Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4443
Peer-review started: May 16, 2020
First decision: June 7, 2020
Revised: June 8, 2020
Accepted: September 10, 2020
Article in press: September 10, 2020
Published online: October 6, 2020
Processing time: 134 Days and 18.4 Hours
An aneurysm of the left atrial appendage is one of the rare but potentially hazardous heart defects. The risk of lethal complications grows with its size. To date, about 150 cases of this defect have been described in the literature. We present a case of left atrial appendage aneurysm with the deformation of the mitral valve and the left main coronary and circumflex artery, which required mitral valve annuloplasty and bifurcation stenting.
A 58-year-old man presented to our hospital complaining of shortness of breath, general weakness, dizziness during physical exertion, and fatigue. Based on the results of echocardiography, an aneurysm of the left atrium was suspected. A free-breathing real-time cine magnetic resonance imaging with electrocardiograph synchronization confirmed the diagnosis of left atrial appendage aneurysm. The patient underwent an aneurysmectomy via a median sternotomy with cardiopulmonary bypass. Intraoperative transesophageal echocardiography revealed relative mitral insufficiency that was corrected with an annuloplasty ring. Intraoperative coronary angiogram showed impaired blood flow in the left main coronary and circumflex artery and 60% stenosis. For this reason, bifurcation stenting was performed. The patient had an uneventful postoperative clinical course and was discharged from the hospital on the 10th day in a satisfactory condition.
Left atrial appendage aneurysm is a rare and dangerous heart pathology that requires surgery to prevent related complications.
Core Tip: Left atrial appendage aneurysm is one of the rare, but potentially hazardous heart defects. We present a case of left atrial appendage aneurysm resection and mitral valve annuloplasty. This case highlights the fact that the disease is diagnosed either by chance or when examining the patient as a result of complications. Echocardiography in most cases will make it possible to establish the diagnosis, but magnetic resonance imaging is necessary for a more detailed assessment of changes in the heart. Surgical treatment is indicated for all patients to prevent fatal disorders.
- Citation: Belov DV, Moskalev VI, Garbuzenko DV, Arefyev NO. Left atrial appendage aneurysm: A case report. World J Clin Cases 2020; 8(19): 4443-4449
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4443.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4443
Left atrial appendage aneurysm is one of the rare but potentially hazardous heart defects. The bigger it grows, the higher is the risk of lethal complications[1]. The paper presents a case of left atrial appendage aneurysm that required a left atrial appendage resection and mitral valve annuloplasty.
The PubMed database, the Google Scholar retrieval system, and the reference lists from related articles were used to search for relevant publications. Articles corresponding to the aim of the review were selected for 1962 to 2019 using the keywords: “left atrial appendage aneurysm”, “left atrial appendage dilatation”, “pathogenesis”, “diagnosis”, “treatment”. The management of patients with left atrial appendage aneurysm was the inclusion criterion.
A 58-year old man was hospitalized to the Federal Center for Cardiovascular Surgery of the Russian Ministry of Health (Chelyabinsk) complaining of dyspnea, general weakness, dizziness during physical exertion, and fatigue.
Over the past five years, the patient experienced rare heart palpitations that have occurred and stopped on their own after a few minutes. Six months before hospitalization, shortness of breath, weakness, and post-exertion dizziness appeared. Heart rate increased to 120 per minute. The electrocardiogram taken in an outpatient clinic revealed an irregular form of atypical atrial flutter. Based on the results of echocardiography, an aneurysm of the left atrium was suspected. Warfarin was prescribed. The maintenance dose was 2.5 mg daily.
The patient had a free previous medical history.
On the patient’s visit to the Center for Cardiovascular Surgery, his vital signs were within normal limits.
The Quick prothrombin activity was 27.9% (reference values were 70%-120%), INR was 2.52, and the prothrombin time was 45.6 s due to warfarin treatment. Other laboratory parameters of blood and urine analyses, blood biochemistry, and arterial blood gas were within normal limits.
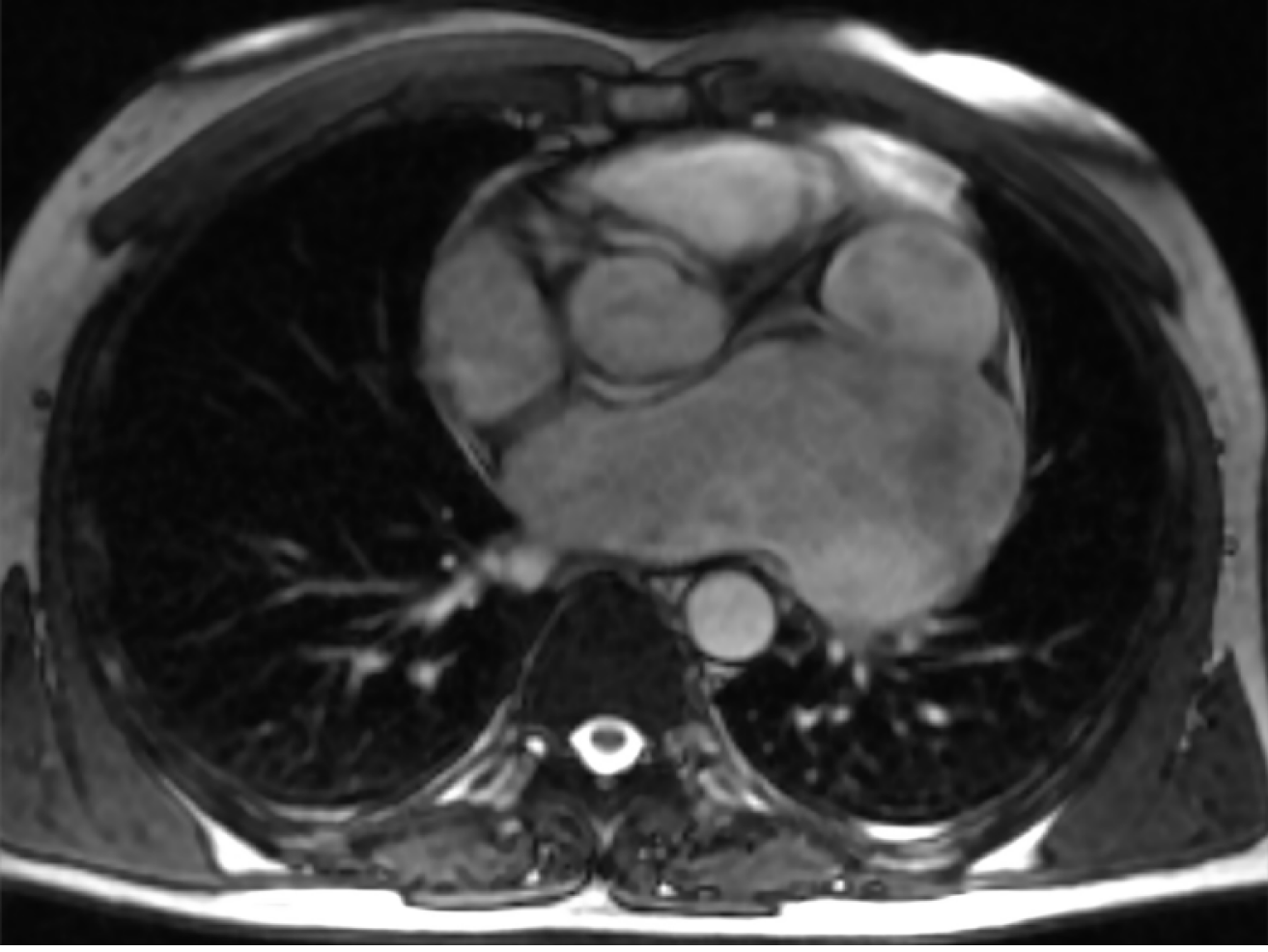
A free-breathing real-time cine magnetic resonance imaging (MRI) with electrocardiograph synchronization did not reveal any defects in the leaves of the pericardium and extrapericardial protrusions of the heart cavities. A giant aneurysm of the left atrial appendage (123 mm × 90 mm × 70 mm in size) had uneven and clear contours, thin walls, and turbulent blood flow in the cavity. The aneurysm had a wide communication with the cavity of the left atrium. The neck of the aneurysm was 51 mm × 55 mm in size. The cavity of the aneurysm had no pathological formations, there were no blood clots. The aneurysmically dilated left atrial appendage was adjacent to the trunk and left branch of the pulmonary artery, to the upper and lower left pulmonary veins, and to the left atrioventricular sulcus. The lower contour of the aneurysm reached the diaphragmatic surface of the pericardium. The left atrium was of normal size (Figure 1). Preoperative coronary angiography showed the absence of coronary artery stenosis.
The final diagnosis of the presented case is left atrial appendage aneurysm.
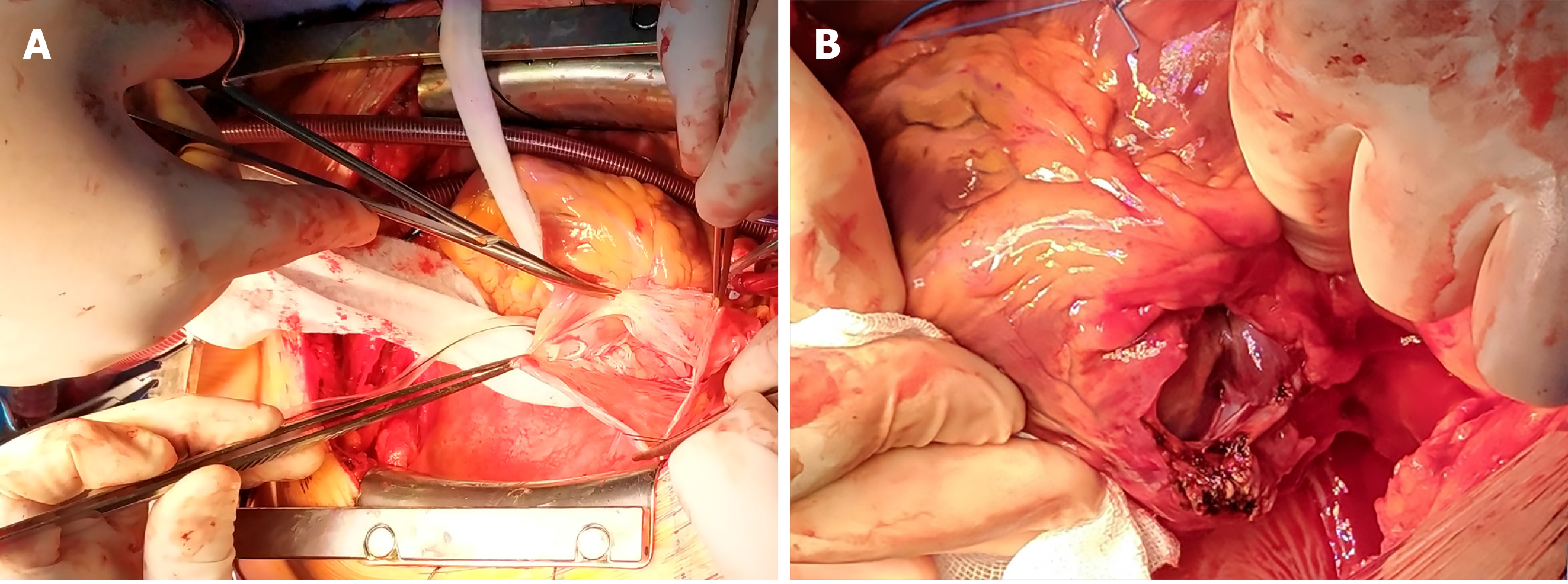
The operative approach was via a median sternotomy with cardiopulmonary bypass. Along the lateral wall of the left atrium, in the projection of the left atrial appendage, there was a pulsating, spherical, and irregularly shaped aneurysm of 10 cm × 8 cm in size. It was not adjacent to the pericardium and involved the posterior wall, reaching the left pulmonary veins ostia.
The intraoperative transesophageal echocardiography showed that the aneurysmal cavity was divided by a short septum and had free communication with the left atrial cavity. Relative mitral insufficiency requiring correction was also revealed.
The mitral valve was accessed through the right contour of the left atrium. The aneurysm of the left atrium was opened from the outside, and its base was resected. The wall of the aneurysm was thin, flabby, and without any blood clots.
In the area of the circumflex artery, the left ventricle was significantly deformed and had an indentation of 3.0 cm × 2.0 cm in size. The lower edge of the resected aneurysm was located near the fibrous annulus of the mitral valve, in the area of anterolateral commissure (A1 and P1 segments). The flaps of the mitral valve and chords were not damaged. Mitral valve annuloplasty was performed by using a PROFILE 3D® 680R annuloplasty ring (Medtronic, United States). Considering that the defect, which formed after excision of the aneurysm, was close to the fibrous annulus and the circumflex artery, we decided to suture it from the inside. In the area of the fibrous annulus, the suture was fixed to the outer layer of the annuloplasty ring (Figure 2). Intraoperative transesophageal echocardiography showed grade 0–1 mitral regurgitation and insignificant mitral regurgitant volume.
Considering the anatomical location of the aneurysm and the absence of visualization of the circumflex artery, we performed coronary angiography. Signs of impaired blood flow in the left main coronary and circumflex artery and 60% stenosis were found. Bifurcation stenting was performed.
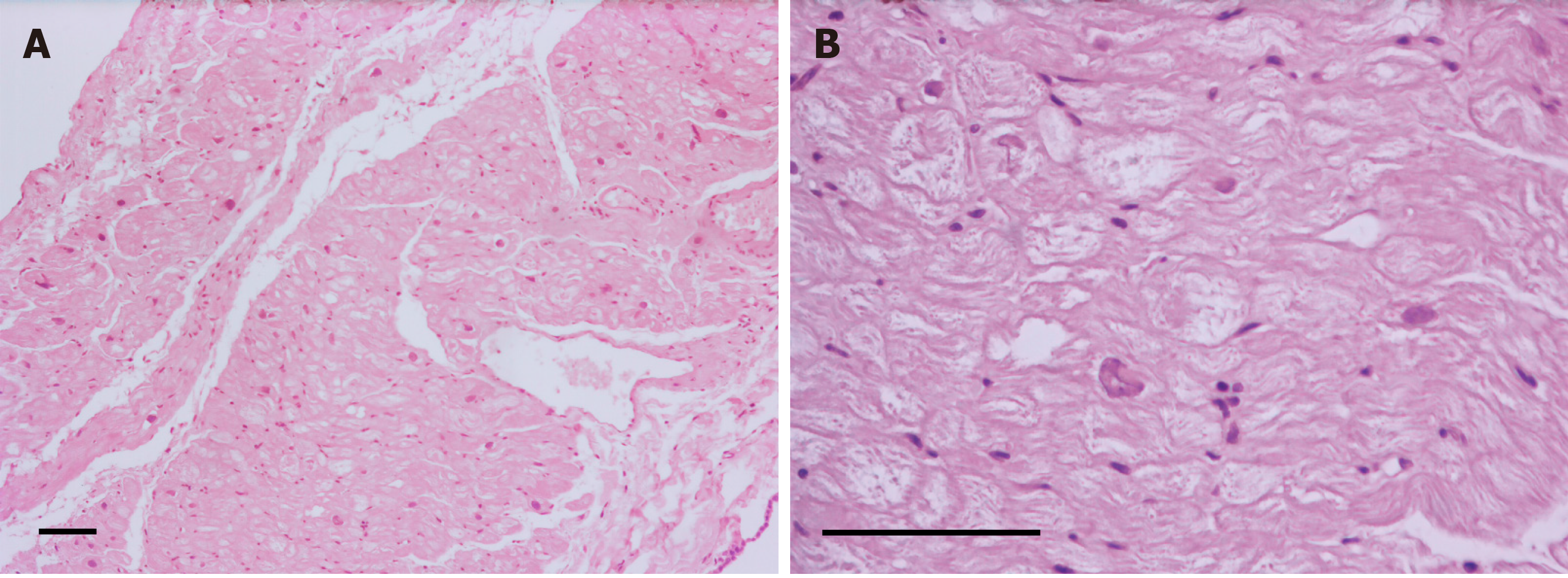
A histological examination of the resected left atrial appendage revealed a 1 mm thin wall of the left atrium with hypertrophied cardiomyocytes with dystrophic changes and vacuolated cytoplasm, and slight fibrosis of the endo- and epicardium (Figure 3).
The patient had an uneventful postoperative clinical course and was discharged from the hospital on the 10th d in a satisfactory condition. Sinus rhythm restored in the early postoperative period. Atrial flutter reappeared 2 mo after discharge from the hospital and required surgical intervention; so, radiofrequency catheter ablation of the cavotricuspid isthmus was performed. Transthoracic echocardiography performed 3 mo after discharge showed a left ventricular systolic pressure of 29 mmHg and an ejection fraction of 60%, grade 0-1 mitral regurgitation, and insignificant mitral regurgitant volume. The left atrium was 43 mm × 53 mm in size.
In 1938, Semans and Taussig reported an isolated expansion of the cavity of the left atrium in a 5-year-old girl[2]. In 1962, Parmley described aneurysmal dilatation of the left atrium appendage in two children[3]. The first child of 11 years old had supraventricular cardiac arrhythmia and two episodes of systemic embolism and underwent resection of the left atrial appendage and removal of the atrial septal defect at the Mayo Clinic. The second, 7-year-old patient had an aneurysm of the left atrial appendage and a concomitant congenital anomaly of the left renal artery and left kidney causing arterial hypertension. In 1963, Williams published a report on an increase in the thin-walled appendage of the left atrium in a 27-year-old man[4]. An attempt to clamp the appendage during surgery was accompanied by cardiac arrhythmia; therefore, appendage resection had to be abandoned. However, due to embolic complications that occurred two years later, the removal of the left atrial appendage with blood clots was performed. To date, about 150 cases of this defect have been described in the literature[5,6].
The defect has a congenital and acquired form. In the congenital form, the formation of the aneurysm occurs due to dysplasia of the scallop muscles and associated atrial muscle fibers[5]. Poor contractile function leads to a gradual expansion and extension of the left atrial appendage as a result of increased internal pressure[7].
Foale et al[8] proposed the following diagnostic criteria for the congenital form: (1) Origin from an otherwise normal atrial chamber; (2) Well-defined communication with the atrial cavity; (3) Location within the pericardium; and (4) Distortion of the left ventricle by an aneurysm.
At the same time, Williams divided congenital aneurysms of the left atrium into extra- and intrapericardial types[4]. In the extrapericardial type, the left atrium or appendage is prolated through the pericardial defect and compressed in it, which leads to the aneurysmal expansion of the extrapericardial part. The intrapericardial type is due to the underdeveloped wall of the left atrium or its appendage[9].
The process of development of acquired aneurysms is the result of damage to the mitral valve or other conditions leading to an increase in pressure in the left atrium[10]. At the same time, it is often difficult to differentiate the acquired and congenital forms, as in our case, since moderate changes of the mitral valve can be caused by the presence of the appendage aneurysm itself[11].
Clinical signs of the disease occur in the third decade of life[1]. The most common manifestations are heart palpitations (43%), shortness of breath (22%), heart rhythm disturbances (15%), embolic disorders of cerebral circulation (11%), and chest pain and discomfort (7%)[12].
Heart rhythm disturbances occur as a result of structural remodeling of the left atrial appendage, leading to electrical dissociation of cardiomyocytes and local disturbances in conduction that favor the emergence and maintenance of arrhythmia[13]. Left atrial appendage dilatation, atrial fibrillation, blood stasis, and thrombosis of the aneurysmal cavity are responsible for subsequent thromboembolic complications[5].
Despite the large size of the aneurysm, our patient did not have any of the following symptoms associated with compression of surrounding structures: (1) Compression of the left ventricle by the aneurysm may cause an increase in filling pressure and diastolic dysfunction, leading to the appearance of shortness of breath and heart failure[13,14]; (2) Compression of the left anterior descending artery may manifest as angina pectoris[15]; (3) A characteristic sign of irritation of the left phrenic nerve is hiccups[6]; and (4) The aneurysm proximity to the respiratory tract may cause a dry, unproductive cough[16].
Cases of left atrial appendage aneurysm rupture with a lethal outcome have been described[9].
In most cases, the disease is detected by chance because of a non-specific clinical picture. A convexity at the contour of the left atrium determined on a chest X-ray requires differential diagnosis with a pericardial cyst and heart and mediastinal tumors[10,11].
Echocardiography is considered the main method for diagnosing left atrial appendage aneurysm and the presence of blood clots in it[1]. While, due to the limited echo window, the transthoracic examination does not always make it possible to accurately establish the diagnosis, the transesophageal approach may provide a more detailed and clear visualization[10].
Computed tomography and MRI are useful in unclear cases. MRI has a high resolution, which makes it optimal in assessing the surrounding structures and cardiac abnormalities. However, MRI has certain disadvantages, such as the need for regular heart rhythm and patient’s exposure to nephrotoxic contrast agents. Cardiac computed tomography makes it possible to evaluate the anatomy of the coronary arteries, if there is a suspicion of their compression, but cannot provide functional data as accurately as echocardiography or MRI[10].
Surgical treatment is indicated for all patients to prevent the occurrence of atrial fibrillation, systemic embolism, or myocardial dysfunction[17,18]. We performed a left atrial appendage aneurysm resection via median sternotomy with cardiopulmonary bypass, which is considered the operation of choice, especially in patients with thrombosis of the aneurysmal cavity and the need for concomitant interventions[19].
Aneurysmectomy through left-sided lateral thoracotomy should be considered if isolated lesions of the left atrial appendage are present without significant violations of the heart anatomy[20]. Endoscopic surgery is most suitable for patients with minor aneurysms in the absence of thrombosis[21].
The issue of performing a concomitant intervention to restore sinus rhythm remains debatable. Following the most recent 2017 guidelines from the Society of Thoracic Surgeons, surgical ablation for atrial fibrillation is recommended at the time of concomitant mitral operations to restore sinus rhythm (Class I, Level A)[22]. However, removal of the aneurysm usually results in resolution of atrial arrhythmias with no need for additional surgery[23,24]. Moreover, сoncomitant atrial fibrillation surgery increases the risk for requiring a permanent pacemaker[25]. We decided to abandon concomitant surgery for atrial fibrillation to limit the overall risks of the operation. Also, there was a possibility that atrial flutter might disappear after resection of the aneurysm. Unfortunately, arrhythmia disappeared only temporarily and required radiofrequency catheter ablation 2 mo after discharge from the hospital.
This is a case report and the conclusions are subject to the inherent bias associated with the retrospective design. Also, this study design does not allow us to establish a cause-effect relationship between atrial appendage aneurysm and mitral regurgitation, as well as to differentiate between congenital and acquired forms of the aneurysm.
Left atrial appendage aneurysm is a rare heart defect. Given the nonspecific clinical picture, the disease is diagnosed either by chance or during the examination of a patient when complications arise. Echocardiography helps to establish the diagnosis in most of the cases. However, MRI is necessary for a more detailed assessment of changes in the heart. Surgical treatment is indicated for all patients to prevent fatal disorders. In the case when the circumflex artery is not visualized, coronary angiography may help to avoid adverse events. Antiarrhythmic surgery can decrease the risk of thromboembolic complications and may be performed either at the time of concomitant left atrial appendage resection or as a stand-alone surgical procedure, depending on the clinical situation.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ho CM S-Editor: Zhang L L-Editor: A P-Editor: Xing YX
| 1. | Chen Y, Mou Y, Jiang LJ, Hu SJ. Congenital giant left atrial appendage aneurysm: a case report. J Cardiothorac Surg. 2017;12:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Semans JH, Taussig HB. Congenital "aneurysmal" dilatation of the left auricle. Bull Johns-Hopkins Hosp. 1938;63:404. |
| 3. | Parmley LF. Congenital atriomegaly. Circulation. 1962;25:553-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Williams WG. Dilatation of the Left Atrial Appendage. Br Heart J. 1963;25:637-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Aryal MR, Hakim FA, Ghimire S, Ghimire S, Giri S, Pandit A, Bhandari Y, Bhandari N, Pathak R, Karmacharya P, Pradhan R. Left atrial appendage aneurysm: a systematic review of 82 cases. Echocardiography. 2014;31:1312-1318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Asfalou I, Boumaaz M, Raissouni M, Sabry M, Benyass A, Zbir EM. Huge left atrial appendage aneurysm revealed by chronic hiccups. J Saudi Heart Assoc. 2017;29:293-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Wang HQ, Zhang Z, Yang H, Wu S, Fu YH, Song ZM, Wan F. A Huge Congenital Left Atrial Appendage Aneurysm. Chin Med J (Engl). 2017;130:3011-3012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Foale RA, Gibson TC, Guyer DE, Gillam L, King ME, Weyman AE. Congenital aneurysms of the left atrium: recognition by cross-sectional echocardiography. Circulation. 1982;66:1065-1069. |
| 9. | Chowdhury UK, Seth S, Govindappa R, Jagia P, Malhotra P. Congenital left atrial appendage aneurysm: a case report and brief review of literature. Heart Lung Circ. 2009;18:412-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Wang B, Li H, Zhang L, He L, Zhang J, Liu C, Wang J, Lv Q, Shang X, Liu J, Xie M. Congenital left atrial appendage aneurysm: A rare case report and literature review. Medicine (Baltimore). 2018;97:e9344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Valentino MA, Al Danaf J, Morris R, Tecce MA. Giant left atrial appendage aneurysm: A case of mistaken identity. J Cardiol Cases. 2017;15:129-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Bamous M, Aithoussa M, Abetti A, Boulahya A. Congenital left atrial appendage aneurysm: Atypical presentation. Ann Pediatr Cardiol. 2017;10:293-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Li M, Wang Y, Liu S, Yang J, Ma C. Giant left atrial appendage aneurysm compressing the left ventricular wall diagnosed by multiple imaging technology. Cardiol J. 2019;26:416-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Harland DR, Suma V, Muthukumar L, Port SC, Werner PH, Tajik AJ. Giant Congenital Left Atrial Appendage Aneurysm Presenting With Recurrent Supraventricular Tachycardia and Chest Pain. CASE (Phila). 2019;3:129-132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Wagdy K, Samaan A, Romeih S, Simry W, Afifi A, Hassan M. Giant left atrial appendage aneurysm compressing the left anterior descending coronary artery. Echocardiography. 2016;33:1790-1792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Toufan M, Pourafkari L, Afrasiabi A, Sohrabi M, Nader ND. Left atrial appendage aneurysm presenting with chronic cough. Neth Heart J. 2017;25:526-527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Teng P, Ni Y, Sun Q, Zhao H. Giant Left Atrial Appendage Aneurysm: Surgical Treatment to Prevent Potential Complications. Heart Surg Forum. 2018;21:E464-E465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Lukin OP, Belov DV, Milievskaya EB. [Organization of the cardiosurgical medical care in the Ural Federal District]. Grudnaya i serd-sosud hir. 2018;60:281-286. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Victor S, Nayak VM. Aneurysm of the left atrial appendage. Tex Heart Inst J. 2001;28:111-118. [PubMed] |
| 20. | Clark JB, Ting JG, Polinsky RJ, Wolfe LT. Resection of a Giant Left Atrial Appendage Aneurysm via Limited Thoracotomy. World J Pediatr Congenit Heart Surg. 2014;5:475-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Ruttkay T, Scheid M, Götte J, Doll N. Endoscopic Resection of a Giant Left Atrial Appendage. Innovations (Phila). 2015;10:282-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Badhwar V, Rankin JS, Damiano RJ, Gillinov AM, Bakaeen FG, Edgerton JR, Philpott JM, McCarthy PM, Bolling SF, Roberts HG, Thourani VH, Suri RM, Shemin RJ, Firestone S, Ad N. The Society of Thoracic Surgeons 2017 Clinical Practice Guidelines for the Surgical Treatment of Atrial Fibrillation. Ann Thorac Surg. 2017;103:329-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 362] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 23. | Burke RP, Mark JB, Collins JJ, Cohn LH. Improved surgical approach to left atrial appendage aneurysm. J Card Surg. 1992;7:104-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Vagefi PA, Choudhry M, Hilgenberg AD. Excision of an aneurysm of the left atrial appendage. J Thorac Cardiovasc Surg. 2007;133:822-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Huffman MD, Karmali KN, Berendsen MA, Andrei AC, Kruse J, McCarthy PM, Malaisrie SC. Concomitant atrial fibrillation surgery for people undergoing cardiac surgery. Cochrane Database Syst Rev. 2016;CD011814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |