Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4535
Peer-review started: March 17, 2020
First decision: July 25, 2020
Revised: July 31, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: October 6, 2020
Processing time: 194 Days and 18.8 Hours
Neonatal distal humeral physeal fractures are rare and difficult to diagnose. Thus, missed diagnoses and delayed healing are possible. Few studies have reported surgical treatment, because a callus may develop at the fracture site 5 d after the fracture, resulting in difficult reduction, and reduction of the limb may cause further physeal injury. Other surgical challenges include the provision of adequate anesthesia and complexity of the operation. However, without appropriate reduction and fixation, a varus elbow deformity may develop. Manual reduction and percutaneous pin fixation are ideal treatment options.
A 4-day-old neonate with left elbow pain accompanied by limited movement for 4 d was admitted, and diagnosed with delayed physeal fracture of the distal humerus based on physical examination, ultrasonography, and magnetic resonance imaging. The patient was treated by manual reduction combined with percutaneous pin fixation under arthrography. Postoperatively, the reduction was successful. The upper limbs could have been lifted and the fingers could have been moved freely on the second day after the operation.
The techniques of manual reduction and percutaneous pin fixation, to treat neonatal distal humeral physeal fractures, are safe and reliable.
Core Tip: Physeal fractures of the distal humerus are rare in the neonate, and can be easily missed or misdiagnosed. Only a few reports of the management of such cases exist. Early diagnosis and treatment can be challenging. In this article, we present the case of a 4-day-old neonate with a left distal humeral physeal fracture, and introduce the use of manual reduction and percutaneous pin fixation under arthrography. Excellent results were achieved in this case. The techniques are an ideal treatment for this injury.
- Citation: Tan W, Wang FH, Yao JH, Wu WP, Li YB, Ji YL, Qian YP. Percutaneous fixation of neonatal humeral physeal fracture: A case report and review of the literature. World J Clin Cases 2020; 8(19): 4535-4543
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4535.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4535
Physeal fracture of the distal humerus is a rare injury in neonates that can be easily missed or misdiagnosed. Both vaginal delivery and cesarean delivery of newborns can induce this injury. Obstetric factors, such as difficult delivery, macrosomia, and cephalopelvic disproportion, are risk factors for this type of injury, and a breech delivery or emergency cesarean section can be extremely risky[1-6]. In addition, child abuse can also be a contributing factor to the injury[7]. Congenital diseases like congenital rickets, mucopolysaccharidosis, osteogenesis imperfecta, and other metabolic bone diseases may also be primary causes of the injury, in which neonatal fracture may be the first symptom of those diseases[2,3]. The main pathogenic mechanism is associated with the application of rotary shear force or traction to the epiphysis of the distal humerus, resulting in traumatic separation[2,4,8-10]. In neonates, the physis of the distal humerus is smooth and transverse without ossification centers, which is the weakest point of the distal humerus that is prone to physeal fractures due to rotary shear force or traction[3,7,11,12].
The epiphysis of the injured site is not yet ossified in the neonate, which makes it difficult to detect the injury on plain radiographs of the elbow. Thus, this injury is prone to escape diagnosis or be misdiagnosed. In most of the previous reports of treatment with closed or open reduction under anesthesia, fracture malunion was the typical outcome following a missed diagnosis[11,13-15].
A few researchers have reported no significant difference in function or appearance between the injured side and the healthy side at a later stage, even if the affected limb was not subjected to reduction; however, due to the long fixation time, obvious swelling that may occur, and difficult care of the child, this conclusion was not supported by a long-term follow-up[3,10]. The neonatal arm is too short to exert manipulative reduction to fix the fracture, compared with the arms of older children. Previous reports have not mentioned specific methods of manual reduction and fixation. In June 2019, we performed closed manual reduction and percutaneous pin fixation to treat a physeal fracture of the distal humerus in a neonate, with the aid of arthrography. Postoperative arthrography revealed that the reduction was successful. This article reports the case retrospectively and reviews the relevant literature.
A 4-day-old neonate was admitted to our hospital with left elbow pain accompanied by limited movement for 1 d.
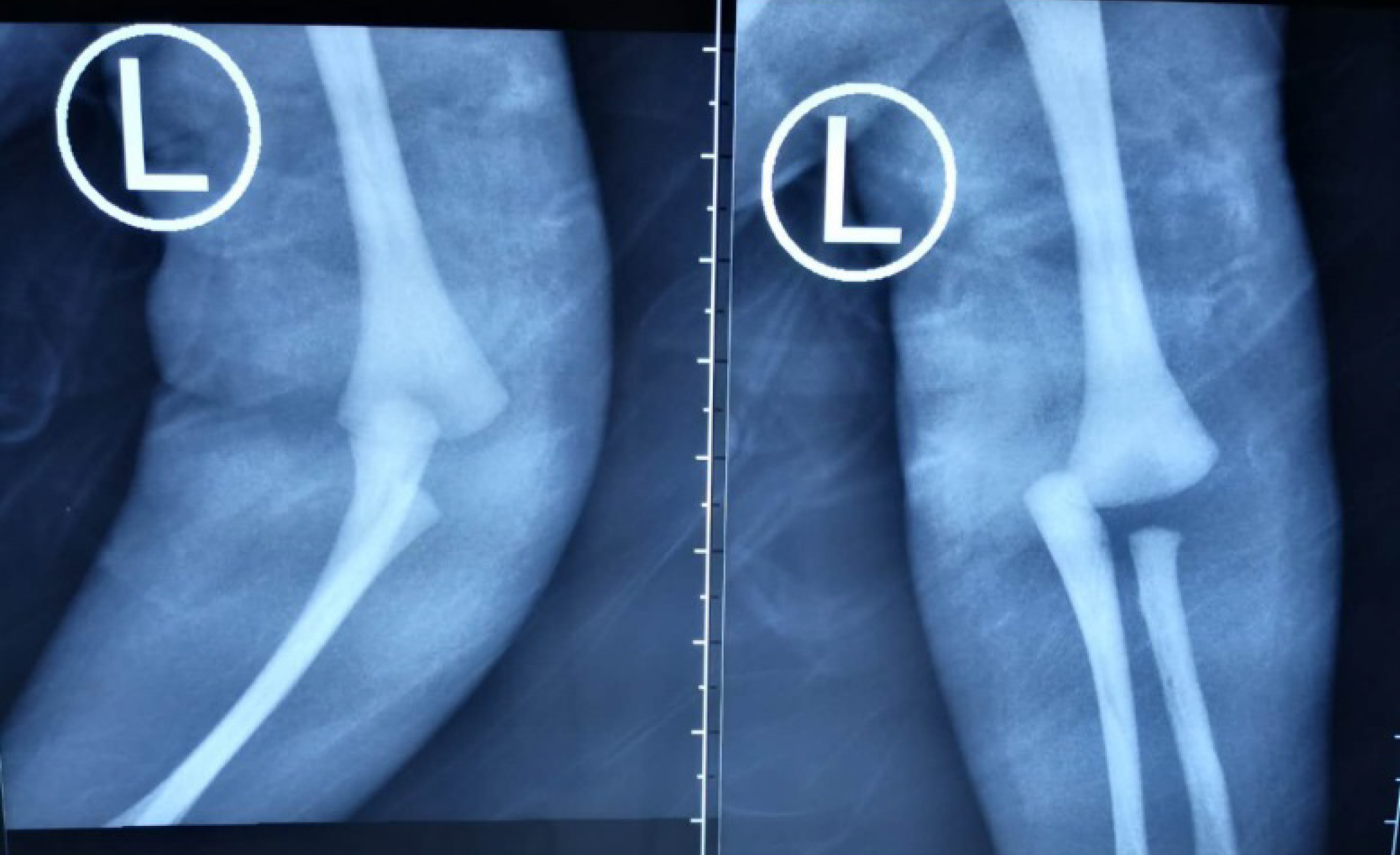
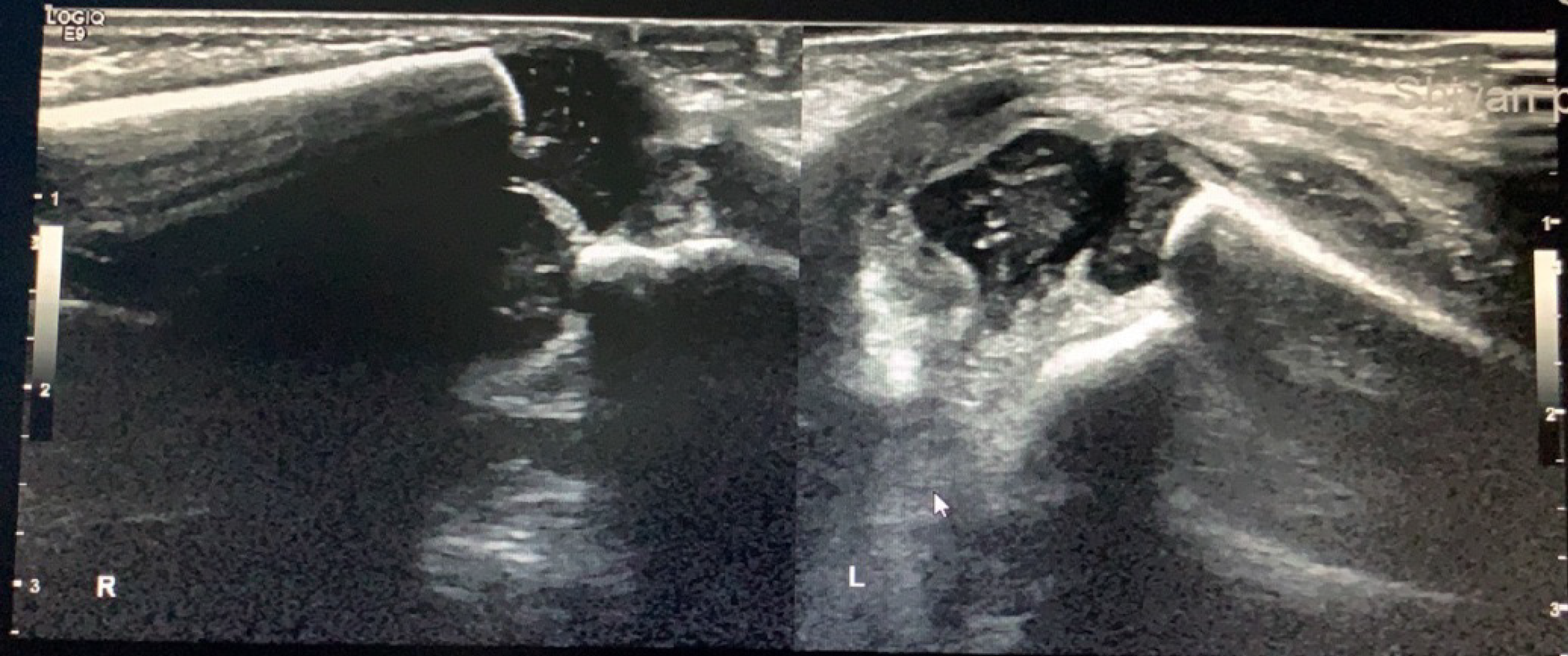
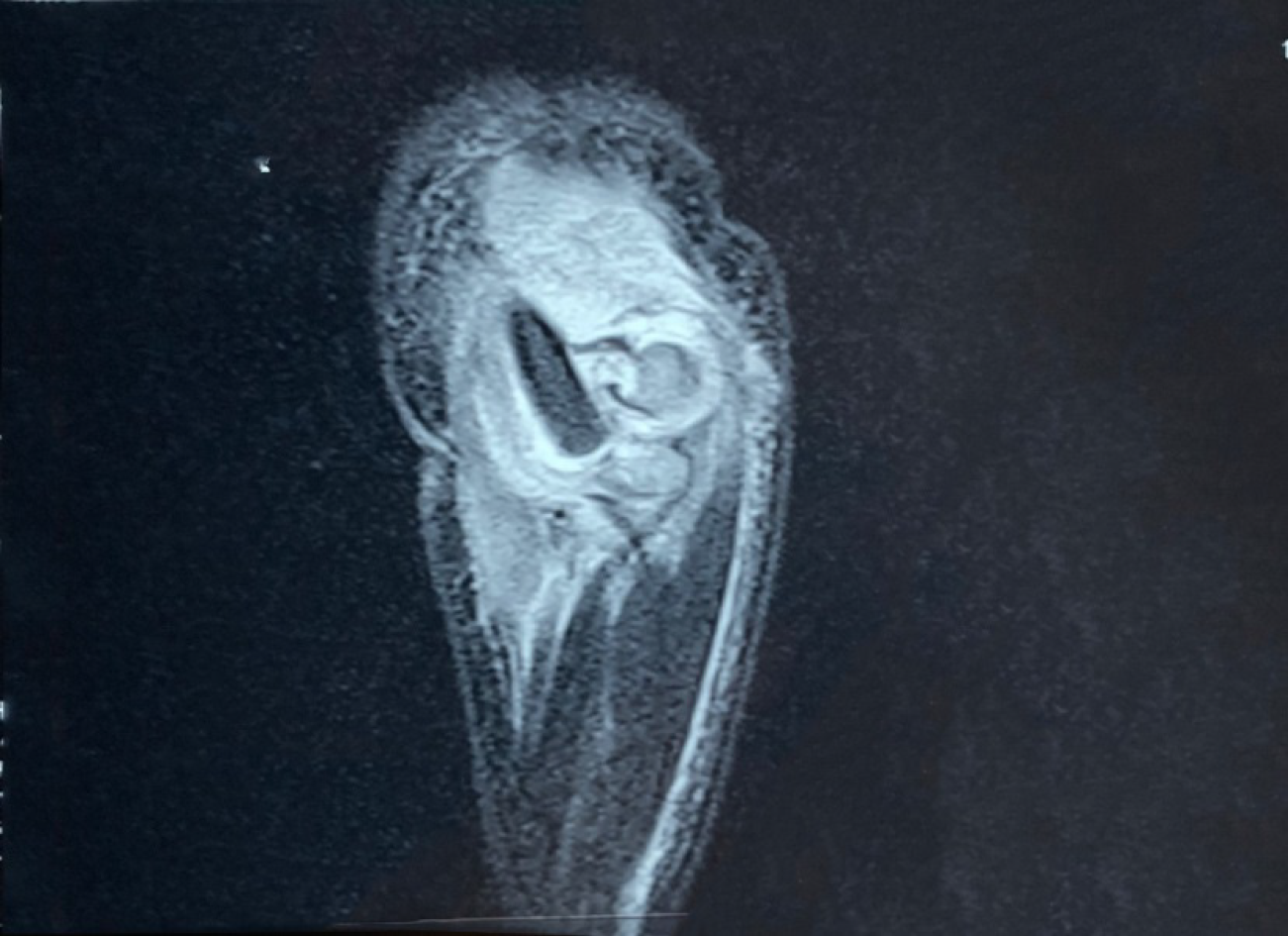
The patient, who was born at another hospital, was noted by a nurse, during a bath on the third day after birth, to have abnormal movement of his left upper limb and swelling of the elbow joint, accompanied by mild tenderness, which made him cry excessively. Anteroposterior and lateral radiographs of the elbow joint indicated dislocation of the elbow joint (Figure 1). Emergency ultrasonography and magnetic resonance imaging (MRI) were performed, which confirmed the existence of a fracture and separation of the distal humeral physis of the left elbow (Figures 2 and 3). Two attempts at manual reduction by the local orthopedists failed to reset the fracture; hence, the patient was transferred to our hospital and arrived on the fourth day after birth.
Physical examination revealed swelling of the elbow joint with mild tenderness, and limited motion of the left upper limb (Figure 4).
No abnormalities on preoperative examination.
Anteroposterior and lateral radiographs of the elbow joint indicated dislocation of the elbow joint. Preoperative MRI and ultrasonography suggested physeal fracture of the left distal humerus, swollen soft tissue surrounding the elbow joint, and no evidence of callus formation at the distal end of the fracture.
Physeal fracture of the left distal humerus.
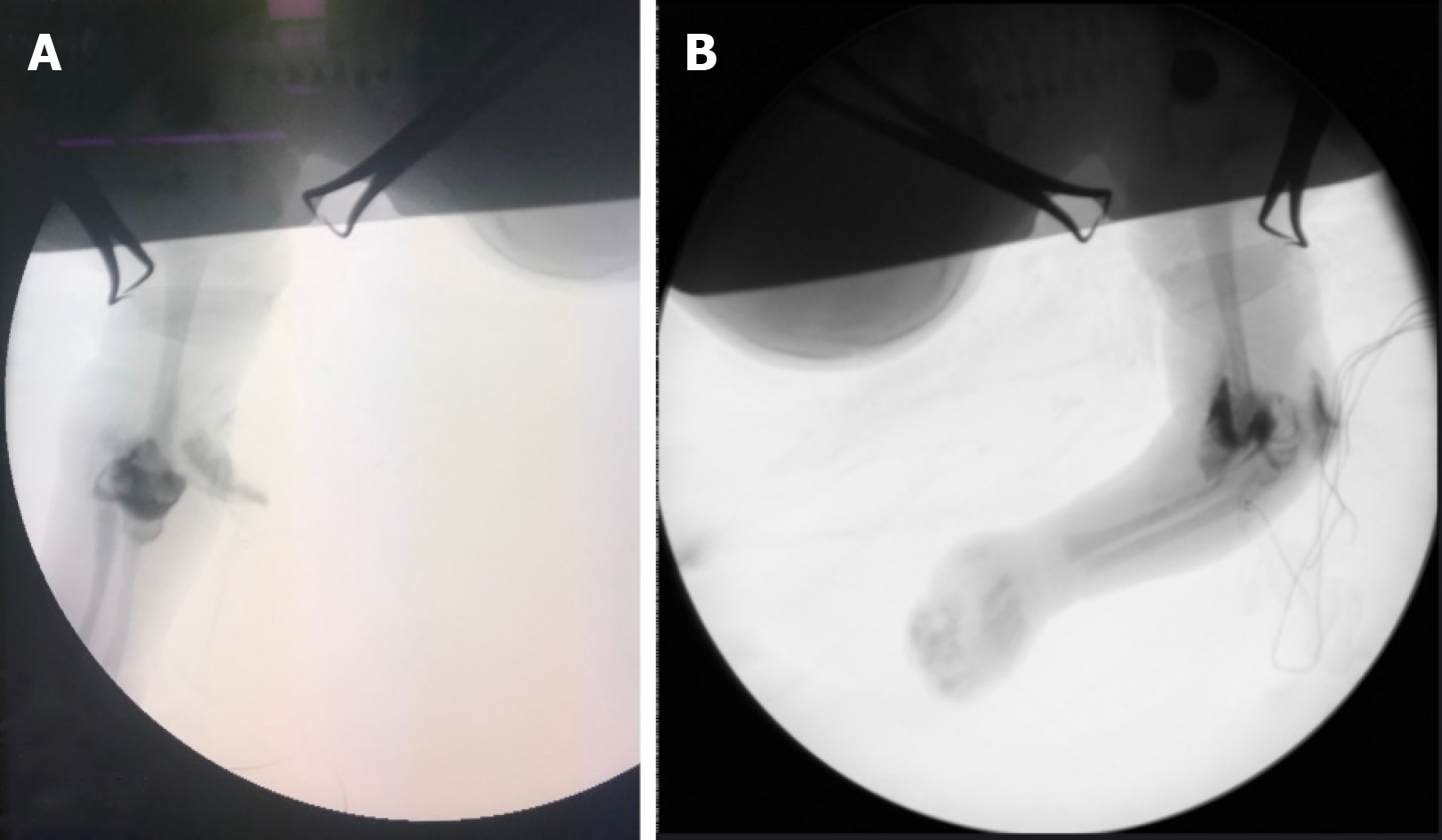
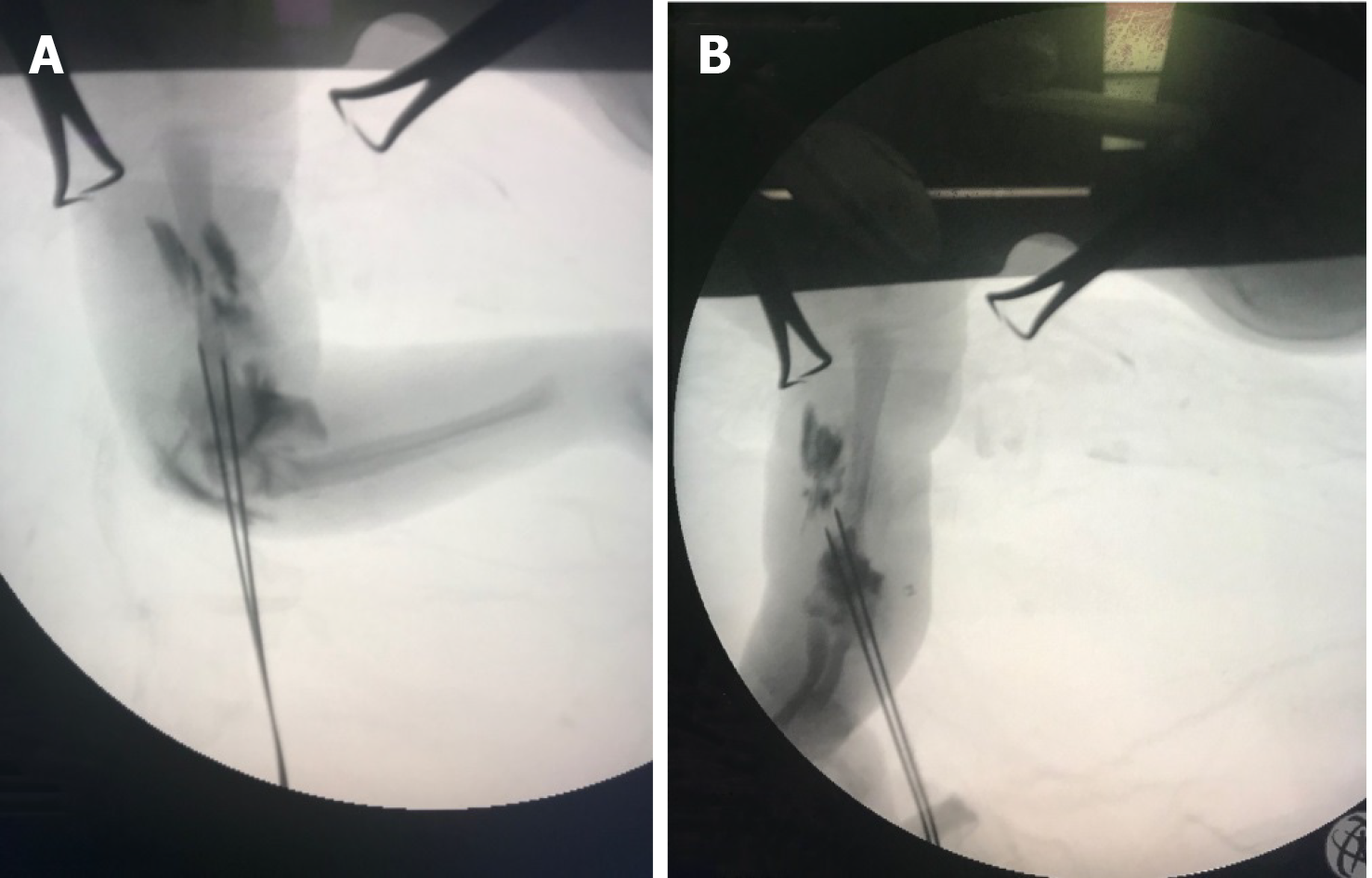
An emergency surgery was performed under inhalation anesthesia. During the operation, elbow arthrography was performed, revealing physeal fracture of the left distal humerus (Figure 5). The surgeon stood between the limbs and the head of the patient, and used a single-hand technique for reduction. The surgeon pulled the patient's forearm with his left thumb, forefinger, and middle finger, pushing the medial condyle of the distal humerus with his left little finger, while the surgeon held the upper arm of the patient with his right thumb and forefinger (Figure 6). The elbow was flexed to 30° with gradual traction and kept traction for 2 min, after which the left middle finger of the surgeon was gradually used as the fulcrum to flex and pronate the forearm. Finally, the forearm was held in place at extreme flexion with the surgeon’s thumb and forefinger.
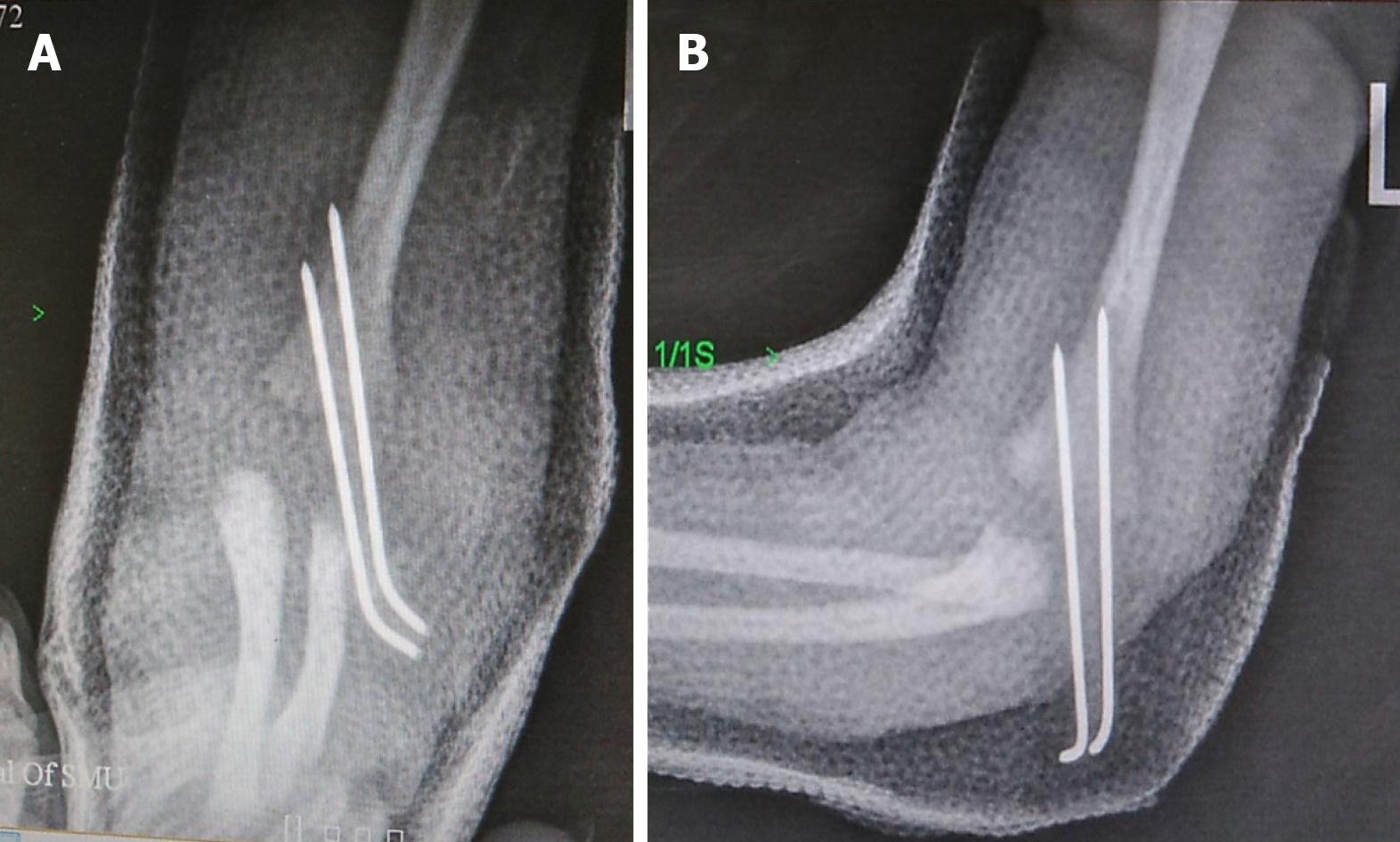
The fractures were fixed, using two Kirschner wires that were inserted from the lateral condyle of the humerus to cross the fracture line, with the aid of an electric drill in the right hand of the surgeon (Figure 7). Satisfactory reduction was confirmed by C-arm fluoroscopy (Figure 8). The patient’s upper limb was immobilized to 50° of elbow flexion by using a cast.
On the second day after the operation, the upper limbs of the patient could have been lifted and the fingers could have been moved freely.
In terms of differential diagnoses, a physeal fracture of the distal humerus in neonates needs to be differentiated from dislocation of the elbow and brachial plexus palsy. The manifestation of a dislocated elbow is very similar to that of a physeal fracture of the distal humerus. The main difference is the fact that the relationship between the medial and lateral condyles of the humerus and the olecranon is maintained in a physeal fracture of the distal humerus, even after injury; however, in elbow dislocations, the relationship of the medial and lateral condyles and olecranon appears to be disrupted[5,8,9,16-18].
Therefore, if a neonate has the above-mentioned clinical manifestations and physical examination suggests a normal three-point relationship between the medial and lateral condyles of the humerus and olecranon of the ulna, the possibility of a physeal fracture of the distal humerus should be considered. Furthermore, the physeal fracture can be distinguished from dislocation of the elbow and humeral lateral condyle fractures. Nevertheless, it is often difficult to identify the injury in this way when the swelling is severe[5,8,19,20].
In addition, since the affected limb may present pseudoparalysis manifestations, like wrist and finger extension disorders after injury, as in the present case, attention should be paid to differentiating the injury from brachial plexus nerve injury. This type of injury can be identified by observing the spontaneous movements of the hand, wrist, and shoulder and through the use of nerve conduction tests[3,21].
Because the epiphyseal ossification centers of the humerus, radius, and ulna in the elbow are not ossified in neonate, the alignment of the capitellum and radius is difficult to be revealed on plain radiograph, making the diagnosis difficult[2,4,16,22]. Ultrasonography can better display the relationship between the epiphysis and metaphysis, blood and fragment within the joint space, as well as any interactions in real-time[3,8,19,22-25]. Thus, the use of ultrasonography has a number of advantages in the neonatal intensive care unit, including its portability and facilitation of continuous monitoring of the later stages of healing. It can therefore be used as the primary means of auxiliary examination. However, ultrasonography also has its disadvantages, as the technique may induce pain in neonates, and there is a higher requirement for the surgeons' skills, as it is not always a simple procedure.
Moreover, MRI can accurately reveal the condition of bone, cartilage, and soft tissue in the joint, with the advantages of obtaining images in all planes. Furthermore, there is no need for specific positioning of the neonate and no radiation risk; however, sedation is required during the examination, which can limit the wider application of MRI[2,4,8,10,16]. Arthrography can better display and facilitate intraoperative observation of fracture displacement and reduction with the C-arm imaging[12,26]. It is economical but invasive.
Some researchers have proposed that callus formation at the ends of a physeal fracture of the distal humerus in the neonate begins to form on the fifth day after the injury. Reduction is not recommended when the fracture is older than 5 d[5,21,27].
In the present case, the patient underwent ultrasonography and MRI on the third day after the injury. Four days after the injury, clinical examination showed that the elbow joint was still swollen, and tenderness and crepitus were still evident at the fracture site. However, ultrasonograms revealed no callus formation, as treatment was not delayed in this case.
The effects of reduction were satisfactory, indicating that our treatment was timely. Callus formation was not observed at any point in time. Callus formation is mainly thought to be due to unstable fracture without fixation or restriction of activity from the time of diagnosis to treatment.
Various methods for treatment of physeal fractures of the distal humerus in the neonate have been reported, including closed reduction under anesthesia, plaster or splint fixation, open reduction, and Kirschner wire fixation. In most cases, both functions and appearance were favorably restored during follow-up[10,11,16,22,28]. However, Ratti et al[3], in a retrospective study of 33 cases, showed that some patients who underwent conservative treatment had malunion and cubitus varus deformity in the later stage.
If fixation is inadequate after closed reduction, subsequent deformities may also occur. Jacobsen et al[11] reported that a neonate who underwent closed reduction and plaster fixation had a mild cubitus valgus deformity during follow-up, even though this did not affect the appearance or function of the limb. A few researchers have demonstrated that even if the neonatal physeal fracture of the distal humerus is not treated, follow-up results in most cases are optimistic; however, there have been no long-term follow-up reports to support this conclusion[3,10]. This case was treated by rapid closed reduction and percutaneous pin fixation without consideration of the risk of fixation with extreme flexion, or the risk of displacement after reduction. Nevertheless, concerns about waiting for deformity remodeling were allayed and the potential for any medical disputes was reduced. Meanwhile, the care and feeding of the patient also became easier.
The patient in the present case was first treated by manual reduction after a definitive diagnosis at the local hospital. This procedure was not successful. Therefore, we considered the extent of displacement to be serious. The proximal end of the fracture passed through the brachial muscle into the anterior subcutaneous tissue of the elbow in a “buttonhole” shape. Thus, soft tissue was embedded between the fracture ends. Therefore, we considered the fracture of this neonate as an “irreversible” physeal fracture of the distal humerus.
Some authors believe that closed reduction is impossible, and consider open reduction to be the preferred treatment[16,29,30]. However, other authors believe that closed reduction and Kirschner wire fixation should be attempted in the treatment of “irreversible” physeal fractures of the distal humerus, because the dissection of soft tissue, and exposure and reduction of the fracture ends during open reduction may lead to intra-articular injury, thereby aggravating the elbow injury[29,31].
Extension traction is not suitable for the reduction of completely displaced “irreversible” physeal fractures of the distal humerus in the neonate. This is because extension traction cannot achieve reduction, as it may keep the anterior structures of the elbow, such as biceps tendon and brachialis muscle tense, thereby locking more tightly the proximal fracture end that is likely to be anteriorly displaced. This could severely compress the soft tissue under the proximal fracture end.
Compared with older children, the neonatal arm is too short for the exertion of manipulative reduction and fracture fixation. Previous reports have not mentioned the specific methods of manual reduction and fixation. In this case, the surgeon stood between the affected limb and head of the patient, held the limb, and exerted traction reduction using only the fingers. Satisfactory reduction and fixation of the broken end of the fracture were achieved. The upper limb of the patient could have been lifted the day after the operation, and the fingers could have been moved freely. Thus, we believe that the traction on the nerves and blood vessels was alleviated after reduction.
The techniques of manual reduction and percutaneous pin fixation to treat physeal fractures of the distal humerus in a 4-day-old neonate, combined with arthrography, were safe and reliable. Ultrasonography, MRI, and arthrography can reveal the intra-articular area favorably, which is helpful in the diagnosis. Surgery can be performed satisfactorily under ultrasonography or arthrography. On the fourth day after birth, no callus formation was evident at the fracture end, on physical examination or imaging findings. Callus formation at the fracture end of the newborn is related to the stability of the fracture ends and the fracture site. As anesthesia and reduction technology permit, manual reduction and percutaneous Kirschner wire fixation with arthrography are recommended for the treatment of physeal fractures of the distal humerus in the neonate. This approach can achieve early symptomatic relief, reduce the waiting time for malunion by remodeling, stabilize the fracture ends, and minimize the complications associated with the operation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Salvadori M S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Kaya B, Daglar K, Kirbas A, Tüten A. Humerus Diaphysis Fracture in a Newborn during Vaginal Breech Delivery. Case Rep Obstet Gynecol. 2015;2015:489108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Sabat D, Maini L, Gautam VK. Neonatal separation of distal humeral epiphysis during Caesarean section: a case report. J Orthop Surg (Hong Kong). 2011;19:376-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Ratti C, Guindani N, Riva G, Callegari L, Grassi FA, Murena L. Transphyseal elbow fracture in newborn: review of literature. Musculoskelet Surg. 2015;99 Suppl 1:S99-S105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Türkmen F, Acar MA, Sever C, Erkoçak ÖF, Göncü G, Toker S. Distal Humeral Epiphyseal Separation in Newborn: A Case Report and Review of The Literature. Eur J Pharm Sci. 2014;3:74-76. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Malik S, Khopkar SR, Korday CS, Jadhav SS, Bhaskar AR. Transphyseal Injury of Distal Humerus: A Commonly Missed Diagnosis in Neonates. J Clin Diagn Res. 2015;9:SD01-SD02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Hamilçıkan Ş, Yılmaz K, Can E. Humeral Diaphysis Fracture in a Neonate After Vaginal Delivery. Sisli Etfal Hastan Tip Bul. 2018;52:51-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Eide P, Djuve Å, Myklebust R, Forseth KF, Nøttveit A, Brudvik C, Rosendahl K. Prevalence of metaphyseal injury and its mimickers in otherwise healthy children under two years of age. Pediatr Radiol. 2019;49:1051-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Navallas M, Díaz-Ledo F, Ares J, Sánchez-Buenavida A, López-Vilchez MA, Solano A, García García J, Maiques JM, Mur-Sierra A, Alier A. Distal humeral epiphysiolysis in the newborn: utility of sonography and differential diagnosis. Clin Imaging. 2013;37:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Downs DM, Wirth CR. Fracture of the distal humeral chondroepiphysis in the neonate. A case report. Clin Orthop Relat Res. 1982;155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Gigante C, Kini SG, Origo C, Volpin A. Transphyseal separation of the distal humerus in newborns. Chin J Traumatol. 2017;20:183-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Jacobsen S, Hansson G, Nathorst-Westfelt J. Traumatic separation of the distal epiphysis of the humerus sustained at birth. J Bone Joint Surg Br. 2009;91:797-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Chou ACC, Wong HYK, Kumar S, Mahadev A. Using the Medial and Lateral Humeral Lines as an Adjunct to Intraoperative Elbow Arthrography to Guide Intraoperative Reduction and Fixation of Distal Humerus Physeal Separations Reduces the Incidence of Postoperative Cubitus Varus. J Pediatr Orthop. 2018;38:e262-e266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Guven MF, Kaynak G, Inan M, Caliskan G, Unlu HB, Kesmezacar H. Results of displaced supracondylar humerus fractures treated with open reduction and internal fixation after a mean 22.4 years of follow-up. J Shoulder Elbow Surg. 2015;24:640-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Bukvić N, Kvesić A, Brekalo Z, Bosak A, Bukvić F, Karlo R. The problem of post-traumatic varization of the distal end of the humerus remaining after the recovery of a supracondylar fracture. J Pediatr Orthop B. 2013;22:372-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Persiani P, Di Domenica M, Gurzi M, Martini L, Lanzone R, Villani C. Adequacy of treatment, bone remodeling, and clinical outcome in pediatric supracondylar humeral fractures. J Pediatr Orthop B. 2012;21:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Söyüncü Y, Cevikol C, Söyüncü S, Yildirim A, Akyildiz F. Detection and treatment of traumatic separation of the distal humeral epiphysis in a neonate: a case report. Ulus Travma Acil Cerrahi Derg. 2009;15:99-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Menon TJ. Fracture separation of the lower humeral epiphysis due to birth injury: a case report. Injury. 1982;14:168-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Paige ML, Port RB. Separation of the distal humeral epiphysis in the neonate. A combined clinical and roentgenographic diagnosis. Am J Dis Child. 1985;139:1203-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Patil MN, Palled E. Epihyseal Separation of Lower end Humerus in A Neonate-Diagnostic and Management Difficulty. J Orthop Case Rep. 2015;5:7-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Barrett WP, Almquist EA, Staheli LT. Fracture separation of the distal humeral physis in the newborn. J Pediatr Orthop. 1984;4:617-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Kaushal R, Gupta PN, Gupta R, Bahadur R. Distal humeral epiphyseal separation associated with radial nerve palsy in a neonate as a result of birth trauma. Injury Extra. 2005;36:12-14. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Sherr-Lurie N, Bialik GM, Ganel A, Schindler A, Givon U. Fractures of the humerus in the neonatal period. Isr Med Assoc J. 2011;13:363-365. [PubMed] |
| 23. | Dias JJ, Lamont AC, Jones JM. Ultrasonic diagnosis of neonatal separation of the distal humeral epiphysis. J Bone Joint Surg Br. 1988;70:825-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Varghese J, Teng M, Huang M, Balsam D. Birth injuries to growth plates: A sheep in wolves' clothing. J Clin Ultrasound. 2017;45:511-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Baessler AM, Wessel RP, Caltoum CB, Wanner MR. Ultrasound diagnosis of medial clavicular epiphysis avulsion fracture in a neonate. Pediatr Radiol. 2020;50:587-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Hariharan AR, Ho C, Bauer A, Mehlman CT, Sponseller PD, O'Hara N, Elliott M, Abzug JM. Transphyseal Humeral Separations: What Can We Learn? A Retrospective, Multicenter Review of Surgically Treated Patients Over a 25-Year Period. J Pediatr Orthop. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Mane PP, Challawar NS, Shah H. Late presented case of distal humerus epiphyseal separation in a newborn. BMJ Case Rep. 2016;2016:bcr2016215296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Princic J, Tonin M, Ales A. [Birth trauma as the cause of fracture of the distal epiphysis of the humerus. A case report]. Unfallchirurg. 1995;98:487-488. [PubMed] |
| 29. | Elstrom JA, Pankovich AM, Kassab MT. Irreducible supracondylar fracture of the humerus in children. A report of two cases. J Bone Joint Surg Am. 1975;57:680-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 30. | Millis MB, Singer IJ, Hall JE. Supracondylar fracture of the humerus in children. Further experience with a study in orthopaedic decision-making. Clin Orthop Relat Res. 1984;90-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Li X, Shi Q, Wu W, Ou L, Yan H, Jin D. [Closed reduction and percutaneous pinning in treatment of "irreducible" supracondylar humerus fractures in children]. Zhonghua Wai Ke Za Zhi. 2015;53:763-766. [PubMed] |