Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4565
Peer-review started: May 6, 2020
First decision: May 15, 2020
Revised: May 24, 2020
Accepted: August 26, 2020
Article in press: August 26, 2020
Published online: October 6, 2020
Processing time: 144 Days and 12.6 Hours
Angiosarcoma is a rare disease with a poor prognosis. Its occurrence in the small intestine is low, and gastrointestinal bleeding caused by small intestinal angiosarcoma is unusual.
Here, we report the case of a 57-year-old man who presented with hematochezia for 1 mo. The patient had a medical history of chronic viral hepatitis B for 15 years. The causes of gastrointestinal bleeding were initially diagnosed as esophagogastric variceal bleeding or portal hypertensive gastropathy before endoscopy. However, after a complicated diagnostic and therapeutic process, including gastroendoscopy, colonoscopy, contrast-enhanced computed tomographic (CT), positron emission computed tomography/CT, capsule endoscopy, and pathological and immunohistochemical examinations, small intestinal angiosarcoma was diagnosed. Arrest of bleeding was achieved after surgical treatment. Furthermore, the patient had lung cancer with bone and adrenal metastases. At the follow-up 10 mo after the operation, the patient was alive.
Gastroenterologists should maintain strong vigilance to small intestinal angiosarcoma, which is necessary for the early identification of this infrequent but fatal disease.
Core Tip: Angiosarcoma is a rare disease with a poor prognosis. Its occurrence in the small intestine is low, and gastrointestinal bleeding caused by small intestinal angiosarcoma is unusual. We report a rare case of small intestinal angiosarcoma that caused gastrointestinal hemorrhage in a patient with a history of chronic hepatitis B and lung cancer with bone and adrenal metastases. The diagnosis of a small intestinal angiosarcoma was made by pathological and immunohistochemical examinations and arrest of bleeding was achieved after surgical treatment. Gastroenterologists should maintain strong vigilance to small intestinal angiosarcoma, which is necessary for the early identification of this infrequent but fatal disease.
- Citation: Hui YY, Zhu LP, Yang B, Zhang ZY, Zhang YJ, Chen X, Wang BM. Gastrointestinal bleeding caused by jejunal angiosarcoma: A case report. World J Clin Cases 2020; 8(19): 4565-4571
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4565.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4565
Angiosarcomas are rare, aggressive mesenchymal sarcomas of cells with vascular endothelial features, which account for 1%–2% of all sarcomas that occur in the skin and subcutaneous tissues[1]. Angiosarcomas can be found in any part of the body, primarily in the skin, subcutaneous tissues, breast, heart, and liver, but extremely rare in the gastrointestinal tract especially the small intestine[2]. The specific etiology of angiosarcoma remain unknown. Several risk factors have been associated with its development, including radiation exposure, vinyl chloride, thorotrast, arsene, and chronic lymphedema[3]. The clinical signs and symptoms of small intestinal angiosarcoma are nonspecific, including nonspecific abdominal pain, weight loss, anemia, intestinal perforation, nausea/vomiting, intestinal obstruction, or hemorrhage[4]. A rapid and accurate diagnosis of small intestinal angiosarcoma is difficult due to this variability in clinical presentation. Moreover, the prognosis of small intestinal angiosarcoma is extremely poor due to the limited diagnostic methods for lesions in the small intestine and the late detection. It is rare for patients with intestinal angiosarcomas to live for much more than a year after diagnosis[5].
In this paper, we report a 57-year-old man who presented with hematochezia for 1 mo due to angiosarcoma of the small intestine; moreover, the patient had a medical history of chronic viral hepatitis B for 15 years.
A 57-year-old man who presented with a 1-mo history of intermittent hematochezia was admitted to our hospital.
The patient complained of intermittent hematochezia since a month ago, once every 2 d. There was no hematemesis, nausea, vomiting, or abdomen pain and no discomfort such as fever, cough, chest tightness, or difficult breathing. He presented to hospital due to severe fatigue and blood routine examination before hospitalization showed a hemoglobin level of 58 g/L with normal white blood cell and platelet counts, MCV level of 70.5 (82.0–100.0) fl, MCH level of 22.0 (27.0–34.0) pg, and MCHC level of 312 (316–354) g/L. Fecal occult blood test was positive.
The patient had a history of chronic viral hepatitis B for 15 years.
The vital signs were stable on admission. The patient’s temperature was 36.6 °C. Physical examination revealed pale skin. We observed no ascites, spider angioma, palmar erythema, or splenomegaly.
Initial laboratory investigations showed a hemoglobin level of 60 g/L with normal white blood cell and platelet counts, MCV level of 75.2 (82.0–100.0) fl, MCH level of 23.3 (27.0–34.0) pg , MCHC level of 309 (316–354) g/L, serum ferritin level of 22.7 (21.8–274.6) ng/mL, serum iron level of 15.2 (5.4–28.6) μmol/L, and neuron-specific enolase level of 47.71 (0–16.3) μg/L. Fecal occult blood test was positive. Serum levels of other tumor markers, blood biochemistries, and urine analysis were within the normal range.
No esophageal varices or lesions were detected on the basis of gastroendoscopy and colonoscopy.
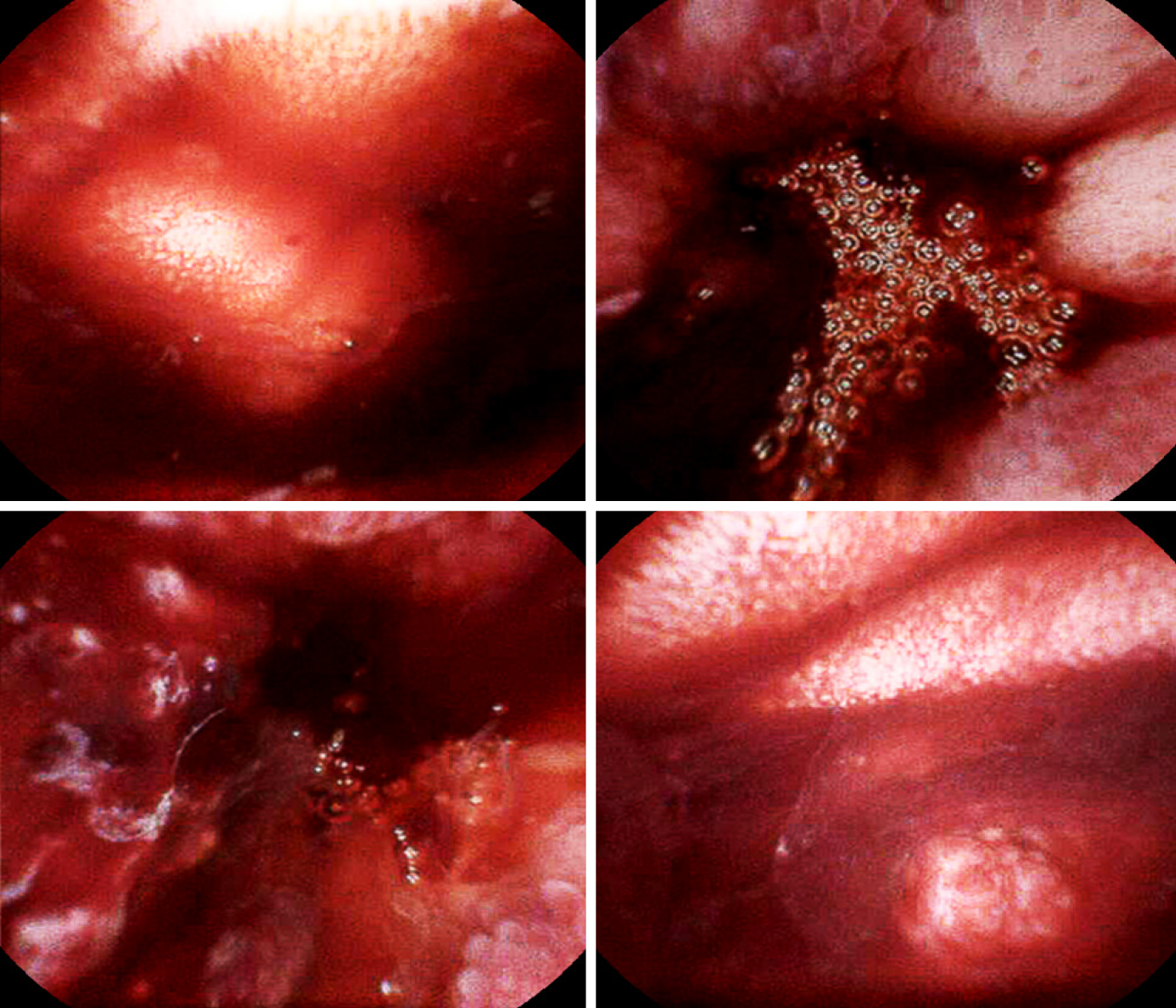
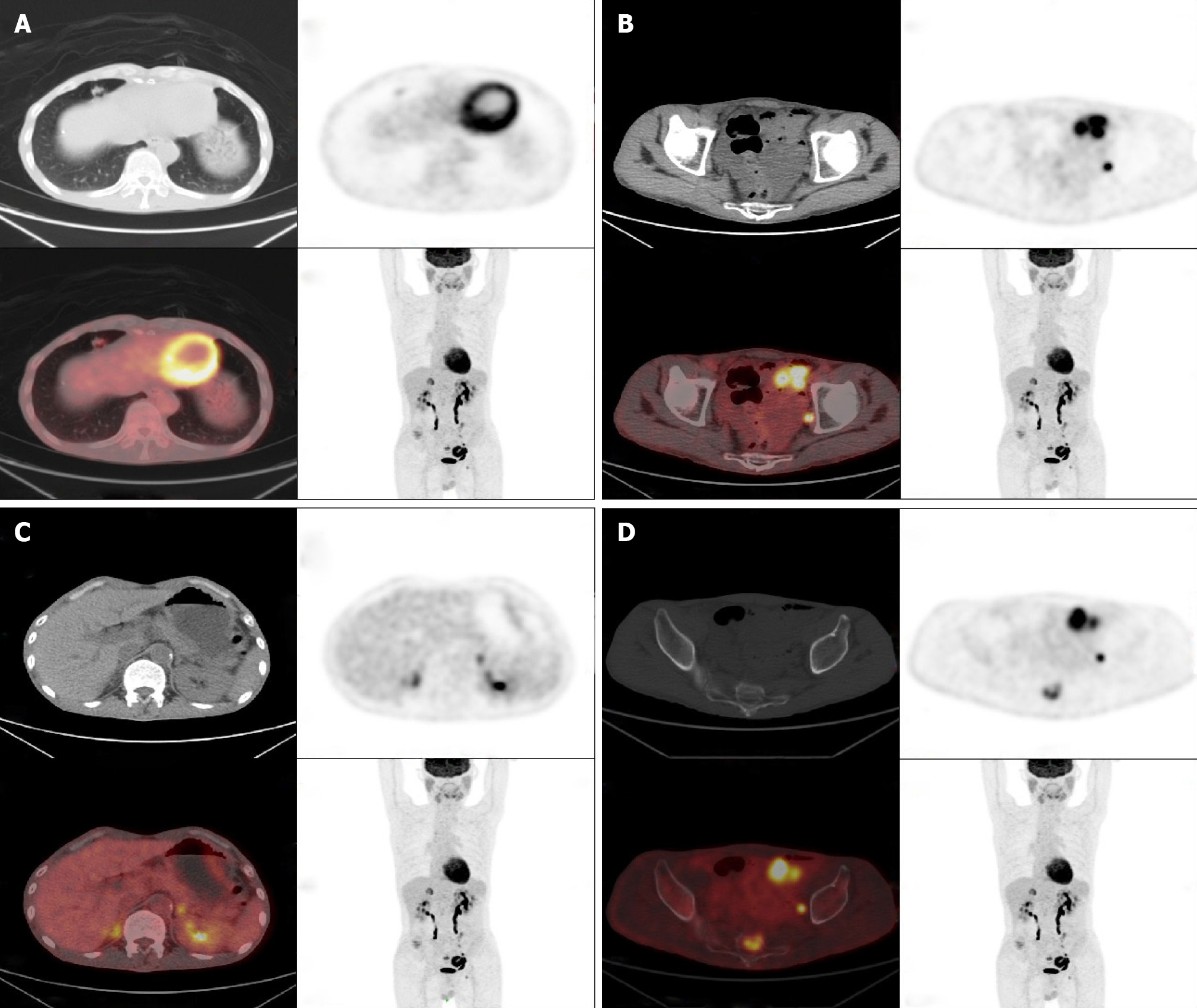
His abdominal contrast-enhanced computed tomographic (CT) scan showed segmental wall thickening and eccentric of the small intestine. The small bowel wall was enhanced with multiple lymph nodes in the abdomen and retroperitoneal space in the enhanced arterial phase. Capsule endoscopy was administered, which revealed an ulcerated eminence lesion (Figure 1) that was causing massive overt gastrointestinal bleeding. Positron emission computed tomography/CT revealed a small intestinal malignant tumor, malignant tumor of the lung, and metastatic carcinoma of adrenal glands and bones (Figure 2).
The patient was diagnosed with a primary small intestinal angiosarcoma and lung cancer with bone and adrenal metastases.
After hospitalization, repeated blood transfusions were required due to a continued drop in hemoglobin. Then, an exploratory laparotomy was performed due to persistent gastrointestinal hemorrhage, in which a tumor about 3.4 cm × 6.0 cm was found in the small intestine about 130 cm distal from the Treitz ligament (Figure 3). Partial small intestine resection with end-to-end jejunostomy was performed. Subsequently, arrest of bleeding was achieved. After surgical resection, the patient was managed with comprehensive treatment.
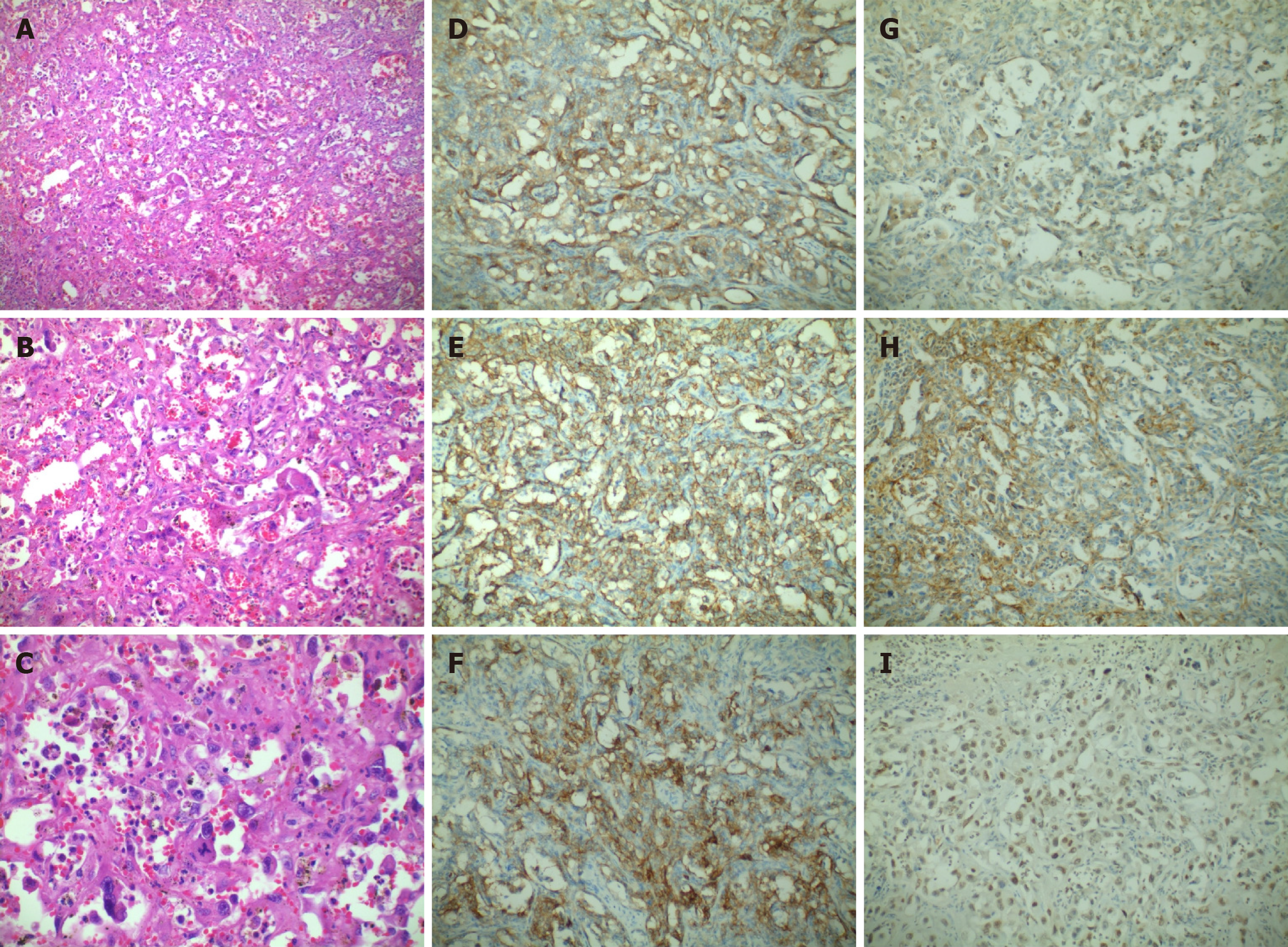
Histopathology (Figure 4) showed some vascular channels which were composed with irregular and anastomosing channels lined by enlarged epithelioid-appearing endothelial cells. Immunohistochemical staining showed positive results for CD30, CD31, CD34, Fli-1, FVIII, VEGR, EMA, CK, and ERG but negative results for SMA, CD117, DOG-1, and S-100. These results were consistent with the findings of epithelioid angiosarcoma.
A diagnostic process and adjuvant chemotherapy were refused by the patient’s relatives due to economic difficulties. The patient recovered well without any gastrointestinal bleeding events and was discharged after 8 d. At the follow-up 10 mo after the operation, the patient was alive.
Gastrointestinal hemorrhage is a critical condition requiring rapid diagnosis and prompt treatment. A big part of gastrointestinal bleedings occur in the upper or lower gastrointestinal tract; small intestinal bleeding remains a relatively uncommon event, accounting for 5%-10% of all patients with gastrointestinal hemorrhage[6]. Patients with bleeding from the small intestine generally undergo multiple diagnostic examinations and require multiple hospitalizations and blood transfusions due to the incapability of visualizing the small intestine properly. Therefore, accurately recognizing the cause and site of bleeding is a necessary condition to establish appropriate and effective treatment strategies.
Angiosarcoma is a rare malignant neoplasm of the vascular endothelium with features of the hyperproliferation and wide distribution of tumor cells. Fewer than 70 cases of small intestine angiosarcoma have been reported with only 12 initially presenting as gastrointestinal bleeding[5,7]. For our patient, it was the first report that primary small intestinal angiosarcoma causes gastrointestinal hemorrhage, who had lung cancer with bone and adrenal metastases.
The etiology of angiosarcoma is still unclear. Based on the current data, several risk factors have been implicated with its pathogenesis, including radiation exposure, postsurgery, vinyl chloride, thorotrast, arsene, and chronic lymphedema. However, the patient did not have any of these potential risk factors.
Small intestinal angiosarcoma is difficult to diagnose and delayed diagnosis often occurs due to the nonspecific clinical manifestations. In this case, capsule endoscopy was administered. The observations revealed bleeding due to an ulcerated eminence lesion in the intestinal wall of the jejunum. In addition, endoscopy, CT, and positron emission computed tomography/CT contributed to the diagnosis of angiosarcoma, but the definitive diagnosis of angiosarcoma was confirmed by pathological and immunohistochemical examinations. The abovementioned histopathological results in our case were in accord with epithelioid angiosarcoma[8].
At the present situation, adjuvant radiotherapy and/or chemotherapy after surgical resection may be helpful; however, the effect of these treatments on angiosarcoma is still unclear[5]. Despite all efforts, the prognosis of angiosarcoma is very poor. In general, patients die within several months of diagnosis, and some die shortly after surgery[1,9,10]. Patients surviving for much more than a year after intestinal angiosarcomas diagnosis are rare[5,11]. Our patient underwent surgery and achieved arrest of bleeding. However, this patient gave up adjuvant radiotherapy and chemotherapy because of financial constraints. Our patient has been alive for 10 mo during the follow-up period.
The present study may be the first case of primary small intestinal angiosarcoma leading to gastrointestinal bleeding in a patient who has not only chronic hepatitis B but also lung cancer with bone and adrenal metastases. This case report suggests that gastroenterologists should remain on high alert for small intestinal angiosarcoma, which is indispensable for the early identification of this rare but deadly disease. Moreover, capsule endoscopy is a useful method to detect the bleeding source in the small bowel.
We thank Professor Qiu-Song Chen and Ning Lu for assisting in the preparation of this manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fujimori S S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Wu YXJ
| 1. | Zacarias Föhrding L, Macher A, Braunstein S, Knoefel WT, Topp SA. Small intestine bleeding due to multifocal angiosarcoma. World J Gastroenterol. 2012;18:6494-6500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Singla S, Papavasiliou P, Powers B, Gaughan J, von Mehren M, Watson JC, Farma JM. Challenges in the treatment of angiosarcoma: a single institution experience. Am J Surg. 2014;208:254-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Ni Q, Shang D, Peng H, Roy M, Liang G, Bi W, Gao X. Primary angiosarcoma of the small intestine with metastasis to the liver: a case report and review of the literature. World J Surg Oncol. 2013;11:242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Turan M, Karadayi K, Duman M, Ozer H, Arici S, Yildirir C, Koçak O, Sen M. Small bowel tumors in emergency surgery. Ulus Travma Acil Cerrahi Derg. 2010;16:327-333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Nai Q, Ansari M, Liu J, Razjouyan H, Pak S, Tian Y, Khan R, Broder A, Bagchi A, Iyer V, Hamouda D, Islam M, Sen S, Yousif A, Hu M, Lou Y, Duhl J. Primary Small Intestinal Angiosarcoma: Epidemiology, Diagnosis and Treatment. J Clin Med Res. 2018;10:294-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997;92:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Li R, Ouyang ZY, Xiao JB, He J, Zhou YW, Zhang GY, Li Q, Gu H, Leng AM, Liu T. Clinical Characteristics and Prognostic Factors of Small Intestine Angiosarcoma: a Retrospective Clinical Analysis of 66 Cases. Cell Physiol Biochem. 2017;44:817-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11:983-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 538] [Cited by in RCA: 666] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 9. | Fraiman G, Ganti AK, Potti A, Mehdi S. Angiosarcoma of the small intestine: a possible role for thalidomide? Med Oncol. 2003;20:397-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Zhai ZZ, Wang L, Zuo XL. A Rare Cause of Gastrointestinal Bleeding in a Patient With a History of Alcoholic Cirrhosis. Gastroenterology. 2019;156:e6-e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Lahat G, Dhuka AR, Hallevi H, Xiao L, Zou C, Smith KD, Phung TL, Pollock RE, Benjamin R, Hunt KK, Lazar AJ, Lev D. Angiosarcoma: clinical and molecular insights. Ann Surg. 2010;251:1098-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 158] [Article Influence: 10.5] [Reference Citation Analysis (0)] |