Published online Mar 6, 2020. doi: 10.12998/wjcc.v8.i5.932
Peer-review started: November 24, 2019
First decision: December 23, 2019
Revised: January 2, 2020
Accepted: January 8, 2020
Article in press: January 8, 2020
Published online: March 6, 2020
Processing time: 102 Days and 18.5 Hours
Generally, hemangiomas do not require surgical intervention; however, cases of large hemangiomas, potentially involving the throat and trachea, necessitate surgical therapy. Here, we present a case of hypopharyngeal hemangioma in an adult that was successfully treated with neodymium-doped yttrium aluminum garnet (Nd-YAG) laser.
Laryngoscopic examination of a 61-year-old man demonstrated the presence of a large, submucosal vascular lesion that extended into the epiglottis, left arytenoid cartilage, lateral to the aryepiglottic fold, and pyriform sinus. The lesion was resected and photocoagulated with limited hemorrhage using Nd: YAG laser. The hypopharyngeal hemangioma was completely excised. The patient showed no recurrence of hypopharyngeal hemangioma during the 1.5-year follow-up period.
Laser therapy is one of the effective tools for treating hemangiomas with rapid, uncontrolled growth or in functional areas, with few side effects and complications. The present case of a male patient with a large hypopharyngeal hemangioma, treated with YAG laser, demonstrates the efficacy of laser photocoagulation in treating cases of hemangiomas, without the risk of bleeding or airway obstruction. The favorable postoperative outcomes demonstrated by our patient with Nd: YAG laser therapy indicate its consideration in the therapy of similar cases.
Core tip: Owing to the rarity of hemangiomas, not much information is known about the incidence and treatment of such cases. Hemangiomas generally do not require surgical interventions. However, owing to the large size of the tumor in our patient, we used neodymium-doped yttrium aluminum garnet laser photocoagulation to treat the tumor. The therapy was successful, and showed no occurrence of bleeding, airway obstruction, or postoperative infections. We believe that our study makes a significant contribution to the literature because the favorable results observed in our patient highlight the beneficial effects of laser photocoagulation in treating hemangiomas.
- Citation: Jin M, Wang CY, Da YX, Zhu W, Jiang H. Surgical resection of a large hypopharyngeal hemangioma in an adult using neodymium-doped yttrium aluminum garnet laser: A case report. World J Clin Cases 2020; 8(5): 932-938
- URL: https://www.wjgnet.com/2307-8960/full/v8/i5/932.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i5.932
Clinically, hemangiomas are divided into pediatric and adult types, and can occur at any age. In adults, hemangiomas usually occur in the larynx, and rarely in the hypopharynx. Laryngeal hemangiomas are slowly progressing vascular tumors, which are commonly diagnosed in children, but rarely, in adults[1].
The terms capillary hemangioma and venous hemangioma were commonly used to describe various types of hemangioma in the past; however, their usage is not precise. Many diagnosed cases of venous aneurysms are actually vascular malformations rather than true hemangioma[2]. Therefore, an important definition is that hemangiomas are true vascular tumors with distinct clinical and biological characteristics, derived from vascular malformations.
Hemangioma can be found all over the body, including the liver[3], gastrointestinal tract[4], central nervous system[5], pancreas[6], gall bladder[7], thymus[8], spleen[9], lymph nodes[10], lung[11], urinary bladder[12], and adrenal glands[13]. In adults, hemangiomas rarely occur in the hypopharynx. Because of the rarity of cases of hypopharyngeal hemangiomas, the exact incidence of the tumor remains unknown. The diagnosis of hemangioma is usually based on clinical history and presentation. In addition, computed tomography and magnetic resonance imaging have both been used in clinical practice. Magnetic resonance imaging and magnetic resonance angiography represent the best diagnostic tools to demonstrate, respectively, soft-tissue components and relationships with nearby structures[14,15]. Time-resolved imaging of contrast kinetics is a recently introduced technique that can obtain dynamic images during the arterial, capillary, and venous phases. It improves temporal resolution with respect to contrast-enhanced magnetic resonance angiography technique[16]. It is possible to acquire three dimensional volumes during the passage of gadolinium, to detect the vascularization of the region of interest over time, similar to digital subtraction angiography. Digital subtraction angiography is an invasive, relatively expensive, time-consuming technique, with risk of vascular injury and exposure to ionization[17].
Currently, there is no established consensus for treating hemangiomas because of their rarity. However, large-sized hemangiomas require therapeutic intervention, including surgical resection, corticosteroid injection, ethanol injection, cryosurgery, radium or gold implants, and interferon treatment[18].
We present the case of a hypopharyngeal hemangioma (12 mm × 15 mm) in an adult that was successfully treated with neodymium-doped yttrium aluminum garnet (Nd-YAG) laser (wavelength, 1064 nm).
On May 2, 2017, a 61-year-old male patient presented to the Jinshan Hospital of Fudan University (Shanghai, China). The patient had no hoarseness of voice, hemoptysis, expectoration, or dyspnea. Due to upset stomach, he underwent a gastroscopy, which revealed a hypopharyngeal tumor.
The patient had no history of cigarette smoking. He has suffered from hypertension for more than 20 years.
When the patient presented to our hospital, his temperature was 36.6 °C, heart rate was 80 bpm, respiratory rate was 18 breaths/min, blood pressure was 150/90 mmHg, and oxygen saturation in room air was 98%.
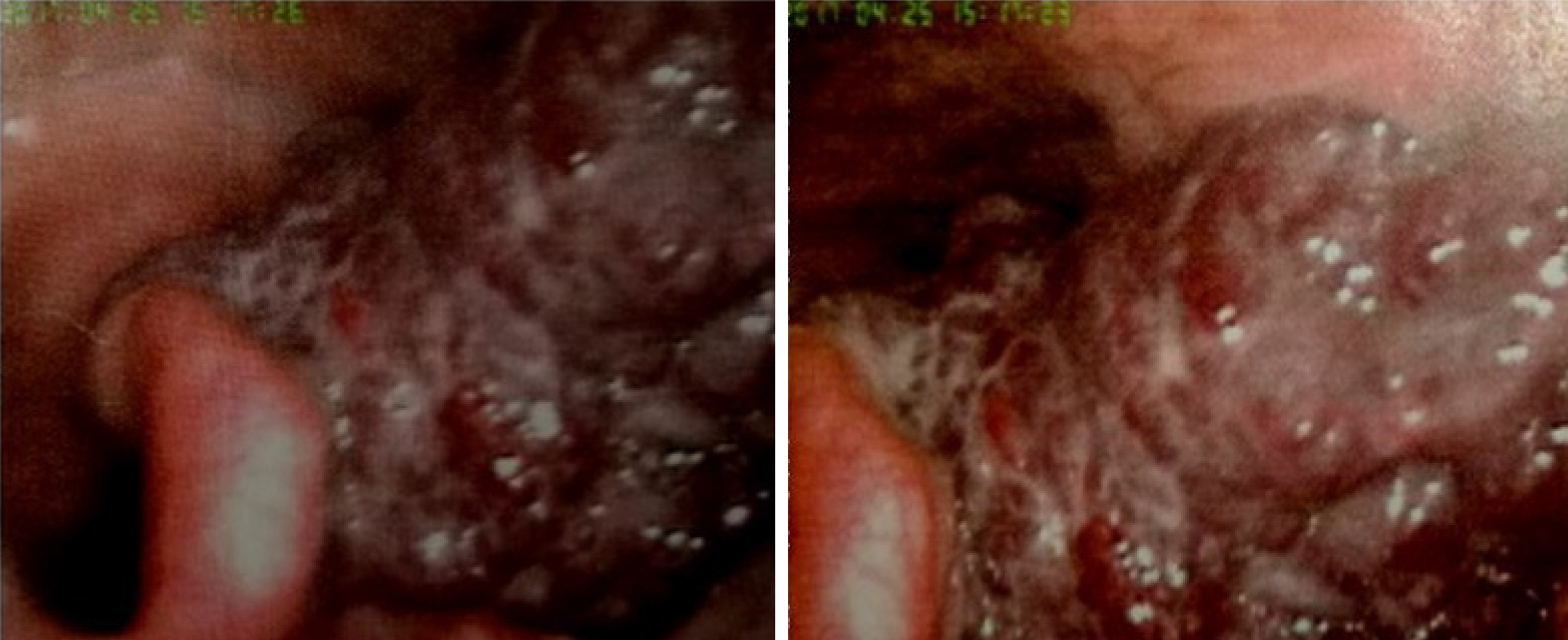
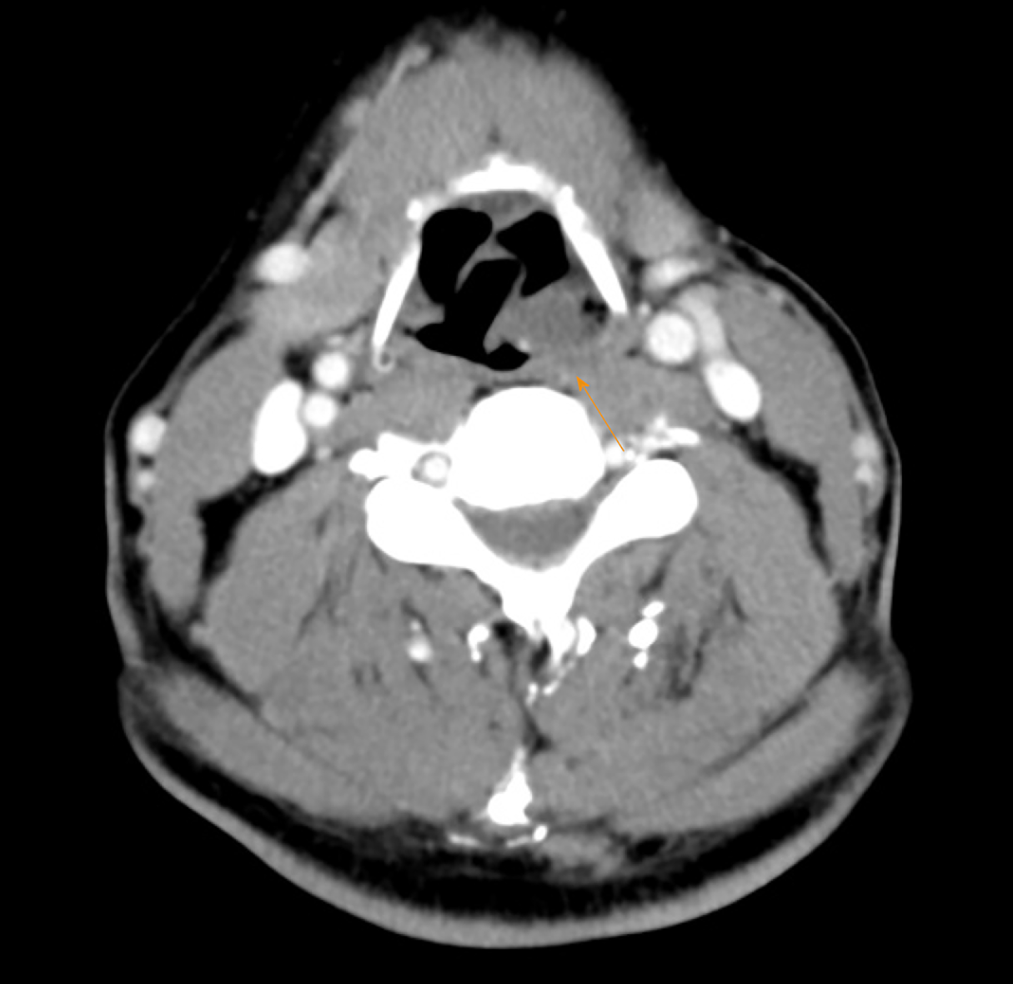
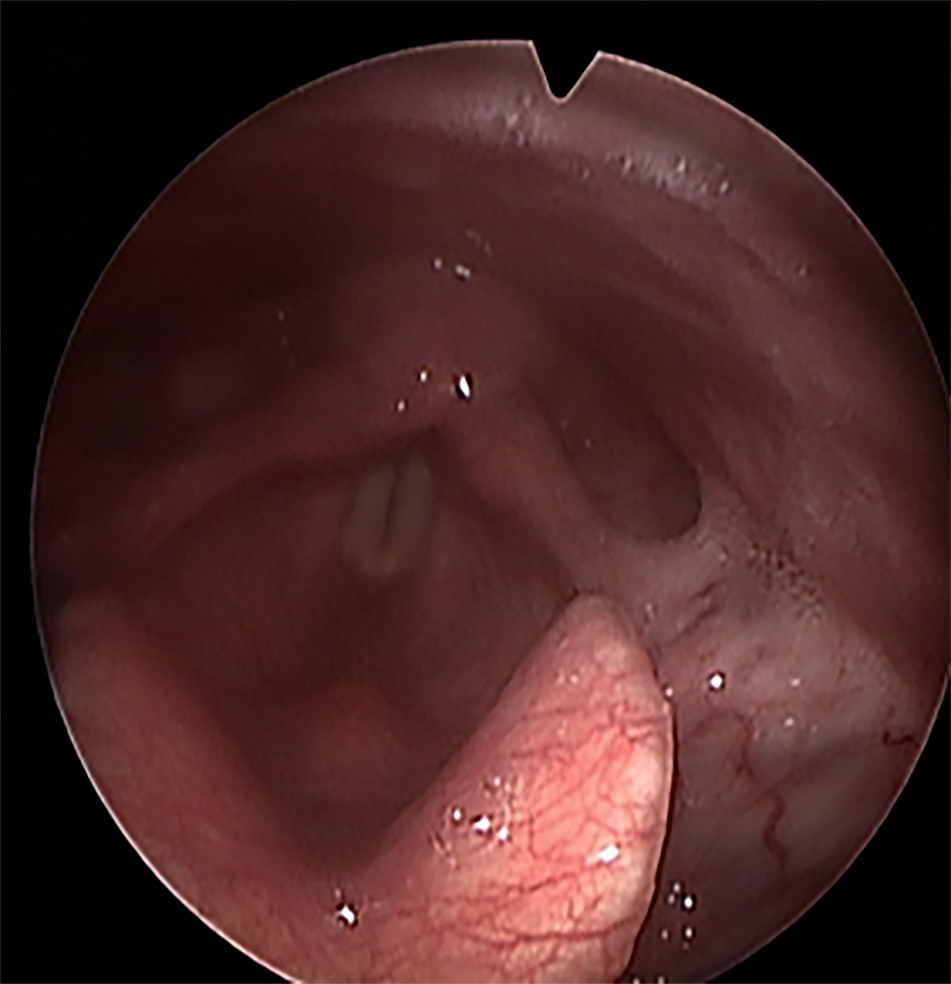
Laryngoscopic examination performed on April 25, 2017, outside our hospital, demonstrated the presence of a submucosal vascular lesion that extended into the epiglottis, left arytenoid cartilage, lateral to aryepiglottic fold, and pyriform sinus. The blue-black-colored mass showed a grape-cluster-like appearance (Figure 1). Computed tomography was performed to determine the depth and extent of invasion of the lesion (12 mm × 15 mm), and to plan for the therapeutic strategies to protect and preserve important anatomical structures (Figure 2).
The patient was diagnosed with a hypopharyngeal hemangioma.
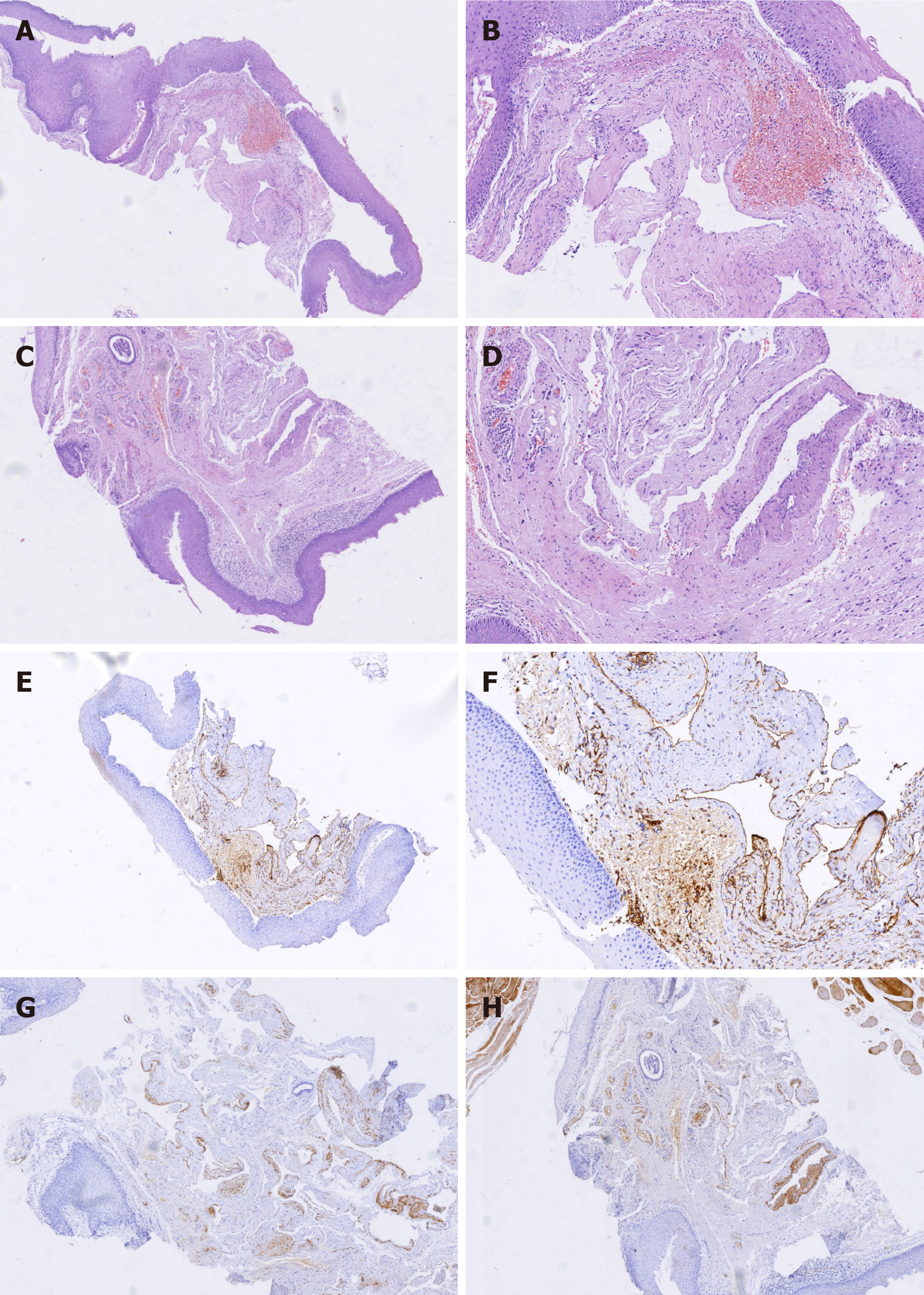
Ensuring limited hemorrhage, the lesion was resected and photocoagulated with Nd: YAG laser on May 4, 2017. The Nd: YAG laser (wavelength of 1064 nm, HGL-MY100C, Huaguang, Wuhan, China) was used in the continuous mode at 7 W. Photocoagulation was performed in a sweeping fashion until visible blanching and involution were observed. The hypopharyngeal hemangioma was completely excised. Moreover, the lesion was resected and sent for histopathological examination. Pathological examination confirmed the tumor to be a cavernous hemangioma (Figure 3). CD31 immunostaining was observed on the walls of the blood vessels (Figure 3E and F), whereas, the smooth muscle of some vessels showed positive immunostaining for desmin (Figure 3G and H). Histological examination showed the presence of vascular hyperplasia and hemangiectasis beneath the squamous mucosa.
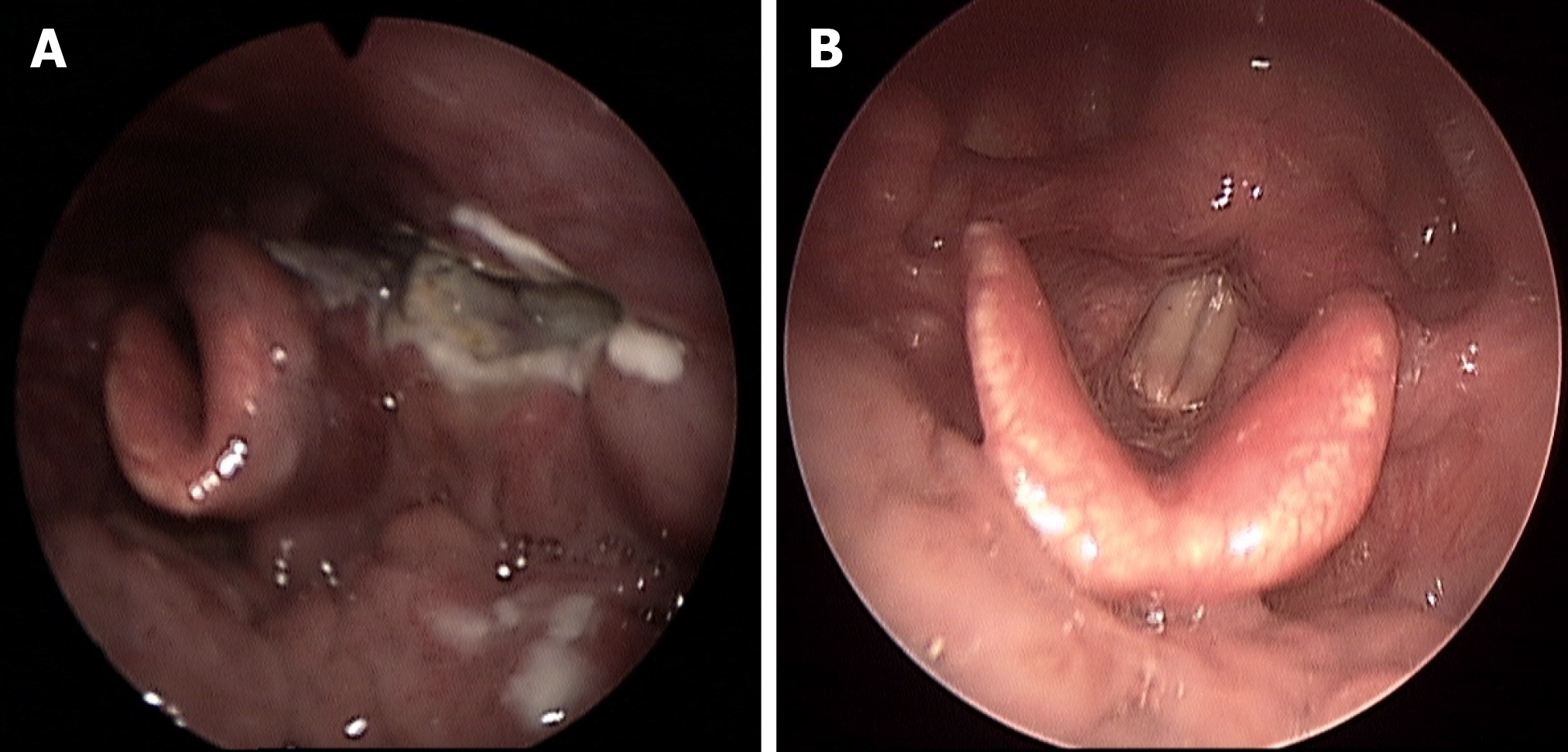
Postoperatively, the patient showed no signs of airway obstruction or bleeding. The patient resumed regular diet from the subsequent day. A video laryngoscopy performed on May 8, 2017 showed reduction of the mucosal edema and good movement of the arytenoid was observed (Figure 4A). Postoperatively, anti-inflammatory medication and symptomatic treatment were administered. The patient was discharged 6 d after surgery.
Forty-seven days after the surgery, an additional video laryngoscopy was performed on June 20, 2017, which showed excellent repair of the arytenoid cartilage mucosal incision (Figure 4B). Furthermore, there was no recurrence of the hypopharyngeal hemangioma at the 1.5-year postoperative follow-up (Figure 5).
The patient did not experience any adverse events from the use of the laser. Excessive bleeding and airway problems were not encountered, and the postoperative pain was limited. The use of Nd: YAG laser provided excellent long-term outcomes and complete symptom resolution without any hemorrhage, and ensured complete healing of the hypopharyngeal areas without any stenosis or scarring.
For cases of hemangiomas, a pathological examination is usually required to make a definitive diagnosis. Currently, depending on the vessel size and vessel wall thickness, hemangiomas can be classified into three histopathological types: Capillary, cavernous, and mixed. The most common type is cavernous, which shows an expanded blood vessel with thin walls[19]. Large hemangiomas require treatment to prevent the development of ulcers, necrosis, or infection of vital organs.
The true pathogenetic mechanism of vascular abnormalities in hemangiomas remains unclear. Various treatment methods have been reported, and the choice of optimal treatment method still remains controversial[20]. The treatment of hemangiomas depends on the primary site and growth phase of the tumor. Barring a few exceptions, surgery should not be the first choice of treatment. It is worth noting that although different laser systems are effective for treating superficial or deep hemangioma, systemic treatment with steroid or β-blockers (still in clinical trials) should assume priority as the first-line treatment. For cases involving the throat or trachea, early treatment is usually required to prevent the occurrence of airway obstruction[20].
Since our findings were obtained from a single case, additional multicenter, randomized controlled trials are needed to confirm the use of YAG laser resection as an effective treatment for hypopharyngeal hemangiomas.
Laser therapy is one of the effective tools for treating hemangiomas with rapid, uncontrolled growth or in functional areas, with few side effects and complications. The present case of a male patient with a large hypopharyngeal hemangioma, treated with YAG laser, demonstrates the efficacy of laser photocoagulation in treating cases of hemangiomas, without the risk of bleeding or airway obstruction. The favorable postoperative outcomes demonstrated by our patient with Nd: YAG laser therapy indicate its consideration in the therapy of similar cases. For cases similar to ours, a complete surgical resection with a YAG laser is recommended.
We would like to acknowledge Dr. Xuan-Guang Ye for preparing the pathology slides and performing photography.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Razek AA, Kupeli S S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Martins RH, Lima Neto AC, Semenzate G, Lapate R. Laryngeal hemangioma. Braz J Otorhinolaryngol. 2006;72:574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Zheng JW, Zhou GY, Wang YA, Zhang ZY. Management of head and neck hemangiomas in China. Chin Med J (Engl). 2008;121:1037-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Yoon SS, Charny CK, Fong Y, Jarnagin WR, Schwartz LH, Blumgart LH, DeMatteo RP. Diagnosis, management, and outcomes of 115 patients with hepatic hemangioma. J Am Coll Surg. 2003;197:392-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 133] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Lin J, Bigge J, Ulbright TM, Montgomery E. Anastomosing hemangioma of the liver and gastrointestinal tract: an unusual variant histologically mimicking angiosarcoma. Am J Surg Pathol. 2013;37:1761-1765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Abe M, Misago N, Tanaka S, Masuoka J, Tabuchi K. Capillary hemangioma of the central nervous system: a comparative study with lobular capillary hemangioma of the skin. Acta Neuropathol. 2005;109:151-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Mundinger GS, Gust S, Micchelli ST, Fishman EK, Hruban RH, Wolfgang CL. Adult pancreatic hemangioma: case report and literature review. Gastroenterol Res Pract. 2009;2009:839730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Crucitti A, La Greca A, Antinori A, Antonacci V, Magistrelli P. Cavernous hemangioma of the gallbladder. Case report and review of the literature. Tumori. 2005;91:432-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Papagiannopoulos K, Sheppard MN, Goldstraw P. Thymic hemangioma presenting with recurrent pleural effusion. Ann Thorac Surg. 2000;70:297-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Willcox TM, Speer RW, Schlinkert RT, Sarr MG. Hemangioma of the spleen: presentation, diagnosis, and management. J Gastrointest Surg. 2000;4:611-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Terada T. Capillary cavernous hemangioma of the lymph node. Int J Clin Exp Pathol. 2013;6:1200-1201. [PubMed] |
| 11. | Zhao J, Shao J, Zhu L, Yu K, Zhao R, Ding W, Zhang J, Han Y. Solitary pulmonary capillary hemangioma: Clinicopathologic and radiologic characteristics of nine surgically resected cases. Pathol Res Pract. 2018;214:1885-1891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Ikeda T, Shimamoto K, Tanji N, Ohoka H, Nishio S, Yokoyama M, Ikeda M. Cavernous hemangioma of the urinary bladder in an 8-year-old child. Int J Urol. 2004;11:429-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Xu HX, Liu GJ. Huge cavernous hemangioma of the adrenal gland: sonographic, computed tomographic, and magnetic resonance imaging findings. J Ultrasound Med. 2003;22:523-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Josephson CB, White PM, Krishan A, Al-Shahi Salman R. Computed tomography angiography or magnetic resonance angiography for detection of intracranial vascular malformations in patients with intracerebral haemorrhage. Cochrane Database Syst Rev. 2014;CD009372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Romano A, Tavanti F, Rossi Espagnet MC, Terenzi V, Cassoni A, Suma G, Boellis A, Pierallini A, Valentini V, Bozzao A. The role of time-resolved imaging of contrast kinetics (TRICKS) magnetic resonance angiography (MRA) in the evaluation of head-neck vascular anomalies: a preliminary experience. Dentomaxillofac Radiol. 2015;44:20140302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Razek AA, Gaballa G, Megahed AS, Elmogy E. Time resolved imaging of contrast kinetics (TRICKS) MR angiography of arteriovenous malformations of head and neck. Eur J Radiol. 2013;82:1885-1891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Kahana A, Lucarelli MJ, Grayev AM, Van Buren JJ, Burkat CN, Gentry LR. Noninvasive dynamic magnetic resonance angiography with Time-Resolved Imaging of Contrast KineticS (TRICKS) in the evaluation of orbital vascular lesions. Arch Ophthalmol. 2007;125:1635-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Huang CM, Lee KW, Huang CJ. Radiation therapy for life-threatening huge laryngeal hemangioma involving pharynx and parapharyngeal space. Head Neck. 2013;35:E98-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Abrahamson J, Shandling B. Intestinal hemangiomata in childhood and a syndrome for diagnosis: a collective review. J Pediatr Surg. 1973;8:487-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Zheng JW, Zhou Q, Yang XJ, Wang YA, Fan XD, Zhou GY, Zhang ZY, Suen JY. Treatment guideline for hemangiomas and vascular malformations of the head and neck. Head Neck. 2010;32:1088-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (1)] |