Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4681
Peer-review started: April 27, 2020
First decision: May 1, 2020
Revised: May 11, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: October 6, 2020
Processing time: 153 Days and 20.4 Hours
Parathyroid adenoma is a benign parathyroid tumor, with serum parathyroid hormone and calcium ion concentrations as the typical basis for diagnosis. Its clinical manifestations are complex and changeable; thus it is easily missed or misdiagnosed. Approximately 85% of patients with parathyroid adenoma develop primary hyperparathyroidism, and abnormalities in bones, kidneys and other organs can occur. Brown tumors are rare.
We report a rare case of fibrocystic osteitis associated with a parathyroid adenoma, which was discovered by chance due to a rib tumor. Abnormally elevated serum parathyroid hormone and calcium ion were found before surgery. We suspected primary hyperparathyroidism, and color Doppler ultrasound suggested the presence of a thyroid mass. With informed consent by the patient and her family, we first removed the rib tumor, and one week later, resection of the parathyroid adenoma and thyroid mass was performed on both sides, and the patient recovered well after surgery.
In the case of parathyroid adenoma combined with brown tumor, the bone cyst will gradually decrease in size with time without treatment. If not, surgery should be performed as soon as possible.
Core Tip: We report a rare and interesting case of fibrocystic osteitis associated with a parathyroid adenoma, which was discovered by chance due to a rib tumor. The patient only had respiratory symptoms. Computed tomography examination revealed a huge mass on the right rib and a suspected giant cell tumor of the bone. Interestingly, abnormal serum parathyroid hormone and calcium ion were found preoperatively and further examination revealed primary hyperparathyroidism. The pathology of the rib tumor showed a bone cyst, suggesting that this rib tumor was likely related to parathyroid adenoma.
- Citation: Han L, Zhu XF. Parathyroid adenoma combined with a rib tumor as the primary disease: A case report. World J Clin Cases 2020; 8(19): 4681-4687
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4681.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4681
Parathyroid adenoma is a benign parathyroid lesion, which is sporadic in the population. The incidence rate of parathyroid adenoma in the Asian population is lower than that in the Caucasian population, especially in middle-aged women. Parathyroid adenoma lacks typical clinical features in the early stage, and is easily neglected. It is worth noting that abnormal serological indicators often have important roles in the diagnosis of parathyroid adenoma, including significantly increased serum parathyroid hormone (PTH) and calcium, and enlarged parathyroid gland on auxiliary ultrasound, which often indicates abnormal parathyroid function.
Primary hyperparathyroidism (PHPT), often secondary to parathyroid adenoma, is often accompanied by structural and functional abnormalities of the corresponding target organs. At present, only a few cases of PHPT with pathological changes of bone tissue have been reported, and most of these changes are osteoporosis or fractures, and costal tumors are very rare.
We report a unique case of parathyroid adenoma which was found by chance after the diagnosis of a rib tumor.
The patient had a cough and sputum production for 20 d. Computed tomography (CT) identified a right rib tumor.
On August 17, 2019, a 53-year-old woman attended the Respiratory Department of our hospital for treatment due to a cough and sputum production for 20 d, occasionally yellow sticky sputum. Self-static anti-inflammatory, expectorant and other symptomatic drugs were administered (specific drug and dosage are unknown). Two days previously, CT examination of the chest in our hospital suggested a mass of the right rib, bone destruction and expansive growth. The right lower lobe of the lung showed a scattered area in the form of a cord and an increase in light lamellar density. The patient was admitted for thoracic surgery. Since the onset, the patient has had a normal diet and no significant weight loss. On preoperative examination, it was found that the patient's serum PTH was 527.60 pg/mL (reference range: 15-65 pg/mL) and serum calcium ion was 3.67 mmol/L (reference range: 2.2-2.7 mmol/L). Abnormal parathyroid gland function was suspected. We then invited the general surgeon to consult. HPHT was suspected, and after consultation with the family, it was decided to transfer the patient to general surgery for further treatment after thoracic surgery.
After undergoing rib tumor resection, anti-inflammatory, expectorant and other drugs were administered. The patient was in a stable condition and was transferred to general surgery for further treatment.
The superficial lymph nodes in the entire body were not enlarged, the neck was soft, the jugular veins were not filled or dilated, the trachea was centered, and there was no obvious enlargement of bilateral thyroid. In the left lying position, with the muscles relaxed, the inner edge of the shoulder blade on the right thorax could touch the local ridge of the sixth rib. The thoracic cage was normal with no intercostal space widening. The lungs were percussively unvoiced, breathing unvoiced, no dry and wet rales, and no wheeze.
PTH was 527.60 pg/mL (reference range: 15-65 pg/mL), serum calcium ion was 3.67 mmol/L (reference range: 2.2-2.7 mmol/L), alkaline phosphatase was 455 U/L (reference range: 50-135 U/L), uric acid was 440.3 μmol/L (reference range: 155-357 μmol/L), serum phosphorus was 0.70 mmol/L (reference range: 0.85-1.51 mmol/L), triglyceride was 4.32 mmol/L (reference range: Cholesterol: 5.75 mmol/L (reference range: 2.3-5.18 mmol/L), and no obvious abnormalities in other indicators were found.
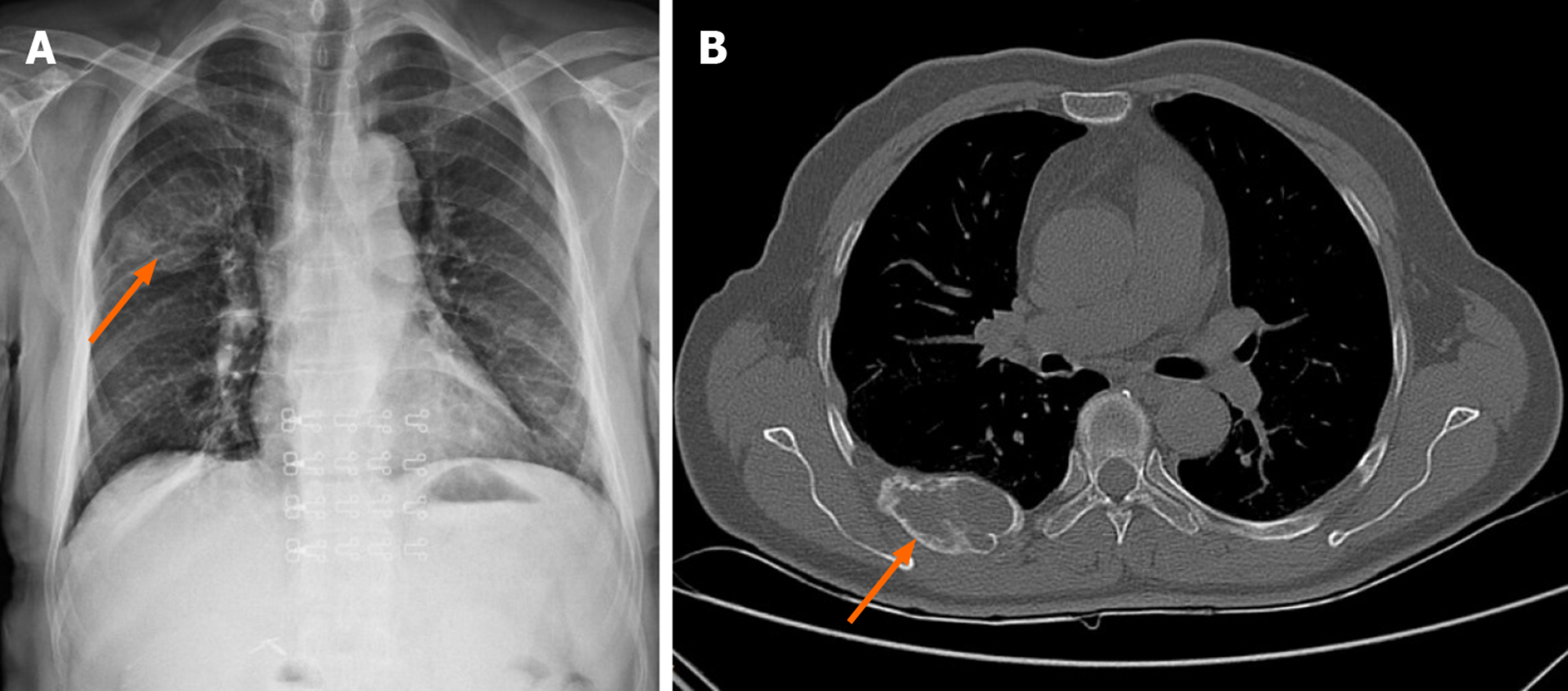
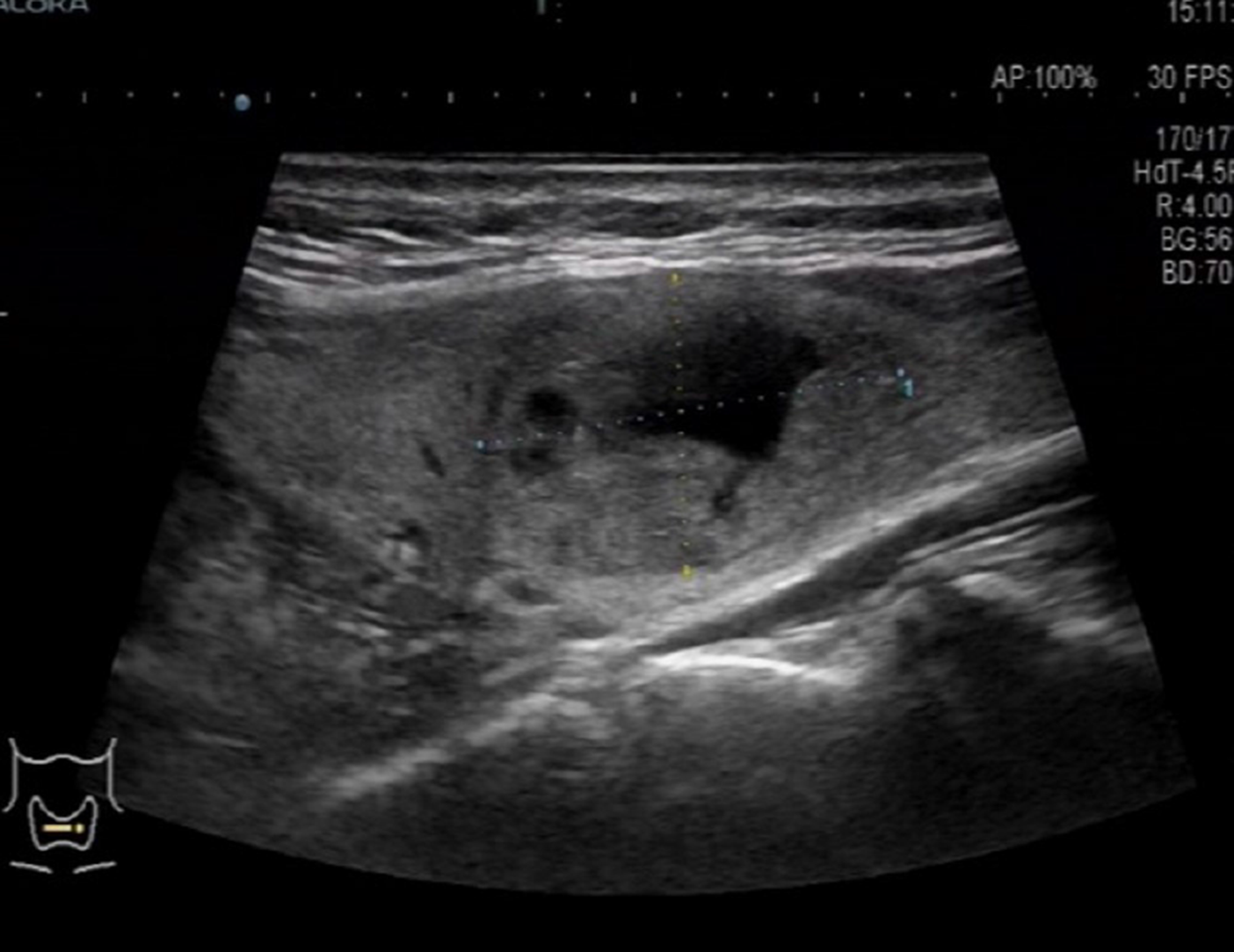
CT scan of the chest revealed right rib bone destruction with expansive growth, visible separation, and tracheobronchial patency. The shadow in the lung hilum was not large. In the right lower lung, there were strip-like, increased flaky density shadows, fuzzy edges, and no obvious thickening of bilateral pleura (Figure 1). Thyroid color Doppler ultrasound showed a solid mixed tumor of the right thyroid leaf cyst (TI-RADS: Class 3) (Figure 2).
The diagnosis of parathyroid adenoma with brown tumor was considered, but the nature of the tumor was unclear.
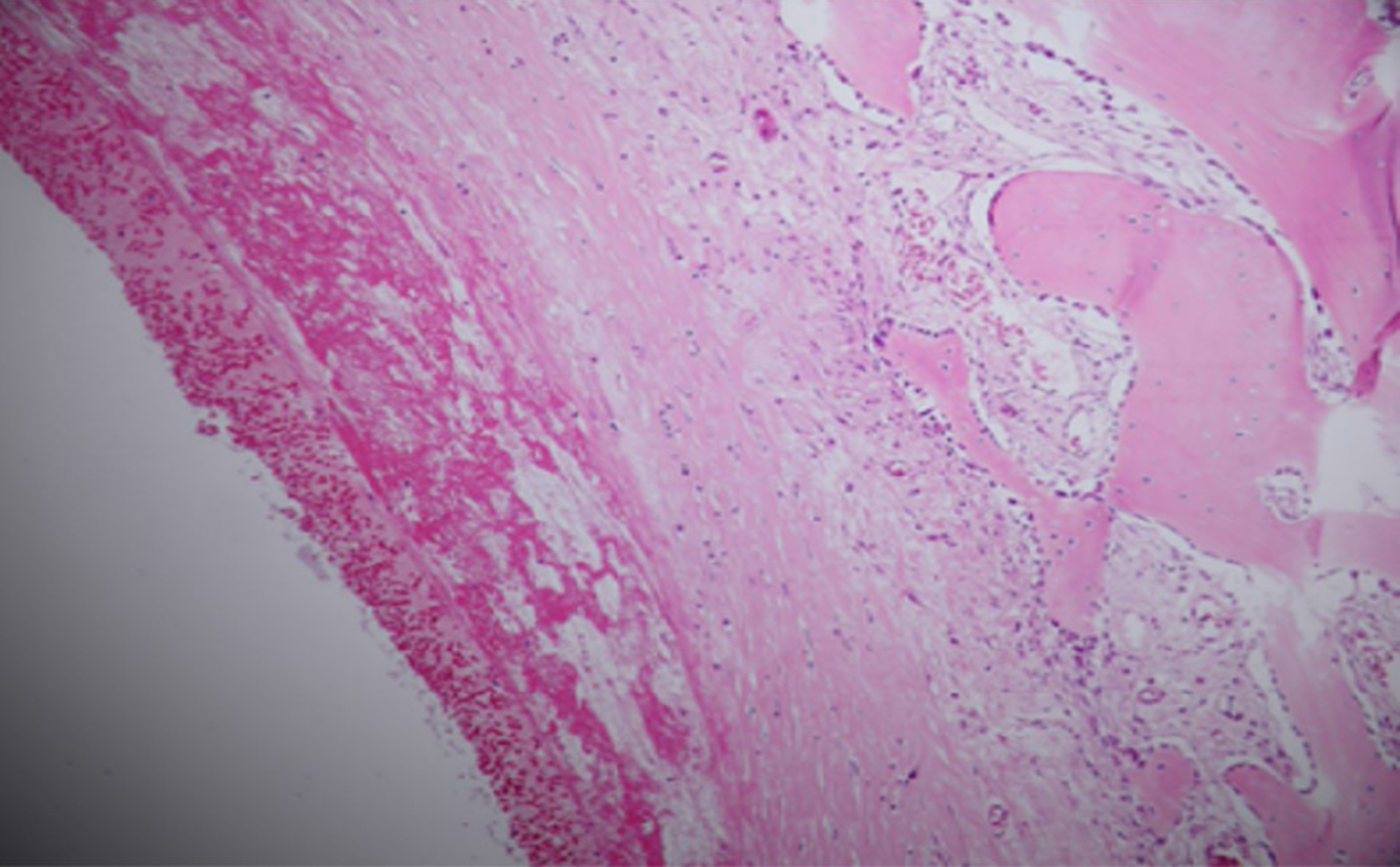
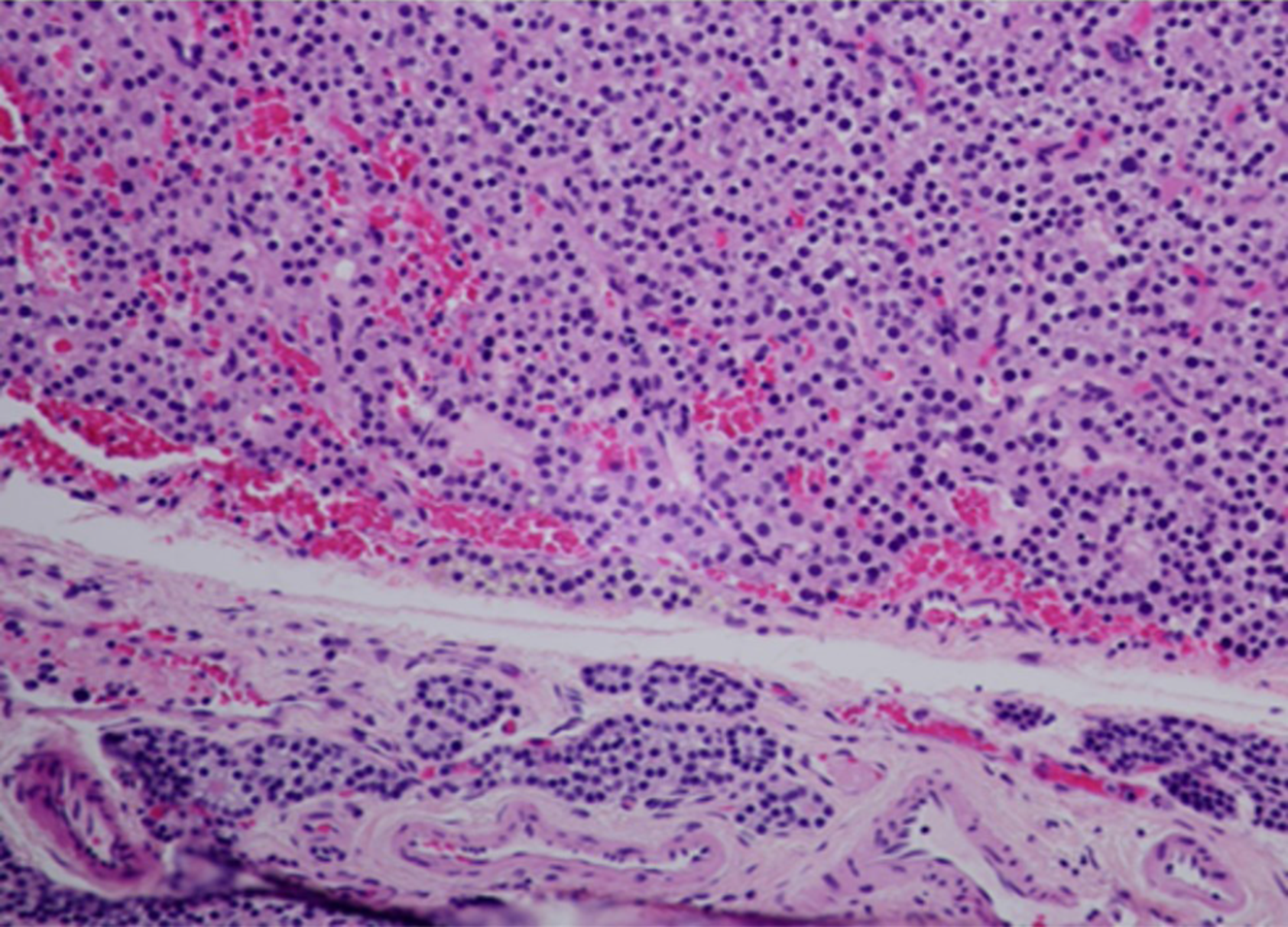
The patient was admitted for thoracic surgery on August 19, 2019. The tumor was removed on August 22. A right posterolateral chest wall incision was selected, and it was found that the irregular mass in the posterior costal part of the right 6th rib was approximately 10 cm long, with an uneven internal density, invasion of the parietal pleura, abundant nourishing blood vessels and bleeding. Complete resection of the damaged rib tissue was performed, followed by postoperative chest CT (Figure 3), and pathology showed an aneurysmal bone cyst (Figure 4). The patient underwent parathyroidectomy in the general surgery department on August 30. The right thyroid mass was removed during the operation. Intraoperative pathology indicated a right thyroid follicular tumor (1.5 cm in diameter), with abundant cells and cystic changes, and infiltration of the capsule is not excluded in the cell. Another tumor 1.5 cm × 1.0 cm in size was removed during surgery. The pathological results showed that the tumor was a parathyroid adenoma (Figure 5).
On September 2, 2019, serum PTH (28.71 pg/mL) and calcium (2.43 mmol/L) were in the normal range. The patient was discharged on September 6, 2019, with regular follow-up.
Parathyroid adenoma is a common benign parathyroid tumor. Eighty-five percent of patients can have PHPT[1,2]. The symptoms involve multiple systems, including hypercalcemia and urinary tract abnormalities. Stones caused by calcium salt deposition can also manifest as osteoporosis, pathological fractures and other symptoms. Most patients have symptoms at the time of consultation. A few patients lack typical clinical manifestations, and often have kidney, bone and other diseases[3]. According to the different manifestations of affected organs, PHPT can be divided into bone disease-based types, where patients may have bone pain, are prone to fracture, and fibrocystic osteitis is a typical skeletal lesion of PHPT combined with bone cysts, brown tumors, osteoporosis and fragile fractures, as shown by conventional bone radiography[4]. The primary target organ of PHPT is the kidney, which can develop into kidney stones[5]. It can also manifest as urinary calculi and osteolytic bone changes, as well as other systemic lesions[6,7].
In the present case, the patient presented with a rib tumor, and CT was suggestive of giant cell tumor of bone, and osteolytic changes on admission. Preoperative examination revealed a significant increase in serum calcium and serum PTH. We considered this to be parathyroid gland dysfunction. With the consent of the patient and her family, we first performed rib tumor resection, and the pathology revealed a cyst. The patient was in good physical condition after surgery. Parathyroidectomy was subsequently performed in the general surgery department. Postoperative serum calcium and serum PTH levels decreased. We consider that the rib tumor may have been fibrocystic osteitis secondary to parathyroid adenoma.
Fibrocystic osteitis, also known as brown tumor, mostly manifests in the middle and late stages of hyperparathyroidism, and is a metabolic bone disease caused by calcium and phosphorus abnormalities[8]. Fibrocystic osteitis occurs in the clavicle, long bones, and pelvis[9]. The imaging manifestations of osteolytic bone destruction include clear boundaries and it often causes bone expansion, and other subperiosteal bone resorption. It is not a real tumor, but abnormally increased PTH in the body stimulates osteoclast activity, which leads to osteolysis and destruction[10].
At present, there is no clear treatment plan for parathyroid adenoma complicated with fibrocystic osteitis, and there is no consistent guideline recommendation whether to treat fibrocystic osteitis surgically. Parathyroidectomy was performed in this patient with PHPT and fibrocystic osteitis. Postoperative blood calcium returned to normal levels and bone changes were reversed. In such patients, parathyroidectomy is the first treatment choice for fibrocystic osteitis. Postoperative PTH is reduced, bone destruction is controlled, fracture risk is reduced, and bone density gradually increased in the later stage, thereby completely inhibiting fibrocystic changes. During the development of osteitis, Vander Walde found that irrespective of age, and blood calcium levels, patients with surgically removed parathyroid glands have a lower risk of fractures than those without surgery; thus, surgical treatment of fibrocystic osteitis can be eliminated[11]. Of course, different patients have different outcomes due to the severity of the disease, whether they have fractures, and their vitamin status. When pathological fractures occur, the reversion time of bone lesions is relatively long, which may be related to the slow recovery of cortical bone density. However, for obvious local bone and joint pain, pathological fracture or high fracture risk, and recurrence after reversal, orthopedic surgery can be performed to relieve the symptoms of local pain and fix the fracture, but only if the diagnosis is clear, in order to reduce secondary damage to patients caused by overtreatment.
Agarwal G followed the clinical recovery, bone turnover, bone mineral density, and biochemical indicators on bone radiology of 51 patients with PHPT and fibrocystic cysts[12]. Qualitative destruction recovered, and bone tumors persisted in a few patients, requiring further surgical intervention. Wang performed a large rib brown tumor resection in patients who had been treated with zoledronic acid for 17 mo with elevated serum calcium and PTH. One patient reported hip pain and abnormal pelvic X-rays after surgery. A parathyroid adenoma was subsequently found. Pain relief was achieved after adenoma resection. It took at least 2 years for fibrotic osteitis to recover[13]. Khalil reported a patient with brown tumor lesions in the right pelvis, and surgery was considered due to a persistent increase in focal pain. Pain was relieved postoperatively. When there is a high risk of pathological fractures or patients have persistent focal bone pain, surgery should be considered at the appropriate site[14]. Satpathy reported a case of parathyroid adenoma with mandibular fibrocystic osteitis. After parathyroidectomy, the patient's bone lesions were significantly reduced during the 6 mo of regular follow-up, while complete bone reconstruction took longer. The author believed that the removal of parathyroid adenomas and achieving normal blood calcium levels are options for treating parathyroid glands with fibrocystic osteitis. If primary bone disease does not shrink significantly after 6 mo of treatment, surgical curettage should be considered[15].
As the incidence of fibrocystic osteitis is extremely low, and the primary manifestations in parathyroid glands are not fully understood, doctors are often confused by the association with bones. Surgical removal of bone tumors does not include a comprehensive preoperative examination. Although the pain caused by the patient's skeletal disease can be relieved temporarily, after a period of time, the bone disease will recur and brown tumors in other areas can occur. Therefore, an appropriate preoperative examination is necessary to diagnose parathyroid adenoma with fibrocystic osteitis and plan reasonable treatment. Giant cell tumors of bone and brown tumors have osteolytic lesions of cortical bone, which often confuse doctors and can be misdiagnosed. Therefore, it is necessary to combine the patient's other clinical manifestations, medical history, and reasonable examination methods for the diagnosis of brown tumors, such as preoperative color Doppler ultrasound. With regard to the treatment of parathyroid adenoma with fibrocystic osteitis, previous studies have reported that skeletal lesions will gradually be controlled and bone cysts will be reversed in the majority of patients. However, the reconstruction of intact bone takes a long time, and long-term skeletal lesions cannot be completely controlled, which may cause pathological fractures, and although there are certain risks, surgical intervention is still required. Some brown tumors can occur on the face. If they cannot be treated within a short time, they will also affect the patient's mental status. Therefore, surgical removal can be performed at the patient's request, and the disease should be detected early to establish a correct diagnosis. The patient's symptoms should be comprehensively evaluated, not only to avoid misdiagnosis, but also to reduce trauma.
Parathyroid adenoma with brown tumor is relatively rare, a comprehensive preoperative physical examination and evaluation of the patient's condition are conducive to a more accurate diagnosis and treatment. At present, in patients with a brown tumor, most are treated with parathyroid adenoma resection, and after a period of time, the brown tumor may gradually disappear. However, if the brown tumor does not improve and the patient's physical condition is affected, surgical treatment with regular follow-up is necessary.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coco D S-Editor: Zhang L L-Editor: Webster JR P-Editor: Liu JH
| 1. | Sutbeyaz Y, Yoruk O, Bilen H, Gursan N. Primary hyperparathyroidism presenting as a palatal and mandibular brown tumor. J Craniofac Surg. 2009;20:2101-2104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Silva BC, Cusano NE, Bilezikian JP. Primary hyperparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32:593-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 74] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 3. | Aresta C, Passeri E, Corbetta S. Symptomatic Hypercalcemia in Patients with Primary Hyperparathyroidism Is Associated with Severity of Disease, Polypharmacy, and Comorbidity. Int J Endocrinol. 2019;2019:7617254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Minisola S, Gianotti L, Bhadada S, Silverberg SJ. Classical complications of primary hyperparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32:791-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 5. | Marx SJ. Hyperparathyroid and hypoparathyroid disorders. N Engl J Med. 2000;343:1863-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 262] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 6. | Pal R, Arya AK, Aggarwal A, Singh P, Dahiya D, Sood A, Singh T, Ram S, Bhansali A, Bhadada SK. Weight gain after curative parathyroidectomy predicts increase in bone mineral density in patients with symptomatic primary hyperparathyroidism. Clin Endocrinol (Oxf). 2020;93:28-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Weber TJ, Koh J, Thomas SM, Hogue JA, Scheri RP, Roman SA, Sosa JA. Impaired calcium sensing distinguishes primary hyperparathyroidism (PHPT) patients with low bone mineral density. Metabolism. 2017;74:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Misiorowski W, Czajka-Oraniec I, Kochman M, Zgliczyński W, Bilezikian JP. Osteitis fibrosa cystica-a forgotten radiological feature of primary hyperparathyroidism. Endocrine. 2017;58:380-385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Khalatbari MR, Moharamzad Y. Brown tumor of the spine in patients with primary hyperparathyroidism. Spine (Phila Pa 1976). 2014;39:E1073-E1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Rejnmark L, Ejlsmark-Svensson H. Effects of PTH and PTH Hypersecretion on Bone: a Clinical Perspective. Curr Osteoporos Rep. 2020;18:103-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | VanderWalde LH, Liu IL, Haigh PI. Effect of bone mineral density and parathyroidectomy on fracture risk in primary hyperparathyroidism. World J Surg. 2009;33:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Agarwal G, Mishra SK, Kar DK, Singh AK, Arya V, Gupta SK, Mithal A. Recovery pattern of patients with osteitis fibrosa cystica in primary hyperparathyroidism after successful parathyroidectomy. Surgery. 2002;132:1075-83; discussion 1083-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Wang WD, Zhang N, Qu Q, He XD. Huge brown tumor of the rib in an unlocatable hyperparathyroidism patient with "self-recovered" serum calcium and parathyroid hormone: A case report. World J Clin Cases. 2019;7:4321-4326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Khalil PN, Heining SM, Huss R, Ihrler S, Siebeck M, Hallfeldt K, Euler E, Mutschler W. Natural history and surgical treatment of brown tumor lesions at various sites in refractory primary hyperparathyroidism. Eur J Med Res. 2007;12:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Satpathy AS, Dasgupta A, Dutta C, Mohan NVK, Satpathy S. Osteitis fibrosa cystica of mandible in hyperparathyroidism-jaw tumor syndrome: A rare presentation and review of literature. Natl J Maxillofac Surg. 2017;8:162-166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |