patient. This case highlights the importance of preoperative three-dimensional reconstruction and careful skeletonization and identification of aberrant anatomic structures during surgery.
- Citation: Wang FQ, Zhang R, Zhang HL, Mo YH, Zheng Y, Qiu GH, Wang Y. Rare location and drainage pattern of right pulmonary veins and aberrant right upper lobe bronchial branch: A case report. World J Clin Cases 2021; 9(32): 9954-9959
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9954.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9954
Aberrations of pulmonary vessels and the bronchus are potentially dangerous which may increase risk of vascular injury and transection of the wrong vessel(s) during surgery[1]. Due to the increasing number of lung cancer and lung surgery[2,3], preoperative identification of anatomic variation in lung is much important for the operation safety.
Thin-section computed tomography (CT) is widely applied before lung surgery[4,5]. Recently, three-dimensional reconstruction has been increasingly adopted, which can demonstrate variations more intuitively[1]. Herein, we reported the coexistence of infrequent location of right upper lobe vein, right pulmonary venous drainage pattern, and the right preeparterial bronchus in one patient (as evinced by dissection and imaging examination).
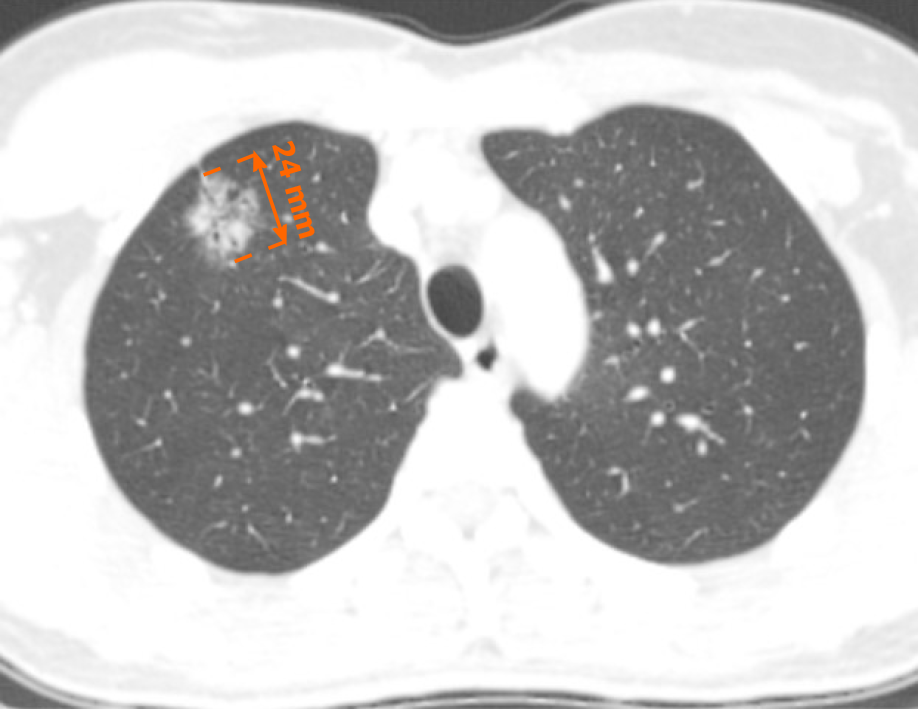
A 44-year-old female patient was admitted for ground-glass nodule (GGN) with a maximum diameter of 24 mm in the right upper lobe (Figure 1).
One month before admission, a GGN with a maximum diameter of 24 mm in her right upper lobe was found in chest CT for health examination. She had no pulmonary symptoms.
She underwent breast augmentation about seven years ago and denied any other surgical history.
The patient denied any relevant family history.
Her temperature was 36.5°C, heart rate was 78 bpm, respiratory rate was 20 breaths per minute, blood pressure was 132/97 mmHg and oxygen saturation in room air was 100%. Her chest wall and breath sounds were normal. Heart rhythm was regular.
Preoperatively, her routine blood test, urinalysis, liver function, renal function and coagulation test were all in the normal ranges.
The Cranial and abdominal CT with contrast and bone scan with single photon emission computed tomography showed no sign of metastasis.
The final diagnosis of the presented case is adenocarcinoma in upper lobe of right lung.
Considering that the diameter of this GGN was more than 20mm, we thus planned to perform VATS right upper lobectomy and lymph node dissection, if necessary.
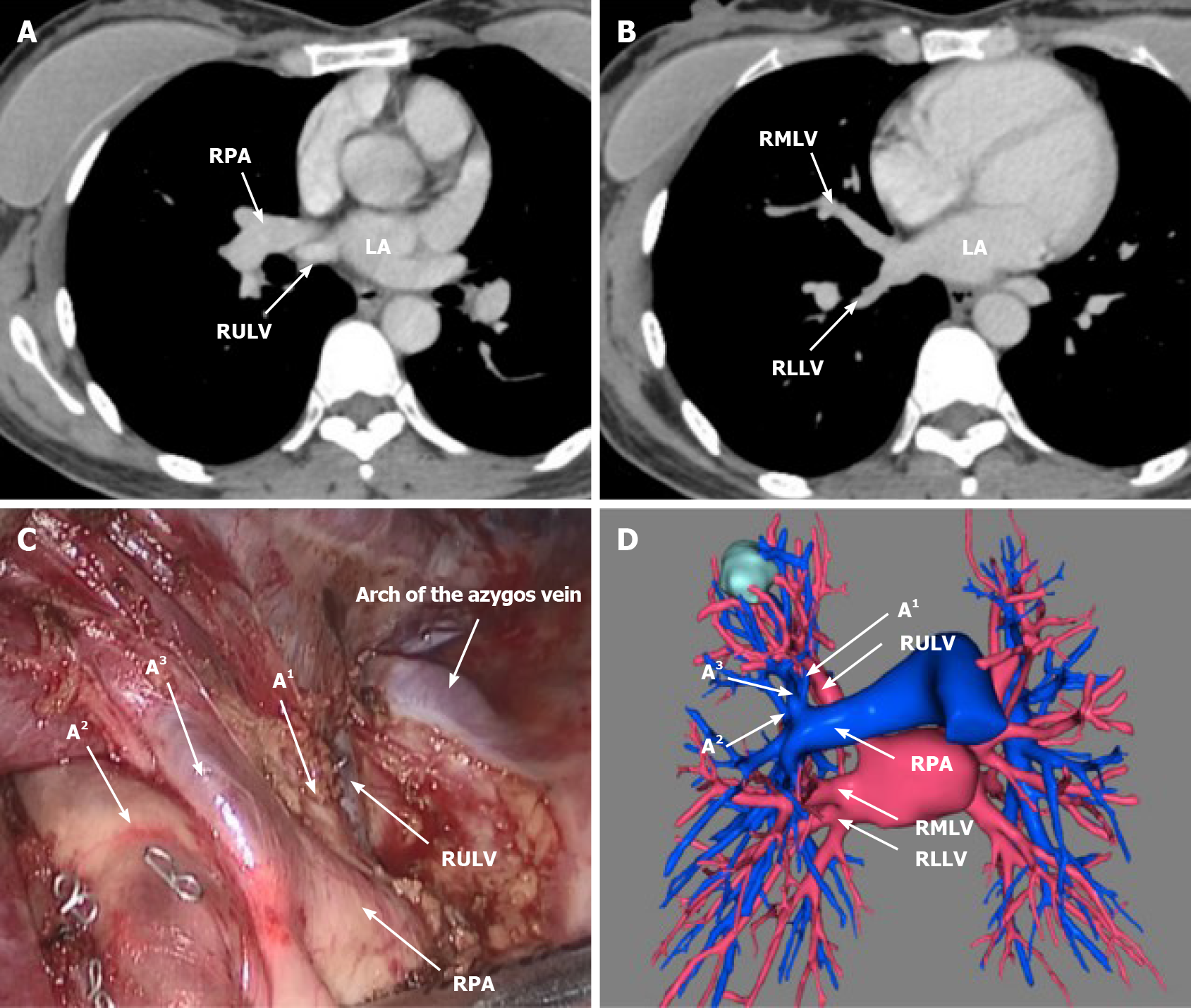
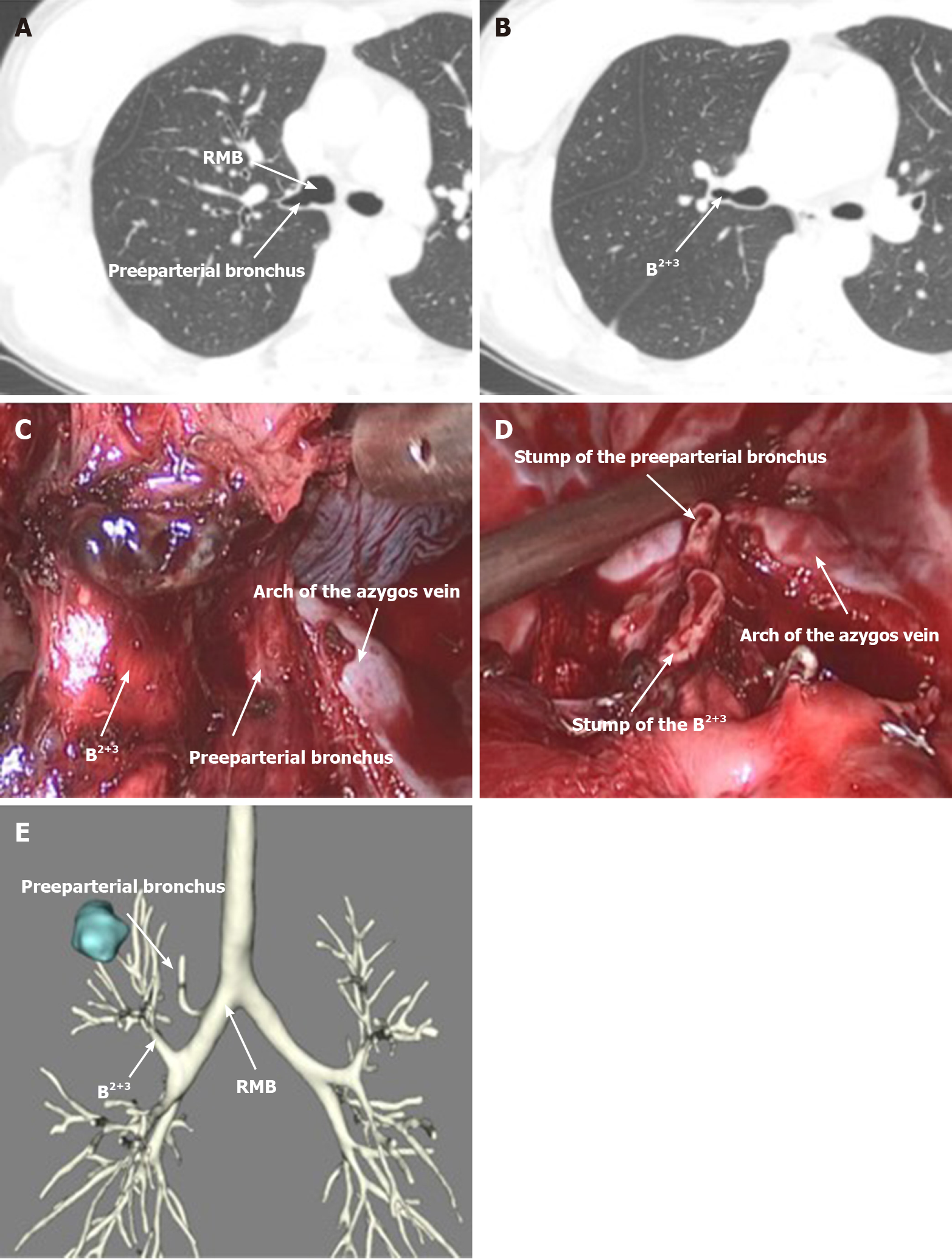
There was no obvious aberration when we explored the thoracic cavity at the beginning. We dissected mediastinal pleura on the ventral side of the hilum. Thereafter, the right pulmonary artery was shown but there was no right upper lobe vein (RULV). We then divided the horizontal fissure and finally the RULV was shown on the dorsal side of the right pulmonary artery (RPA) (Figure 2). To identify the right middle lobe vein (RMLV), we retraced the RULV to the dorsal side of the right descending interlobar artery, while no venous convergence of RMLV and RULV was found. Subsequently, we stapled RULV and A1 to reveal the right upper lobe bronchus. Interestingly, instead of arising from the right upper lobe bronchus, B1 in this case arose directly from the right main bronchus (RMB), also called the right preeparterial bronchus (Figure 3)[4]. B2+3 then arose as one trunk from the RMB below B1. Intraoperative frozen section revealed that the GGN was an adenocarcinoma in superior lobe of right lung adenocarcinoma, so we performed a right upper lobectomy and systematic lymph node dissection.
Postoperatively, we carefully reviewed thin-section CT and reconstructed three-dimension model of lung: Results showed that RULV lay behind the RPA and drained into the left atrium (LA) alone. RMLV joined the right lower lobe vein (RLLV) to form a short common trunk draining into LA (Figure 2). Meanwhile, B1 arose from RMB alone and B2+3 arose from RMB below B1 (Figure 3).
No postoperative complication arose. The patient was discharged on the postoperative day 4. The follow-up is performed in the out-patient department every 3 mo during the first year and every 6-8 mo during the following 2-5 years after surgery. Presently, the patient recovered well and showed no signs of recurrence upon the last follow-up. Written informed consent was obtained from the patient.
In this case, infrequent preeparterial bronchus and aberrations in course and location of pulmonary veins were found in one patient at the same time. Although the aberrations were not quite obvious to be identify in axial images preoperatively, we found such aberrations and avoided wrong ligation of vessels and bronchus during operation by careful dissection. Meanwhile, such aberrations were confirmed with postoperative three-dimension reconstruction visually. Based on the literature review, such complex aberrations of pulmonary vessels and bronchus had seldom been reported before.
Complex variations in pulmonary bronchus and vessels are quite rare and may increase the difficulty of lobectomy. Dr. Chassagnon reported that the right preeparterial bronchus occurred in only 0.9% of people in a study of 1200 bronchograms[4]. In this case, we dissected fissure firstly and divided the pulmonary artery and vein afterwards. So, the bronchus can be exposed optimally. But if we performed the single-direction thoracoscopic lobectomy and undermine fissure in the last stage, anomalous bronchus may cause difficulty of dissection. Besides, it is reported that RMLV joins RLLV to form one common trunk drain into LA in only in 2%-3% of patients[5]. However, it is worth noting that aberrant right pulmonary venous drainage patterns are not rare, which may occur in 32% of patients[5]. Ligation of such aberrant veins by mistake can result in severe complications.
Moreover, abnormal location of the entire RULV behind RPA is also extremely rare. There had been only three cases reported with such an aberration before[1,6,7]. This aberration caused several difficulties in our experience. Firstly, the RPA in this case was located in usual site of the right pulmonary vein which was also wrapped by pericardium. Hence, the right pulmonary trunk or its branch wrapped by pericardium might be misidentified as the RULV and then ligated by mistake. Secondly, due to the RPA being situated in front of the RULV, even after we divided the right upper lobe artery, the RPA still covered the proximal part of the RULV, which was posed difficulties to surgeons assessing whether middle lobe vein had been secured when stapling the RULV.
Compared with chest CT, three-dimensional reconstruction can help to identify variations more intuitively[8]. Preoperative chest CT is the most important form of imaging examination before lung surgery, but some variations are difficult to identify on axial images[9]. Three-dimensional reconstruction can help to identify variations more intuitively, however, preoperative three-dimensional reconstruction is not adopted as a matter of routine in most medical centers. Hence, it is necessary for thoracic surgeons to have knowledge of pulmonary anatomy variants, make full use of preoperative imaging, and carefully skeletonize and identify anatomic structures during surgery, especially for surgeons operating without the help of preoperative three-dimensional reconstruction.
In conclusion, we reported an extremely rare case of anatomic aberrations in course and location of right pulmonary veins and right preeparterial bronchus occurred simultaneously in one patient. Preoperative three-dimensional reconstruction and making full use of contrasted thin-section CT and is effective for identification of the anatomic variations. Furthermore, careful dissection and identification of anatomic structures can help to confirm the aberration and avoid wrong dissection or vascular injury during operation.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Darbari A S-Editor: Wang LL L-Editor: A P-Editor: Liu JH
| 1. | Otsuki Y, Go T, Chang SS, Matsuura N, Yokomise H. Anomalous right upper lobe pulmonary veins draining posterior to the pulmonary artery. Gen Thorac Cardiovasc Surg. 2019;67:901-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Postmus PE, Kerr KM, Oudkerk M, Senan S, Waller DA, Vansteenkiste J, Escriu C, Peters S; ESMO Guidelines Committee. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28: iv1-iv21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1256] [Cited by in RCA: 1341] [Article Influence: 167.6] [Reference Citation Analysis (0)] |
| 3. | Park S, Park IK, Kim ER, Hwang Y, Lee HJ, Kang CH, Kim YT. Current Trends of Lung Cancer Surgery and Demographic and Social Factors Related to Changes in the Trends of Lung Cancer Surgery: An Analysis of the National Database from 2010 to 2014. Cancer Res Treat. 2017;49:330-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Chassagnon G, Morel B, Carpentier E, Ducou Le Pointe H, Sirinelli D. Tracheobronchial Branching Abnormalities: Lobe-based Classification Scheme. Radiographics: a review publication of the Radiological Society of North America, Inc 2016; 36: 358-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Marom EM, Herndon JE, Kim YH, McAdams HP. Variations in pulmonary venous drainage to the left atrium: implications for radiofrequency ablation. Radiology. 2004;230:824-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 208] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 6. | Ichiki Y, Kakizoe K, Hamatsu T, Suehiro T, Koike M, Tanaka F, Sugimachi K. A rare anomaly of the right superior pulmonary vein: Report of a case. Int J Surg Case Rep. 2017;38:26-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Yurugi Y, Nakamura H, Taniguchi Y, Miwa K, Fujioka S, Haruki T, Takagi Y, Matsuoka Y, Kubouchi Y. Case of thoracoscopic right upper lobectomy for lung cancer with tracheal bronchus and a pulmonary vein variation. Asian J Endosc Surg. 2012;5:93-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Nagashima T, Shimizu K, Ohtaki Y, Obayashi K, Kakegawa S, Nakazawa S, Kamiyoshihara M, Igai H, Takeyoshi I. An analysis of variations in the bronchovascular pattern of the right upper lobe using three-dimensional CT angiography and bronchography. Gen Thorac Cardiovasc Surg. 2015;63:354-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Aokage K, Yoshida J, Ishii G, Matsumura Y, Haruki T, Hishida T, Nagai K. Identification of early t1b lung adenocarcinoma based on thin-section computed tomography findings. J Thorac Oncol. 2013;8:1289-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |