Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4624
Peer-review started: June 19, 2020
First decision: July 24, 2020
Revised: July 28, 2020
Accepted: September 4, 2020
Article in press: September 4, 2020
Published online: October 6, 2020
Processing time: 100 Days and 10.3 Hours
Esophageal carcinosarcoma, usually presenting as a pedunculated polypoid mass, is a rare malignancy with coexisting sarcomatoid and carcinomatous components. Its imaging and endoscopic characteristics are similar to those of leiomyosarcoma, liposarcoma and so forth. The diagnosis needs histological confirmation. Surgical resection is the traditional therapy. Endoscopic resection is minimally invasive but still controversial. This paper reports the case of a patient with a giant esophageal carsinosarcoma who underwent a palliative endoscopic resection.
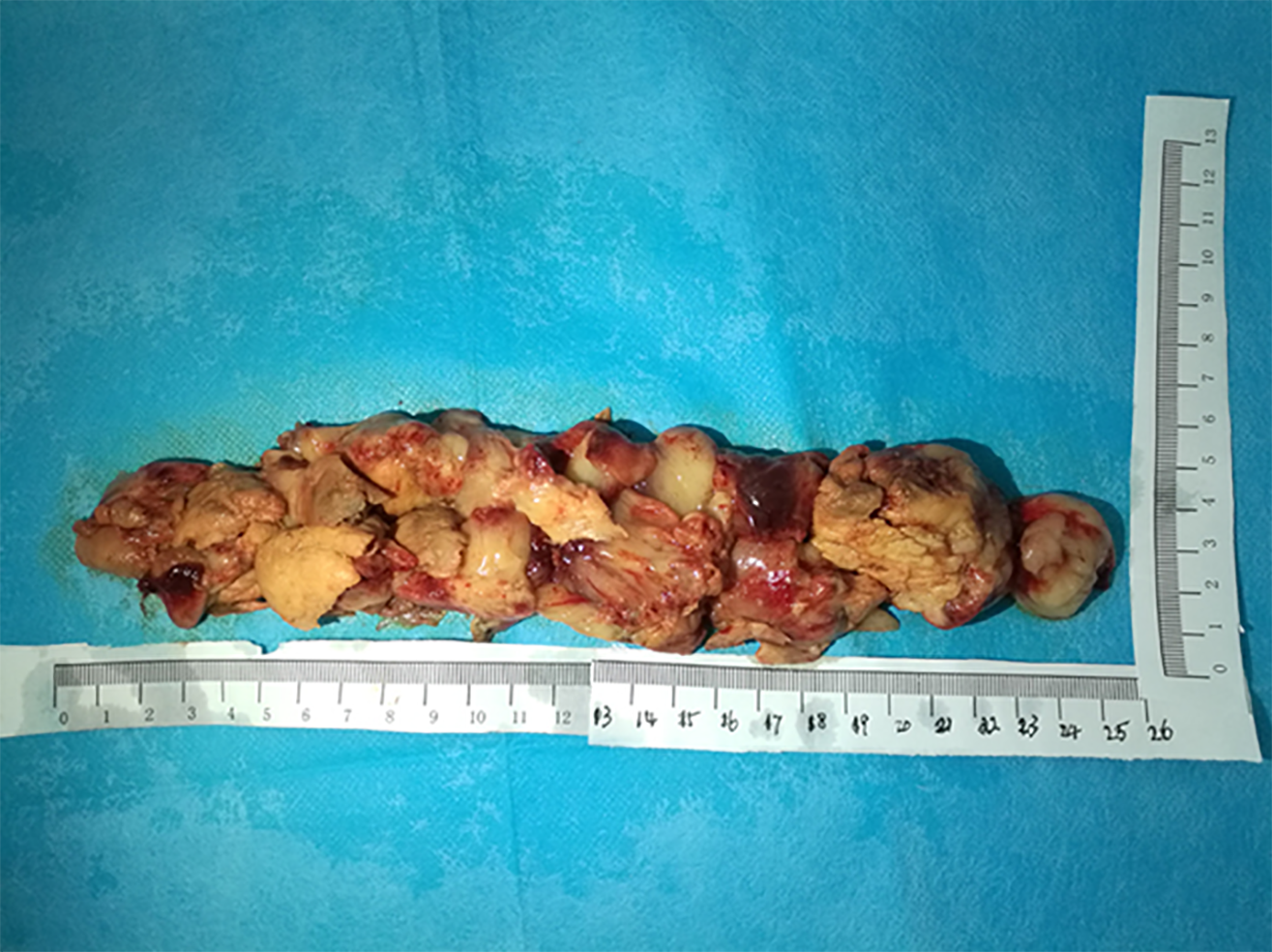
A 55-year-old male patient presented with dysphagia and weight loss for 1 mo. Imaging and endoscopy showed a gray-white, polypoid, stalk-like mass, with a bulky pedicle located in the middle and lower esophagus. The mass almost filled the whole esophageal lumen, but the endoscope could still pass through. Despite the suspicion of a malignancy, repeated biopsies indicated necrosis and inflammation. After multidisciplinary team consultation, an endoscopic resection to diagnose and relieve the obstruction was recommended. The pedicle of the mass was cut off, the bleeding was stopped, and the mass was cut into pieces and pulled out. The mass was 26 cm × 5 cm × 4 cm in size. The final diagnosis was esophageal carcinosarcoma. No postoperative complications occurred. After 1 mo, the patient gained 6 kg and endoscopic reexamination revealed no obstruction. Radical surgery with lymph node dissection was carried out successfully. This lesion was the largest endoscopically resected esophageal carcinosarcoma reported to date.
Endoscopic palliative resection can help obtain adequate tissue for diagnosis and relieve obstructions in patients with giant esophageal carcinosarcoma.
Core Tip: A patient presented with dysphagia and weight loss for 1 mo. Imaging and endoscopy indicated a polypoid stalk-like mass located in the middle and lower esophagus, almost filling the whole esophageal lumen. Repeated biopsies failed to diagnose its nature. An endoscopic palliative resection was performed on this patient, and no postoperative complications occurred. After 1 mo, the patient gained 6 kg and endoscopic reexamination revealed no obstruction. This is the largest endoscopically resected esophageal carcinosarcoma reported to date. Endoscopic palliative resection can help obtain adequate tissue for diagnosis and relieve the obstruction.
- Citation: Li Y, Guo LJ, Ma YC, Ye LS, Hu B. Endoscopic palliative resection of a giant 26-cm esophageal tumor: A case report. World J Clin Cases 2020; 8(19): 4624-4632
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4624.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4624
Esophageal carcinosarcoma is a rare malignancy with coexisting sarcomatoid and carcinomatous components[1]. Carcinosarcoma has also been termed as spindle cell carcinoma, sarcomatoid carcinoma, pseudosarcoma, and squamous cell carcinoma with sarcomatoid changes[1]. On imaging and endoscopic examinations, the majority of esophageal carcinosarcomas present as a bulky intraluminal polypoid mass, similar to leiomyosarcoma, gastrointestinal stromal tumor, fibrovascular polyp, liposarcoma and so forth[2-5]. Therefore, histological confirmation is vital for the final diagnosis. However, preoperative biopsies usually produce negative results, and consequently a more effective method is needed to accomplish diagnosis[4].
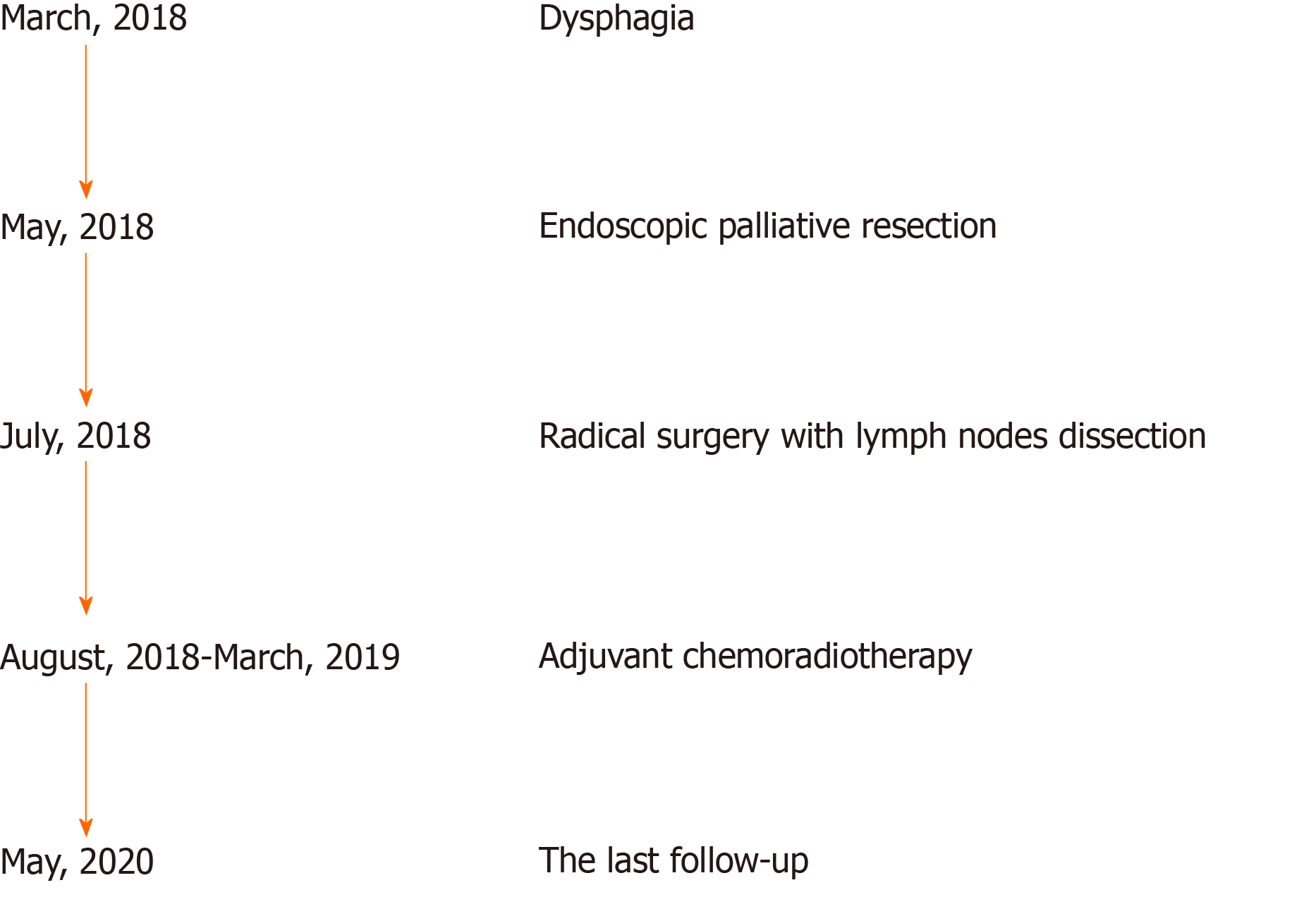
Esophagectomy with regional lymph node dissection has been the traditional therapy for esophageal carcinosarcoma, and the endoscopic procedure is recommended as a promising approach[1,3]. However, a PubMed search for “esopha-geal carcinosarcoma” AND “endoscopic resection”, “esophageal sarcomatoid carcinoma” AND “endoscopic resection” or "carcinosarcoma" AND "endoscopic resection" returned only four case reports. Endoscopic resection has been performed for superficial esophageal carcinosarcomas or patients in poor condition[1,6]. This paper reports the case of a palliative endoscopic resection of a giant esophageal polypoid mass, thus confirming the diagnosis and relieving the obstruction. This lesion was confirmed to be esophageal carcinosarcoma (T1bN1M0). The timeline of this case is shown in Figure 1.
A 55-year-old male patient presented to the Gastroenterology Department of West China Hospital for dysphagia and weight loss for 1 mo.
The patient suffered dysphagia while eating solid or semi-solid food and lost 6 kg in 1 mo. He also felt slight retrosternal pain while changing position, without reflux, vomit, fever, or cough.
The patient had no specific previous illness or family history. On average, the patient had a smoking history of 60 cigarettes a day for 30 years and a drinking history of 80 g/d for 20 years.
At admission, the patient’s temperature was 36.5 °C, heart rate was 76 bpm, respiratory rate was 20 breaths per minute, blood pressure was 119/89 mmHg, oxygen saturation in room air was 99%, height was 172 cm, and weight was 63 kg. No other special finding was reported.
A routine blood test indicated leukocytosis with the white blood cell count at 12.08 × 109/L (normal range, 3.5 × 109/L to 9.5 × 109/L) and mainly neutrophils (81.9%; normal range, 40%-75%). The hemoglobin concentration and platelet count were normal. The serum albumin concentration had declined to 29.9 g/L (normal range, 40–55 g/L). The serum C-reactive protein concentration had increased to 74.8 mg/L (normal range, < 5.0 mg/L), and the erythrocyte sedimentation rate was 60 mm/h (normal range, < 21.0 mm/h). The serum tumor markers, including CEA, AFP, and CA 19-9, had normal concentrations.
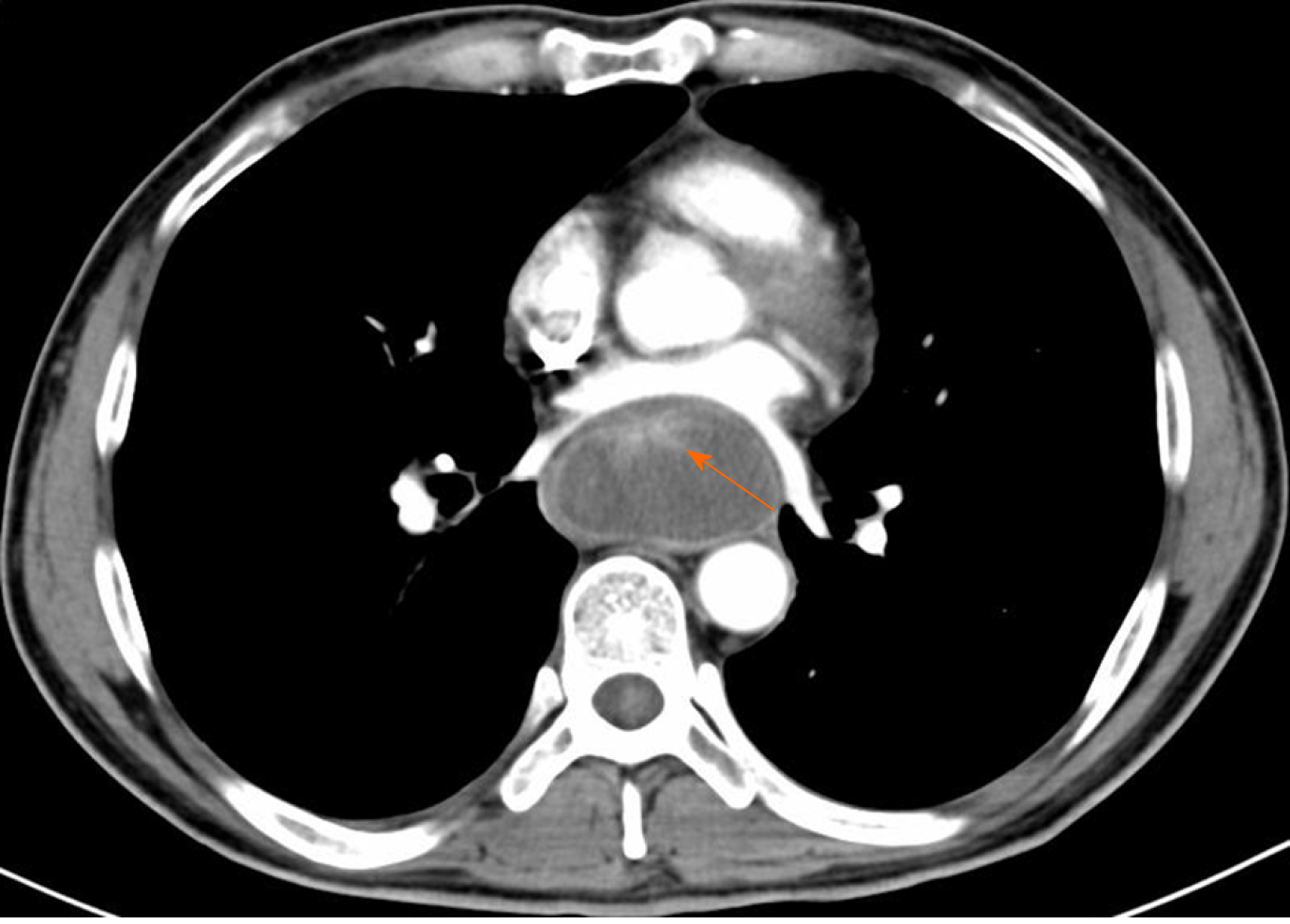
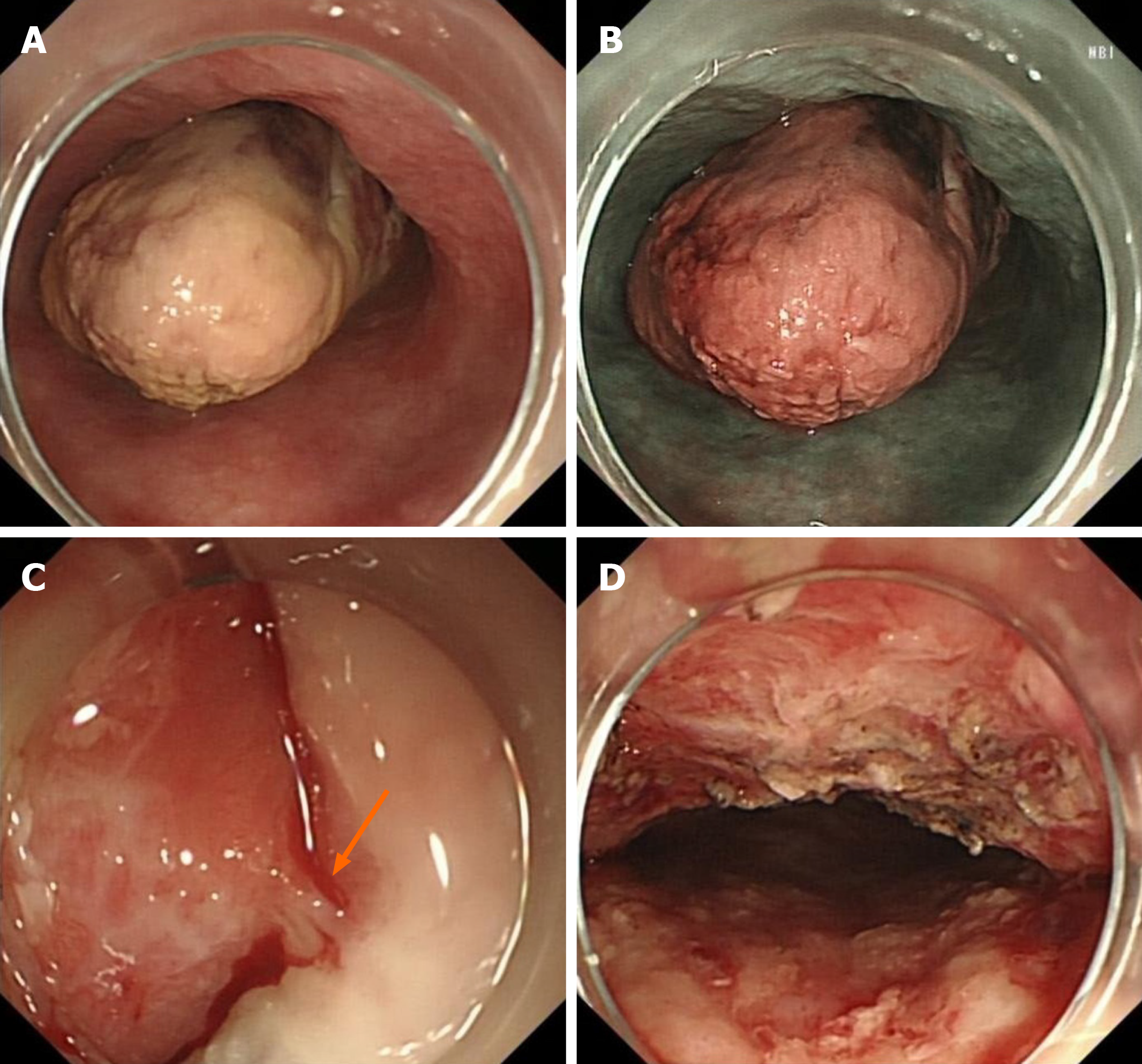
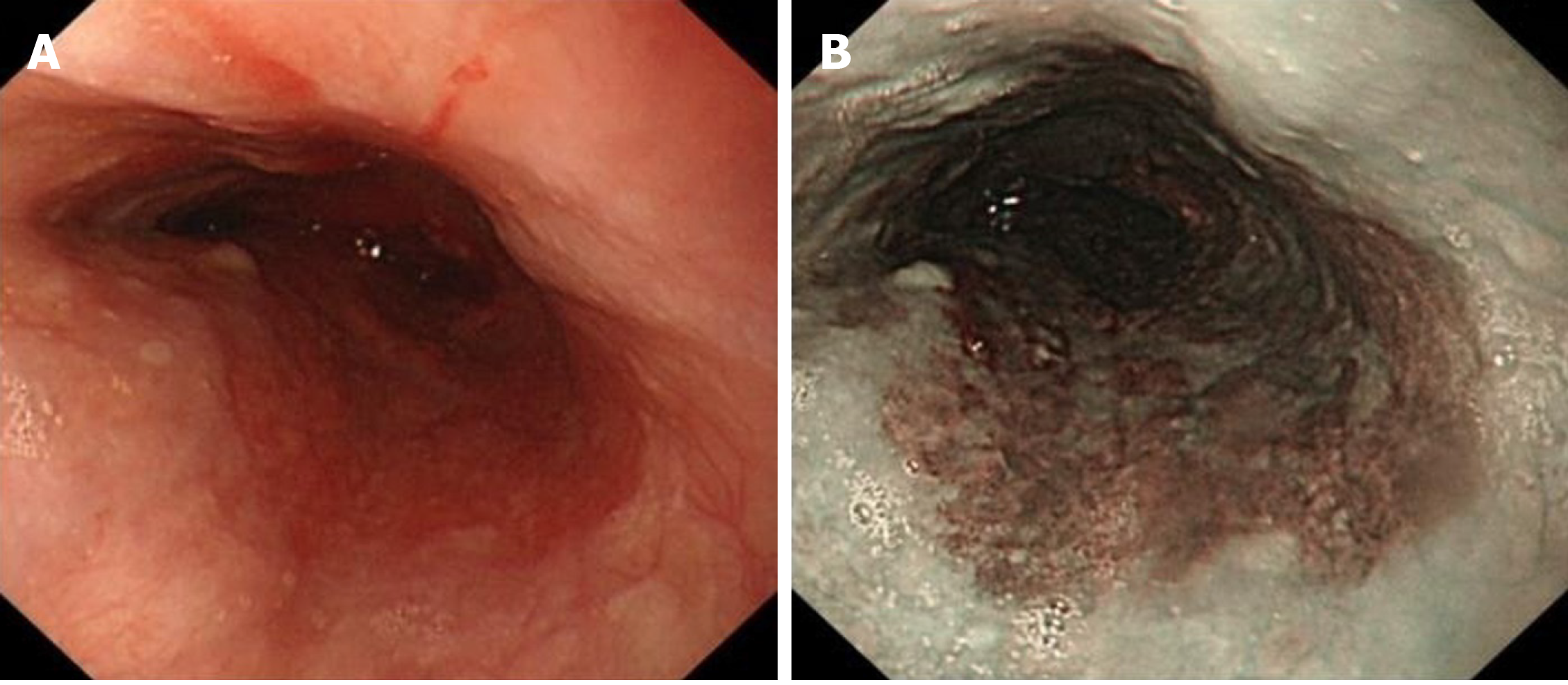
An X-ray barium meal examination showed a huge intraluminal stalk-like mass along the middle and lower esophagus (Figure 2). Computed tomography (CT) showed a prominently enhanced anterior area of the mass beside the esophageal wall, and the maximum sectional area was about 5.6 cm × 3.5 cm (Figure 3). Endoscopy indicated that the mass was polypoid, gray-white, with a bulky pedicle, located in the esophagus 22-45 cm from the incisors and almost filled the whole esophageal lumen, but the endoscope could still pass through (Figure 4A-C).
The biopsy in West China Hospital indicated necrosis and inflammation, similar to the result of the initial biopsy in the previous hospital.
Despite the suspicion of a malignancy, the diagnosis of this giant esophageal mass is still unclear. Repeated biopsy or a partial resection to diagnose should be the priority. Further surgery, chemotherapy, or radiotherapy should be done based on the final diagnosis.
A further biopsy might still fail due to the repeated insignificant results of the biopsy. A partial or total resection of the mass to acquire sufficient tissue for pathological diagnosis is necessary. It would also contribute to relieve the obstruction and improve nutrition. An endoscopic resection is optimal for the advantage of minimal invasiveness. If it fails, additional surgery should be performed.
The mass could probably be malignant. First, an endoscopic partial resection is required to obtain adequate tissue for pathological diagnosis, and if possible, a total resection of the mass to relieve the obstruction should be the optimal choice. If needed, additional therapy should be provided.
The disease was diagnosed after endoscopic palliative resection. The final diagnosis was esophageal carcinosarcoma (T1bN1M0), with submucosal invasion and right superior paratracheal lymph node metastasis. Immunochemical staining indicated that the tumor cells were positive for pancytokeratin (PCK) and negative for cluster of differentiation 34 (CD34), Desmin, and S-100, and Ki 67 index was 20%-30% (Figure 5).
Endoscopic resection was conducted as follows: (1) The basal part of the mass was sought first, which was 33 cm from the incisors; (2) 0.01% epinephrine saline and methylene blue were injected into the submucosa to lift the lesion from the muscle layer; (3) Dissection was performed within the submucosa beneath the mass with a Hybrid knife and an insulation-tipped diathermic knife; (4) Bleeding was stopped with hemostatic forceps; and (5) The mass was cut into pieces with a snare and pulled out. The mass was totally resected, and the wound was intact (Figure 4D). The mass was about 26 cm × 5 cm × 4 cm in size (Figure 6).
No postoperative complications occurred. Oral intake was resumed 2 d later. After 1 mo, the patient gained 6 kg, and endoscopic reexamination revealed no obstruction (Figure 7). Radical surgery with lymph node dissection and adjuvant chemoradiotherapy were carried out. The patient received six cycles of chemoradiotherapy (175 mg/m2 of paclitaxel and 80 mg/m2 of nedaplatin at first day) and 25 times of radiotherapy with a total dosage of 45 Gy (1.8 Gy per time) from August 2018 to March 2019. A 2-year follow-up revealed that the patient lived well, without recurrence or metastasis.
In 1865, Virchow initially introduced “carcinosarcoma,” a rare malignancy with coexisting carcinomatous and sarcomatoid components. Later studies demonstrated that carcinosarcoma, sarcomatoid carcinoma, spindle cell carcinoma, pseudosarcoma, and squamous cell carcinoma with sarcomatoid changes were one disease, and they could occur in the lung, thyroid, breast, uterus, esophagus and so forth[1]. Esophageal carcinosarcoma accounted for about 0.5%-2.8% of all esophageal carcinomas and mainly occurred in middle-aged and elderly male patients with a heavy smoking or drinking history[7-9]. The majority of esophageal carcinosarcomas presented as a bulky intraluminal polypoid mass and were located in the middle and lower esophagus[1,2,7]. Sarcomatoid components formed the body of the polypoid mass, and carcinomatous components (mostly squamous cell carcinoma) surrounded the base of the tumor, with a distinct transitional area between the two components[8,10,11]. The doubling time of esophageal carcinosarcoma was reported to be 2.2-5 mo, and the 5-year overall survival was 26.7%-61.9%[4,8,9,12].
About the oncogenesis, the metaplastic hypothesis held that two components derived from a common undifferentiated stem cell, while the collision hypothesis believed that two components derived from different stem cells undergoing malignant transformation simultaneously[7,13-15]. Recent studies indicated that TP53 mutation was common in patients with esophageal carcinosarcoma, consistent with positive immunohistochemical staining for p53, occurring in both sarcomatoid and carcinomatous components[16,17]. These findings indicated that the two components originated from the same stem cell.
Regarding preoperative diagnosis, Zhang et al[18] and Hashimoto et al[4] reported that 14.1% (10/71) and 17.9% (5/28) of esophageal carcinosarcomas, respectively, were suspected to have sarcomatous components based on biopsy. Although imaging and endoscopy showed characteristic features, preoperative diagnosis was still difficult. A similar situation occurred in the case reported in this paper. The causes might be as follows: (1) The carcinomatous and sarcomatous components were distributed zonally; or (2) The tumor grew rapidly and the tumor size was huge, resulting in superficial necrosis.
Lymph node and distant metastases of esophageal carcinosarcoma have been frequently observed in previous studies, and metastasis of epithelial components is more common[3,4,19,20]. Endoscopic ultrasonography (EUS), CT, and positron emission tomography are important for TNM staging of esophageal cancers preoperatively, although practices in esophageal carcinosarcomas are scarce. Ji et al[6] and Kuo et al[3] reported esophageal carcinosarcoma to be a hypoechoic mass with a regular margin. EUS contributed to determine the invasion depth and regional lymph node involvement. The preoperative EUS diagnosis of esophageal carcinosarcoma reached high consistency with final pathological staging (T staging: 7/7, 100%; N staging: 5/7, 71.4%)[3,6].
A surgical resection with regional lymph node dissection was the traditional treatment for esophageal carcinosarcomas without distant metastasis[1,4]. Endoscopic techniques, with the advantages of minimal invasion and preservation of the esophagus, have also been applied to the resection of esophageal carcinosarcoma (Table 1). In 2004 and 2009, Pesenti et al[21] and Ji et al[6] conducted the first and second endoscopic resections of esophageal carcinosarcoma, respectively, with good tolerance and favorable prognosis. In 2013, Xu et al[22] reported the case of an 84-year-old male patient with multiple carcinosarcomas along the esophagus and stomach. He was in serious condition and received a palliative endoscopic resection of the esophageal lesion to relieve the obstruction. He resumed a normal food intake postoperatively, but succumbed 7 mo later. In 2018, Yabuuchi et al[23] reported the fourth case with a slightly elevated lesion in the middle thoracic esophagus. This patient received an endoscopic submucosal dissection but the follow-up information was unclear. The patient in our study was the fifth patient with esophageal carcinosarcoma who underwent an endoscopic resection, and the mass was much larger than those in the previous cases. A palliative endoscopic resection was performed first due to unclear diagnosis and esophageal obstruction. The patient recovered well 1 mo later. After surgical resection and adjuvant chemoradiotherapy, the patient got a favorable prognosis. This practice suggested that endoscopic resection is applicable for patients with esophageal carcinosarcoma: (1) A total endoscopic resection is achievable for small and superficial tumors; (2) A palliative endoscopic resection relieves esophageal obstruction in patients with serious condition; and (3) A partial resection could attain adequate tissue for undiagnosed tumors. Further prospective large-sampled studies are needed to verify these findings.
| Case number | Year | Ref. | Sex | Age (yr) | Comorbidity | Endoscopic procedure | Tumor location | Tumor size (cm) | Additional surgery | Adjuvant chemoradiotherapy | Follow-up time (yr) | Recurrence or metastasis |
| 1 | 2004 | Pesenti et al[21] | Male | 73 | Cardiac dysfunction | Endoscopic mucosal resection | Cervical esophagus | 3 × 7 | No | Yes | 2.5 | No |
| 2 | 2009 | Ji et al[6] | Male | 61 | None | Endoscopic polypectomy | 25-30 cm from the incisors | 5 × 3 × 3 | No | No | 1.5 | No |
| 3 | 2013 | Xu et al[22] | Male | 80 | Gastrointestinal bleeding and severe anemia | Endoscopic mucosal resection | 30 cm from the incisors, gastric antrum | 4 × 2.5 × 1.5 | No | No | 0.5 | NA |
| 4 | 2018 | Yabuuchi et al[23] | Female | 77 | None | Endoscopic submucosal dissection | Middle thoracic esophagus | NA | NA | NA | NA | NA |
| 5 | 2020 | Present paper | Male | 55 | None | Endoscopic palliative resection | 22-45 cm from the incisors | 26 × 5 × 4 | Yes | Yes | 2 | No |
This paper reports the case of a patient with a giant esophageal polypoid mass who underwent a palliative endoscopic resection. This lesion turned out to be esophageal carcinosarcoma (T1bN1M0). An endoscopic resection confirmed the diagnosis and relieved the esophageal obstruction.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Treviño González JL S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Schizas D, Mastoraki A, Bagias G, Ioannidi M, Kanavidis P, Moris D, Tsilimigras DI, Spartalis E, Arkadopoulos N, Liakakos T. Carcinosarcomas of the esophagus: systematic review of a rare nosologic entity. J BUON. 2018;23:1432-1438. [PubMed] |
| 2. | Ng YA, Lee J, Zheng XJ, Nagaputra JC, Tan SH, Wong SA. Giant pedunculated oesophageal liposarcomas: A review of literature and resection techniques. Int J Surg Case Rep. 2019;64:113-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kuo CJ, Lin TN, Lin CJ, Wu RC, Chang HK, Chu YY, Lien JM, Su MY, Chiu CT. Clinical manifestation of esophageal carcinosarcoma: a Taiwan experience. Dis Esophagus. 2010;23:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Hashimoto M, Kitagami H, Niwa H, Kikkawa T, Ohuchi T, Takenouchi T, Hosokawa M. Prognosis and prognostic factors of esophageal spindle cell carcinoma treated by esophagectomy: a retrospective single-institution analysis. Esophagus. 2019;16:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 5. | Ward MA, Beard KW, Teitelbaum EN, Sharata AM, Dunst CM, Swanstrom LL, Reavis KM. Endoscopic resection of giant fibrovascular esophageal polyps. Surg Endosc. 2018;32:1066-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Ji F, Xu YM, Xu CF. Endoscopic polypectomy: a promising therapeutic choice for esophageal carcinosarcoma. World J Gastroenterol. 2009;15:3448-3450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Iascone C, Barreca M. Carcinosarcoma and pseudosarcoma of the esophagus: two names, one disease--comprehensive review of the literature. World J Surg. 1999;23:153-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Wang L, Lin Y, Long H, Liu H, Rao H, He Y, Rong T, Liang Y. Esophageal carcinosarcoma: a unique entity with better prognosis. Ann Surg Oncol. 2013;20:997-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Iyomasa S, Kato H, Tachimori Y, Watanabe H, Yamaguchi H, Itabashi M. Carcinosarcoma of the esophagus: a twenty-case study. Jpn J Clin Oncol. 1990;20:99-106. [PubMed] |
| 10. | Ogasawara N, Tamura Y, Funaki Y, Yamaguchi Y, Shimozato A, Yanamoto K, Takahashi E, Miyachi M, Sasaki M, Kasugai K. Rapidly growing esophageal carcinosarcoma reduced by neoadjuvant radiotherapy alone. Case Rep Gastroenterol. 2014;8:227-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Ishida H, Fujishima F, Onodera Y, Konno-Kumagai T, Maruyama S, Okamoto H, Sato C, Heishi T, Sakurai T, Taniyama Y, Kamei T, Sasano H. Esophageal Carcinosarcoma with Basaloid Squamous Cell Carcinoma: A Case Report and Review of the Literature. Tohoku J Exp Med. 2019;249:255-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Sasajima K, Taniguchi Y, Morino K, Yamashita K, Onda M, Hao K, Takubo K. Rapid growth of a pseudosarcoma of the esophagus. J Clin Gastroenterol. 1988;10:533-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Nikitakis NG, Drachenberg CB, Papadimitriou JC. MDM2 and CDK4 expression in carcinosarcoma of the esophagus: comparison with squamous cell carcinoma and review of the literature. Exp Mol Pathol. 2002;73:198-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Ota S, Kato A, Kobayashi H, Yonezumi M, Yamaguchi J, Musashi M, Imamura M, Asaka M. Monoclonal origin of an esophageal carcinosarcoma producing granulocyte-colony stimulating factor: a case report. Cancer. 1998;82:2102-2111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Iwaya T, Maesawa C, Tamura G, Sato N, Ikeda K, Sasaki A, Othuka K, Ishida K, Saito K, Satodate R. Esophageal carcinosarcoma: a genetic analysis. Gastroenterology. 1997;113:973-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Tsuyama S, Saito T, Akazawa Y, Yanai Y, Yatagai N, Akaike K, Hayashi T, Suehara Y, Takahashi F, Takamochi K, Hashimoto T, Kajiyama Y, Tsurumaru M, Fukunaga T, Yao T. Molecular and clinicopathological analyses of esophageal carcinosarcoma with special reference to morphological change. Virchows Arch. 2019;475:415-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Lu H, Yang S, Zhu H, Tong X, Xie F, Qin J, Han N, Wu X, Fan Y, Shao YW, Mao W. Targeted next generation sequencing identified clinically actionable mutations in patients with esophageal sarcomatoid carcinoma. BMC Cancer. 2018;18:251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Zhang B, Xiao Q, Yang D, Li X, Hu J, Wang Y, Wang W. Spindle cell carcinoma of the esophagus: A multicenter analysis in comparison with typical squamous cell carcinoma. Medicine (Baltimore). 2016;95:e4768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Sanada Y, Hihara J, Yoshida K, Yamaguchi Y. Esophageal carcinosarcoma with intramural metastasis. Dis Esophagus. 2006;19:119-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Ziauddin MF, Rodriguez HE, Quiros ED, Connolly MM, Podbielski FJ. Carcinosarcoma of the esophagus--pattern of recurrence. Dig Surg. 2001;18:216-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Pesenti C, Bories E, Danisi C, Monges G, Giovannini M. Endoscopic treatment of esophageal carcinosarcoma: report of a case. Endoscopy. 2004;36:95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Xu F, Zou WB, Li XP, Xu YM, Qi XF, Hu LH, Li ZS, Yao DK. Multiple carcinosarcomas of the esophagus and stomach. Oncol Lett. 2013;5:1017-1021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Yabuuchi Y, Tanaka M, Ono H. Carcinosarcoma of the esophagus with rapid morphological change. Am J Gastroenterol. 2018;113:642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |