Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.806
Peer-review started: October 1, 2019
First decision: November 4, 2019
Revised: December 11, 2019
Accepted: December 14, 2019
Article in press: December 14, 2019
Published online: February 26, 2020
Processing time: 148 Days and 0.9 Hours
Situs inversus totalis (SIT) is a rare congenital anomaly that refers to a completely reversed location of abdominal and thoracic organs. An extremely small number of patients with this condition, especially those with rectal neoplasms, have been reported. Surgery in these patients is technically challenging. Therefore, we reconstructed a three-dimensional (3D) digital model with the Materialise’s interactive medical image control system (Mimics) as a guide for laparoscopic resection.
We report the case of a 68-year-old woman with rectal neoplasms and SIT diagnosed by electronic colonoscopy biopsy and enhanced computed tomography (CT), which showed that there was a soft tissue mass protruding into the lumen in the lower rectal segment, a lesion that involved the serosal layer, multiple enlarged peripheral lymph nodes, and visceral situs abnormalities. Based on the CT images, we reconstructed a 3D model with Mimics to assist with our surgical planning. Then, we performed laparoscopy-assisted radical resection of the rectal neoplasms and total excision of the lesion. Adjuvant chemotherapy with the XELOX regimen (oxaliplatin 150 mg, D1 + Xeloda 1.0 g, Bid, D1-14) was initiated 1 mo after the operation. The patient recovered well after surgery, and her physical condition remained stable.
Preoperative 3D reconstruction of the imaging results could help reduce the unknown risks during surgery caused by anatomical abnormalities and improve the perioperative safety for patients.
Core tip: This case is the first to use the Materialise’s interactive medical image control system (Mimics) to reconstruct a three-dimensional (3D) model using computed tomography images of a patient with situs inversus totalis and rectal neoplasms, which helped to get a better understanding of anatomical structures and make preoperative plans. The more details of anatomy surgeons grasp, the less operating time is needed, and this could improve the quality of surgery and thereby enhance the perioperative safety of patients. Mimics is easy to operate and visually displays 3D anatomical structure, which shows advantages in patients with rare anatomical changes.
- Citation: Chen T, Que YT, Zhang YH, Long FY, Li Y, Huang X, Wang YN, Hu YF, Yu J, Li GX. Using Materialise's interactive medical image control system to reconstruct a model of a patient with rectal cancer and situs inversus totalis: A case report. World J Clin Cases 2020; 8(4): 806-814
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/806.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.806
Situs inversus totalis (SIT), also termed situs inversus viscerum, is a rare congenital anatomic abnormality of the human viscera with an incidence of 0.01% to 0.1% in the normal population. The whole internal organs of SIT patients, including the heart, lungs, septum transversum, liver, spleen, stomach, and intestines, are inverted by 180 degrees to present an approximately mirror image of the anatomy of a typical person. This condition is occasionally discovered unintentionally during check-up examinations. Although this condition does not affect normal health or longevity, the recognition of this anomaly is vital to treating many diseases, especially for patients who require surgical invention[1].
To get better acquainted with the aforementioned condition, Materialise's interactive medical image control system (Mimics, Materialise Co., Leuven, Belgium), into which the Digital Imaging and Communications in Medicine computed tomography (CT) images are put, can be used to reconstruct the three-dimensional (3D) models of target organs. This technology can visually display and accurately locate the anatomical structure, which is conducive to the formulation and implementation of the surgical program.
This case information is organized into a timeline presented in Table 1.
| Date | Clinical treatment course |
| August 6, 2018 | The patient reported intermittent bloody stool for approximately 6 mo that became aggravated in recent days. And then, the patient underwent a physical examination, in which digital rectal examination revealed that a mass was about 5 cm above the anal verge, and the tip of the glove was stained with blood |
| August 16, 2018 | Abdominopelvic contrast-enhanced computed tomography scans revealed that a soft tissue mass, approximately 4.5 cm from the lower rectum to the anus, was irregularly infiltrated into the serous membrane. The mass was seen to protrude into the lumen, with metastatic lymph nodes detected around. Colonoscopy showed a palpable encircling mass in the lower rectum, 10-13 cm above the anal verge. Part of the mass was sent for biopsy |
| August 20, 2018 | After hospitalization, relevant examinations were further made to the patient to clarify the diagnosis. Laboratory findings showed that the occult blood test was positive, plasma D-dimer level was 0.81 mg/L fibrinogen equivalent unit, and the potassium ion concentration in serum was 3.48 mmol/L |
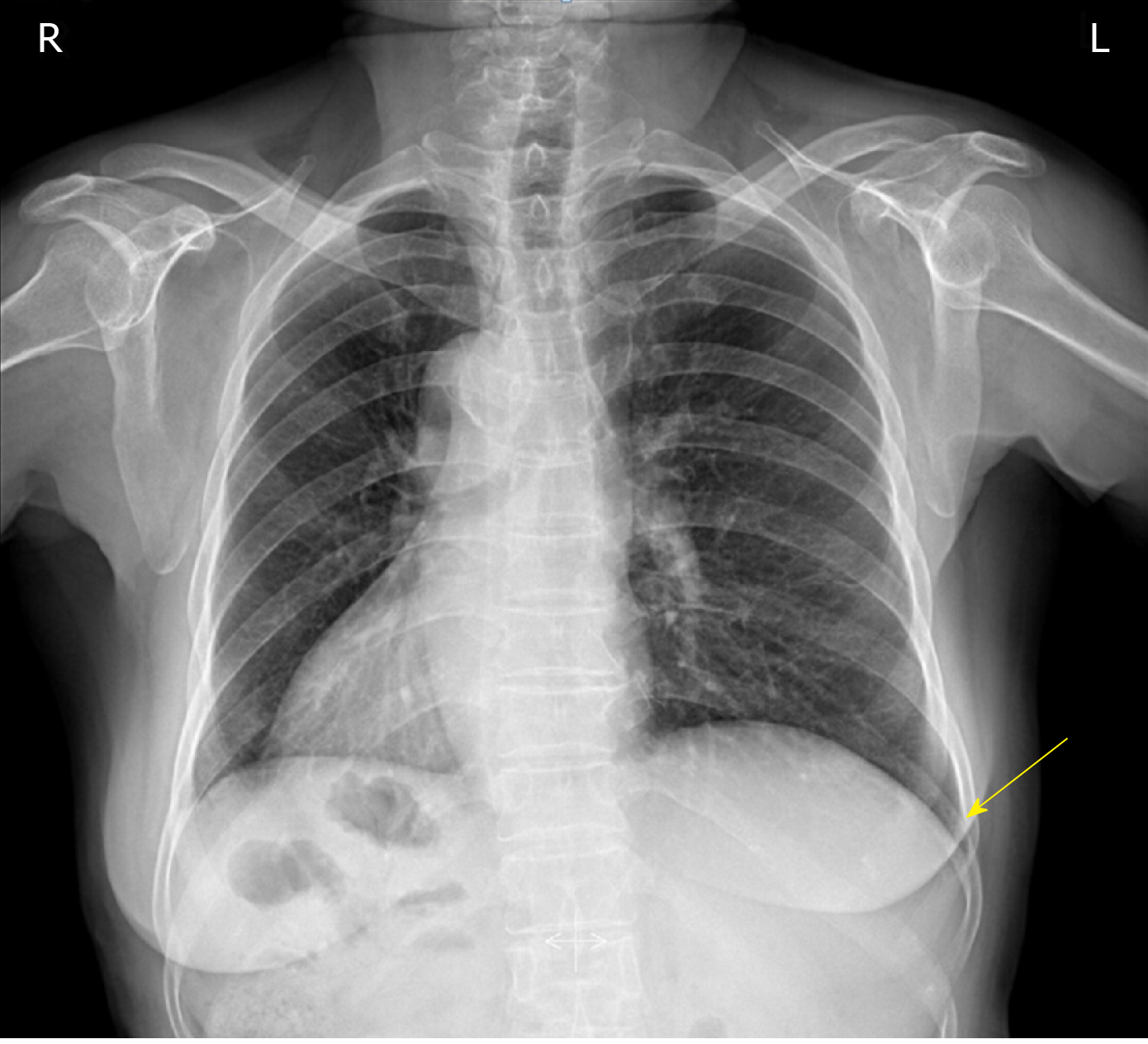
| August 21, 2018 | Chest posterior-anterior radiograph and electrocardiographic examination showed dextrocardia |
| August 23, 2018 | MRI scans (3.0T) revealed that a soft tissue mass, approximately 70 mm from the lower rectum to the anus, was irregularly infiltrated into the serous membrane. The mass was seen to protrude into the lumen, with metastatic lymph nodes detected around. No absolute operation contraindication was found in the preoperative examinations. Before surgery, we reconstructed a 3D model of organs with Mimics, which helped preoperative plans. Laparoscopy-assisted radical resection of rectal cancer with distal ileostomy was performed successfully under general anesthesia |
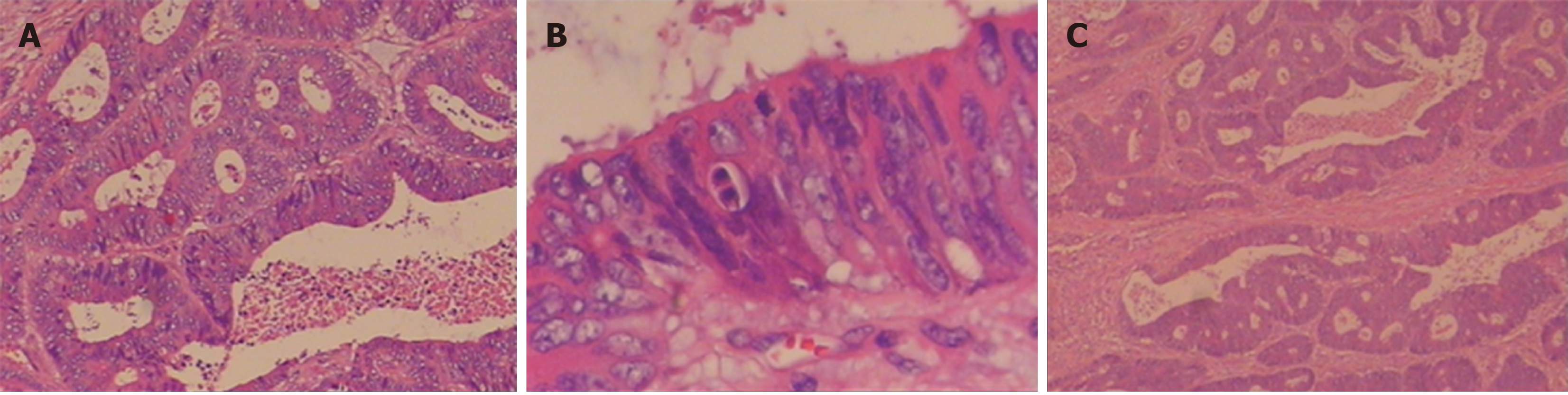
| August 28, 2018 | Postoperative pathological examination showed differentiated colorectal adenocarcinoma invading into the full wall of the bowel. No cancer residues were found in the incised edge of either side, and the circumferential edge was 1 mm away from the tumor. The lymph nodes (LN1, LN2, and LN3) showed no metastasis of the tumor tissue (0/16, 0/8, and 0/6) |
| September 29, 2018 | Adjuvant chemotherapy with the XELOX regimen (oxaliplatin + Xeloda) was initiated 1 mo after the operation. The patient recovered well after surgery, and her physical condition remains stable |
A 68-year-old Chinese Han woman with a clear medical history was admitted to our hospital because she reported intermittent bloody stool for approximately 6 mo that had become aggravated for nearly 11 d.
Proximately 6 mo ago, it was found that there was bright red blood at the end of the stool with no obvious incentive for defecation. There was no chills, high fever, nausea, vomiting, abdominal pain, or diarrhea.
The patient’s family history was unremarkable.
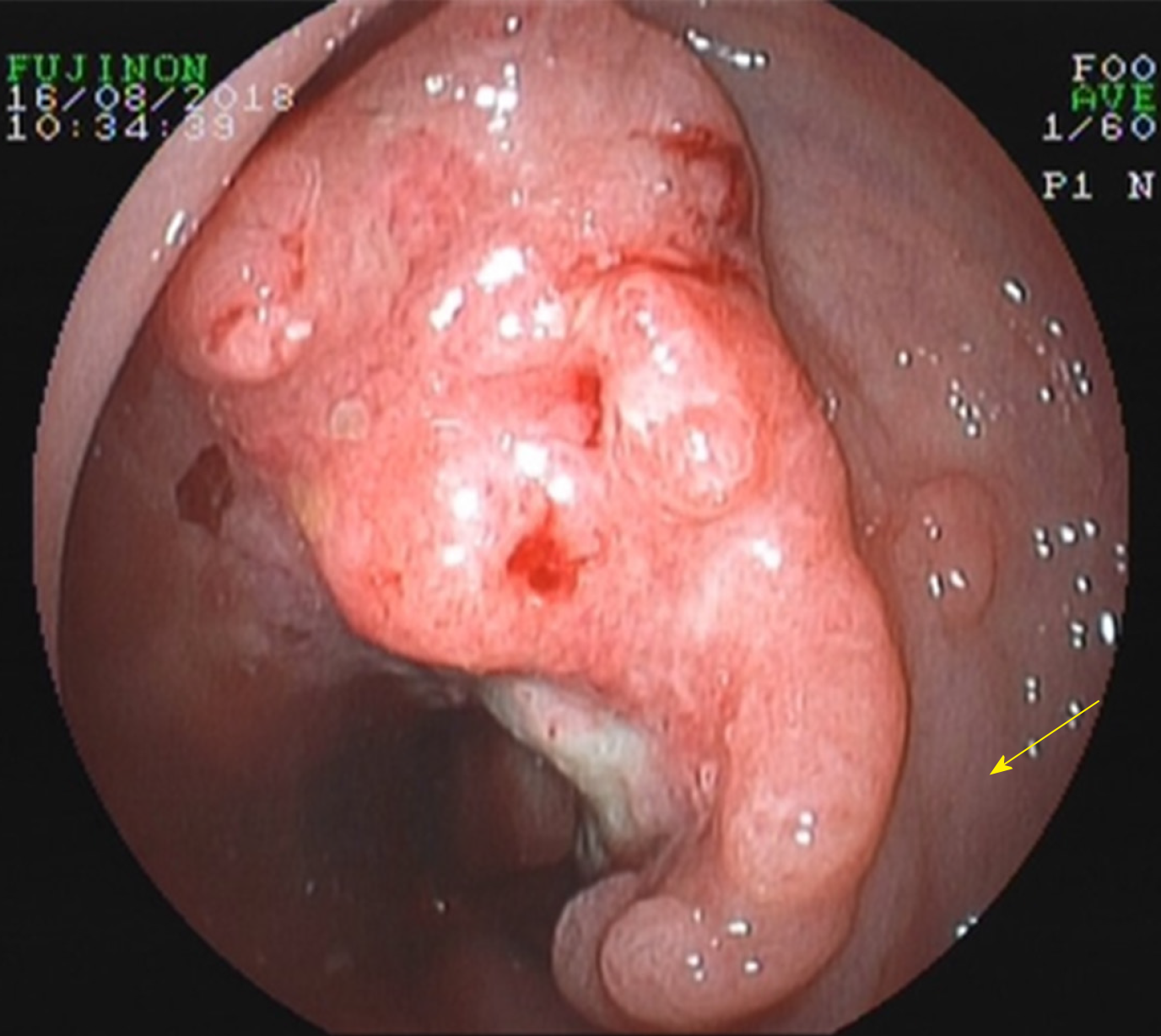
Digital rectal examination revealed that a mass was about 5 cm above the anal verge and the tip of the glove was stained with blood. A palpable encircling mass was found in the lower rectum, 10-13 cm above the anal verge, on colonoscopy (Figure 1). Part of the mass was sent for biopsy and pathology confirmed the presence of moderately differentiated adenocarcinoma from a biopsy specimen (Figure 2). Chest posterior-anterior radiograph (Figure 3) and electrocardiographic examination showed dextrocardia.
The occult blood test was positive. Plasma D-dimer level was 0.81 mg/L fibrinogen equivalent unit, and potassium ion concentration in serum was 3.48 mmol/L.
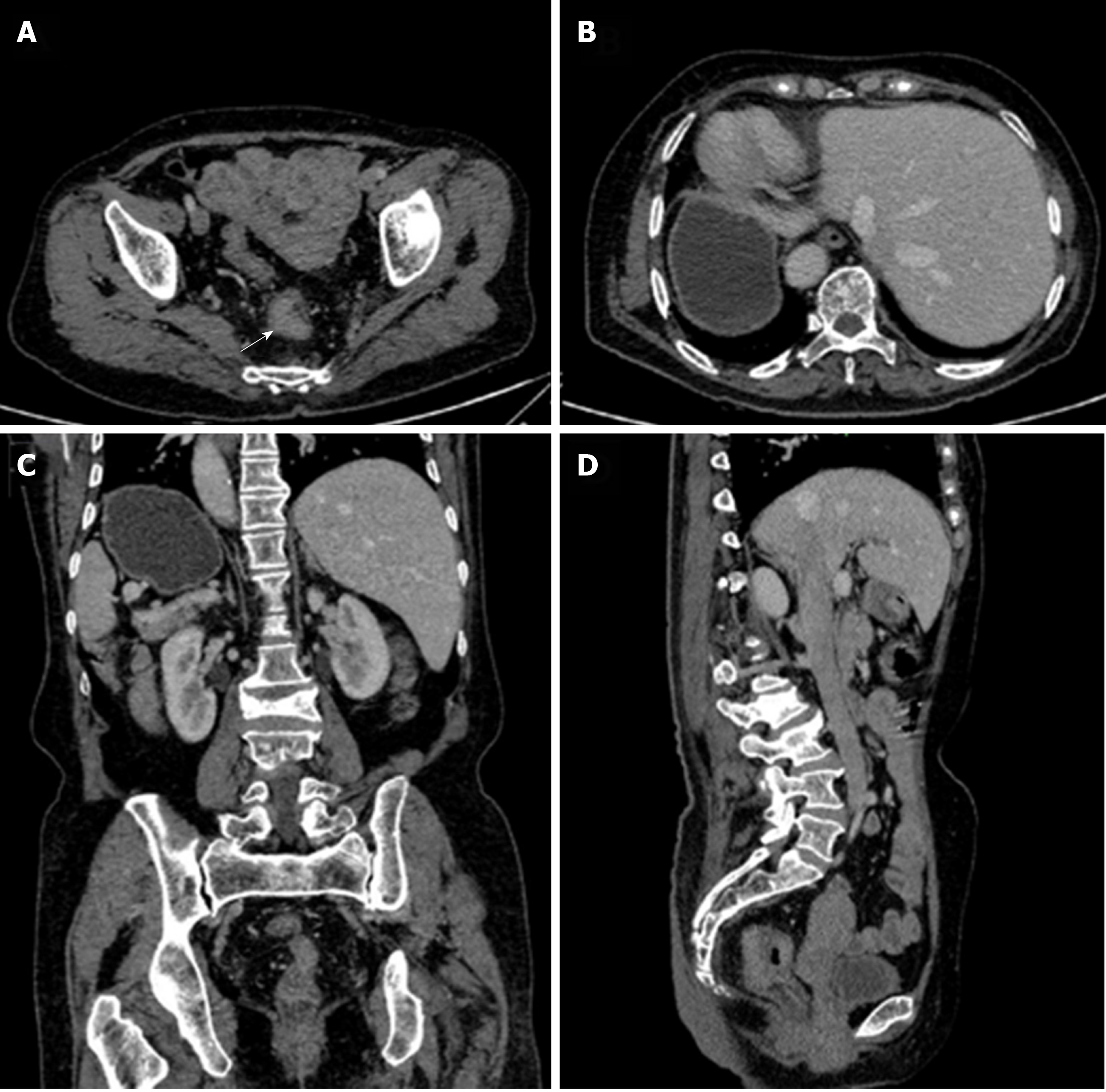
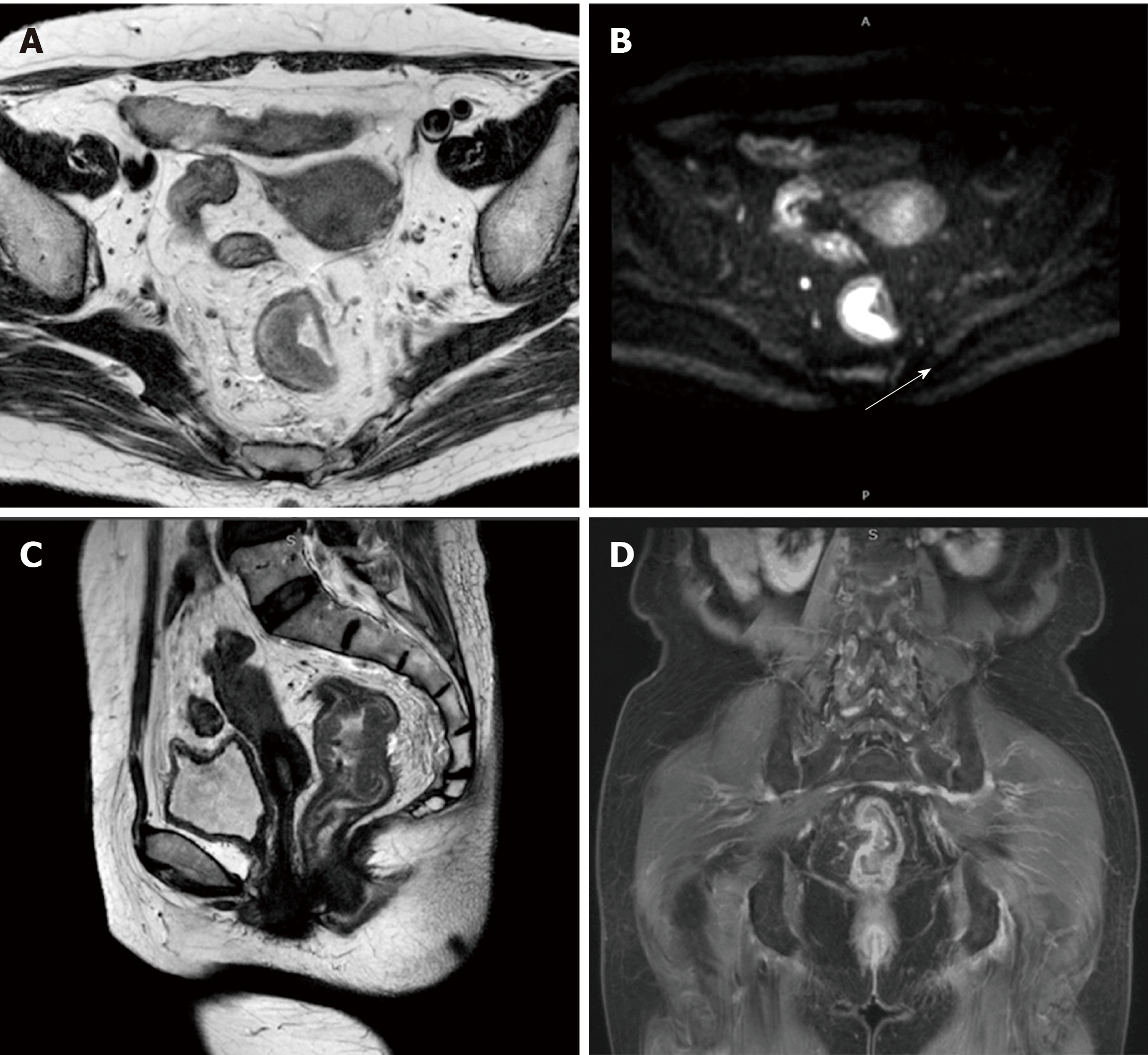
Abdominopelvic contrast-enhanced CT scans revealed that a soft tissue mass, approximately 4.5 cm from the lower rectum to the anus, was irregularly infiltrated into the serous membrane. The mass was seen to protrude into the lumen, with metastatic lymph nodes detected around. CT further revealed the complete transposition of the abdominal viscera, indicating SIT (Figure 4). Magnetic resonance imaging (MRI) scans (3.0T) revealed that a soft tissue mass, approximately 70 mm from the lower rectum to the anus, was irregularly thickened (Figure 5) and was seen to protrude into the lumen.
Malignant rectal tumor (cT3aN2Mx), ascending colon polyp, and SIT with no absolute contraindication.
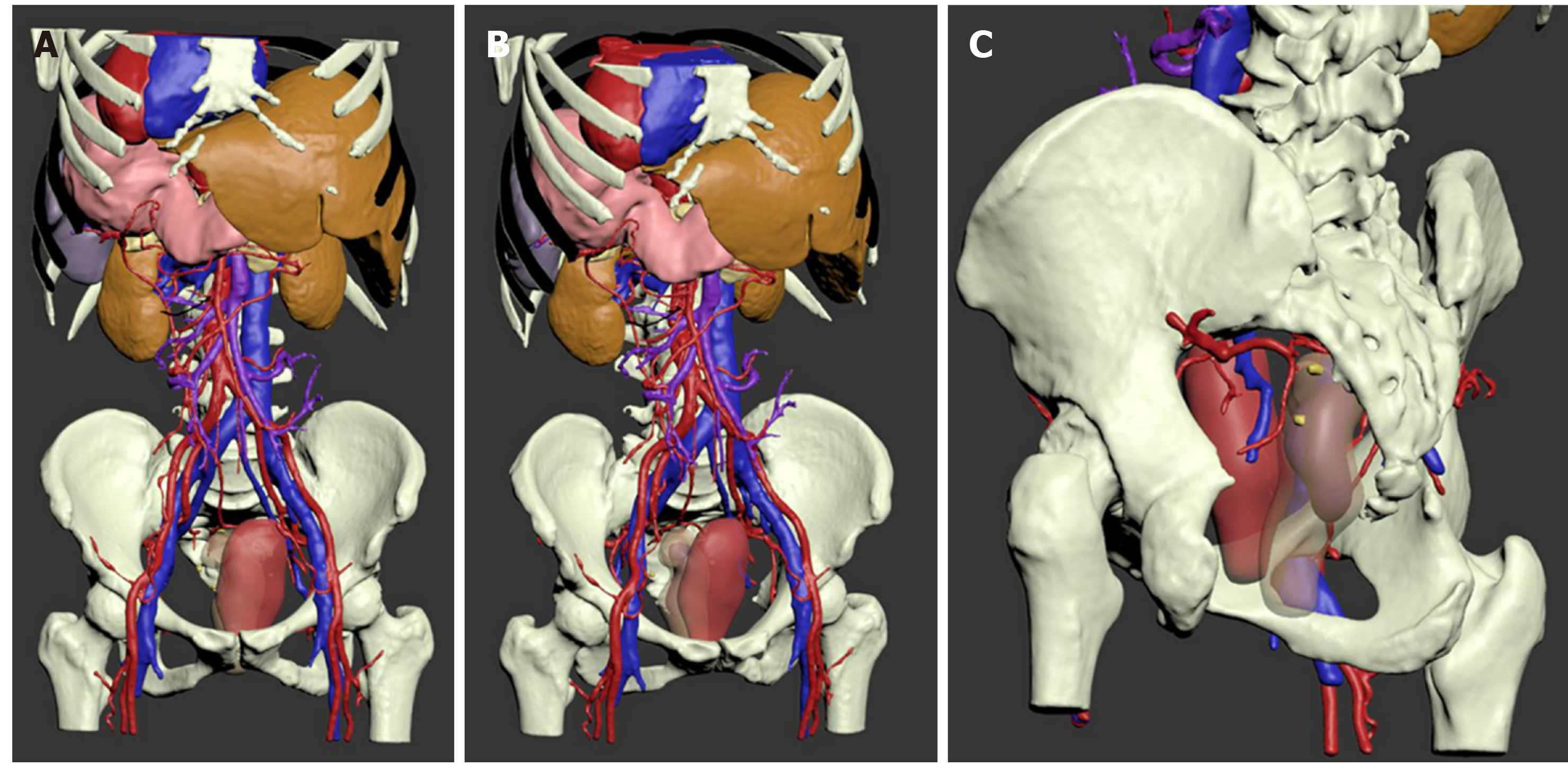
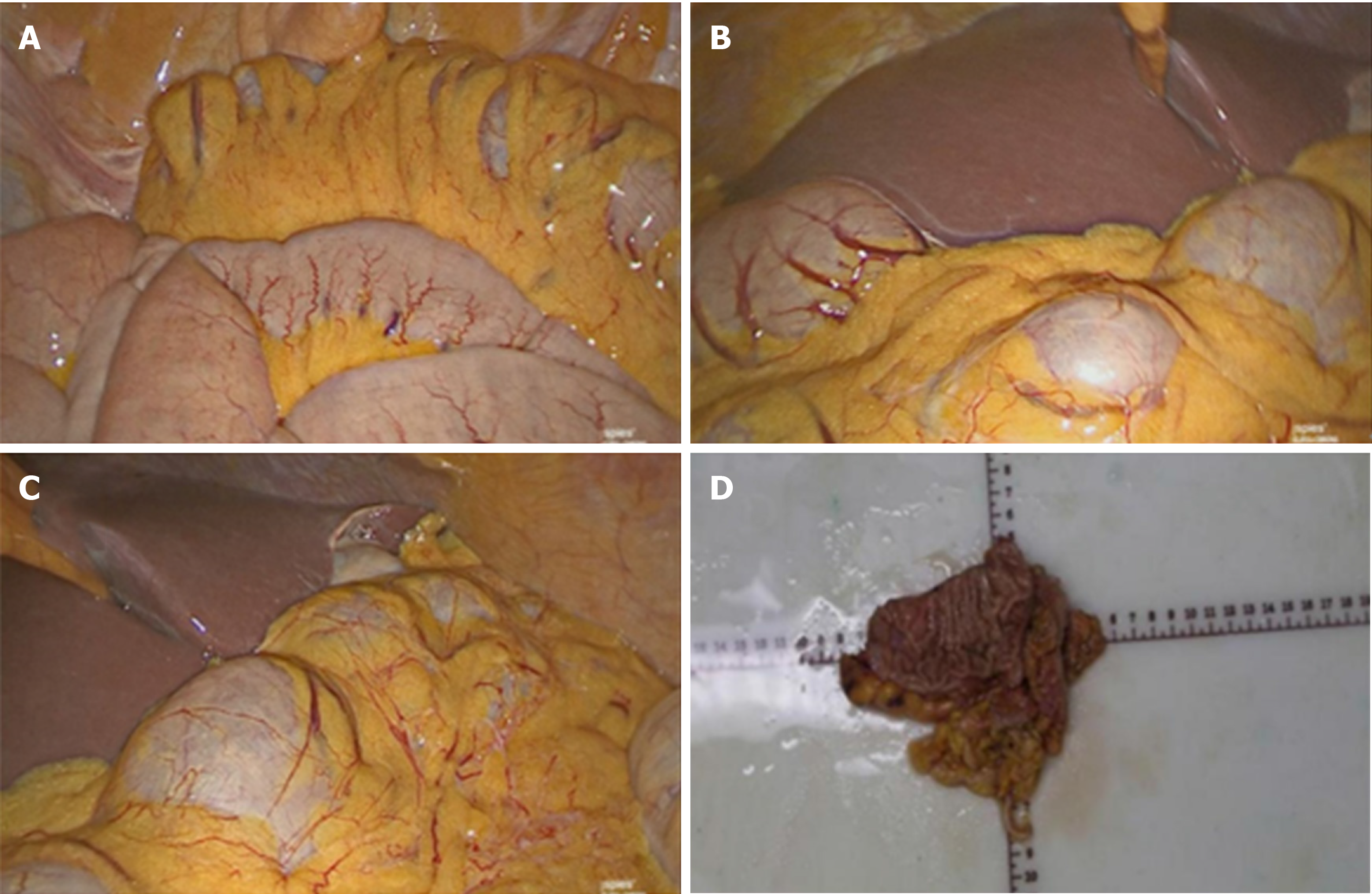
No absolute surgical contraindication was found in the preoperative examinations. Before surgery, we imported the Digital Imaging and Communications in Medicine CT images into Mimics. According to the characteristic CT value range of each organ, we carried out thresholding, masking, segmentation, and boundary dressing to restore each anatomical structure, then a 3D virtual model was generated. Combined with CT images, a furthermore profound understanding of lesion and the surrounding structures of the patient was available (Figure 6). Laparoscope-assisted radical resection of rectal cancer (Figure 7) with distal ileostomy was performed successfully under general anesthesia. Postoperative pathological examination suggested differentiated colorectal adenocarcinoma invading into the full wall of the bowel. No cancer residues were found in the incised edge of either side, and the circumferential edge was 1 mm away from the tumor. The lymph nodes (LN1, LN2, and LN3) showed no metastasis of the tumor tissue (0/16, 0/8, and 0/6). The postoperative condition of the patient was generally good without obvious discomfort (Figure 7). Adjuvant chemotherapy with the XELOX regimen (oxaliplatin 150 mg, D1 + Xeloda 1.0 g, Bid, D1-14) was initiated 1 mo after the operation. Assisted acid-inhibiting and stomach-protecting medicine and injection of recombinant human granulocyte stimulating factor to enhance immunity were administered.
The patient recovered well after surgery, and her physical condition remains stable.
Traditionally, surgeons have used ultrasound, CT, or MRI scans to visualize and simulate the anatomy of a patient for reference. The quality of the surgical procedure depends on the surgeon's own clinical experience. Moreover, the application and promotion of laparoscopic gastrointestinal surgery are limited due to the complex structure of the peritoneal vessels and multiple anatomical variations caused by lymph node dissection. For the sake of solving the problems above, Mimics 20.0 (from Materialise NV) was used to reconstruct a 3D model of abdominal organs and blood vessels of the patient through the delineation and segmentation of tissues and organs and to provide an objective basis for surgeons to design and optimize the surgical scheme. Li et al[2] provided that 3D models can better help doctors be familiar with anatomical information, develop personalized surgery plans, and reduce the learning time of young doctors on special anatomical structures.
Until 2001, Bilimoria et al[3] from the United States counted only 14 patients worldwide with all internal organs reversed complicated with malignant tumors, and none of the patients had reported rectal cancer. So far, only three cases of rectal cancer complicated with SIT in the whole chest and abdomen have been reported in the literature; this report highlights the fourth case, as shown in Table 2.
SIT is a rare anomaly in which the abdominal and thoracic cavity structures are located opposite to their usual positions and has an incidence of 1/10000-50000 persons[4]. This anomaly is not a premalignant condition. Most SIT patients can continue to live a normal life, but some may develop severe lung disease (bronchiectasis, unilateral lung defect), cardiovascular system abnormalities (ventricular septum, intra-atrial defects), and digestive system abnormalities (duodenal stenosis, atresia). The etiologic nature of this anomaly is not known. Some authors believe that this condition is related to familial genetic factors. However, other authors believe that changes in chromosome structure or number, unusual nucleotide arrangements, or mutations in DNA molecules can be the underlying cause of developmental abnormalities in embryos[7]. Some experts believe that in the 4th week of embryonic development, if the intestinal loop is reversed clockwise with the supratentorial artery as the axis, or if the intestinal loop is not translocated after returning from the umbilical cord, retroversion of the abdominal situs inversus will occur[3].
Fabricius first reported cases of SIT in 1600, and the first case of SIT in China was reported by Peking Union Medical College Hospital in 1928. Due to the low incidence of SIT, patients with this abnormality and malignancy are very rare. Only nine SIT patients with laparoscopic surgery were reported[8].
This report is the first case to use 3D reconstruction with Mimics to analyze the anatomical features of a patient with both SIT and rectal cancer. The anatomical descriptions from surgery confirmed that all of the mirrored anatomical features are consistent with the 3D modeling images displayed by the system before laparoscopic surgery. Nanfang Hospital of Southern Medical University has applied laparoscopic surgical navigation based on Mimics to some routine laparoscopic surgeries for stomach cancer. This procedure is designed to reduce the risk of bleeding and abdominal organ damage during surgery that arise from limited vision and unknown anatomical features before laparoscopic surgery.
Visceral inversion in SIT patients may also be accompanied by major vascular abnormalities, which will increase the operative time and the probability of complications[9-11]. Therefore, careful preoperative anatomical evaluation is very important, especially for laparoscopic surgery[6].
SIT is a rare disease, but it begins to appear more frequently, and we ought to pay more attention to it. It is necessary to share and learn about the surgical experience with this disease. Based on the above case report, we would like to provide some advice for other clinicians: 3D reconstruction of the imaging result with Mimics can help to enhance the surgeon’s understanding of patients with abdominal viscera and tumor lesions, and planning and evaluation for the operation in order to reduce the operation process of anatomic abnormalities caused by unpredictable risks. Meanwhile, we could get prepared to make preoperative psychological and equipment. Less operation time would improve the perioperative safety of the patients. In addition, the 3D model can be used to visually teach and guide the operation of an entire team, in the late, for young doctors learning about rare cases. As reusable and collectable digital data, it can also be shared online, providing more learning opportunities for surgeons in every region.
Preoperative 3D reconstruction of the imaging results could help reduce the unknown risks during surgery caused by anatomical abnormalities and improve the perioperative safety for patients.
We would like to appreciate those who devoted their efforts and time into this case, and also helpers who provided suggestions and support to us.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Akbulut S, Filippou D, Rungsakulkij N S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Ma YJ
| 1. | Blegen HM. Surgery in Situs Inversus. Ann Surg. 1949;129:244-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Li J, Lin J, Xu J, Meng H, Su N, Fan Z, Li J, Yang Y, Li D, Wang B, Fei Q. A Novel Approach for Percutaneous Vertebroplasty Based on Preoperative Computed Tomography-Based Three-Dimensional Model Design. World Neurosurg. 2017;105:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Bilimoria MM, Parsons WG, Small W, Talamonti MS. Pancreaticoduodenectomy in a patient with ampullary carcinoma and situs inversus. Surgery. 2001;130:521-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Huh JW, Kim HR, Cho SH, Kim CY, Kim HJ, Joo JK, Kim YJ. Laparoscopic total mesorectal excision in a rectal cancer patient with situs inversus totalis. J Korean Med Sci. 2010;25:790-793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Choi SI, Park SJ, Kang BM, Lee KY, Lee HC, Lee SH. Laparoscopic abdominoperineal resection for rectal cancer in a patient with situs inversus totalis. Surg Laparosc Endosc Percutan Tech. 2011;21:e87-e90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Fang JF, Zheng ZH, Wei B, Chen TF, Lei PR, Huang JL, Huang LJ, Wei HB. Laparoscopic resection for rectal cancer and cholecystectomy for patient with situs inversus totalis. J Minim Access Surg. 2015;11:210-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Niikawa N, Kohsaka S, Mizumoto M, Hamada I, Kajii T. Familial clustering of situs inversus totalis, and asplenia and polysplenia syndromes. Am J Med Genet. 1983;16:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 69] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Sasaki K, Nozawa H, Kawai K, Hata K, Kiyomatsu T, Tanaka T, Nishikawa T, Otani K, Kaneko M, Emoto S, Murono K, Watanabe T. Laparoscopic hemicolectomy for a patient with situs inversus totalis: A case report. Int J Surg Case Rep. 2017;41:93-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Kim YW, Ryu H, Kim DS, Kim IY. Double primary malignancies associated with colon cancer in patients with situs inversus totalis: two case reports. World J Surg Oncol. 2011;9:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Yazar FM, Emre A, Akbulut S, Urfalıoğlu A, Cengiz E, Sertkaya M, Yıldız H, Bülbüloğlu E. Laparoscopic Sleeve Gastrectomy in Situs Inversus Totalis: a Case Report and Comprehensive Literature Review. Indian J Surg. 2016;78:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |