Published online Oct 6, 2021. doi: 10.12998/wjcc.v9.i28.8470
Peer-review started: May 26, 2021
First decision: June 15, 2021
Revised: June 26, 2021
Accepted: July 22, 2021
Article in press: July 22, 2021
Published online: October 6, 2021
Processing time: 124 Days and 20 Hours
Lymphomas are the second most common malignancy of the head and neck. In this region, the vast majority of extranodal lymphomas are located in the palatine tonsil, accounting for about 51%. Tonsillar lymphomas are aggressive tumors with intermediate- or high-grade histology. We here report a case of primary non-Hodgkin’s lymphoma of the palatine tonsil and analyze its ultrasound features.
A 40-year-old man presented with right palatine tonsil swelling for 2 mo after a cold, accompanied by dysphagia, snoring, and suffocation. He had no sore throat, fever, or history of upper respiratory tract infection or tuberculosis. The patient was generally in good health and denied other diseases. He was diagnosed with acute tonsillitis initially and treated with antibiotics for 7 d. However, there was no improvement with the treatment. Tonsil biopsy and ultrasound-guided biopsy of the biggest lymph node of the right neck showed the typical pathology of non-Hodgkin lymphoma.
Primary lymphoma of the tonsils is rare, and its diagnosis is challenging. Ul
Core Tip: Primary lymphoma involving the tonsils is a rare malignancy. We report a 40-year-old man presenting with right palatine tonsil swelling for 2 mo confirmed as a tonsillar lymphoma. Ultrasound can clearly show the features of primary non-Hodg
- Citation: Jiang R, Zhang HM, Wang LY, Pian LP, Cui XW. Ultrasound features of primary non-Hodgkin’s lymphoma of the palatine tonsil: A case report. World J Clin Cases 2021; 9(28): 8470-8475
- URL: https://www.wjgnet.com/2307-8960/full/v9/i28/8470.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i28.8470
Lymphomas of the head and neck arise from lymph nodes as well as extranodal sites. Waldeyer’s ring is the most common anatomical site for extraneous lymphoma in this region (35%-65% of all head and neck lymphomas). Within the Waldeyer’s ring, more than 50% of lymphomas arise in the palatine tonsil[1,2]. Patients with tonsillar lym
A 40-year-old man presented with right palatine tonsil swelling for 2 mo.
The patient presented with right palatine tonsil swelling for 2 mo after a cold, accompanied by dysphagia, sleep snoring, and suffocation. He had no sore throat, fever, or history of upper respiratory tract infection or tuberculosis. He was diagnosed with acute tonsillitis initially and treated with antibiotics for 7 d. However, there was no improvement with the treatment.
The patient was generally in good health and denied other diseases.
The patient did not have any addictions or any significant family history.
Physical examination revealed right-sided tonsillar enlargement (grade III) with surface ulceration, but without pharyngeal portion hyperemia. Several mobile, nontender lymph nodes were palpable in the right swelling submandibular area, with the largest measuring about 5 cm × 7 cm.
Results of biochemical, serologic, and pathologic examinations were all within normal limits. Bone marrow test showed normal erytheroid/myeloid ratio and percentages of myeloid and lymphoid cells.
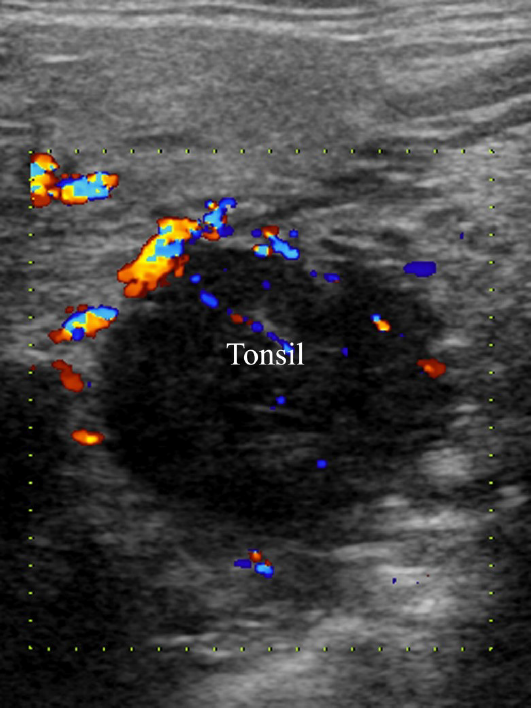
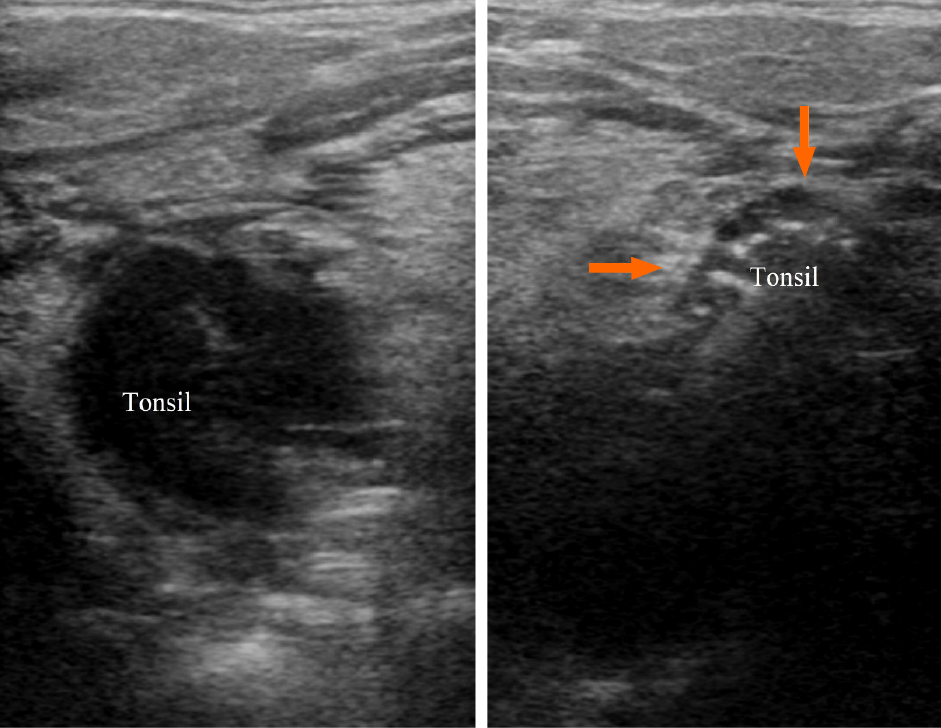
Ultrasound (7-12 MHz linear array transducer, ARIETTA 70, Hitachi Healthcare, Japan) of the right neck and submandibular area demonstrated that the volume of the right tonsil increased significantly. It appeared as a hypoechoic round mass with well-defined margins, homogeneous echo, and rich blood flow signals (Figure 1). In the level IA area of the right neck, multiple enlarged lymph nodes were seen with a clearly defined boundary and hypoechoic internal echoes. They partly integrated without visible echogenic hilar structures and remarkable blood flows could be observed on color Doppler imaging.
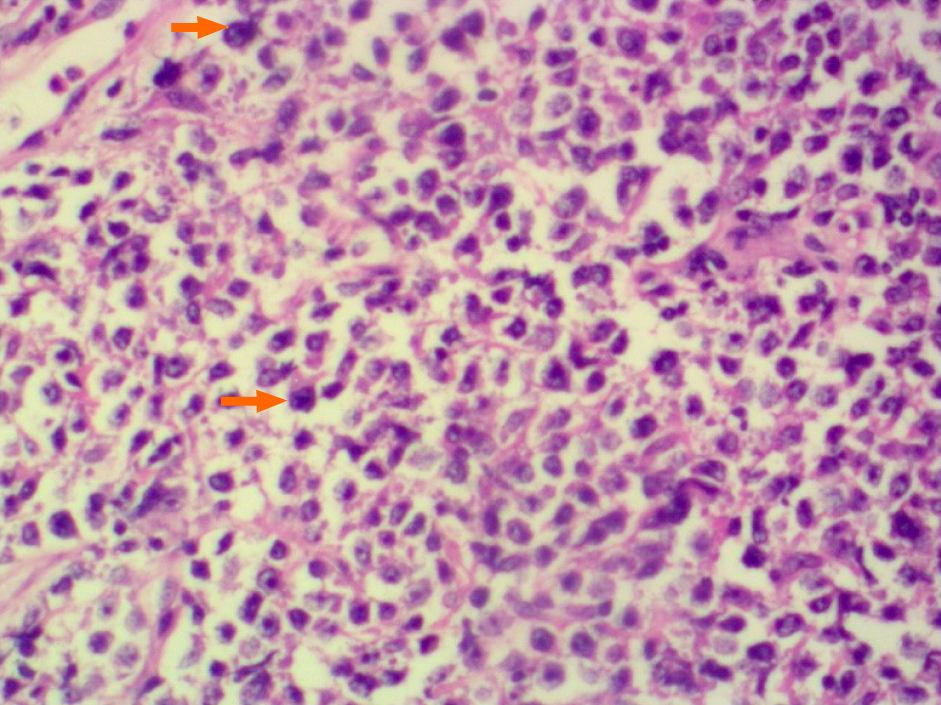
Non-germinal center type diffuse large B cell lymphoma (DLBCL) (Figure 2).
The patient underwent chemotherapy followed by radiotherapy. The chemotherapy regimen included six courses of cyclophosphamide, doxorubicin, vincristine, and prednisone.
At the 6-mo follow-up, there were no signs of any recurrence of the tumor. No further follow-up was available to be reported.
Primary lymphomas are aggressive tumors of lymphoid tissues that are comprised of lymphocytic or reticulocytic derivatives of varying degrees of differentiation[4]. Lymphomas are the second most common malignancy of the head and neck after squamous cell carcinoma[5]. Approximately 2.5% of malignant lymphomas arise in the oral and paraoral region, mainly from Waldeyer’s ring, including the nasopharynx, palatine tonsils, adenoids, lingual tonsils, and the base of the tongue[6,7]. Within the Waldeyer’s ring, more than 50% of lymphomas arise in the palatine tonsil[8,9]. Most lymphomas involving the tonsil are non-Hodgkin’s lymphomas (NHLs), and the most prevalent lymphoma subtype is DLBCL[10,11], which comprises approximately 30% of all NHLs[12]. Tonsillar lymphomas are aggressive tumors of intermediate or high grade, mainly occurring in men with a male/female ratio of 1.3:1.1[1]. However, the disease can affect patients with a wide age range including children[13,14]. The tumors may present in early stage and have a favorable outcome despite a high incidence of aggressive histology. Common symptoms include mass in the throat, dysphagia, odynophagia, and sore throat, some of which are similar to those of tonsillitis. Only 25% of patients have systemic symptoms in head and neck lymphomas[2]. Due to the similar clinical presentations, differentiation of primary tonsil lymphoma from ton
Currently, ultrasound is not routinely used for the diagnosis of oropharyngeal diseases. Coquia et al[16] obtained clear images of tonsils on B mode and color Doppler ultrasound. Normal tonsils are presented on ultrasound as homogeneously ovoid echogenic soft tissue with stripes and internal linear echogenicity. Posterior to the palatine tonsil is the pharyngeal constrictor, which is hypoechoic on the ultrasound. Color Doppler ultrasound can show the multiple vessels of the external carotid artery supplying the palatine tonsil.
According to our observations, the characteristics of primary tonsil lymphomas are as follows: Spherical tonsils with significantly increased volume; hypoechoic struc
Contrast-enhanced computed tomography (CT) and positron emission tomogra
Primary lymphoma involving the tonsils is a rare malignancy and it is difficult for clinicians to make a correct diagnosis timely based on the physical examination alone. Currently, multiple imaging modalities have been used in the differential diagnosis of oropharyngeal diseases. Ultrasound can clearly show the features of primary lym
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Machado P S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yuan YY
| 1. | Mohammadianpanah M, Daneshbod Y, Ramzi M, Hamidizadeh N, Dehghani SJ, Bidouei F, Khademi B, Ahmadloo N, Ansari M, Omidvari S, Mosalaei A, Dehghani M. Primary tonsillar lymphomas according to the new World Health Organization classification: to report 87 cases and literature review and analysis. Ann Hematol. 2010;89:993-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (2)] |
| 2. | Cabeçadas J, Martinez D, Andreasen S, Mikkelsen LH, Molina-Urra R, Hall D, Strojan P, Hellquist H, Bandello F, Rinaldo A, Cardesa A, Ferlito A. Lymphomas of the head and neck region: an update. Virchows Arch. 2019;474:649-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Kolokotronis A, Konstantinou N, Christakis I, Papadimitriou P, Matiakis A, Zaraboukas T, Antoniades D. Localized B-cell non-Hodgkin's lymphoma of oral cavity and maxillofacial region: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Tankwal M, Munjal V. Primary isolated nonhogkin's loymphoma of the tonsil -a case report. Indian J Otolaryngol Head Neck Surg. 1999;52:68-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Epstein JB, Epstein JD, Le ND, Gorsky M. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:519-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 156] [Article Influence: 6.5] [Reference Citation Analysis (1)] |
| 6. | Aiken AH, Glastonbury C. Imaging Hodgkin and non-Hodgkin lymphoma in the head and neck. Radiol Clin North Am. 2008;46:363-378, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 7. | Rayess HM, Nissan M, Gupta A, Carron MA, Raza SN, Fribley AM. Oropharyngeal lymphoma: A US population based analysis. Oral Oncol. 2017;73:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | ROSENBERG SA, DIAMOND HD, JASLOWITZ B, CRAVER LF. Lymphosarcoma: a review of 1269 cases. Medicine (Baltimore). 1961;40:31-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 749] [Cited by in RCA: 657] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 9. | Solomides CC, Miller AS, Christman RA, Talwar J, Simpkins H. Lymphomas of the oral cavity: histology, immunologic type, and incidence of Epstein-Barr virus infection. Hum Pathol. 2002;33:153-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Hart S, Horsman JM, Radstone CR, Hancock H, Goepel JR, Hancock BW. Localised extranodal lymphoma of the head and neck: the Sheffield Lymphoma Group experience (1971-2000). Clin Oncol (R Coll Radiol). 2004;16:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Gao DL, Fu QQ, Zhang TT, Li SL, Pan Y, Zhai QL. [Analysis of Clinicopathological Characteristics and Prognosis of 112 Patients with Primary Waldeyer's Ring Lymphoma]. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2015;23:1301-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Lee YY, Van Tassel P, Nauert C, North LB, Jing BS. Lymphomas of the head and neck: CT findings at initial presentation. AJR Am J Roentgenol. 1987;149:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Bouayed K, Bousfiha AA, Madani A, Zafad S, Harif M, Benchekroun S. [Unilateral tonsillar enlargement in children: thinking about lymphoma]. Arch Pediatr. 2006;13:1460-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Cuestas G, Martínez Font A, Demarchi MV, Martínez Corvalán MP, García Rivello H, Morandi A, Razetti J, Boccio C. [Palatine tonsil lymphoma in children with tonsillar asymmetry. Case report]. Arch Argent Pediatr. 2015;113:e219-e222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Kallel S, Hadj Taieb H, Makni S, Ghorbel A. Lymphoma presenting as a peritonsillar abscess. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Coquia SF, Hamper UM, Holman ME, DeJong MR, Subramaniam RM, Aygun N, Fakhry C. Visualization of the Oropharynx With Transcervical Ultrasound. AJR Am J Roentgenol. 2015;205:1288-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |