Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.4895
Peer-review started: May 8, 2020
First decision: July 25, 2020
Revised: August 16, 2020
Accepted: September 10, 2020
Article in press: September 10, 2020
Published online: October 26, 2020
Processing time: 171 Days and 7.1 Hours
Hutch diverticulum arises from the compromised muscular development at the ureteral orifice. It is a congenital disease and extremely rare in adult, only accounting for about 3% occurrence worldwide. It can be either symptomatic or asymptomatic, and relies on image tools for diagnosis and preoperative planning. Indications for surgery are dependent on the complications from the diverticulum. Metaplasia is about 10% among those with hutch diverticulum, and it still has chances turning into malignancy, especially urothelial cell carcinoma.
A 27-year-old man was presented with frequently recurrent urinary tract infection for one year, and had suffered from intermittent right flank pain for 3 mo. No past medical histories were recorded before. No obvious abnormalities on laboratory data and urine examination were found. Under ultrasound, right hydronephrosis was seen and an anatomical abnormality was observed on intravenous pyelography. Further computed tomography urogram showed one diverticulum seated at superolateral side of right ureteral orifice. Cystoscopy was done and biopsy results showed focal metaplasia. After discussing with him, robotic-assisted diverticulectomy with reconstruction was performed. Right hydronephrosis was greatly improved after surgery. He has completed his 1.5-year follow-ups, and no malignancies were seen from urine cytology and image of intravenous pyelography.
Robotic-assisted diverticulectomy and reconstruction to hutch diverticulum is a safe and efficient operation, providing several advantages over open and laparoscopic ones.
Core Tip: Hutch diverticulum is an uncommon congenital anatomical defects in childhood, involving bladder and ureteral opening. Mostly cases are diagnosed in their first decades and predominately at solitary side. The symptoms prompting one to seek help at clinics include recurrent urinary tract infection, colic flank pain, and hematuria. If hutch diverticulum comes into existence, it will enlarge with every-time voiding. Indications for operation are dependent on complications from it or suspicious of malignant changes. Size of diverticulum and its anatomical complexities mainly determine the intricacies of the surgery. In our experiences, robotic-assisted surgery provides several advantages over open and laparoscopic ones.
- Citation: Yang CH, Lin YS, Ou YC, Weng WC, Huang LH, Lu CH, Hsu CY, Tung MC. Adult metaplastic hutch diverticulum with robotic-assisted diverticulectomy and reconstruction: A case report. World J Clin Cases 2020; 8(20): 4895-4901
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/4895.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.4895
Hutch diverticulum arises from the site where the ureteral ostium joins the bladder. The pathological mechanism is thought to be that the muscular development around the ureteral orifice, where Waldeyer’s sheath grows and goes into the bladder, is compromised or fails. Hutch diverticulum is an extremely rare congenital disease that occurs in children and, especially, adults. It is usually diagnosed during the first 10 years in childhood, predominantly in male and at the solitary site, as a characteristic of congenital disease. Any congenital diseases causing defective muscular or connective tissue development, such as occipital horn syndrome, prune belly syndrome, and ehlers-danlos syndrome, increases the risk of acquiring hutch diverticulum[1]. However, the eldest reported case was documented to be a 83-year-old patient[2], which suggests that this disease may also be diagnosed in the elderly[3]. Aside from male cases, it could be found in female patients as well[4]. If the diverticulum exists, it will enlarge with voiding every single time, and will further cause related symptoms and signs.
Although it might be asymptomatic and accidentally found, the most common symptoms of hutch diverticulum are recurrent urinary tract infection (UTI), hydronephrosis, colic flank pain, hematuria, and other abnormal urodynamic occasions, like lower urinary tract symptoms and obstructive uropathy. Generally, hutch diverticulum possess less than 3% occurrence worldwide, and there are only seven published adult cases available on PubMed in the past 10 years. Complications brought by hutch diverticulum, like symptomatic stone formation, diverticulum rupture, bothersome recurrent UTI, or other deteriorating conditions, are indicative of operation[5,6]. Acute episodes sometimes occur in patients with special underlying conditions, such as history of substances abuse[7]. Malignant changes are rarely reported, only accounting for less than 5% of patients and without specific documented predisposing factors. Metaplasia is seldom observed, and the occasion involving the surrounding organs is especially extremely rare[8].
A 27-year-old man complained of frequently recurrent urinary tract infection for one year.
He had visited local medical doctors a lot for the past one year, receiving oral antibiotics for his recurrent urinary tract infection. The frequency he described was around once a month. Fever was occasionally accompanied with it. It would have response to antibiotics therapies at first with quick resolution of symptoms, but the disease-free interval became shorter and shorter for the recent 3 mo, with exaggerating flank colicky pain.
None.
His temperature was 35.1°C, and heart rate was 74 bpm. Respiratory rate was 16 breaths per minute, and blood pressure was 147/64 mmHg. Oxygen saturation in room air was 98%. Knocking pain at right costovertebral angle was obvious when performing physical examination.
Complete blood cell (white blood cell: 7400/UL; red blood cell: 5270000/UL; hemoglobulin: 16.0 g/DL) and renal functions tests (creatinine: 0.81 mg/DL; blood urea nitrogen: 14 mg/DL) were all within normal range. No evidence of urinary tract infection and hematuria (white blood cell: 0/HPF; leukocyte esterase: Negative; nitrites: Negative; red blood cell: 0/HPF) from urine examination, and no abnormalities were observed from urine cytology.
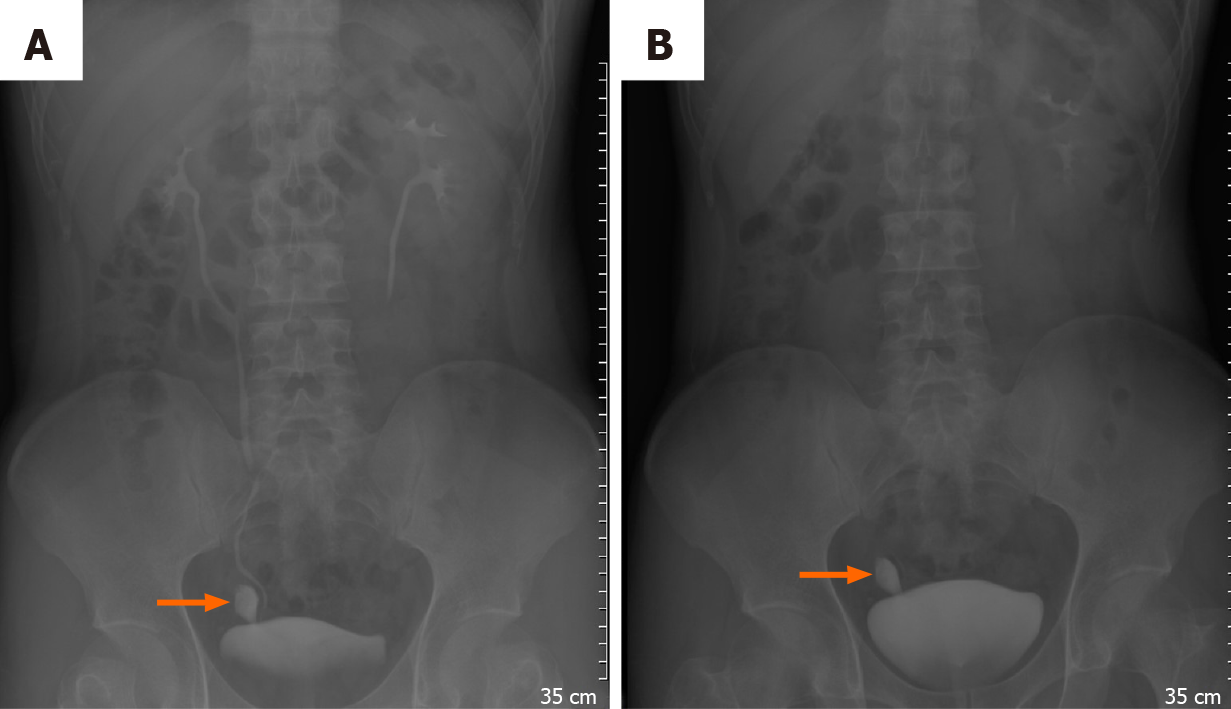
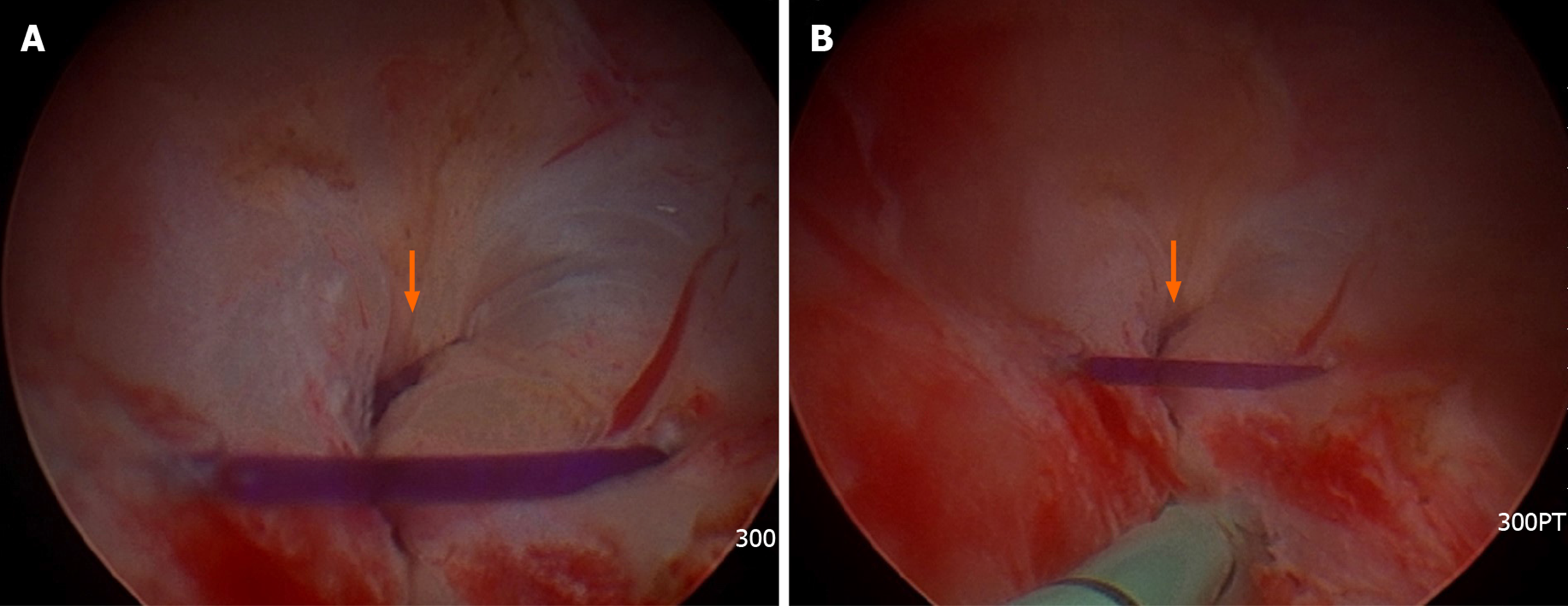
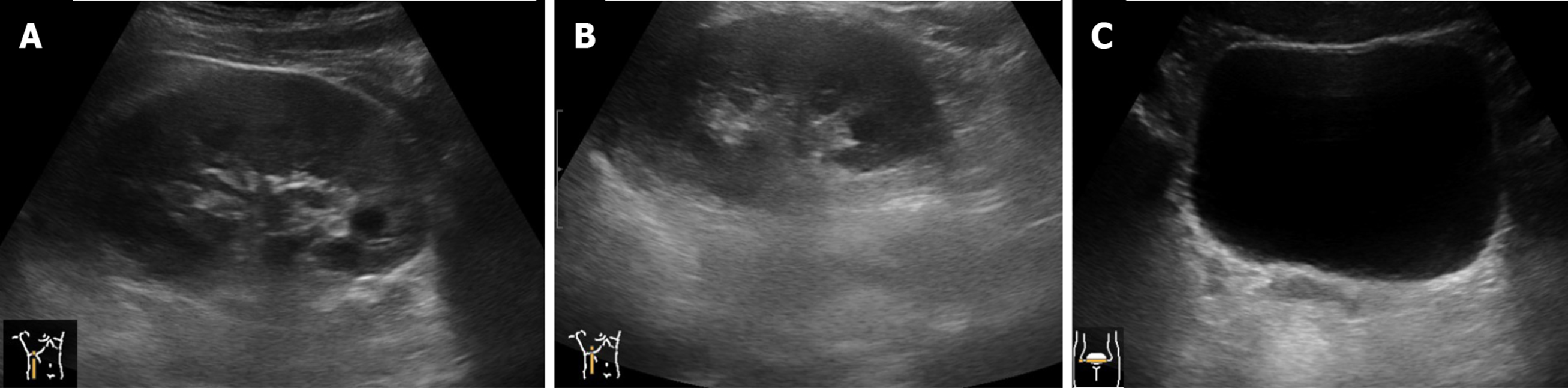
Under renal ultrasound, a right hydronephrosis was seen. Thereafter, an intravenous pyelography (IVP) (Figure 1) was administered, and a well-defined contrast-filling object was seen. Bladder rupture, ureteral tear, or anatomical abnormalities all could be included in differential diagnosis. Contrast retention in this object was evident on the 30-min IVP. The computed tomography urogram revealed a diverticulum near the right ureteral orifice, seated superolateral to the right ureterovesical junction. An ostium of diverticulum could be seen entering into the bladder (Figure 2), and hutch diverticulum was thereby diagnosed.
The final diagnosis of this case is adult type hutch diverticulum with focal squamous metaplasia.
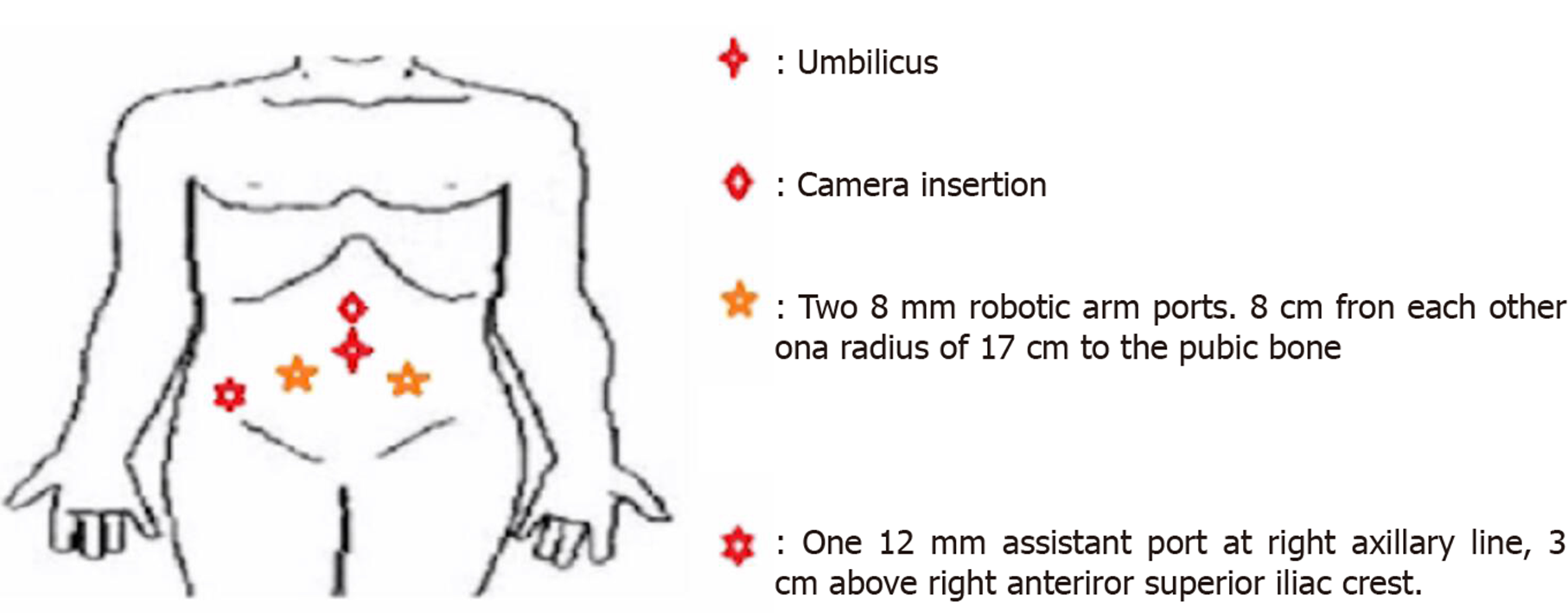
One month later, a robotic-assisted diverticulectomy with reconstruction was then performed under the indication of metaplasia change from biopsy and symptomatically recurrent UTI. Prior to surgery, we instilled 300 mL normal saline via cystoscopy into the diverticulum to bulge it out. Thereafter, he was positioned in a trendelenburg position about 30 degrees (Figure 3). The camera was placed right above the umbilicus, and two 8 mm robotic ports were placed at both sides of the camera port, with 8 cm from each on a radius of 17 cm to the pubic bone. A 12 mm assistant port was settled along the right axillary line, 2 cm above the anterior superior iliac crest (Figure 4). The operation was began with transperitoneal route. After identifying the right seminal vesicle, the diverticulum was seen by tracing lateral to it. After detecting the diverticulum and right ureter, they were both carefully dissected. Transection of the diverticulum neck was done, and the cutting defect on the right ureter was carefully sealed (Figure 5) by running suture in end. The operation lasted for 140 min, and the total blood loss was measured 20 mL.
He left hospitol after urethral catheter was removed successfully, and total hospital stays were 5 d. Following discharge, we arranged ultrasound of the bladder and kidneys for surveillances. Besides, IVP was done for follow-ups at the same time. Relief of the right hydronephrosis could be seen on the image two weeks after the operation and bladder was intact without extravasation (Figure 6). Surgical pathology exhibited focal squamous metaplasia.
The right ureteral stent was removed one month after that. Neither lower urinary tract symptoms nor UTI were reported, and post-void residual urine volume was 43 mL one month after surgery. To date, he has finished monthly follow-ups for 1.5 years. Urine cytology at the 6th, 12th and 18th month, and intravenous pyelography at 12th month were all negative for malignancies.
It majorly relies on the image tools like ultrasound, IVP, computed tomography urogram, or magnetic resonance urogram for diagnosis of Hutch diverticulum. Among them, computed tomography urogram and magnetic resonance urogram are tools of choice not only in precise identification, also in preoperative, if necessary, planning for anatomical relations with the surroundings. However, from time to time, the image of it can mimic the bladder rupture and, herein, delicate judgement is needed.
Based on literature review, both surgical and nonsurgical are feasible to be the initial therapeutic modalities for hutch diverticulum. Indications for operation are dependent on any complications or suspicious malignant changes. Robotic-assisted surgery to the bladder diverticulum has been proven safe and efficient long ago[9-11]. Myer et al[9] reported five cases of robotic-assisted laparoscopic diverticulectomy, and one of them was diverticulectomy to hutch diverticulum with ureteral reimplantation. They concluded that this method was safe and effective compared to open endoscopic and laparoscopic procedures. Robotic-assisted approach features the minimal blood loss intraoperatively, low complication rates, short hospital stays, and non-significant postvoid urine residuals during surveillances[10,11]. Based on our experiences from this case, during surgery, robotic-assisted operation is a feasible method not only in diverticulectomy but also in reconstruction. Advantages of robotic-assisted surgery include quick targeting of the diverticulum neck, allowing sophisticated dissection among the diverticulum, ureter, and the adjacent anatomies, and quality sealing of the ureter and bladder defects. These advantages allow robotic-assisted rival the open and laparoscopic ways especially when diverticulum is hard to be approached or operated, such as large size, deep operative plane, narrow pelvic brim, or complicated anatomies. Sometimes hutch diverticulum could be diagnosed bilaterally[12] in children. Robotic-assisted approach might also provide more pros than others during reimplantation and reconstruction[12,13] of the ureters, but, from time to time, it might require more complex techniques in pediatrics surgery.
There are several methods of locating the diverticulum. In this case, we used saline instillation to bulge the diverticulum. On the other hand, simultaneous illumination by cystoscopy was adopted for this purpose[14], serving as a novel method in identifying the diverticulum. Ashton et al[10] proposed the method that putting a urethral catheter into the diverticulum first, then inflating the balloon at the neck of it. To date, this article is the first one providing a step-by-step robotic-assisted experience, concluding techniques from other literatures. We hope this report will provide other surgeons with feasible operations to cope with similar situations, especially those of large size diverticulum or complex anatomical features. Perhaps, some innovative methods will be further developed.
As for surveillance strategies after operation, if performed, should focus on the resolution of these symptoms and signs, intact reconstructed anatomies, no operative complications and recovery of urodynamic function. Metaplasia, like this case we presented, is rarely reported, only accounting for about 10%[4] maximally. Involving the surrounding organs may sometimes be suspicious, although it is extremely uncommon[8]. Nevertheless, like other diverticulum, chances are still there being malignant changes, such as urothelial cell carcinoma under the most occasions. Herein, tailored strategies like urine cytology and repeating image examination are suggested periodically.
Hutch diverticulum is a rare congenital disease, not only in children but also in adults. Indications for surgery are dependent on any of the related complications or possible malignant changes. Among all operative methods, robotic-assisted is a safe and efficient method for a well-trained urologist, providing several advantages over open and laparoscopic ones. It is still possible to be seen with malignant changes. Herein, periodic surveillances are necessary and imperative.
We thank the technical helps from the technicians of functional urological team of Tungs’ Taichung MetroHarbor Hospital.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Avtanski D, Desai DJ, Sun X S-Editor: Zhang L L-Editor: A P-Editor: Liu JH
| 1. | Legros L, Revencu N, Nassogne MC, Wese FX, Feyaerts A. [Multiple bladder diverticula caused by occipital horn syndrome]. Arch Pediatr. 2015;22:1147-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | De Oliveira PS, De Oliveira TR, Martinho D, Lopes T. Hutch bladder diverticulum - unusual cause of adult obstructive uropathy. Arch Ital Urol Androl. 2017;89:162-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Fanning DM, Morrin M, Power R. An unusual presentation of bilateral Hutch diverticula. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Pace AM, Powell C. Congenital vesical diverticulum in a 38-year-old female. Int Urol Nephrol. 2005;37:473-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Telli O, Guclu AG, Haciyev P, Burgu B, Gogus C. A rare entity in adults: Bilateral Hutch diverticulum with calculi. Can Urol Assoc J. 2015;9:E343-E344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Palmero Martí JL, Ramirez Backhaus M, Alvarez Barrera A, Amoros Torres A, Benedicto Redon A. Hutch bladder diverticula: a very uncommon entity in adults. Arch Esp Urol. 2012;65:636-639. [PubMed] |
| 7. | Kumar S, Gupta D, S Rau S. Polysubstance abuse related subacute urinary retention and Hutch diverticulum of urinary bladder. Clin Pract. 2011;1:e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Chezar K, Gotto G, Medlicott S, Trpkov K. Urothelial metaplasia of the seminal vesicle and ejaculatory duct associated with crossed-fused renal ectopia and Hutch diverticulum of the bladder. Can J Urol. 2018;25:9360-9362. [PubMed] |
| 9. | Myer EG, Wagner JR. Robotic assisted laparoscopic bladder diverticulectomy. J Urol. 2007;178:2406-10; discussion 2410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Ashton A, Soares R, Kusuma VRM, Moschonas D, Perry M, Patil K. Robotic-assisted bladder diverticulectomy: point of technique to identify the diverticulum. J Robot Surg. 2019;13:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Cacciamani G, De Luyk N, De Marco V, Sebben M, Bizzotto L, De Marchi D, Cerruto MA, Siracusano S, Benito Porcaro A, Artibani W. Robotic bladder diverticulectomy: step-by-step extravesical posterior approach - technique and outcomes. Scand J Urol. 2018;52:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Aljasser A, Alqasem S, Almutham A, Abduldaem O, Alnemer M, Abo Rubeea S. Bilateral ureteric re-implant for an 18 mo old boy with a huge bilateral hutch diverticulum presented with recurrent urinary retention. Urol Case Rep. 2020;32:101197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Sinha A, Pathak M, Vig A, Saxena R. Robotic surgery in paediatric patients: Our initial experience and roadmap for successful implementation of robotic surgery programme. J Minim Access Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Macejko AM, Viprakasit DP, Nadler RB. Cystoscope- and robot-assisted bladder diverticulectomy. J Endourol. 2008;22:2389-2391; discussion 2391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |