Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.3979
Peer-review started: January 10, 2021
First decision: February 12, 2021
Revised: February 19, 2021
Accepted: March 9, 2021
Article in press: March 9, 2021
Published online: June 6, 2021
Processing time: 123 Days and 19.3 Hours
Obturator dislocation is a rare type of hip dislocation, accounting for about 2%-5% of all hip dislocations. The occurrence of old unreduced obturator dislocation is even more infrequent, with only 17 cases reported in nine studies, most of which were from the 1950s to 1980s in developing countries.
A 38-year-old woman from Hunan Province, China presented with stiffness of the left hip in abduction, flexion, and external rotation after falling from a 2-meter-tall tree onto her left knee 1.5 mo prior. Pelvic radiograph and computed tomography revealed obturator dislocation of the left hip accompanied by impaction fracture at the superolateral aspect of the left femoral head without associated acetabulum fracture. Open reduction was performed, resulting in restoration of the concentric alignment of the left hip. After surgery, 6-wk skin traction was applied and the patient was kept in bed for an additional 2 wk. At 3 mo after surgery, the patient reported experiencing some pain, which did not affect the function of the affected limb, and some movement restriction but no abduction deformity or claudication was present. An X-ray showed that the left hip was homocentric, and there was no sign of posttraumatic arthritis or avascular necrosis.
Open reduction may be an effective treatment strategy for the rare condition of old unreduced obturator dislocation with short neglect time.
Core Tip: Obturator dislocation is a rare type of hip dislocation, accounting for about 2%-5% of all hip dislocations, and there are even fewer cases of old unreduced obturator dislocations. We present a very rare case of old unreduced obturator dislocation treated by open reduction. The patient underwent open reduction via the Smith-Peterson approach rather than total hip arthroplasty because of her low income. At the 3 mo follow-up, the patient reported experiencing some pain, which did not affect function, and some movement restriction but no abduction deformity or claudication was present.
- Citation: Li WZ, Wang JJ, Ni JD, Song DY, Ding ML, Huang J, He GX. Old unreduced obturator dislocation of the hip: A case report. World J Clin Cases 2021; 9(16): 3979-3987
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/3979.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.3979
Only 5%-13% of all hip dislocations are traumatic anterior dislocations, which occur less frequently than posterior hip dislocations[1-5]. According to Epstein’s classification, anterior dislocation is divided into pubic and obturator dislocation based on whether the femoral head is displaced superiorly or inferiorly[6]. Obturator dislocation is a rare type of hip dislocation, accounting for about 2%-5% of all hip dislocations[7]. The occurrence of old unreduced obturator dislocation of the hip is even more infrequent, with only 17 cases reported in nine studies[8-16], most of which were from the 1950s to 1980s in developing countries. There has been just one reported case of old unreduced obturator dislocation of the hip in an adult in the last 25 years.
We report herein a very rare case of old unreduced traumatic obturator hip disloca
A 38-year-old woman from Hunan Province, China presented with stiffness of the left hip in abduction, flexion, and external rotation after falling from a 2-meter-tall tree on her left knee 1.5 mo prior.
Pain and swelling of the left knee, and fixed abduction and flexion of the left hip occurred immediately after falling. Rather than going to the hospital, the patient applied a traditional Chinese medicine herbal ointment of unknown composition. The left knee improved within 2 wk but the left hip remained stiff, so she could only walk with the aid of a stick. Due to the lack of improvement in the left hip, an X-ray was performed at a local clinic at 1.5 mo after the fall, which showed dislocation of her left hip. She was subsequently transferred to our hospital.
The patient had a free previous medical history.
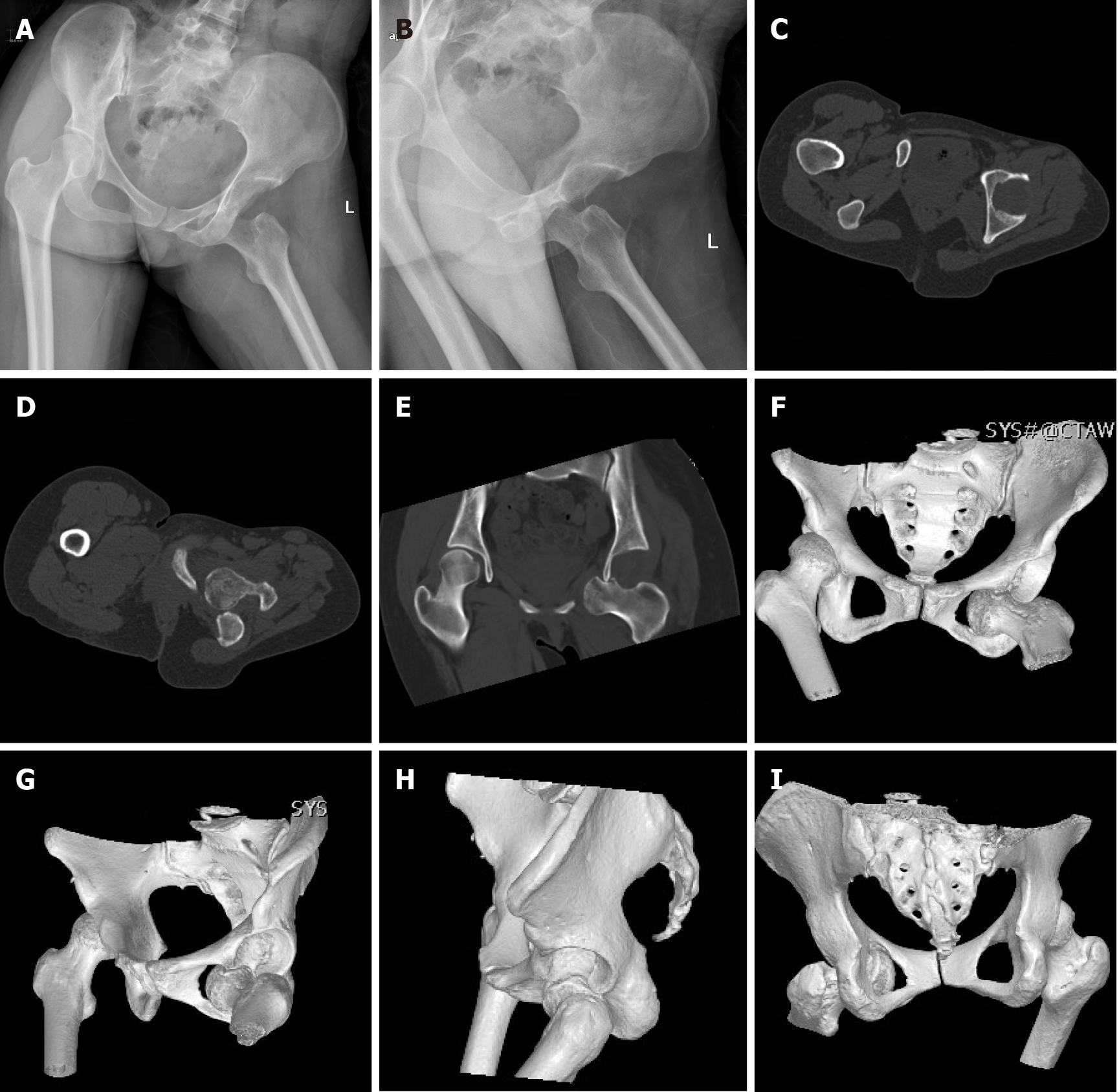
The patient experienced compensatory scoliosis to the left, and the pelvis was lower on the left side. The left hip showed elastic fixation in 40° of flexion, 45° of abduction, and 30° of external rotation (Figure 1). The pressure point was examined near the hip joint, and the range of motion of the hip was limited. The Trendelenburg test was positive. The patient could only walk with the aid of a stick and was not able to load any weight on her left leg. The neurovascular status of the left leg was good.
Radiographs at admission revealed dislocation of the left hip and femoral head impaction fracture without any injury of the left knee (Figure 2A and B). Computed tomography showed obturator hip dislocation. The femoral head shifted to the inferior and anterior side of the obturator foramen, with impaction fracture at the superolateral aspect of the left femoral head without associated fracture of the acetabulum (Figure 2C-I).
The treatment options for old unreduced obturator dislocation of the left hip and impaction fracture of the ipsilateral femoral head were discussed with the patient. She decided to undergo open reduction only, and refused further intervention such as bone grafting or total hip arthroplasty because of her low income, even though she was informed that the incidence of posttraumatic arthritis and avascular necrosis would be high with treatment by delayed reduction alone.
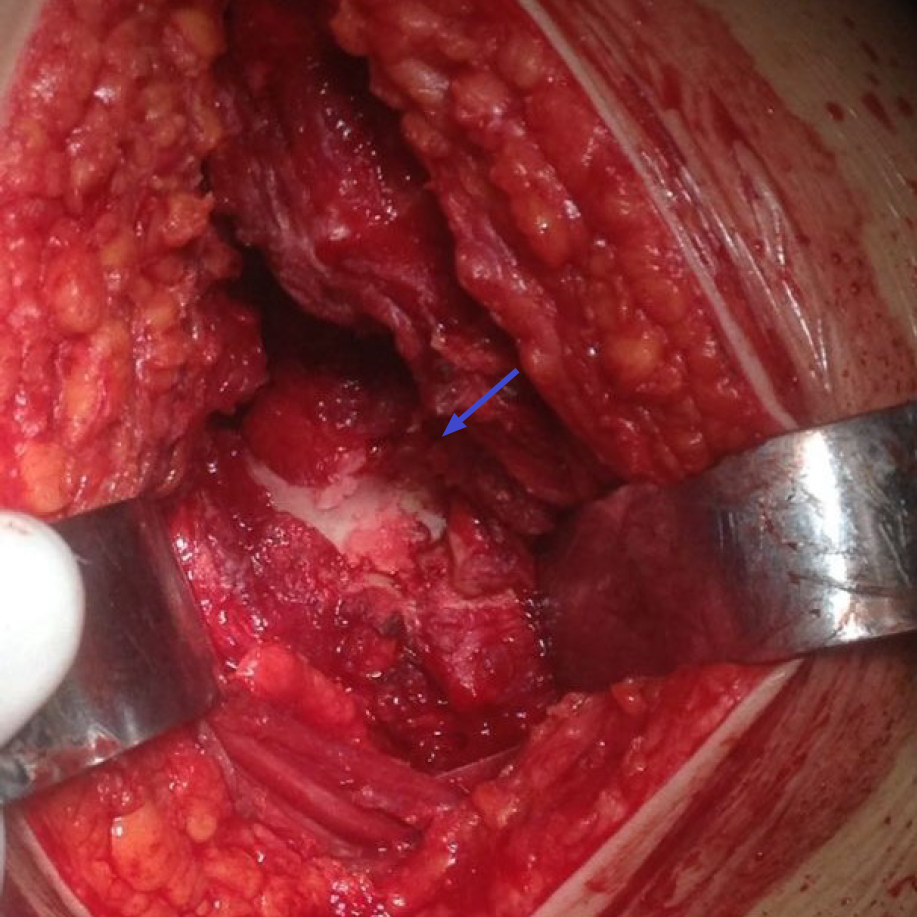
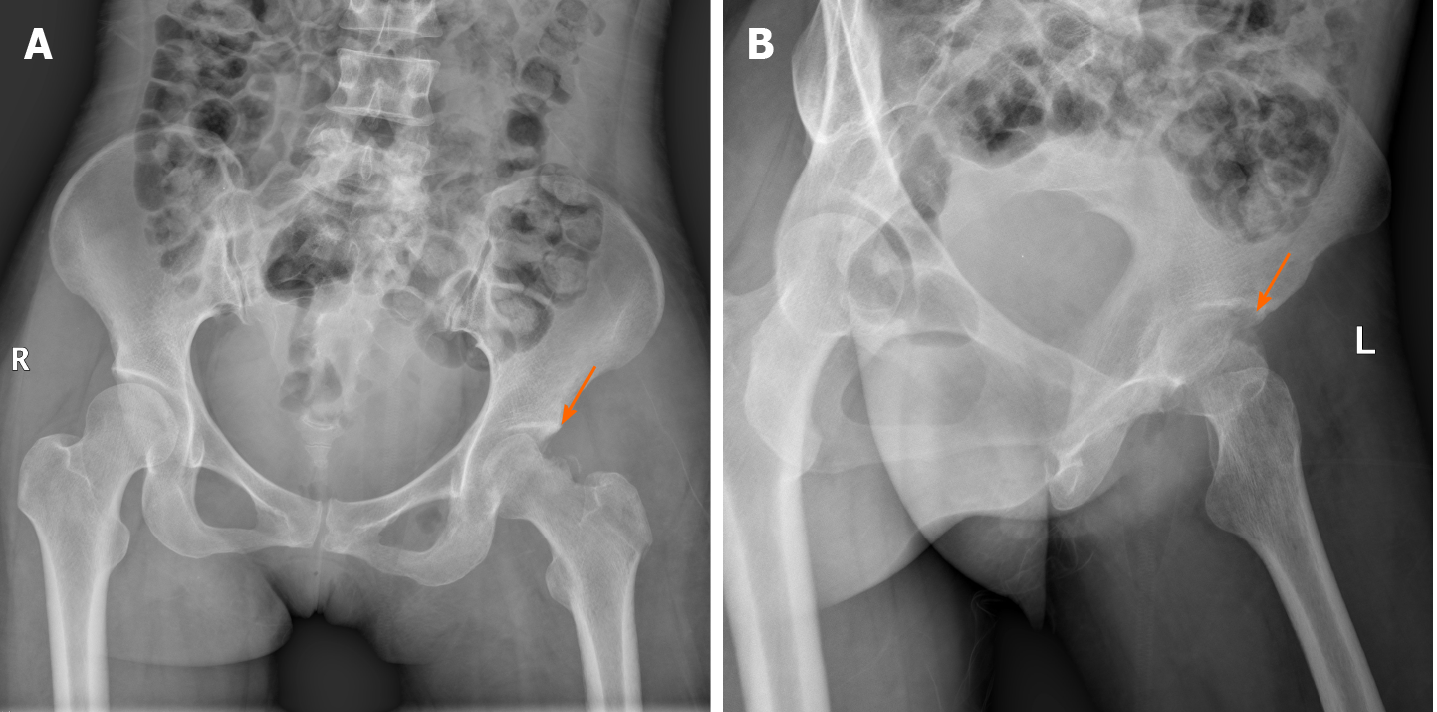
The surgery was performed 3 d after admission. After general anesthesia, the patient was placed in the supine position on a radiolucent operating table and the left leg was prepared and draped freely. Open reduction for obturator hip dislocation was performed using the Smith-Peterson approach. Intraoperatively, the femoral head was locked with the superior ramus of the pubis and embedded in the pelvis, so a subtrochanteric Schanz screw parallel to the femoral neck was used as a joystick to help unlock and reduce the femoral head. The acetabulum was completely filled with fibrous tissue, which was separated and removed. After reduction, the anterosuperior aspect of the femoral head showed collapse and articular damage (Figure 3). The hip was completely stabilized without re-dislocation in a full passive range of motion. Intraoperative fluoroscopy was used to evaluate the concentric alignment of the left hip. The hip anterior capsule, subcutaneous tissue, and skin were sutured sequentially. The suction drain was removed 24 h after surgery. After surgery, 6-wk skin traction was applied and the patient was kept in bed for an additional 2 wk. Prophylactic cefazolin was used from 30 min before surgery to 24 h postoperatively. Oral rivaroxaban was applied for 6 wk to prevent deep venous thromboembolism. The patient started toe-touch weight-bearing with crutches 2 mo after surgery. Postoperative X-rays showed satisfactory reduction of the hip (Figure 4).
Old unreduced traumatic obturator dislocation accompanied by impaction fracture at the superolateral aspect of the femoral head.
Open reduction via the Smith-Peterson approach.
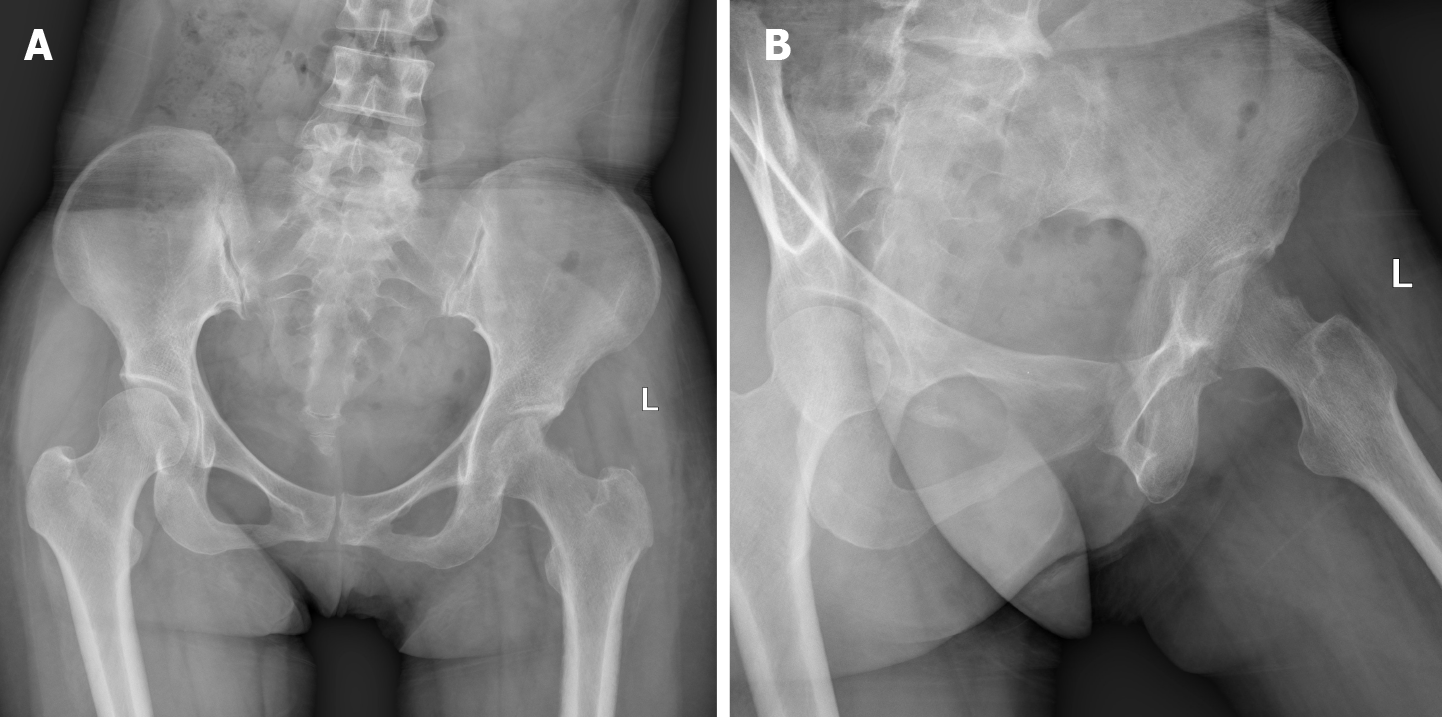
The 3-mo follow-up revealed a fair outcome according to Garret’s modification of the Thompson and Epstein classification[17], indicative of some pain that did not affect the function of the affected limb, and some movement restriction but no abduction deformity or claudication. An X-ray showed that the left hip was homocentric, and there was no sign of posttraumatic arthritis or avascular necrosis (Figure 5). The patient refused further follow-up because she could not afford additional treatment, even though she was informed that posttraumatic arthritis and avascular necrosis would occur and seriously affect her daily life.
Although the accurate definition of old unreduced hip dislocation is not recognized, any hip dislocation lasting for more than 72 h is considered “old” or “neglected”[18]. Due to poorly organized health services and inadequate means to diagnose and treat injuries, the majority of reports on old unreduced hip dislocations are from developing countries[19]. Little has been reported about old unreduced hip dislocations, and old unreduced obturator dislocations have been even less studied. To the best of our knowledge, only 17 cases of old unreduced obturator dislocation in nine studies have been reported, including just one case reported in an adult in the last 25 years (Table 1).
| No. | Ref. | No. of cases | Year | Country | Sex | Age | Delay in securing proper treatment (mo) | Treatment | Follow-up in (mo) | Outcome |
| 1 | Mikhail[8] | 1 | 1956 | Saudi Arabia | Male | 24 | 12 | Open reduction | 0.5 | Walking with crutches |
| 2 | Hamada[9] | 3 | 1957 | Egypt | Case 1: Female | 24 | 144 | Osteotomy of femoral neck | No follow-up | Unknown |
| Case 2: Male | 12 | 12 | Osteotomy of femoral neck | No follow-up | Unknown | |||||
| Case 3: Female | 9 | 5 | Osteotomy of femoral neck | No follow-up | Unknown | |||||
| 3 | Aggarwal and Singh[10] | 6 | 1967 | India | Case 1: Male | 45 | 12 | Trochanteric osteotomy | 48 | Fixed hip in flexion of 25°. Back to his original occupation. |
| Case 2: Male | 55 | 9 | Trochanteric osteotomy | 39 | Fixed straight hip. Walking with crutches | |||||
| Case 3: Male | 20 | 5 | Trochanteric osteotomy | 25 | Fixed hip in flexion of 15°. Walking without support | |||||
| Case 4: Male | 22 | 3 | Trochanteric osteotomy | 11 | Fixed hip in flexion of 20°. Working as a farmer again | |||||
| Case 5: Male | 35 | 11 | Open reduction | 11 | A painful hip with limited movements | |||||
| Case 6: Male | 28 | 3 | Trochanteric osteotomy | 10 | Fixed hip in flexion of 15°. Able to do his routine work | |||||
| 4 | Scadden and Dennyson[11] | 1 | 1978 | South Africa | Female | 16 | 1 | Open reduction | 12 | Walking with a slight limp but without any pain. No fixed deformities |
| 5 | Younge and Lifeso[12] | 1 | 1988 | Saudi Arabia | Male | 16 | 72 | Open reduction first, and then hip fusion | 31 | Walking no better than before surgery with recurrent flexion contracture |
| 6 | Nagi et al[13] | 2 | 1992 | India | Case 1: Male | 35 | 7.5 | Modified Girdlestone hip arthroplasty | 25 | 2.5 cm shortening. Full range of flexion and rotations with limited abduction of 20°. Some pain present on prolonged walking |
| Case 2: Male | 28 | 9.5 | Modified Girdlestone hip arthroplasty | 33 | 3 cm shortening. Full range of flexion and rotations with limited abduction of 20°. Some pain present on prolonged walking | |||||
| 7 | Pathania et al[14] | 1 | 1995 | India | Male | 16 | 4 | Open reduction | 11 | Almost full pain-free movement of hip |
| 8 | Albayrak et al[15] | 1 | 2006 | Turkey | Male | 5 | 1.5 | Open reduction | 12 | No complaints and no functional restriction |
| 9 | Pankaj et al[16] | 1 | 2011 | India | Male | 33 | 6 | Total hip arthroplasty | 18 | Walking unsupported without symptom |
The hip is a stable joint, and the weakest point is the posteroinferior capsule. Therefore, anterior hip dislocations are more infrequent than posterior dislocations[20], accounting for up to 13% of all hip dislocations[21]. Anterior dislocation occurs as a result of a force acting on an abducted hip joint, which is then flexed and externally rotated to dislocate the femoral head forward[22,23]. The eventual position of the femoral head is determined by the degree of flexion at the time of injury. According to Epstein’s classification, the anterior dislocation can be divided into pubic (type I) and obturator (type II) dislocation[2]. Obturator dislocation, which represents 2%-5% of all hip dislocations[7], is the most rare type of hip dislocation and is usually caused by falls[22]. As was the case in our report, obturator dislocation occurs when a force is transmitted from the knee to the femoral head while the limb is in a position of extreme flexion, abduction, and lateral rotation.
Epstein and Wiss[6] further subdivided anterior hip dislocation into three subtypes based on the location of the incidental fractures, of which type B is accompanied by fractures of the femoral head and/or neck. Brumback et al[24,25] also proposed an improved classification of fracture dislocations of the hip to emphasize the importance of individualized therapy, but it does not appear to have prognostic potential. Unreduced hip dislocation is classified into four types by modified Garret’s classification according to the duration between injury and diagnosis in the hospital, where the neglect time for type I is 3 d to 3 wk, type II is 3 wk to 3 mo, type III is 3 mo to 12 mo, and type IV is more than 12 mo[19].
Little has been reported about old unreduced traumatic hip dislocations, and old unreduced obturator dislocation has been even less studied. Due to the infrequency of old unreduced traumatic hip dislocations, treatment options and outcome measures are scarce, based on small case series. The options in the literature include closed reduction, heavy traction and abduction, open reduction, osteotomy, and hip fusion to arthroplasty (Table 1).
Closed reduction has been less applied than open reduction due to the difficulty of reduction, which is usually proportional to the delay in securing proper treatment. Pai[19] reported 3 of 29 old unreduced anterior dislocations but did not define if they were obturator. Closed reduction was achieved in modified Garrett’s type I dislocation and heavy traction and abduction failed in modified Garrett’s type III dislocation, which then was treated by open reduction. The outcomes of both patients were satisfactory. Another patient underwent a Girdlestone hip arthroplasty but with an unsatisfactory outcome.
Mikhail[8], Aggarwal and Singh[10], Scadden and Dennyson[11], Younge and Lifeso[12], Pathania et al[14], Albayrak et al[15], and Pankaj et al[16] reported seven old unreduced obturator dislocations treated by open reduction. Four of the seven patients made a good recovery and were pain-free for routine work, two had fair outcomes with slight limp and some pain, and one had a poor outcome and needed hip fusion. There was no significant difference in age or gender. However, the neglect time of patients with good outcomes was up to 6 mo, which was much shorter than those with fair or bad outcomes, similar to many studies showing that neglect time is an important prognostic factor[19,21,26].
Osteotomy of the femoral neck or trochanter for the treatment of old unreduced obturator dislocation was reported in studies by Hamada[9] and Aggarwal and Singh[10]. All patients had fixed hips with various degrees of flexion but without any abduction, accompanied by little pain that could be tolerable in daily life. Nagi et al[13] reported two patients with unreduced obturator dislocations, who received a modified Girdlestone arthroplasty by taking a subcapital osteotomy to keep the possibility of total hip replacement at a later stage. Both patients had shortened legs and a full range of flexion and rotation with limited abduction. Some pain was reported with prolonged walking at the final follow-up. Total hip arthroplasty was only used for one 33-year-old male patient with unreduced obturator dislocated hip, who presented to the hospital with complaints of deformity of the right hip following a road traffic accident 6 mo prior[16]. At the 18-mo follow-up, he could walk unsupported without any symptoms.
Based on these limited studies, treatment for delayed unreduced dislocation has been somewhat empirical and no method has been proven to be superior. We strongly recommend total hip arthroplasty for our patient because of the high incidence of further complications, such as avascular necrosis, especially along with indentation fracture of the femoral head. The incidence of femoral head necrosis is closely related to the duration between injury and reduction, and is up to 50% if reduction is implemented more than 6 h after injury[27]. Femoral head indentation fractures have been presented to occur in 15% to 55% of patients after anterior hip dislocation[2,28]. Patients with femoral head fractures deeper than 4 mm reportedly have a poor prognosis, which is thought to predispose for posttraumatic arthritis in 88%[21]. However, our patient refused any further treatment except reduction due to economic reasons.
There is no consensus on the management of hip dislocation after either open or closed reduction. Post-reduction immobilization using traction or cast and non-weight-bearing were recommended for the prevention of femoral head necrosis[5,26]. For old unreduced dislocation, traction is not only to reduce the risk of avascular necrosis, but also to ameliorate soft tissue contracture around the hip joint. The time of traction and non-weight-bearing following hip reduction is highly variable, ranging from 1 wk to 6 wk in traction and 2 wk to 12 wk in non-weight-bearing [4,5,7,8,11,14,18,20,22,26]. Although a few studies in recent years have shown that traction did not change the risk of avascular necrosis and prognosis[5], 6-wk skin traction and totally 8-wk non-weight-bearing were applied for our patient.
Our patient was living in a rural area of central China that is remote and has a nearly inaccessible mountaintop, so her last follow-up occurred 3 mo after surgery. The patient reported some pain that did not affect the function of the affected limb, and some movement restriction, but no abduction deformity or claudication was present. Nevertheless, late complications including traumatic arthritis and femoral head necrosis cannot be ruled out as the follow-up period has only been 3 mo.
We report an extremely rare case of old unreduced traumatic obturator hip dislocation accompanied by impaction fracture at the superolateral aspect of the femoral head without associated fracture of the acetabulum in a 38-year-old woman. Treatment for old unreduced dislocation has been somewhat empirical and no method has been proven to be superior. Open reduction may be an effective option for rare old unreduced obturator dislocation with short neglect time.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Hunan Province Association of Rehabilitation Medicine; and Hunan Health Service Industry Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kahila A S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am. 1951;33-A:746-78; passim. [PubMed] |
| 2. | Rancan M, Esser MP, Kossmann T. Irreducible traumatic obturator hip dislocation with subcapital indentation fracture of the femoral neck: a case report. J Trauma. 2007;62:E4-E6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Lima LC, do Nascimento RA, de Almeida VM, Façanha Filho FA. Epidemiology of traumatic hip dislocation in patients treated in Ceará, Brazil. Acta Ortop Bras. 2014;22:151-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Young S, Banza L. Neglected traumatic anterior dislocation of the hip. Open reduction using the Bernese trochanter flip approach - a case report. Acta Orthop. 2017;88:348-350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Syam K, Saibaba B, Aggarwal S, Santhanam S, Palanisamy G. Update review and clinical presentation in adult inferior dislocation of hip. Eur J Orthop Surg Traumatol. 2017;27:1039-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Epstein HC, Wiss DA. Traumatic anterior dislocation of the hip. Orthopedics. 1985;8:130, 132-134. [PubMed] |
| 7. | Ismael S, Vora J, Thomas P. Adult Traumatic Inferior Hip Dislocation: Rare Case Ended with Open Reduction. J Orthop Case Rep. 2017;7:101-104. [PubMed] |
| 8. | Mikhail IK. Unreduced traumatic dislocation of the hip. J Bone Joint Surg Br. 1956;38-B:899-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Hamada G. Unreduced anterior dislocation of the hip. J Bone Joint Surg Br. 1957;39-B:471-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 10. | Aggarwal ND, Singh H. Unreduced anterior dislocation of the hip. Report of seven cases. J Bone Joint Surg Br. 1967;49:288-292. [PubMed] |
| 11. | Scadden WJ, Dennyson WG. Unreduced obturator dislocation of the hip. A case report. S Afr Med J. 1978;53:601-602. [PubMed] |
| 12. | Younge D, Lifeso R. Unreduced anterior dislocation of the hip in a child. J Pediatr Orthop. 1988;8:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Nagi ON, Dhillon MS, Gill SS. Chronically unreduced traumatic anterior dislocation of the hip: a report of four cases. J Orthop Trauma. 1992;6:433-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Pathania VP, Kumar A, Ghosh D. Unreduced Anterior Dislocation Of The Hip: A Case Report. Med J Armed Forces India. 1995;51:72-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Albayrak M, Doğan A, Sürel YB. [Traumatic obturator hip dislocation in a five-year-old boy: open reduction after a six-week delay in diagnosis]. Acta Orthop Traumatol Turc. 2006;40:260-263. [PubMed] |
| 16. | Pankaj A, Sharma M, Kochar V, Naik VA. Neglected, locked, obturator type of inferior hip dislocation treated by total hip arthroplasty. Arch Orthop Trauma Surg. 2011;131:443-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Sulaiman AR, Munajat I, Mohd FE. Outcome of traumatic hip dislocation in children. J Pediatr Orthop B. 2013;22:557-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Mootha AK, Mogali KV. A Rare Case of Neglected Traumatic Anterior Dislocation of Hip in a Child. J Orthop Case Rep. 2016;6:40-42. [PubMed] |
| 19. | Pai VS. The management of unreduced traumatic dislocation of the hip in developing countries. Int Orthop. 1992;16:136-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Duygulu F, Karaoglu S, Kabak S, Karahan OI. Bilateral obturator dislocation of the hip. Arch Orthop Trauma Surg. 2003;123:36-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Yaari LS, Kadar A, Shemesh S, Haviv B, Leslie MP. Medium-term outcome and classification of traumatic anterior hip dislocations. Hip Int. 2020;1120700020918868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Karaarslan AA, Acar N, Karci T, Sesli E. A Bilateral Traumatic Hip Obturator Dislocation. Case Rep Orthop. 2016;2016:3145343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Jain S, Haughton BA, Grogan RJ. Inferior dislocation of the hip: a case report and literature review. J Orthop Surg (Hong Kong). 2015;23:123-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Brumback RJ, Kenzora JE, Levitt LE, Burgess AR, Poka A. Fractures of the femoral head. Hip. 1987;181-206. [PubMed] |
| 25. | Brumback RJ, Holt ES, McBride MS, Poka A, Bathon GH, Burgess AR. Acetabular depression fracture accompanying posterior fracture dislocation of the hip. J Orthop Trauma. 1990;4:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Sahin V, Karakaş ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: a long-term follow-up study. J Trauma. 2003;54:520-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 157] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 27. | Tekin AÇ, Çabuk H, Büyükkurt CD, Dedeoğlu SS, İmren Y, Gürbüz H. Inferior hip dislocation after falling from height: A case report. Int J Surg Case Rep. 2016;22:62-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Goddard NJ. Classification of traumatic hip dislocation. Clin Orthop Relat Res. 2000;11-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |