Published online Apr 16, 2021. doi: 10.12998/wjcc.v9.i11.2688
Peer-review started: December 18, 2020
First decision: January 17, 2021
Revised: January 18, 2021
Accepted: February 1, 2021
Article in press: February 1, 2021
Published online: April 16, 2021
Processing time: 102 Days and 1 Hours
Abnormalities in the melanocortin receptor 4 (MC4R) gene often lead to obesity, but are rarely associated with other conditions such as epilepsy and sleep disorder.
Here, we present a case of a male obese child with a heterozygous variant in MC4R (c.494G>A, p.Arg165Gln) inherited from his father, who presented with disordered sleep and abnormal facial movements. Examination through melatonin rhythm testing and electroencephalography led to a diagnosis of sleep disorder and epilepsy, as his melatonin rhythm was markedly distorted and the electroencephalography revealed epileptic discharges. He received treatment with an antiepileptic drug; however, the therapy was ineffective and the sleep disorder appeared to be deteriorating. Subsequently, we initiated adjuvant treatment with melatonin. Upon re-examination, his body mass index had decreased, the sleep disturbance had resolved, and his seizures were well controlled. Electro-encephalography review was normal, and a typical melatonin rhythm was restored.
We concluded that, in addition to causing obesity, abnormalities in the MC4R gene may contribute to the development of sleep disorders and epilepsy, and that melatonin can be used as an adjuvant therapy to alleviate these symptoms.
Core Tip: Numerous reports suggest that abnormalities of the melanocortin receptor 4 (MC4R) gene may cause obesity, but are rarely associated with other conditions. The case presented in our manuscript involved a male obese child with a heterozygous variant in MC4R (c.494G>A, p.Arg165Gln) inherited from his father, who presented with epilepsy, sleep disordered and his melatonin rhythm was markedly distorted. This is the first report of the combination of these symptoms in a patient with an MC4R variant. Antiepileptic drug was ineffective and the sleep disorder appeared to be deteriorating. The use of melatonin relieved all his symptoms, and even the electroencephalography review was normal, and a typical melatonin rhythm was restored. We hope that our experience can help the early diagnosis and treatment of this condition.
- Citation: Ge WR, Wan L, Yang G. Melatonin for an obese child with MC4R gene variant showing epilepsy and disordered sleep: A case report. World J Clin Cases 2021; 9(11): 2688-2695
- URL: https://www.wjgnet.com/2307-8960/full/v9/i11/2688.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i11.2688
Melanocortin receptor 4 (MC4R), a key contributor to the regulation of energy balance and body weight in mammals, influences energy metabolism by sensing external signals that regulating appetite, as well as the activity of the autonomic nervous system and nervous endocrine system[1]. Numerous reports suggest that abnormalities of the MC4R gene may cause obesity[1-3]. Furthermore, MC4R is the receptor for melatonin; some studies have demonstrated that melatonin can act on the MC4R in the hypothalamus to generate a physiological sensation of satiety, thereby influencing appetite[4]. Melatonin is also involved in sleep and epilepsy; patients with epilepsy are characterized by an increased phase shift of melatonin release. Melatonin can improve sleep disorder in children with epilepsy, resulting in statistically significant decreases in sleep latency and wakefulness after sleep onset[5,6].
Here, we present a case of a clinically obese child with a variant in the MC4R gene, who had abnormal melatonin rhythms, sleep disturbances, and seizures.
A 7-year-old male patient with the chief complaint of obesity, seizure, and sleep disorder.
The case was a 7-year-old male patient, who presented in June 2018 with pain in both lower extremities, with no obvious cause. On presentation, the pain in the extremities was dull, mainly in the patient’s calves, and did not significantly differ before and after exercise. He did not have walking difficulties and his gait was normal. He attended his local hospital, where he was diagnosed with “growth pain; malnutrition,” and was prescribed an orally administered live Bifidobacterium preparation and calcium. His food intake increased substantially, accompanied by a marked increase in weight. Nighttime sleep, characterized by ease of waking and nightmares (2-3 times/night) and accompanied by physical movements, was simultaneously disordered. Moreover, he did not fall asleep until late at night (23:00 h) and awoke early in the morning (06:00 h), and took excessive naps during the daytime (4-5 times/d). Nevertheless, the lower extremity pain had improved, whereas he complained of gradual weakness of both lower limbs, fatigue, and activity intolerance, which was noticeable when he descended the stairs. He also had intermittent dizziness, with oculogyric crisis and tongue extension, which subsided after approximately 1-2 min, without losing consciousness. The patient was unaware of the oculogyric crisis and tongue extension. His cognition did not show an abnormality, tests of Wechsler Intelligence Scale for Children were normal (IQ: 103) and he continued to attend school normally.
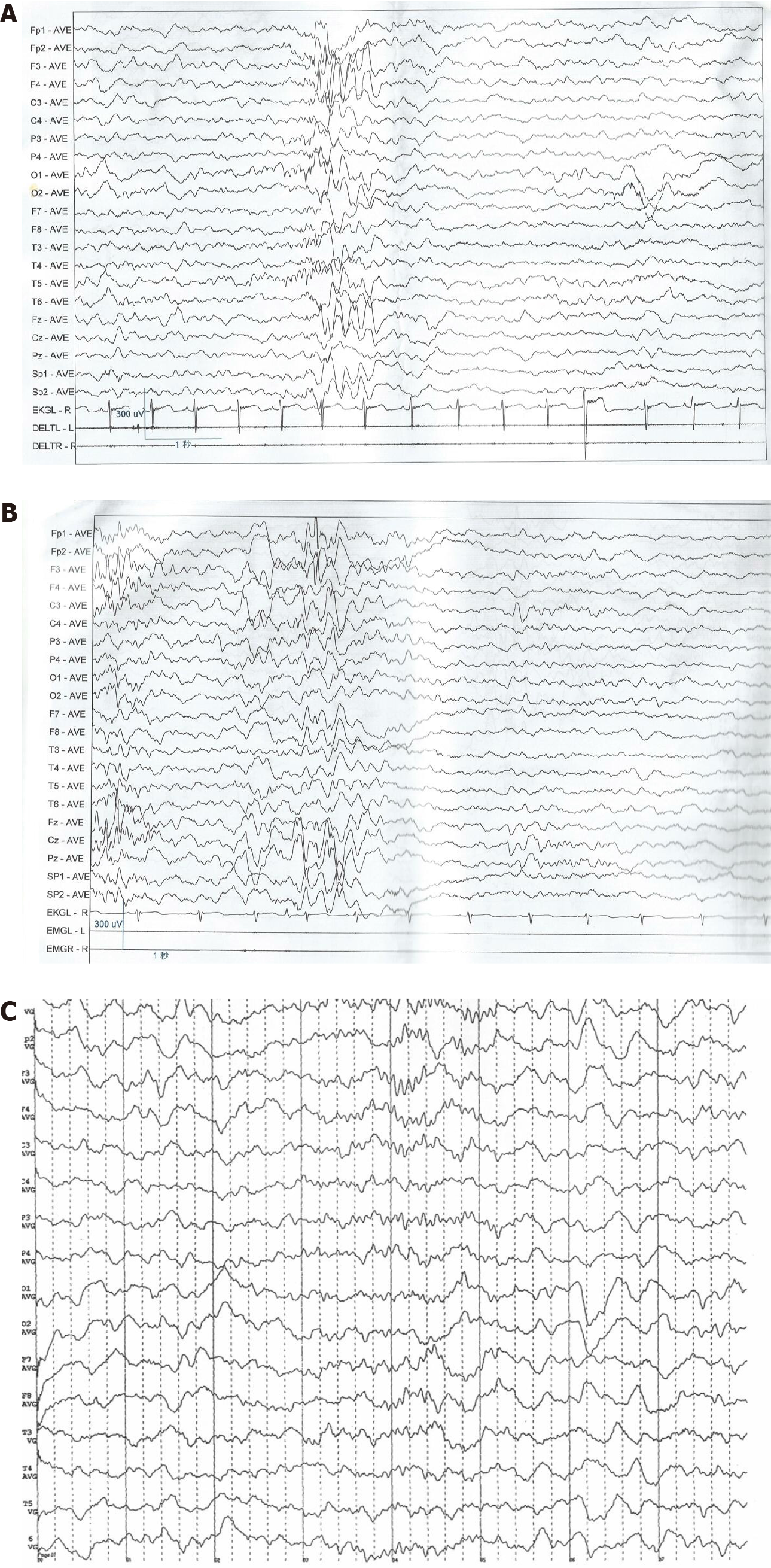
He was first admitted to our hospital in August 2018. Examination through electroencephalography (EEG) revealed a small number of paroxysmal high-wave amplitude (4-5 Hz) slow waves during waking and sleep periods; spikes were visible in the left front and central areas (Figure 1A). Magnetic resonance imaging of the brain showed normal findings. His height and weight were 125 cm and 36.4 kg, respectively, with a Rohrer index of 186.37 (Rohrer index > 156 indicates obesity; 140-156 is overweight); he was diagnosed with obesity and epilepsy. Levetiracetam was administered orally and the dose was gradually increased to 1000 mg (41.1 mg/kg). Treatment significantly relieved the weakness of both lower limbs. However, occasional dizziness, binocular oculogyric crisis, and involuntary tongue extension continued. EEG re-examination at our hospital in January 2019 revealed occasional, sporadic, moderate amplitude spikes in the left frontal area during sleep (Figure 1B). The parents of the patient reported that his weight remained significantly increased and his sleep disorder had deteriorated; he fell asleep at 00:00 h and awoke at 06:00 h, had nightmares (3-4 times/night) accompanied by involuntary limb movements, and napped 5-6 times/d. He was subsequently admitted to our department.
The case had an unremarkable medical history.
The patient was born at term, with a birth weight of 3 kg. Growth and development prior to the onset of symptoms were normal and there was no obvious obesity. The patient was born through spontaneous delivery and had a normal Apgar score. There were no abnormalities noted during the perinatal period. His father was also obese, with height, weight, and body mass index of 173 cm, 88 kg, and 29 (> 97th percentile), respectively. However, he had no history or family history of sleep disorder or epilepsy.
At admission, his height, weight, and Rohrer index were 127 cm, 38.3 kg, and 186.98, respectively.
Saliva samples were collected at 8:00, 12:00, 16:00 and 22:00 respectively, using non-cotton collection devices to avoid any interference with the assay result of salivary melatonin. Melatonin analyses were carried out using liquid chromatography tandem mass spectrometry as previously described[7]. Peripheral blood samples were collected at 0:00, 8:00 and 16:00, and plasma adrenocorticotropic hormone (ACTH) and cortisol levels were detected by using radioimmunological methods.
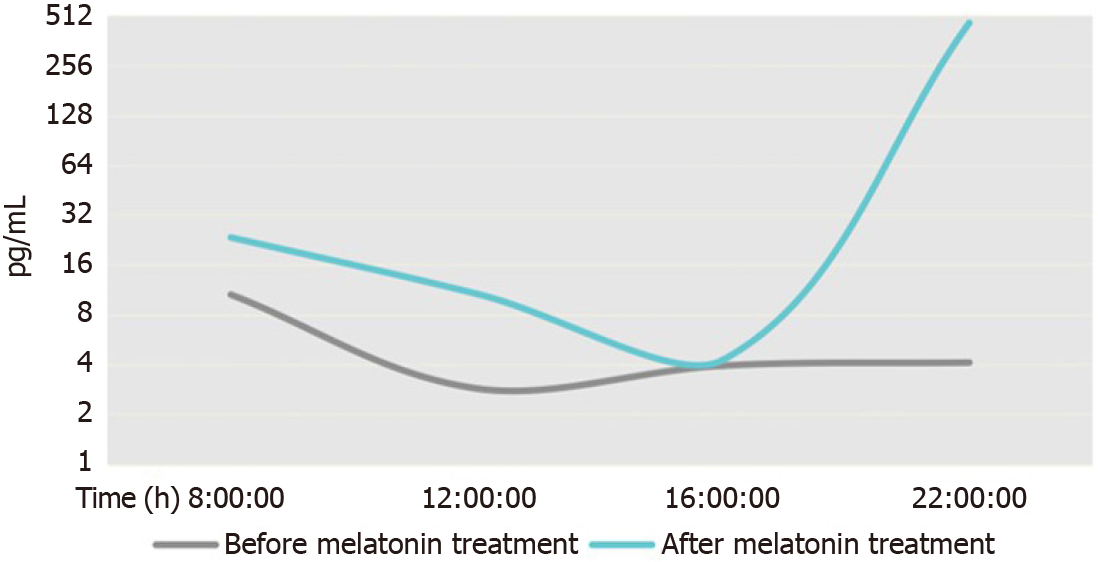
Testing showed that the melatonin secretion rhythm was reversed. There were no significant abnormalities in adrenocorticotropic hormone (ACTH), cortisol concentration and rhythm, blood biochemistry, or thyroid hormones (Table 1).
| Factor | Time (normal as reference) | Before melatonin treatment | After melatonin treatment (7 mo later) |
| Melatonin (pg/mL) | 8:00 (< 5) | 10.56a ↑ | 23.414a ↑ |
| 12:00 (< 5) | 2.86 | 10.677a ↑ | |
| 16:00 (< 5) | 3.935 | 4.261 | |
| 22:00 (> 10) | 4.107a ↓ | 464.298 | |
| ACTH (pmol/L) | 0:00 (0-8.7) | 3.04 | 1.46 |
| 8:00 (2.31-18) | 8.75 | 2.66 | |
| 16:00 (1.7-16.7) | 4.35 | 4.08 | |
| Cortisol (nmol/L) | 0:00 (0-165.7) | 25.7 | 82.66 |
| 8:00 (98.7-797.5) | 431.52 | 101.28 | |
| 16:00 (85.3-495.6) | 223.87 | 131.95 | |
| Triglyceride (mmol/L) | 0.79 | 0.95 | |
| Total triiodothyronine (pmol/L) | 6.11 | 6.14 | |
| Total tetraiodothyronine (pmol/L) | 13.74 | 14.54 | |
| Thyroid-stimulating hormone (mU/L) | 3.13 | 3.05 | |
| Cholesterol (mmol/L) | 4.54 | 2.97 | |
| Blood glucose (mmol/L) | 4.5 | 4.22 | |
| Rorher index | 186.98a ↑ | 186.52a ↑ |
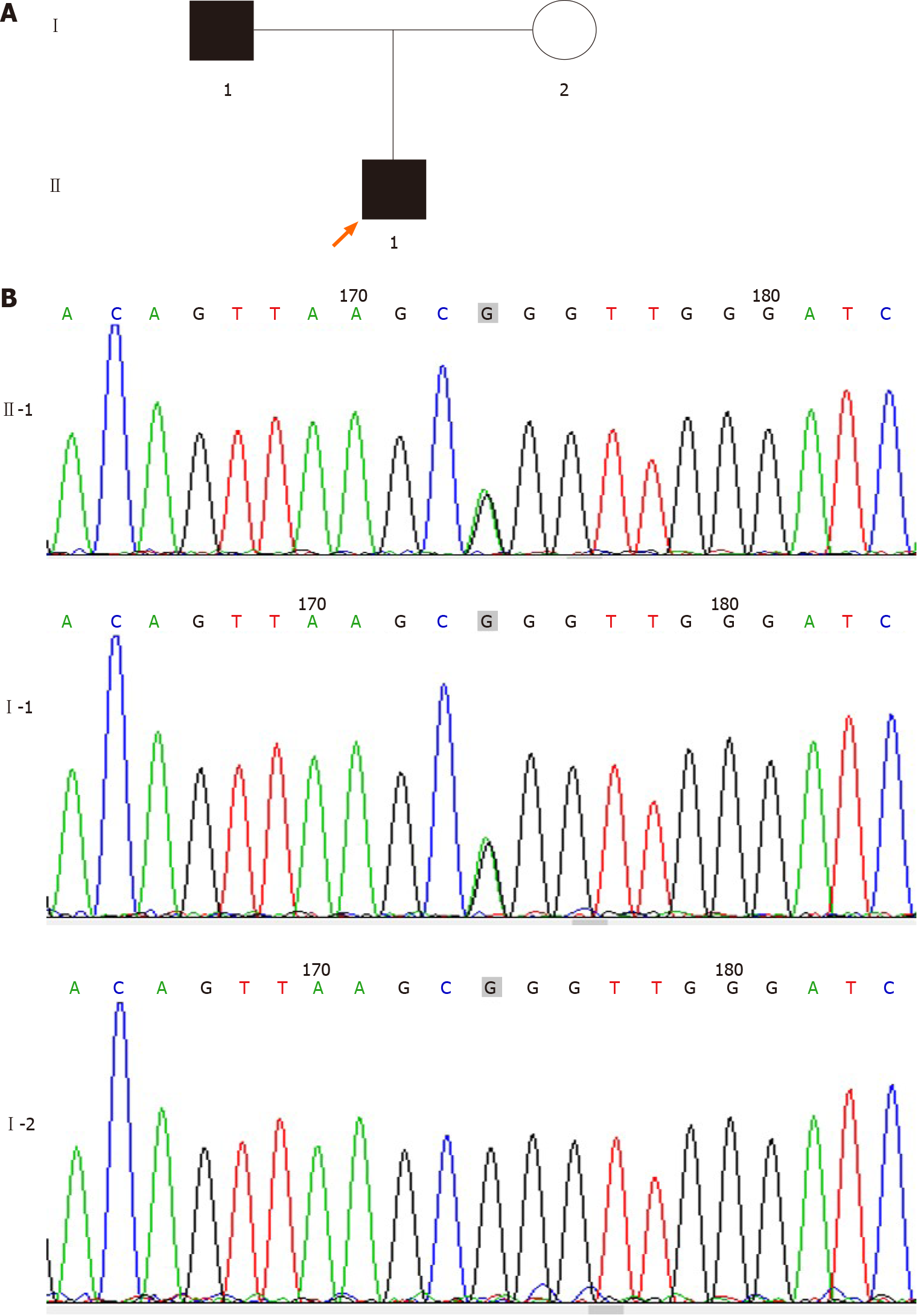
Sequencing was conducted by Findrare genetic-testing companies, Briefly, peripheral blood samples of the proband and his parents were prepared using the IDT xGenExomeResearchPanel V1.0 (Integrated DNA Technologies, Coralville, IA, United States). Sequencing was performed using paired-end, 100-cycle chemistry on the Illumina HiSeq or NextSeq (Illumina, San Diego, CA, United States). The original data of genome sequencing were mapped to the human genome (UCSC h19 human genome assembly), the acquired variation was annotated, and the genetic variation was further screened according to the clinical phenotype. We used the American College of Medical Genetics guidelines for variant interpretation in order to classify the variants. The pathogenic or suspected pathogenic variants associated with clinical phenotypes were verified by Sanger sequencing. Based on the American College of Medical Genetics guidelines, we revealed a heterozygous likely pathogenic point variant, c.494G>A (p.Arg165Gln) in the MC4R gene, originating from the father. Sorting intolerant from tolerant and polymorphism phenotyping analysis predicted that the variant was harmful and associated with obesity (Figure 2).
The final diagnosis was obesity, epilepsy and sleep disorder, which was based on physical, imaging, and laboratory examinations.
Based on this result, we added oral melatonin (Puritan’s Pride, Inc., Oakdale, NY, United States) 3 mg, once per night to the treatment.
Upon re-examination in August 2019 (following 7 mo of treatment with melatonin), his food intake had decreased, and the sleep disorder was relieved. He fell asleep at 21:00 h and awoke at 07:00 h, and the occurrence of nightmares with involuntary limb movement was decreased to approximately once per night, with daytime naps reduced to 2-3 times/d. Height and weight were 132 cm and 42.9 kg, respectively, with a Rohrer index of 186.52. Furthermore, his melatonin rhythm was significantly improved compared with the previous results (Figure 3). There were no abnormalities in ACTH, cortisol concentration and rhythm, blood biochemistry, or thyroid hormones (Table 1), and the EEG showed the absence of epileptic discharges (Figure 1C).
The MC4R gene is associated with energy metabolism. Abnormalities in MC4R can cause severe obesity in humans and animals, with variants in this gene being one of the most common monogenic causes of obesity[4]. Farooqi et al[8] detected this mutation when they sequenced the MC4R gene of 243 unrelated American patients with severe early-onset obesity (all patients developed severe obesity before the age of 10 years). In addition, Thearle et al[9] found that 40 of 4537 American obese children of Indian origin carried a MC4R (c.494G>A, p.Arg165Gln) heterozygous mutation, and in vitro investigation showed that all the above variations could lead to partial loss of function[9]. Of note, the association of this pathogenic variant with obesity has been recorded in the Human Gene Mutation Database; the population frequency of the Genome Aggregation Database was 7/246068, while that of the East Asian population of the Genome Aggregation Database was 1/17234.
In the present case, both father and son were obese and had a mutated MC4R gene. In the last examination, the Rohrer index of the patient was 186.52 and the body mass index of his father was 29. The father did not have epilepsy or sleep disorder. However, we think that these conditions were caused by incomplete penetrance of the epilepsy/disordered sleep phenotypes and/or possible other genetic variants, present in the son but not in the father, that may influence the effects of the MC4R variant. The melatonin rhythm was also clearly disrupted in this child, with low melatonin levels at night, which increased during daytime. This was accompanied by multiple naps during daytime, difficulty in sleeping at night, early awakening in the morning, and other obvious sleep disorders. His epilepsy occurred as focal episodes, with abnormal EEG findings. Hence, the diagnosis of the patient was clear; however, he continued to experience seizures after 6 mo of treatment with simple antiepileptic drugs. EEG review showed that waves associated with epilepsy remained, and there was no noticeable improvement in sleep disturbance.
A MC4R gene defect was previously reported in only one case of a child with a marked sleep disorder and obesity[10], suggesting that sleep disorder in that child was caused by a narrowing of the airway due to obesity. However, our findings indicate that the symptoms observed in the present case more closely resembled those of a rapid eye movement sleep disorder, described as frequent nightmares and associated body movements, which may have been caused by abnormal levels of melatonin[11]. In addition, the study conducted by Goni et al[12] showed that the MC4R gene and the melatonin receptor 1B gene had a clear interaction. Therefore, we hypothesized that the sleep disorders of the patient were related to abnormalities in the MC4R gene. Moreover, there is evidence of an association of abnormal MC4R gene expression and refractory epilepsy[13]. Furthermore, MC4R can act on Kir7.1, a potassium export channel, which is normally expressed as an inhibitor of potassium influx. This potassium channel can act on hypothalamic neurons, and its abnormal function may cause epilepsy[14]; however, there are no cases reported thus far.
Ayça et al[15] confirmed the role of melatonin in regulating circadian rhythms and sleep-waking patterns. Moreover, melatonin can also act on MC4R. For example, one study found that zebrafish fed with different concentrations of melatonin showed a significant increase in the expression of MC4R after 10 d compared with untreated zebrafish[4]. Numerous experimental reports demonstrated that melatonin is closely associated with epilepsy, and abnormal levels of melatonin can lead to epilepsy[5,6]. The anti-convulsive effects of melatonin have been demonstrated in numerous animal experiments[16]. Nevertheless, at present, it is mainly used for the treatment of sleep disorders, with only a few studies administering it as adjuvant treatment along with antiepileptic drugs.
Previous studies have shown that sleep disorders, abnormal melatonin rhythm, and abnormality in Kir7.1 may contribute to epilepsy. Whether the combination of these three factors exacerbates the condition is unclear. However, according to previous literature[5,14], melatonin exerts a positive effect in the regulation of sleep disorders and epilepsy; hence, we administered melatonin in this patient. Fortunately, following the administration of melatonin, his epilepsy resolved, the sleep disorder was corrected, and the abnormal melatonin rhythm was rectified. Furthermore, his Rohrer index was slightly reduced. Nevertheless, considering the severe obesity of this patient, we concluded that treatment with melatonin contributed to the control of his obesity.
In conclusion, we hypothesized that the occurrence of obesity and abnormal melatonin in this patient was associated with the MC4R gene variant, and these abnormalities led to disordered sleep and epilepsy. This is the first report of the combination of these symptoms in a patient with an MC4R variant. Furthermore, in our patient, adjuvant therapy with melatonin exerted a clear curative effect on these symptoms. Therefore, we propose that it is necessary to conduct genetic examination, particularly of the MC4R gene, to identify the etiology in children presenting with obesity, sleep disorders, and epilepsy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jiang XP S-Editor: Gao CC L-Editor: Filipodia P-Editor: Liu JH
| 1. | Adamska-Patruno E, Goscik J, Czajkowski P, Maliszewska K, Ciborowski M, Golonko A, Wawrusiewicz-Kurylonek N, Citko A, Waszczeniuk M, Kretowski A, Gorska M. The MC4R genetic variants are associated with lower visceral fat accumulation and higher postprandial relative increase in carbohydrate utilization in humans. Eur J Nutr. 2019;58:2929-2941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Kim JH, Choi JH. Pathophysiology and clinical characteristics of hypothalamic obesity in children and adolescents. Ann Pediatr Endocrinol Metab. 2013;18:161-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Kühnen P, Clément K, Wiegand S, Blankenstein O, Gottesdiener K, Martini LL, Mai K, Blume-Peytavi U, Grüters A, Krude H. Proopiomelanocortin Deficiency Treated with a Melanocortin-4 Receptor Agonist. N Engl J Med. 2016;375:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 325] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 4. | Piccinetti CC, Migliarini B, Olivotto I, Simoniello MP, Giorgini E, Carnevali O. Melatonin and peripheral circuitries: insights on appetite and metabolism in Danio rerio. Zebrafish. 2013;10:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Paprocka J, Kijonka M, Pęcka M, Sokół M. Melatonin in Epilepsy: A New Mathematical Model of Diurnal Secretion. Int J Endocrinol. 2016;2016:3861461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Jain SV, Horn PS, Simakajornboon N, Beebe DW, Holland K, Byars AW, Glauser TA. Melatonin improves sleep in children with epilepsy: a randomized, double-blind, crossover study. Sleep Med. 2015;16:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 7. | Jensen MA, Hansen AM, Abrahamsson P, Nørgaard AW. Development and evaluation of a liquid chromatography tandem mass spectrometry method for simultaneous determination of salivary melatonin, cortisol and testosterone. J Chromatogr B Analyt Technol Biomed Life Sci. 2011;879:2527-2532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Farooqi IS, Yeo GS, Keogh JM, Aminian S, Jebb SA, Butler G, Cheetham T, O'Rahilly S. Dominant and recessive inheritance of morbid obesity associated with melanocortin 4 receptor deficiency. J Clin Invest. 2000;106:271-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 599] [Cited by in RCA: 539] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 9. | Thearle MS, Muller YL, Hanson RL, Mullins M, Abdussamad M, Tran J, Knowler WC, Bogardus C, Krakoff J, Baier LJ. Greater impact of melanocortin-4 receptor deficiency on rates of growth and risk of type 2 diabetes during childhood compared with adulthood in Pima Indians. Diabetes. 2012;61:250-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Pillai S, Nandalike K, Kogelman Y, Muzumdar R, Balk SJ, Arens R. Severe obstructive sleep apnea in a child with melanocortin-4 receptor deficiency. J Clin Sleep Med. 2014;10:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Dauvilliers Y, Schenck CH, Postuma RB, Iranzo A, Luppi PH, Plazzi G, Montplaisir J, Boeve B. REM sleep behaviour disorder. Nat Rev Dis Primers. 2018;4:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 310] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 12. | Goni L, Cuervo M, Milagro FI, Martínez JA. Gene-Gene Interplay and Gene-Diet Interactions Involving the MTNR1B rs10830963 Variant with Body Weight Loss. J Nutrigenet Nutrigenomics. 2014;7:232-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Liu X, Ou S, Xu T, Liu S, Yuan J, Huang H, Qin L, Yang H, Chen L, Tan X, Chen Y. New differentially expressed genes and differential DNA methylation underlying refractory epilepsy. Oncotarget. 2016;7:87402-87416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Litt MJ, Cone RD, Ghamari-Langroudi M. Characterization of MC4R Regulation of the Kir7.1 Channel Using the Tl+ Flux Assay. Methods Mol Biol. 2018;1684:211-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Ayça S, Aksoy HU, Taştan İ, Polat M. Levels of Melatonin in Continuous Spikes and Waves During Sleep. J Child Neurol. 2019;34:309-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Banach M, Gurdziel E, Jędrych M, Borowicz KK. Melatonin in experimental seizures and epilepsy. Pharmacol Rep. 2011;63:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |