Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4609
Peer-review started: April 26, 2020
First decision: July 25, 2020
Revised: August 4, 2020
Accepted: August 20, 2020
Article in press: August 20, 2020
Published online: October 6, 2020
Processing time: 150 Days and 2.4 Hours
The spontaneous resorption of lumbar disk herniations (LDHs) has been widely reported. However, the majority of these reports analyze the resorption of LDHs that were displaced backwards or downwards. There have been few reports on the spontaneous resorption of upwardly displaced L4/5 LDH that has caused femoral nerve symptoms.
A 55-year-old woman presented to our hospital with acute pain in her left leg. She had been suffering from recurrent lower back pain for approximately 1 year and began to feel pain accompanied with numbness at the anterior aspect of her left leg 7 d previously. On examination, a typical L4 nerve stimulation was noted. An upwardly displaced LDH at the L4/5 level was revealed by magnetic resonance imaging. The patient attained complete relief of her symptoms after 10 wk of nonsurgical treatment and the upwardly displaced herniation almost entirely disappeared. There was no recurrence during a follow-up of 2 years.
Clinicians should be aware that the nerves disturbed by LDHs vary according to the direction of the herniations and the probable resorption of upwardly displaced LDHs should be considered before making a decision on surgery.
Core Tip: This is the first report of the spontaneous resorption of upwardly displaced L4/5 lumbar disk herniation that caused femoral nerve symptoms. No secular trends in the incidence of resorption were identified in the literature review.
- Citation: Wang Y, Liao SC, Dai GG, Jiang L. Resorption of upwardly displaced lumbar disk herniation after nonsurgical treatment: A case report. World J Clin Cases 2020; 8(19): 4609-4614
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4609.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4609
Lumbar disc herniation (LDH) can be treated non-surgically or surgically[1,2]. Resorption of LDH is one of the primary factors that contributes to relief following nonsurgical treatments; and thus has clinical significance in the nonsurgical treatment of LDH. The spontaneous resorption of LDHs has been widely reported[3-16]. However, the majority of these reports analyze the resorption of LDHs that were displaced backwards or downwards in the form of sequestration, extrusion, protrusion, or bulging[17]. The natural history of upwardly displaced LDHs has rarely been documented. In addition, upwardly migrated LDHs may exhibit a different pattern in disturbing nerve roots compared with LDHs displaced backwards or downwards. Therefore, we present this case study to demonstrate the femoral nerve symptoms that result from upwardly displaced L4/5 LDHs and provide an example of the spontaneous resorption of an upwardly displaced L4/5 LDH.
A 55-year-old woman presented to our hospital with acute pain in her left leg for 7 d.
The patient had been suffering from recurrent low back pain for approximately 1 year, and her pain was relieved spontaneously or after nonsurgical treatment. She began to feel pain accompanied by numbness at the anterior aspect of her left leg 7 d before presentation.
The patient underwent appendectomy for appendicitis 15 years ago.
Clinical examination revealed the following: a negative Lasegue’s sign and a positive femoral nerve stretch test of her left leg, hypoesthesia over the distribution of the left femoral nerve, and normal muscle strength and deep tendon reflexes of her legs with a bilateral negative Babinski’s sign. She perceived an electric shock-like sensation in her left leg prompted by lumbar spine extension.
Routine blood, blood biochemistry, serum C-reactive protein level and erythrocyte sedimentation rate were normal.
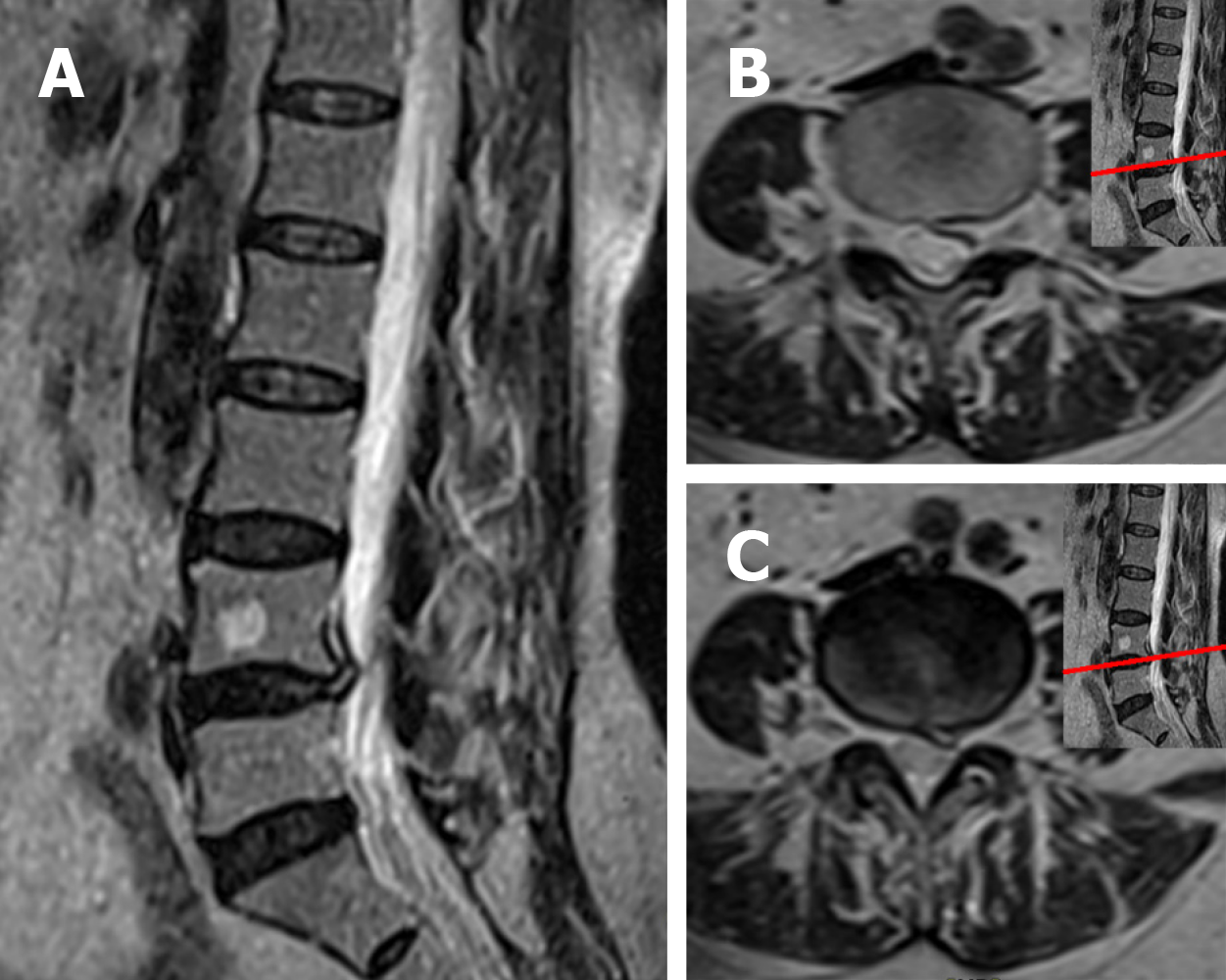
An upwardly displaced LDH at the L4/5 level was revealed by magnetic resonance imaging (MRI) (Figure 1).
The patient was diagnosed with an upwardly displaced L4/5 LDH.
The patient received nonsurgical treatment with Traditional Chinese Medicine for 4 wk, which included bed rest, acupuncture, massage, moxibustion and Chinese medicine fumigation. All of her symptoms were relieved except for moderate lumbago, and she was discharged from the hospital. She underwent a follow-up visit every 2 wk and performed home-based exercise therapy following the doctor's instructions for 6 wk.
She attained complete relief of her symptoms 10 wk after presentation. The upwardly displaced herniation mostly disappeared on the second MRI, which was performed 10 wk after her initial visit (Figure 2). There was no recurrence during a follow-up of 2 years, and only a small amount of herniated disc tissue was found on the third MRI, which was performed 2 years after the patient’s initial visit (Figure 3).
The resorption of LDHs after nonsurgical treatments has been widely reported since the first case in 1984. In these reports, the LDHs were characterized as decreasing or disappearing over time, and the nonsurgical treatments in these reports included bed rest, lumbar support, analgesics, oral steroids, non-steroidal anti-inflammatory drugs, epidural steroid injection, caudal epidural injections of local anesthetic, manipulation, hot back, ultrasound, electrotherapy, traction, exercises, Traditional Chinese Medicine and integrative Korean medicine[3-16]. However, which of these treatments are essential for promoting resorption and the time when resorption takes place remains unclear.
The incidence of resorption varies in the existing reports depending on the different follow-up times. Lee reported the highest incidence of resorption of 96% with an average follow-up time of 341.38 ± 306.83 d[3]. Two studies reported no resorption with follow-ups of 45 d[4] and 20 d[5], suggesting that resorption should not be expected to occur too soon after nonsurgical treatments. The relationship between the incidence of resorption and the time of follow-up was not consistent in these studies, and no secular trends in the incidence of resorption were identified in these studies (Table 1).
| Ref. | Year | Incidence of resorption | Follow-up time |
| Kamanli et al[6] | 2010 | 19% | 4-6 wk |
| Demirel et al[7] | 2017 | 90% | 3 mo |
| Iwabuchi et al[8] | 2010 | 62% | Average 4 mo |
| Gallucci et al[9] | 1995 | 73% | 6 mo |
| Shan et al[10] | 2014 | 80% | 6 mo |
| Autio et al[11] | 2006 | 93% | 1 yr |
| El Barzouhi et al[12] | 2013 | 93% | 1 yr |
| Fagerlund et al[13] | 1990 | 73% | 2 yr |
| Cribb et al[14] | 2017 | 93% | Average 2 yr |
| Shin et al[15] | 2014 | 58% | 3 yr |
| Ilkko et al[16] | 1993 | 83% | Average 5.2 yr |
A meta-analysis reported the overall incidence of resorption of LDHs to be 66.66% (95%CI: 55.12%-78.21%)[18], and randomized controlled trials have confirmed that resorption is a widespread phenomenon in patients with LDHs[7,12,19]. The North American Spine Society has suggested that the probability of resorption should be considered during the management of LDH[20]. Although it is well known that sequestrated and large LDHs are more likely to undergo resorption[21-23], it is still not possible to accurately predict resorption in individual cases; even the possibility of resorption cannot be predicted for individual cases. Thus, for many cases that present without cauda equina syndrome or progressive neurological deficits, there remains no consensus on whether to perform surgical treatments or nonsurgical treatments[1]. However, we cannot ignore the physical decompression that occurs during resorption of LDH, and the probability of resorption should be considered before making a decision on surgery.
The epidural space enlarges down the vertebral column[24]. Thus, in the majority of cases, the LDH tends to protrude downward under the influence of gravity. Most of the existing studies reported resorption of backwardly or downwardly displaced LDHs, while upwardly displaced LDHs have been reported less. Macki et al[25] reported a case of an upwardly migrated L4/5 LDH that was compressing the L5 nerve root and resorbed 5 mo after nonsurgical treatment. Another case presented the resorption of an upwardly migrated L4/5 LDH in a pregnant woman with sciatica[26]. The upwardly displaced L4/5 LDHs of these two cases stimulated the L5 nerve root and resulted in sciatica.
There have been few reports on the spontaneous resorption of upwardly displaced L4/5 LDH that has caused femoral nerve symptoms. In most cases, LDH compresses the nerve root corresponding to the lower vertebral level; accordingly, L4/5 LDH disturbs the L5 nerve root, which originates at the L4/5 disc level and goes downward to the L5/S1 intervertebral foramen, subsequently causing sciatica. In rare cases, the L4/5 disc moves upward along the spinal canal to above the L4/5 disc level, and the herniated disc material is still connected to the L4/5 disc; the herniation may disturb the L5 nerve root at the starting point at the L4/5 disc level or disturb the L4 nerve root, which originates at the L4 vertebral level and leaves the spinal canal above the L4/5 disc plane, or disturb both. In the present case, the herniated L4/5 disc moved upwards to the L4 vertebral level above the starting point of the L5 nerve root, similar to a prolapsed L3/4 disc, leading to compression of the L4 nerve root, which originates at the L4 vertebral level and results in femoral nerve symptoms. The upwardly displaced L4/5 LDH of this patient almost completely disappeared and was accompanied by complete relief of the femoral nerve symptoms 10 wk following nonsurgical treatment with Traditional Chinese Medicine.
Upwardly displaced LDHs are not very common. To our knowledge, this is the first report of the spontaneous resorption of upwardly displaced L4/5 LDH that has caused femoral nerve symptoms. This case also demonstrated that the nerves disturbed vary according to the direction of the herniation. Resorption of the upwardly displaced LDH in this case corresponds with existing reports on the resorption of LDHs.
The nonsurgical treatment of this patient was successful. Clinicians should be aware that the nerves disturbed by LDHs vary according to the direction of the herniation, and the probable resorption of upwardly displaced LDHs should be considered before making a decision on surgery. Future research should explore the relationship between resorption and time as well as methods for predicting resorption.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Sichuan Medical Association, No. 510192181000873.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saad K S-Editor: Zhang L L-Editor: Webster JR P-Editor: Xing YX
| 1. | Ramaswami R, Ghogawala Z, Weinstein JN. Management of Sciatica. N Engl J Med. 2017;376:1175-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, Thomeer RT, Koes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245-2256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 489] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 3. | Lee J, Kim J, Shin JS, Lee YJ, Kim MR, Jeong SY, Choi YJ, Yoon TK, Moon BH, Yoo SB, Hong J, Ha IH. Long-Term Course to Lumbar Disc Resorption Patients and Predictive Factors Associated with Disc Resorption. Evid Based Complement Alternat Med. 2017;2017:2147408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Santilli V, Beghi E, Finucci S. Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: a randomized double-blind clinical trial of active and simulated spinal manipulations. Spine J. 2006;6:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Fan Y, Zhao P. A randomized, placebo-controlled trial of vertebral mobilization treatment on patients with acute radiculopathy caused by lumbar disc herniation. Physiotherapy. 2015;101:eS1714-eS1715. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Kamanli A, Karaca-Acet G, Kaya A, Koc M, Yildirim H. Conventional physical therapy with lumbar traction; clinical evaluation and magnetic resonance imaging for lumbar disc herniation. Bratisl Lek Listy. 2010;111:541-544. [PubMed] |
| 7. | Demirel A, Yorubulut M, Ergun N. Regression of lumbar disc herniation by physiotherapy. Does non-surgical spinal decompression therapy make a difference? Double-blind randomized controlled trial. J Back Musculoskelet Rehabil. 2017;30:1015-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Iwabuchi M, Murakami K, Ara F, Otani K, Kikuchi S. The predictive factors for the resorption of a lumbar disc herniation on plain MRI. Fukushima J Med Sci. 2010;56:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Gallucci M, Bozzao A, Orlandi B, Manetta R, Brughitta G, Lupattelli L. Does postcontrast MR enhancement in lumbar disk herniation have prognostic value? J Comput Assist Tomogr. 1995;19:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Shan Z, Fan S, Xie Q, Suyou L, Liu J, Wang C, Zhao F. Spontaneous resorption of lumbar disc herniation is less likely when modic changes are present. Spine (Phila Pa 1976). 2014;39:736-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Autio RA, Karppinen J, Niinimäki J, Ojala R, Kurunlahti M, Haapea M, Vanharanta H, Tervonen O. Determinants of spontaneous resorption of intervertebral disc herniations. Spine (Phila Pa 1976). 2006;31:1247-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 97] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | el Barzouhi A, Vleggeert-Lankamp CL, Lycklama à Nijeholt GJ, Van der Kallen BF, van den Hout WB, Jacobs WC, Koes BW, Peul WC; Leiden-The Hague Spine Intervention Prognostic Study Group. Magnetic resonance imaging in follow-up assessment of sciatica. N Engl J Med. 2013;368:999-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Fagerlund MK, Thelander U, Friberg S. Size of lumbar disc hernias measured using computed tomography and related to sciatic symptoms. Acta Radiol. 1990;31:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 14. | Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007;89:782-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Shin JS, Lee J, Kim MR, Shin BC, Lee MS, Ha IH. The long-term course of patients undergoing alternative and integrative therapy for lumbar disc herniation: 3-Year results of a prospective observational study. Bmj Open. 2014;4. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Ilkko E, Lähde S, Heikkinen ER. Late CT-findings in non-surgically treated lumbar disc herniations. Eur J Radiol. 1993;16:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Chiu CC, Chuang TY, Chang KH, Wu CH, Lin PW, Hsu WY. The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clin Rehabil. 2015;29:184-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain Physician. 2017;20:E45-E52. [PubMed] |
| 19. | Ozturk B, Gunduz OH, Ozoran K, Bostanoglu S. Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc herniation. Rheumatol Int. 2006;26:622-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL Jr, Toton JF; North American Spine Society. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14:180-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 396] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 21. | Delauche-Cavallier MC, Budet C, Laredo JD, Debie B, Wybier M, Dorfmann H, Ballner I. Lumbar disc herniation. Computed tomography scan changes after conservative treatment of nerve root compression. Spine (Phila Pa 1976). 1992;17:927-933. [PubMed] |
| 22. | Ahn SH, Ahn MW, Byun WM. Effect of the transligamentous extension of lumbar disc herniations on their regression and the clinical outcome of sciatica. Spine (Phila Pa 1976). 2000;25:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Maigne JY, Rime B, Deligne B. Computed tomographic follow-up study of forty-eight cases of nonoperatively treated lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 1992;17:1071-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 90] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Wiltse LL, Fonseca AS, Amster J, Dimartino P, Ravessoud FA. Relationship of the dura, Hofmann's ligaments, Batson's plexus, and a fibrovascular membrane lying on the posterior surface of the vertebral bodies and attaching to the deep layer of the posterior longitudinal ligament. An anatomical, radiologic, and clinical study. Spine (Phila Pa 1976). 1993;18:1030-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 112] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Macki M, Hernandez-Hermann M, Bydon M, Gokaslan A, McGovern K, Bydon A. Spontaneous regression of sequestrated lumbar disc herniations: Literature review. Clin Neurol Neurosurg. 2014;120:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Orief T, Orz Y, Attia W, Almusrea K. Spontaneous resorption of sequestrated intervertebral disc herniation. World Neurosurg. 2012;77:146-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |