Published online Apr 16, 2021. doi: 10.12998/wjcc.v9.i11.2619
Peer-review started: December 7, 2020
First decision: December 21, 2020
Revised: January 9, 2021
Accepted: February 10, 2021
Article in press: February 10, 2021
Published online: April 16, 2021
Processing time: 115 Days and 22.1 Hours
Cryptococcus presenting as an opportunistic pathogen mainly affects immunocompromised patients, but the disseminated form of infection is rare among immunocompetent populations. The partial radiographic characteristics of pulmonary cryptococcosis mimic lung carcinoma, leading to unnecessary open chest exploratory surgery, and the lack of a gold-standard noninvasive diagnostic increases the risk of misdiagnosis. Positron emission tomography/computed tomography (PET/CT), a sensitive method for distinguishing malignant tumors, coupled with cryptococcal latex agglutination test showing a high positive rate may overcome these issues.
A 36-year-old man presented for general examination, without health complaints. Routine CT showed multiple pulmonary nodules and a mass with high maximum standardized uptake value. Initially, we suspected primary malignancy with hematogenous metastasis. Although his routine fungal analysis had been negative, subsequent CT-guided percutaneous core needle biopsy and histopathology examination indicated a diagnosis of pulmonary cryptococcosis. Fluconazole (200 mg/d) antifungal drug treatment was initiated, and 1 mo later the pulmonary mass had reduced in size markedly (on chest CT scan) without any complications.
Serologic and PET/CT examinations may not rule out cryptococcosis, and percutaneous lung puncture is critical under all circumstances.
Core Tip: Cryptococcosis is a systemic fungal infection, with presentation ranging from asymptomatic pulmonary involvement to meningitis and disseminated disease. Generally, cryptococcosis is considered an opportunistic infection in immunocompro-mised individuals, affecting persons with human immunodeficiency virus infection in particular. Mass-like and disseminated cryptococcosis lesions are rare in patients with normal immunity, and a negative result on the cryptococcal latex agglutination test may be related to low-grade virulence of the fungus. We describe here a case of pulmonary cryptococcosis that was likely caused by a low-virulence strain, presenting bilaterally distributed lesions on imaging and mimicking hematogenous metastasis.
- Citation: Li Y, Fang L, Chang FQ, Xu FZ, Zhang YB. Cryptococcus infection with asymptomatic diffuse pulmonary disease in an immunocompetent patient: A case report. World J Clin Cases 2021; 9(11): 2619-2626
- URL: https://www.wjgnet.com/2307-8960/full/v9/i11/2619.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i11.2619
Cryptococcosis is a systemic infection caused by two species of the encapsulated yeast-like fungus Cryptococcus: Cryptococcus gattii (C. gattii) and Cryptococcus neoformans (C. neoforman)[1]. These opportunistic fungal pathogens usually cause cryptococcosis in immunocompromised patients, with the respiratory system being the usual route of infection. Infections in immunocompetent persons are much rarer.
Positron emission tomography/computed tomography (PET/CT) is a useful tool for differentiating benign and malignant tissues. Higher uptake values of fluorodeoxyglu
Cases of pulmonary cryptococcosis, therefore, require further noninvasive testing for a definitive diagnosis; yet, no gold-standard noninvasive diagnostic exists and the risk of misdiagnosis remains large. Prior to a biopsy and histological assessment [by Grocott’s methenamine silver (GMS) staining], the most common suspected diagnoses are lung cancer, inflammatory granuloma, metastases from an extrathoracic malignancy, and pulmonary tuberculosis.
As described below for our case, CT-guided percutaneous core needle biopsy of a presumed lung carcinoma can be critical for a definitive diagnosis of Cryptococcus infection.
A 34-year-old apparently immunocompetent Chinese man presented for general health examination. On routine CT, multiple pulmonary nodules and a mass were incidentally found.
The patient reported having had no symptoms of discomfort prior to presentation, including cough, sputum, chest pain, chills, or fever. He also denied tiring easily, having night sweats, and rapid weight loss.
The patient reported occupation as an engineer, smoking ten cigarettes a day for the past 3 years, and having no pets. He also had no history of allergies, hepatitis B, or diabetes mellitus, or any other significant medical history.
Physical examination upon admission found bilateral lungs to be clear, with no wheezing, rales, or rhonchi detected by auscultation. Temperature was 36.5 °C. Heart rate was 95 beats/min. Respiratory rate was 20 breaths/min. Blood pressure was 104/71 mmHg. There were no other remarkable findings.
Test findings for liver function, renal function, and electrolytes were normal. The values of fasting blood glucose were within the normal range twice during hospitalization. All inflammatory biomarkers were also within the normal range. The result of human immunodeficiency virus (HIV) serology test was negative. Tumor markers in blood, including carcinoembryonic antigen, progastrin-releasing peptide, neuron-specific enolase, and cytokeratin 19-fragments (CYFRA 21.1), were all normal. Serology test for Cryptococcus antigen also gave negative results.
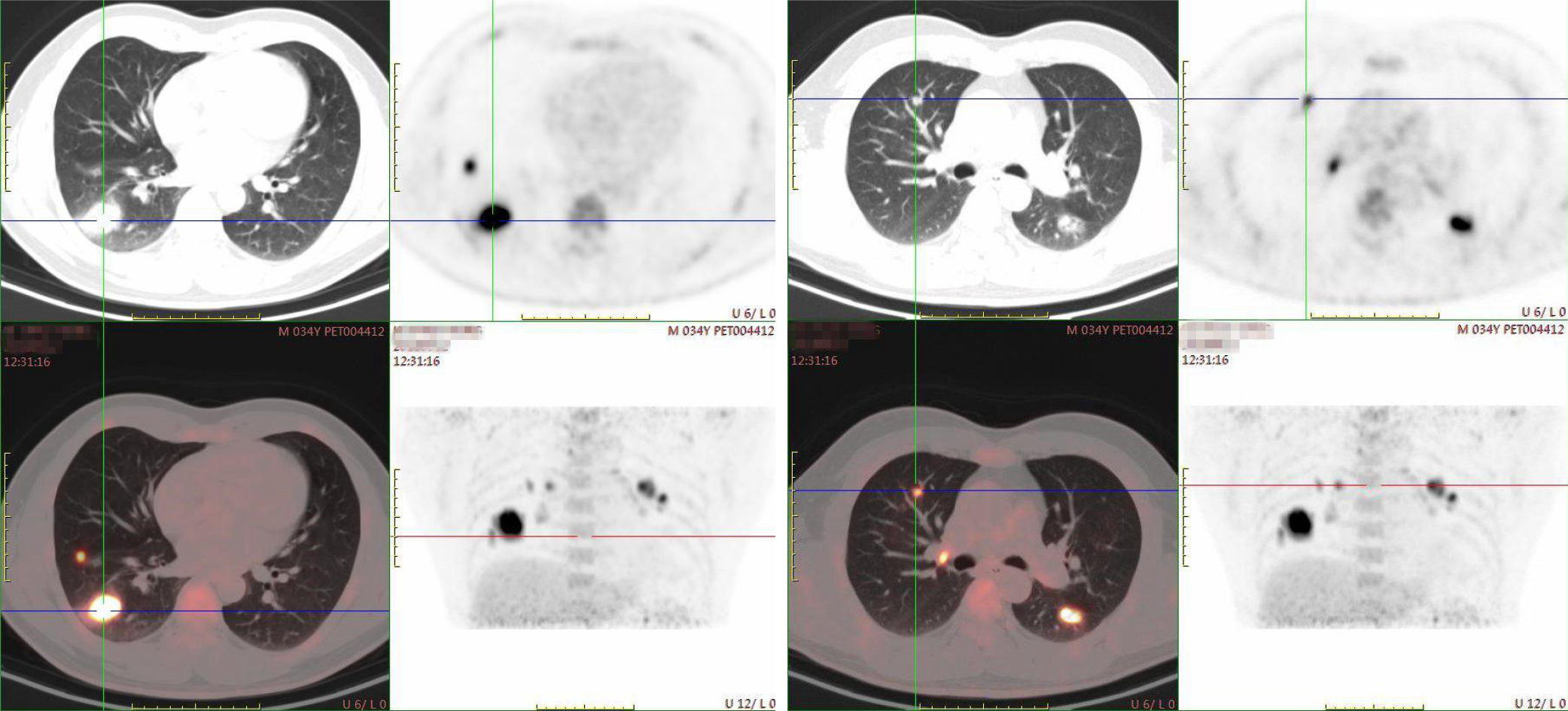
Due to the pulmonary lesions of unknown cause, PET/CT was arranged. The imaging showed multiple nodules in both lungs, enlarged right hilar lymph nodes, and an elliptic mass lesion without clear margin in the right lower lobe (Figure 1). The mass showed higher uptake values of 18F-fluorodeoxyglucose (FDG) and SUVmax of 16.4 in normal scans and 19.1 in delayed scans. The SUVmax for FDG uptake of those nodules was 6.8 in normal scans and 10.2 in delayed scans. The two enlarged lymph nodes in the right hilum gave 4.8 in normal scans and 6.9 in delayed scans.
Subsequently, the patient underwent CT-guided percutaneous core needle biopsy of the right lower-lobe mass. No fungi or remarkable bacteria were found in the puncture fluid smear.
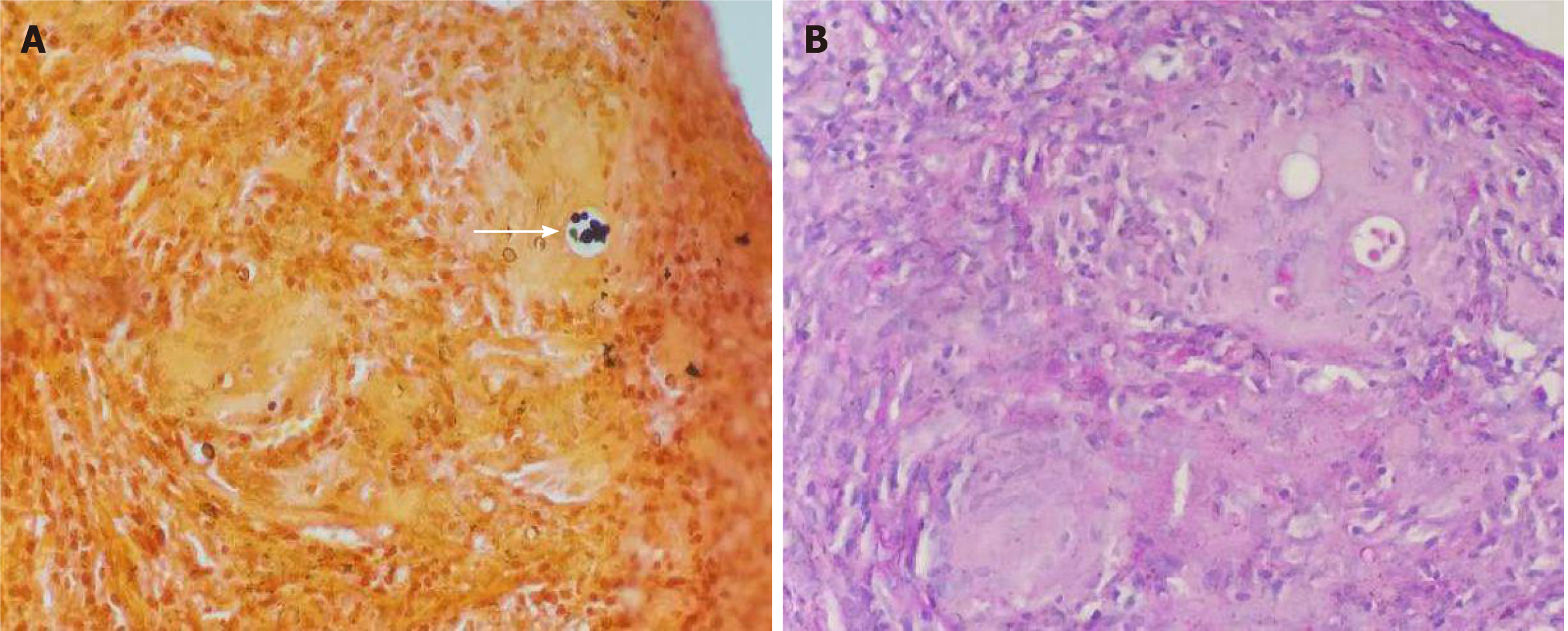
The pathologic consultation found granulomatous inflammation. GMS was positive and periodic acid-Schiff staining was negative (Figure 2). No evidence of malignancy was noted. In summary, a diagnosis of cryptococcal pneumonia was established.
A diagnosis of pulmonary cryptococcosis was made according to the radiologic evidence of pulmonary lesions and positive histopathology, although the serology test for Cryptococcus antigen was negative.
Fluconazole (200 mg) per day orally.
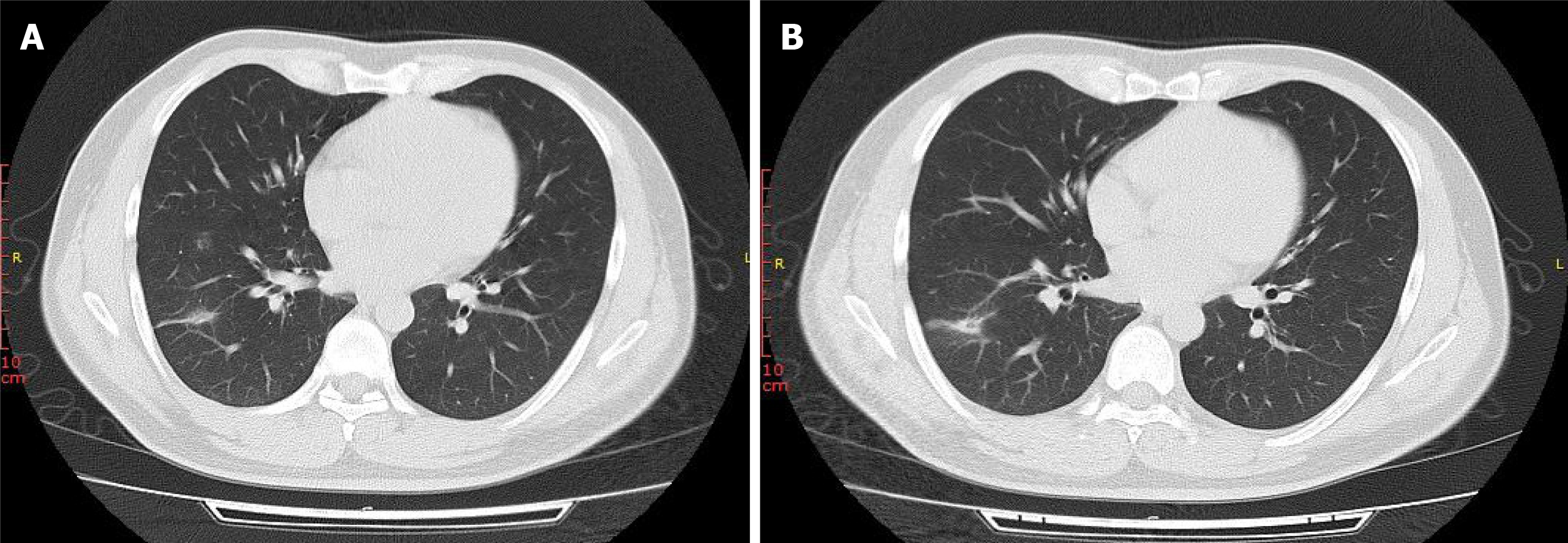
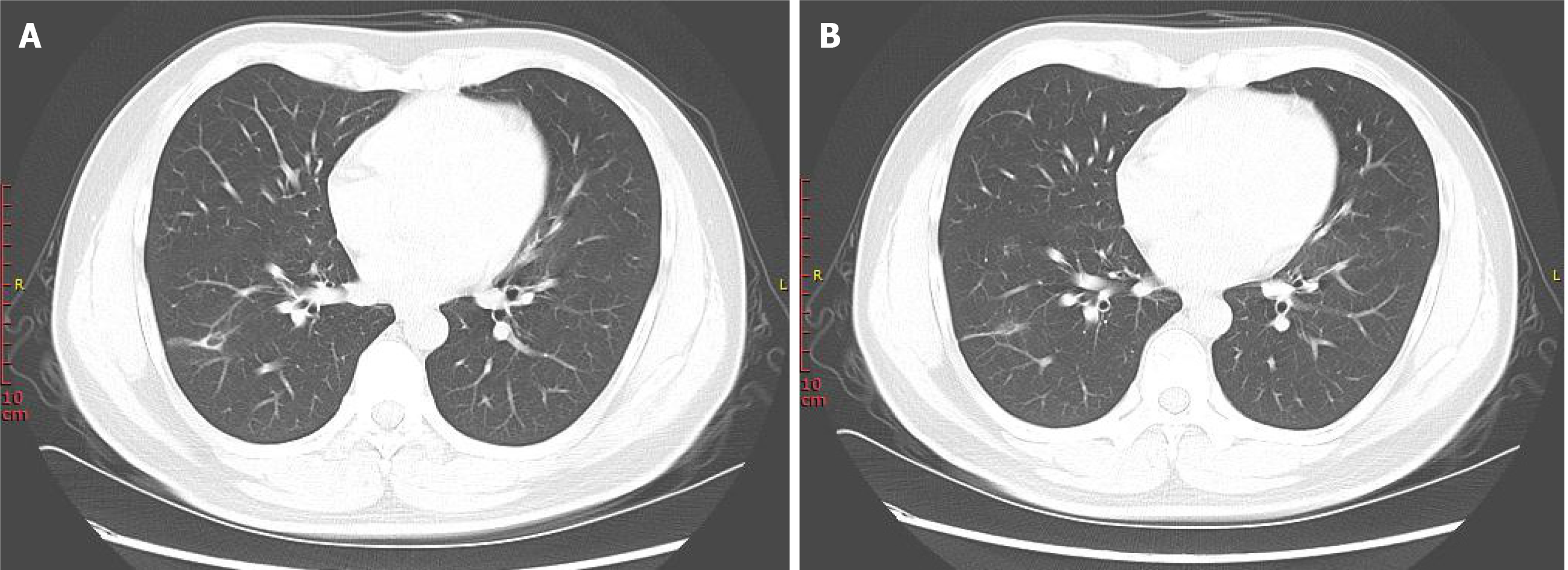
After 1 mo and 3 mo of treatment, the pulmonary lesions were found to be markedly reduced in size on chest CT (Figures 3 and 4).
Pulmonary cryptococcosis is prevalent in patients with compromised cell-mediated immunity, such as those with HIV infection or who have been subject to chemotherapy or other immunosuppressive therapy[3,4]. It is known that patients with HIV infection are more likely to have central nervous system involvement with the cryptococcosis disease than those without. In that group, the disease itself is associated with a high mortality rate. Cryptococcosis can also occur in individuals with normal immunity and causes severe nervous system infections[5], but such cases are rare. Table 1 illustrates the special features of our report.
| Case | Sex, age | Medical history | Diagnostic modalities | Clinical presentation | Imaging | Immuno-assay | Histopathology | Treatment |
| 1, this report | M36 | Good condition | CT-guided percutaneous core needle biopsy | None | Pulmonary nodules and a mass in both lungs; PET-CT showed the SUVmax of the cryptococcal lesions fluctuated from 4.8 to 19.1 | Negative | Granulomatous inflammation; GMS was positive and PSA was negative | Fluconazole |
| 2, Bavishi et al[20] | F67 | Hypertension and cholelithiasis | CT-guided percutaneous core needle biopsy | Recurrent dry cough for 4 yr | Multiple pulmonary nodules in both the lower lobes | Serology cryptococcal antigen titer of 1: 32 | FMS staining was strongly positive | Intravenous amphotericin B for 2 d and then changed to fluconazole |
| 3, Zhou et al[21] | M44 | Good condition | Brochoscopy | 3-mo history of cough, hemoptysis | Pulmonary nodules in both lungs; PET-CT showed the SUVmax of the cryptococcal lesions fluctuated from 9.86 to 10.99 | Titer of more than 1: 1, 280 | GMS stain was positive; Culture of bronchoscopy with brush was positive | Amphotericin B |
| 4, Marroni et al[22] | F21 | Good condition | CT-guided percutaneous core needle biopsy | Rigors, fever, dyspnoea, dry cough, and chest pain | A round mass in the lung | Positive at a titre of 1: 256 | GMS and PSA staining was positive | Fluconazole |
| 5, Oliveira et al[5] | M64 | Arterial hypertension | Fiberoptic bronchoscopy with bronchoalveolar lavage | Fever, weakness, anorexia, headache, dyspnea, cough, purulent sputum production, and disorientation | Pulmonary spherical mass lesion, 5 cm in diameter | The CSF cryptococcal antigen titer was 1: 4096 with a serum titer of 1:2048 | MGG staininh was positive | Amphotericin B |
| 6, Ruan et al[12] | M68 | Good condition | Surgical drainage | Progressive multiple abscesses, fever, lower extremity weakness, and urinary retention | Pulmonary abscess formation and multiple destruction of vertebral bodies | Negative | Culture revealed; Cryptococcus neoformans; India ink staining | Itraconazole; Fluorocytosine; Fluconazole |
For our case, the patient was otherwise healthy and had no neurological symptoms. However, he presented bilaterally disseminated lesions in the lung, which is extremely rare for an asymptomatic immunocompetent person, and this increased the chance of mistaken and missed diagnosis. Interestingly, his cryptococcal latex agglutination test (CLAT) was also negative. In other reports in the literature, the positive rate for CLAT has been high, even exceeding 90%[6,7]. CLAT is also used to evaluate response to therapy for pulmonary cryptococcosis in patients without HIV infection[7].
Most cryptococcal strains are encapsulated by polysaccharides[8] and capsule-deficient C. neoformans may have reduced virulence[9]. A cryptococcal strain that has lost its capsular material can, however, trigger strong inflammatory reactions, which tends to lead to the formation of granulomas composed of histiocytes, giant cells, and lymphocytes. This is consistent with our pathological outcome. We speculated that our patient may have been infected with a low-virulence C. neoformans strain, thus causing the false negative CLAT result[10]. Certainly, other unknown possibilities cannot be excluded.
Of the two Cryptococcus species, C. neoformans is widespread, especially in pigeon feces or in soil contaminated with these feces, and it tends to cause disease in patients who are immunocompromised. In Taiwan, there is evidence to show a significant prevalence of C. gattii infection associated with the eucalyptus tree[11]. C. gattii usually causes disease in immunocompetent persons and behaves as a primary pathogen. The percentage of C. gattii infection in immunocompetent hosts is significantly higher than that of C. neoformans infection[12].
In 2018, the World Health Organization recommended that without the results of cerebrospinal fluid, rapid serum, plasma, or whole-blood cryptococcal antigen assays are the preferred diagnostic methods (either lateral flow assay or latex agglutination assay). Some studies have reported that CLAT has an insufficient sensitivity for C. gattii compared to the lateral flow assay, increasing the risk of delayed diagnosis and probability of misdiagnosis[13]. As such, in order to diagnose cryptococcosis, multiple detection methods should be applied to improve the accuracy of diagnosis.
C. gattii infection is more common in tropical areas[11], which is inconsistent with the geography of our patient’s residential area. During the subsequent visit, the patient told us that one of his neighbors kept pigeons, which supported our speculation that the patient was likely to have been infected with a low-virulence strain of C. neoformans.
The most common radiographic characteristics of pulmonary cryptococcosis consist of solitary pulmonary mass or nodules, combined patchy and nodular shadows, cavitation, and enlarged mediastinal lymph nodes[14]. However, the most common imaging finding of immunocompetent patients is single nodule. Mass-like and bronchopneumonic patterns are common in immunocompromised patients and rare in the patients with normal immunity[15]. PET/CT is a sensitive method for distinguishing malignant tumors from benign tissue, and it has gradually become a useful imaging technology for the differential diagnosis, staging, and follow-up of cancer[16]. The related SUVmax quantitatively measures the FDG uptake of a tumor.
Generally, the SUVmax value of 2.5 is used as the cut-off for differentiating benign lesions from malignant ones, as it is known to have the best sensitivity and specificity for such. However, the diagnostic accuracy of this value is not high in pulmonary infectious diseases, especially for those due to granulomatous diseases[17] such as in our patient. The SUVmax values for cases of pulmonary cryptococcosis may vary widely, indicating anywhere from mild to marked uptake. In previous reports, the SUVmax of the cryptococcal lesions fluctuate from 0.93 to 13.0[15,18], with most cases exceeding the 2.5 threshold. Nevertheless, few of the SUVmax values of pulmonary lesions reach 19.
The mechanism of increased FDG uptake in cryptococcal lesions may be related to the “respiratory burst”, which increases cellular glucose metabolism. Based on this principle, PET/CT can play a role in assessing the treatment of patients with fungal infection[19]. Therefore, diagnosis of malignant tumor by PET/CT should exclude the possibility of fungal infection. Our case was remarkable since we could not find evidence of immunocompromise in our patient; additional reports of such cases and bench-to-bedside studies will help to explain the development of masses and diffuse lesions in patients who are infected with a low-virulence strain (as we suspect our patient was).
We describe here an immunocompetent patient with pulmonary Cryptococcus infection, who manifested a mass and diffuse lesions in his lung while being asymptomatic. Although it is very rare, cryptococcosis must be included in the differential diagnosis of pulmonary lesions in patients without immunosuppression. It is important to recognize that pulmonary fungal infection can mimic metastases, even when the patient has been diagnosed with lung cancer by PET/CT. Furthermore, the potential for false negative results of fungal smears and serologic testing for cryptococcosis is another risk for misdiagnosis of this infectious disease. Thus, percutaneous lung puncture is critical under all circumstances in order to promote more timely initiation of appropriate treatment and avoidance of unnecessary surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tripathy SK S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Li JH
| 1. | Li SS, Mody CH. Cryptococcus. Proc Am Thorac Soc. 2010;7:186-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Sun LM, Chen TY, Chen WJ, Hsieh MJ, Liu JW, Huang CC, Wang CJ. Cryptococcus infection in a patient with nasopharyngeal carcinoma: imaging findings mimicking pulmonary metastases. Br J Radiol. 2002;75:275-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ou KW, Hsu KF, Cheng YL, Hsu GC, Hsu HM, Yu JC. Asymptomatic pulmonary nodules in a patient with early-stage breast cancer: Cryptococcus infection. Int J Infect Dis. 2010;14:e77-e80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Tamagawa S, Hotomi M, Yuasa J, Tuchihashi S, Yamauchi K, Togawa A, Yamanaka N. Primary laryngeal cryptococcosis resembling laryngeal carcinoma. Auris Nasus Larynx. 2015;42:337-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Oliveira Fde M, Severo CB, Guazzelli LS, Severo LC. Cryptococcus gattii fungemia: report of a case with lung and brain lesions mimicking radiological features of malignancy. Rev Inst Med Trop Sao Paulo. 2007;49:263-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Berlin L, Pincus JH. Cryptococcal meningitis. False-negative antigen test results and cultures in nonimmunosuppressed patients. Arch Neurol. 1989;46:1312-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Lin TY, Yeh KM, Lin JC, Wang NC, Peng MY, Chang FY. Cryptococcal disease in patients with or without human immunodeficiency virus: clinical presentation and monitoring of serum cryptococcal antigen titers. J Microbiol Immunol Infect. 2009;42:220-226. [PubMed] |
| 8. | Zeng Y, Wu X, Yi X, Luo B, Zhu M, Rui W, Zhu X, Li X, Li H. Clinicopathologic and ultrastructural study of non-HIV-related primary pulmonary cryptococcosis in China: report of 43 cases. Ultrastruct Pathol. 2011;35:19-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Kronstad JW, Attarian R, Cadieux B, Choi J, D'Souza CA, Griffiths EJ, Geddes JM, Hu G, Jung WH, Kretschmer M, Saikia S, Wang J. Expanding fungal pathogenesis: Cryptococcus breaks out of the opportunistic box. Nat Rev Microbiol. 2011;9:193-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 242] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 10. | Gazzoni AF, Severo CB, Salles EF, Severo LC. Histopathology, serology and cultures in the diagnosis of cryptococcosis. Rev Inst Med Trop Sao Paulo. 2009;51:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Chen YC, Chang SC, Shih CC, Hung CC, Luhbd KT, Pan YS, Hsieh WC. Clinical features and in vitro susceptibilities of two varieties of Cryptococcus neoformans in Taiwan. Diagn Microbiol Infect Dis. 2000;36:175-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Ruan Q, Zhu Y, Chen S, Zhu L, Zhang S, Zhang W. Disseminated cryptococcosis with recurrent multiple abscesses in an immunocompetent patient: a case report and literature review. BMC Infect Dis. 2017;17:369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Tintelnot K, Hagen F, Han CO, Seibold M, Rickerts V, Boekhout T. Pitfalls in Serological Diagnosis of Cryptococcus gattii Infections. Med Mycol. 2015;53:874-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ye F, Xie JX, Zeng QS, Chen GQ, Zhong SQ, Zhong NS. Retrospective analysis of 76 immunocompetent patients with primary pulmonary cryptococcosis. Lung. 2012;190:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Wang SY, Chen G, Luo DL, Shao D, Liu ET, Sun T, Wang SX. 18F-FDG PET/CT and contrast-enhanced CT findings of pulmonary cryptococcosis. Eur J Radiol. 2017;89:140-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Hung GU, Shiau YC, Tsai SC, Ho YJ, Kao CH, Yen RF. Differentiation of radiographically indeterminate solitary pulmonary nodules with. Jpn J Clin Oncol. 2001;31:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Cengiz A, Aydın F, Sipahi M, Dertsiz L, Özbilim G, Bozkurt S, Güngör F, Boz A, Erkılıç M. The role of F-18 FDG PET/CT in differentiating benign from malignant pulmonary masses and accompanying lymph nodes. Tuberk Toraks. 2018;66:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Huang CJ, You DL, Lee PI, Hsu LH, Liu CC, Shih CS, Shih CC, Tseng HC. Characteristics of integrated 18F-FDG PET/CT in Pulmonary Cryptococcosis. Acta Radiol. 2009;50:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Sharma P, Mukherjee A, Karunanithi S, Bal C, Kumar R. Potential role of 18F-FDG PET/CT in patients with fungal infections. AJR Am J Roentgenol. 2014;203:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 20. | Bavishi AV, McGarry TM. A case of pulmonary cryptococcosis caused by capsule-deficient cryptococcus neoformans in an immunocompetent patient. Respir Care. 2010;55:937-941. [PubMed] |
| 21. | Zhou Q, Hu B, Shao C, Zhou C, Zhang X, Yang D, Li C. A case report of pulmonary cryptococcosis presenting as endobronchial obstruction. J Thorac Dis. 2013;5:E170-E173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Marroni M, Pericolini E, Cenci E, Bistoni F, Vecchiarelli A. Functional defect of natural immune system in an apparent immunocompetent patient with pulmonary cryptococcosis. J Infect. 2007;54:e5-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |