Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4388
Peer-review started: May 10, 2020
First decision: June 7, 2020
Revised: June 20, 2020
Accepted: August 22, 2020
Article in press: August 22, 2020
Published online: October 6, 2020
Processing time: 140 Days and 13.5 Hours
Lisfranc injuries have not received much attention by orthopedic doctors in the past, and there is little related research on the diagnosis and treatment of these injuries. In recent years with the rise in foot and ankle surgery, doctors are now paying more attention to this type of injury. However, there is still a high rate of missed diagnosis due to insufficient attention causing treatment delays or inadequate treatments, which eventually result in greater sequelae; including long-term pain, arthritis, foot deformity etc. In particular, for cases with a mild Lisfranc joint complex injury, the incidence of sequelae is higher.
To select an active surgical treatment for an atypical Lisfranc joint complex injury and to evaluate the clinical efficacy of the surgical treatment.
The clinical data of 18 patients, including 10 males and 8 females aged 20-64 years with Lisfranc injuries treated in our department from January 2017 to September 2019 were retrospectively analyzed. All patients were treated with an open reduction and internal fixation method using locking titanium mini-plates and hollow screws or Kirschner wires. X-ray images were taken and follow-up was performed monthly after the operation; the internal fixation was then removed 4-5 mo after the operation; and the American Orthopedic Foot and Ankle Society (AOFAS) score was used for evaluation on the last follow-up.
All patients were followed up for 6-12 mo. A good/excellent AOFAS score was observed in 88.9% of patients.
For atypical Lisfranc joint complex injuries, active open reduction and internal fixation can be performed to enable patients to obtain a good prognosis and satisfactory functional recovery.
Core Tip: This retrospective study evaluated the efficacy of open reduction and internal fixation for atypical Lisfranc joint complex injuries. The new concept of "atypical Lisfranc joint complex injury" was introduced and defined. A novel classification system was also introduced and its practicability determined. Based on this study, it was concluded that open reduction and internal fixation are effective for the treatment of "atypical Lisfranc joint complex injury" and the new classification system had good clinical practicability.
- Citation: Li X, Jia LS, Li A, Xie X, Cui J, Li GL. Clinical study on the surgical treatment of atypical Lisfranc joint complex injury. World J Clin Cases 2020; 8(19): 4388-4399
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4388.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4388
The incidence of Lisfranc injury is relatively low. According to related reports, the incidence rate in the United States is 1/60000, accounting for only 0.2% of total body fractures[1,2]. There are no specific statistics in China. The diagnosis and treatment of a Lisfranc injury varies greatly in different hospitals, resulting in a high rate of missed diagnosis. According to reports, the rate of missed diagnosis of occult Lisfranc injuries in the United States is as high as 20%-40%[3-5], and this may be higher in China. The diagnosis and classification of typical Lisfranc injuries are well known, and the principles of their treatment have resulted in a consensus. While some atypical Lisfranc joint complex injuries do not have typical features such as metatarsal ray displacement and widening of the Lisfranc joint space, their clinical symptoms and the violence suffered at the time of injury are obvious. The radiological findings show avulsion fractures around the Lisfranc joint complex. Conservative treatment is chosen in many cases; however, conservative treatment may cause positional loss due to an imbalance of the dorsal and metatarsus muscle strength after the swelling disappears; in addition, the treatment result is poor, which manifests as persistent pain or long-term arthritis[6]. A retrospective study of the clinical data of 18 patients with Lisfranc joint complex injuries treated in our hospital from January 2017 to September 2019 is reported below.
The data of patients with Lisfranc joint complex injuries treated in our department from January 2017 to September 2019 were compiled and matched cases were selected according to preset inclusion criteria[7].
Inclusion criteria: (1) Those with acute closed fractures or dislocations of the Lisfranc joint complex in a single foot; (2) Those who showed multiple fractures of the tarsometatarsal joint involving the articular surface and with a tarsometatarsal joint displacement less than 2 mm on computed tomography (CT) scans; (3) Those with other site injuries that did not affect the evaluation of postoperative foot function; (4) Those between the ages of 18 and 65; (5) Those who underwent open reduction and internal fixation within 2 wk after injury; and (6) Those who consented and agreed to follow-up.
Exclusion criteria: (1) Those with distal tibiofibular fractures, ankle fractures, hindfoot fractures or open Lisfranc injuries; (2) Those with fractures and dislocations of the contralateral lower extremities; (3) Those with other injuries or a previous history of other foot diseases that may affect the evaluation of postoperative foot function; (4) Those with internal fixation unremoved; (5) Those who underwent tarsometatarsal joint arthrodesis after injury; (6) Those who did not perform rehabilitation exercises and received regular follow-up as required; (7) Those with more than 2 wk from injury to surgery; (8) Those with severe medical diseases who could not tolerate surgery; and (9) Those who were followed up for less than 6 mo.
A total of 18 patients were included in this retrospective study [10 males and eight females with an average age of 40.06 years (range, 20-64)]. Of these patients, 11 had left foot injury and seven had right foot injury. The mechanisms of injury included traffic accident in five cases, bruised or crush injury in eight cases and sprain in five cases. Epidemiological data are listed in Table 1. Examination after admission showed that all patients had tenderness and pain under stress at the tarsometatarsal joints and some patients had typical plantar ecchymosis. Following the injury, orthophoria-oblique radiography was performed and weight-bearing orthophoria-lateral radiography was performed on the injured foot for those who could tolerate the pain. CT examinations were performed in all patients with confirmed or suspected fractures and dislocations on X-ray images who could not tolerate pain under weight-bearing conditions. If it was not possible to determine the stability of the tarsometatarsal joint, a stress test under anesthesia was performed and compared with the healthy foot to improve the test accuracy. In some cases, there were large fracture fragments in the plantar side of the base of the second and third metatarsal bones or multiple large avulsion fractures of the tarsometatarsal joint complex involving the articular surface; we used an aggressive surgical incision to examine the articular surface[7]. For all patients with tarsometatarsal joint instability, open reduction and internal fixation were performed. The internal fixation methods included hollow screws, locking titanium mini-plates and Kirschner wires[8]. Preoperatively, the affected limb was lifted and iced for 48 h and mannitol was injected intravenously to reduce the swelling. After “wrinkle signs” appeared on the skin, surgery was performed. Swellings disappeared 5-9 d after injury in all patients, with an average of 7 d.
| Variable | Count | AOFAS score (mean ± SD) | P value |
| Age | 0.934 | ||
| < 45 yr | 11 | 88.5 ± 8.7 | |
| > 45 yr | 7 | 88.9 ± 5.5 | |
| Left or right foot | 0.679 | ||
| Left | 11 | 89.3 ± 7.9 | |
| Right | 7 | 87.7 ± 7.2 | |
| Gender | 0.367 | ||
| Male | 10 | 87.2 ± 8.0 | |
| Female | 8 | 90.5 ± 6.8 | |
| Injury type | 0.008 | ||
| Type 1 | 5 | 93.8 ± 3.0 | |
| Type 2A | 1 | 71.0 ± 0.0 | |
| Type 3A | 12 | 88.0 ± 6.5 | |
| Mechanism | 0.130 | ||
| High-energy injury | 13 | 87.0 ± 7.7 | |
| Low-energy injury | 5 | 93.0 ± 4.9 |
Abduction stress test: The operator fixed the patient's injured foot with one hand, applied stress in the abduction direction by holding the forefoot in the other hand and obtained an orthophoria foot X-ray to observe the displacement of the tarsometatarsal joint before and after stress[8,9]. A tangent line was made along the tarsal navicular bone and the medial border of the entocuneiform. If the first metatarsus was displaced to the outside of the tangent line under stress, it was positive and if the first metatarsus intersected with the tangent line, it was negative.
Simulated weight-bearing stress test: The injured foot was compared with the healthy foot. The patient laid on his/her back with the knee flexed on the test side. The operator applied vertical stress downward from the proximal end of the calf and an orthophoria X-ray of foot was obtained to observe the changes in the joint space of Lisfranc. If the gap had increased by more than 2 mm or the width was wider than the healthy side by 1 mm, it was positive.
Excessive flexion-extension stress test: The operator fixed the patient's injured foot with one hand and held the forefoot with the other hand to apply plantar flexion and dorsiflexion stress[10]. If the tarsometatarsal joint surface step was greater than 2 mm or the tarsometatarsal joint space increased by more than 1 mm from the healthy side, it was positive. Those suspected to be positive in the stress test underwent surgery.
The operation adopted the classic dorsal incision[11]; that is, the incision was made between the first and second metatarsal rays on the dorsal side for exploration, reduction and fixation. If instability of the fourth and fifth rays was suspected in the preoperative or intraoperative evaluation, an auxiliary incision on the lateral side of the foot dorsum could be added. When making a medial incision, the dorsalis pedis neurovascular bundle was found and protected according to the position of the extensor hallucis longus tendon. The first ray was exposed on the medial side of the neurovascular bundle and the second and third rays were exposed on the lateral side. The sub-fascial tissue was bluntly dissected to avoid iatrogenic damage to the dorsal ligament and joint capsule by the scalpel. Before reduction of the tarsometatarsal joint, the bone fragments, the embedded broken ends of the joint capsule and the ligament in the articular cavity that might have affected the reduction of the joint were removed. At the time of reduction, the articular surface under the torn joint capsule was exposed, the joint was reduced under direct vision and temporarily fixed with fine Kirschner wires. During the operation, the medial column (first ray) and the middle column (second and third rays) were fixed by hollow screws or dorsal locking titanium mini-plates according to the Myerson's three-column theory[12] after X-ray fluoroscopy showed that the fracture-dislocation was well reduced. Hollow screws were chosen because they are easier to implant and easier to locate using guide pins during removal[13]. The lateral columns (fourth and fifth rays) were elastically fixed with Kirschner wires. The dorsal avulsed fragments were reduced and the torn joint capsule and ligament were repaired as best as possible after reduction and temporary fixation. Before closure of the incision, the stability of the tarsometatarsal joint was evaluated under stress again and compared with that before surgery.
Active and passive activities of the toe and ankle joints were started on the second day after the operation and the range of activities was gradually increased. The patients exercised under non-weight-bearing conditions within 1 wk. Six weeks after surgery, the Kirschner wires were removed and partial weight-bearing exercises were performed under the protection of ankle braces. The weight-bearing exercises were completely performed after 12 wk and a foot arch cushion was used to assist. The internal fixation of the medial and middle columns was removed according to the situation after 4-5 mo[14]. The outpatient reviews were performed monthly after the patient was discharged from the hospital and X-ray images were obtained to observe fracture healing. The American Orthopedic Foot and Ankle Society (AOFAS) score was obtained on the patient's last review after removing all internal fixations.
The patients were reviewed monthly to observe fracture healing and complications after the operation. The ankle-foot function scores of the AOFAS were used to evaluate the foot’s functional recovery[15] with a perfect score of 100, 90-99 being excellent, 80-89 being good, 70-79 being acceptable and 69 and below being poor.
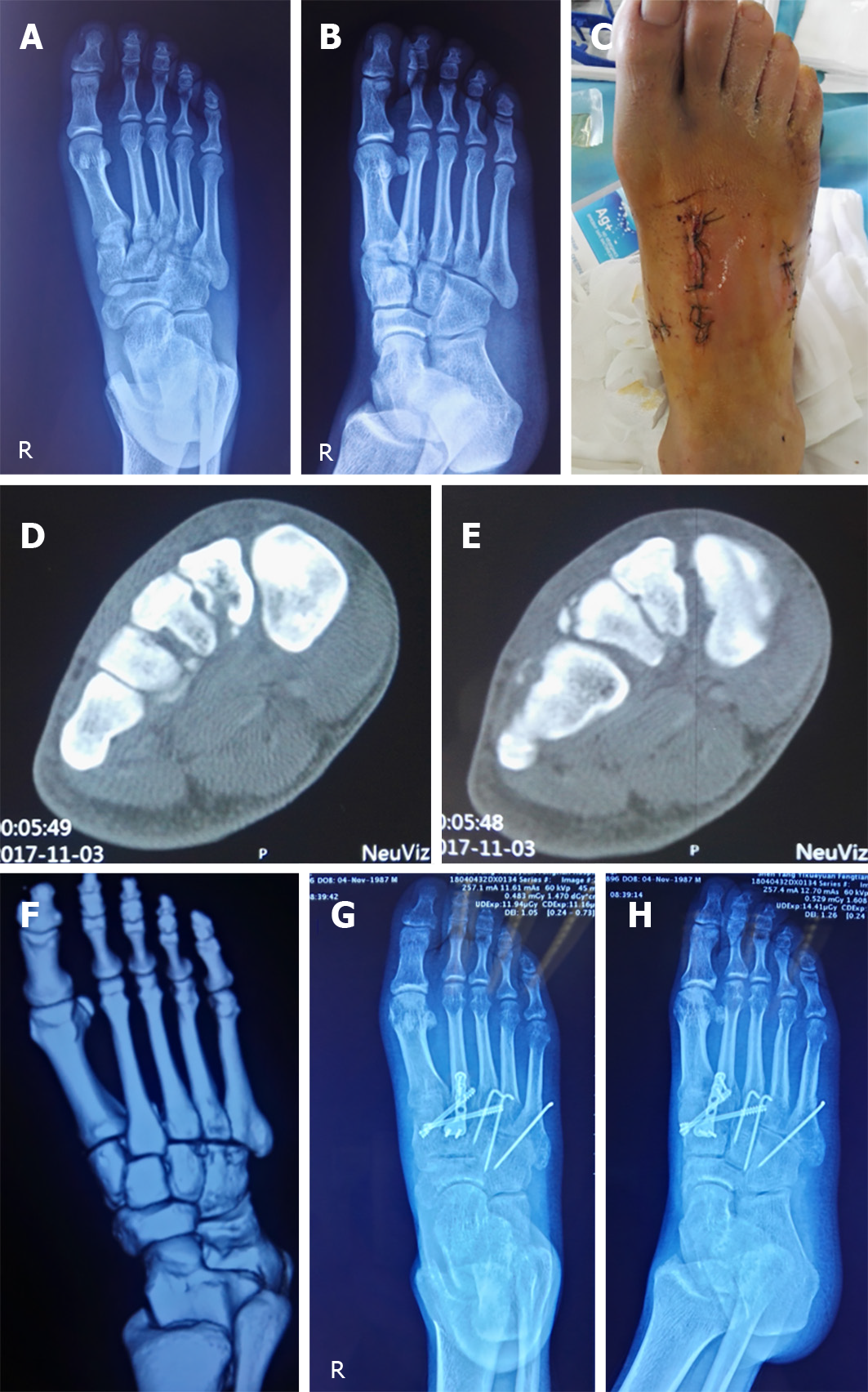
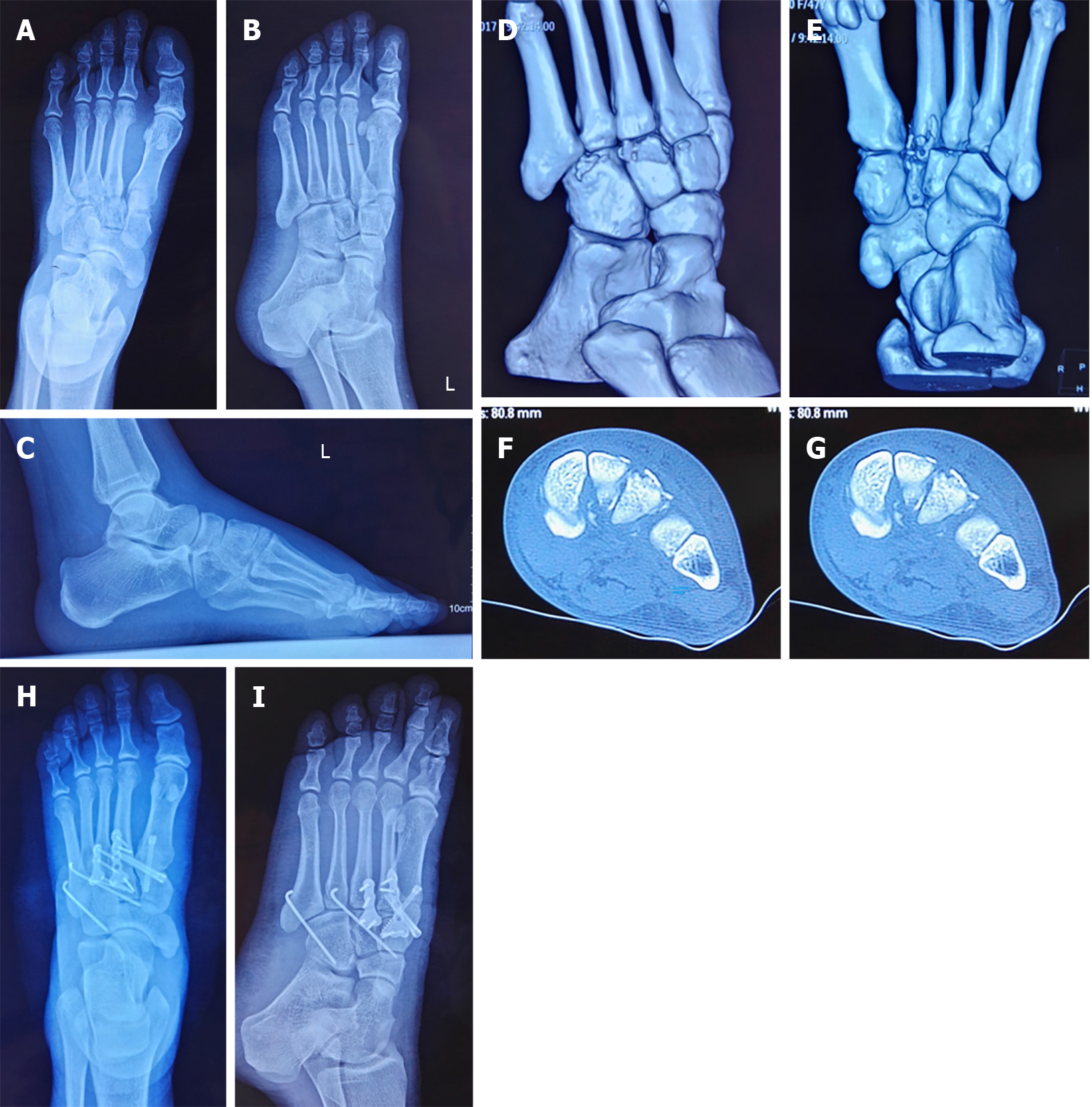
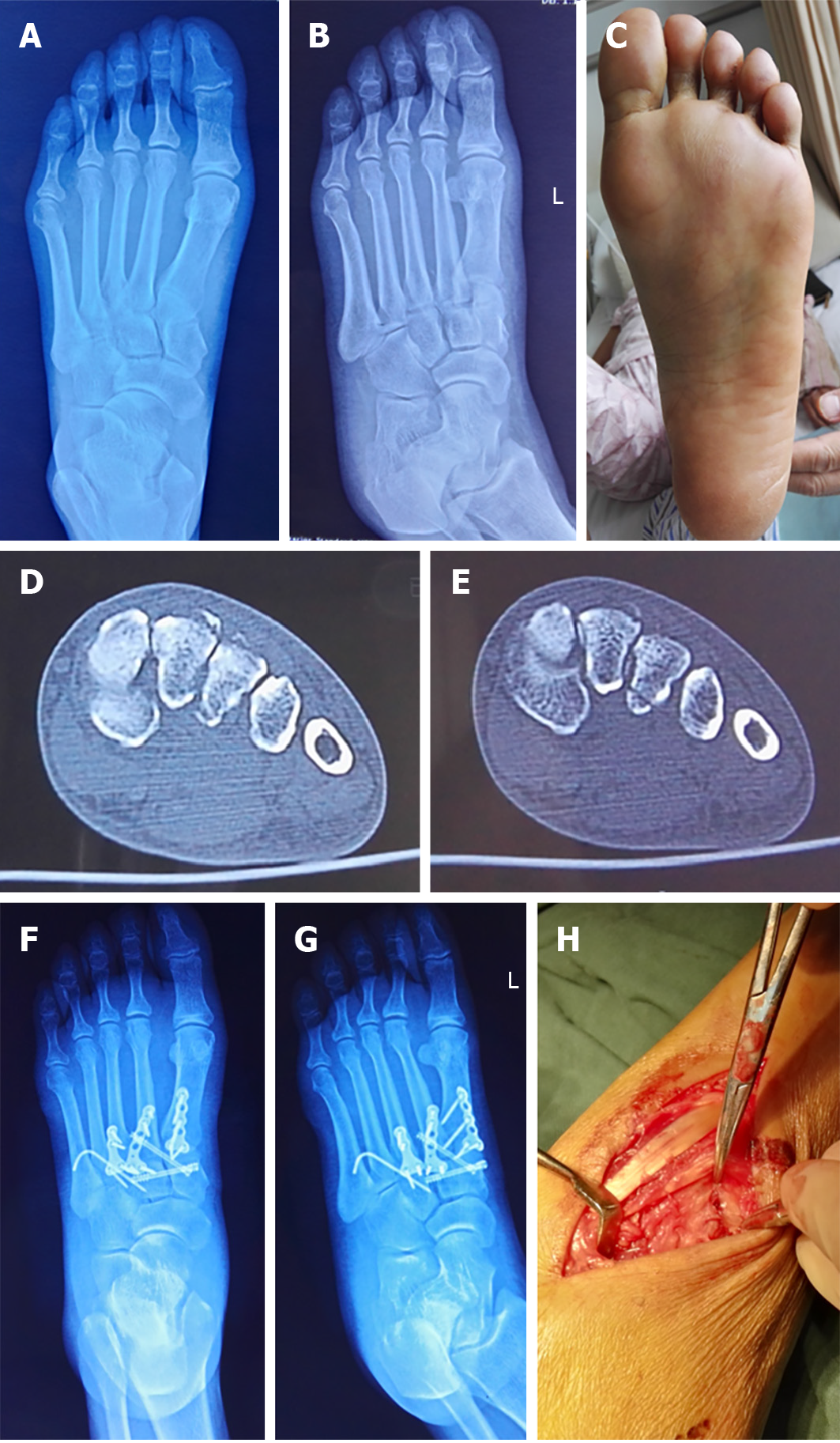
All patients were followed up for 6-20 mo, with an average of 12 mo. All patients' incisions healed in stage 1 and there were no infections. The X-ray results showed no secondary displacement, no foot deformity and no arthritis after trauma. Screw breakage occurred in two patients which did not affect the bone fracture healing. The results of the AOFAS Ankle-Foot Function Score on the last follow-ups were as follows: 12 cases were excellent, five cases were good and one case was acceptable. The excellent/good rate was 88.9%. Figures 1-4 show the case data of 4 patients with an atypical Lisfranc joint complex injury.
A Lisfranc injury often refers to a Lisfranc ligament injury but in a much broader sense refers to an injury of the Lisfranc joint complex[16,17]. According to the nature of external forces, Lisfranc injuries can be divided into two types: Low-energy and high-energy injuries. Low-energy injuries include free-fall injuries of less than 1 m, excessive plantar flexion sprains etc. High-energy injuries include motor vehicle accidents, crush injuries, etc[18]. Most of the low-energy injuries have mild clinical manifestations and are mainly ligament injuries; even if there are fractures, they are mild. Typical imaging manifestations include the "fleck" sign[19] or a small avulsion fracture at the edge of the joint. A dislocation is not obvious after injury; dislocations after trauma may also reduce quickly making diagnosis difficult. In high-energy injuries, the clinical manifestations of most fractures and dislocations are obvious and the findings after imaging are clear at a glance. Regardless of the injury mechanism, most Lisfranc injuries may be typical and can be diagnosed by an X-ray examination followed by standardized treatment. However, for occult simple ligament injuries and avulsion fractures around the Lisfranc joint without obvious displacement, it is difficult to diagnose directly by X-ray. This article mainly discusses the atypical Lisfranc injury of multiple avulsion fractures around the Lisfranc joint complex. In this article, we call this an "atypical Lisfranc joint complex injury". According to clinical treatment experience, this type of injury includes the following characteristics: (1) Presence of bone fractures around the Lisfranc joint complex, and includes the metatarsal base, cuneiform bone, and cuboid bone; (2) Fractures and displacement shown by X-ray images are not obvious and most cases require a CT examination for confirmation; (3) Fractures are often multiple and the displacement of fracture fragments is not obvious; and (4) Results of the stress test mostly show instability. Our hospital's treatment strategies for such injuries are as follows: For positive stress tests, surgical treatment is performed and for negative stress tests, plaster fixation of the foot in the functional position is used for 8-12 wk.
Clinically, how can one identify atypical Lisfranc joint complex injury and its surgical indications? Currently, there are no clear indications in the literature. All the cases included in our retrospective study had positive stress tests. Therefore, for those patients with midfoot pain who had negative X-ray findings during initial consultation, which ones needed further CT examinations or even stress tests under anesthesia? According to our experience, for patients with plantar ecchymosis or obvious tenderness in the midfoot or significant pain in the midfoot under stress, further CT examination is required. For patients with suspected fracture lines on X-ray images, we also recommend a CT examination. For patients with multiple avulsion fractures indicated on CT images, stress tests with or without anesthesia are performed to determine whether the patient needs surgical treatment. Kaar et al[20] reported that in an autopsy study, transverse instability required sectioning of both the interosseous first cuneiform, second metatarsal ligament, the plantar ligament between the first cuneiform and the second and third metatarsals (pC1-M2M3). Longitudinal instability required sectioning of both the interosseous first cuneiform, second metatarsal ligament and the interosseous ligament between the first and second cuneiforms. Raikin et al[21] pointed out in research on the Lisfranc injuries of American football players that rupture or grade-2 sprain of pC1-M2M3 is highly suggestive of an unstable midfoot, for which surgical stabilization is recommended. The appearance of a normal ligament is suggestive of a stable midfoot and the documentation of its integrity may obviate the need for a manual stress radiographic evaluation under anesthesia for a patient with equivocal clinical and radiographic examinations. Studies have also shown that the strength of the plantar ligament of the midfoot is much stronger than that of the dorsal ligament. Once the plantar ligament is damaged, the stability of the Lisfranc joint complex is greatly affected. Lin et al[22] pointed out that the avulsion fractures of the plantar side of the second and third metatarsal base indicated greater violence during trauma and the Lisfranc joint complex being severely damaged which often required surgical reduction and fixation to restore midfoot alignment and stability. Therefore, we concluded that pC1-M2M3 ligament ruptures or ligament attachment point avulsion fractures affect the stability of the Lisfranc joint complex. Thus, it is necessary to be vigilant when there is a metatarsal or interosseous avulsion fracture in the midfoot and the stability of the Lisfranc joint complex needs to be further evaluated; simple dorsal avulsion fractures are often less violent at the time of injury and have little effect on the stability of the Lisfranc joint complex. For patients with Lisfranc joint fractures, stress tests and weight-bearing X-ray radiographs are often difficult to perform. Due to pain, it is difficult for patients to accept further tests[23] and even if the stress test is performed the accuracy will be discounted; in addition, false negative results often occur. Based on these challenges, we recommend that stress tests be performed as much as possible under anesthesia to improve accuracy. In China, due to the weak health consciousness of the people and the uneven level of diagnosis and treatment at different levels of hospitals, the missed diagnosis rate of Lisfranc joint complex injury is high. Even if the diagnosis is clear, some patients have poor compliance with the doctor's orders leading to the poor treatment of Lisfranc joint damage. In light of this medical situation, we advocate that further investigations be actively conducted if Lisfranc joint complex fractures are found. If midfoot instability is diagnosed or highly suspected, surgical treatment should be actively conducted. For patients with multiple fractures involving the plantar side of bones, with larger fracture fragments involving more articular surface and with heavier comminuted fractures of the metatarsal base, we recommend active surgical treatment to better explore, effectively reduce and fix the Lisfranc joint complex to achieve a better treatment outcome. In the diagnosis of Lisfranc joint complex injuries, CT examination is a vital technique. It has strong sensitivity and good specificity and can identify fractures and dislocations that cannot be found and confirmed by X-rays only. However, as CT images are static, they cannot effectively judge the stability of an atypical Lisfranc joint complex injury[24] and as such needs to be combined with stress tests to improve diagnostic accuracy[25]. These injuries are treated according to not only their degree of displacement but also their stability and potential to displace further[14].
The 18 patients included in this study were mostly males and the majority were young adults younger than 45 years. The main injury mechanisms were high-energy injury mechanisms such as car accidents and crush injuries, which indicated that the atypical Lisfranc joint complex injury included in this study was often caused by relatively high-energy direct violence, although there was no obvious difference. As there is no report in the literature or a clear definition of this type of injury, the Myerson classification[26] and Nunley classification[27] methods are also not suitable and have limited prognostic effects[28]. We used the classification method by Lau et al[29] in this study: (1) Type 1: Single column injuries either with or without sagittal displacement of > 2 mm; (2) Type 2A: Two column injuries without sagittal displacement; (3) Type 2B: Two column injuries with > 2 mm sagittal displacement in at least one of the two columns injured; (4) Type 3A: Three column injuries without sagittal displacement; and (5) Type 3B: Three column injuries with > 2 mm sagittal displacement in at least one of the three columns injured. According to the classification method, most cases involve a three-column injury, suggesting that the damage of an atypical Lisfranc joint complex injury is much more severe. In addition, in some cases, even if imaging showed 1 or 2 column injuries, the direct inspection during surgery revealed that joint instability was present in other non-fractured columns. During the operation, tears in the dorsal ligament and articular capsule were seen and the joint space increased significantly under plantar flexion stress. In these cases, we also reduced and fixed these during surgery. Univariate analysis of variance revealed a correlation between postoperative functional score and the number of injured columns (P < 0.01). Latoo et al[30], and Kuo et al[31] pointed out that when assessing Lisfranc injury, the most important thing is the breadth of the foot injury. More columns are usually equivalent to worse functional results. Good anatomical reduction and structural reconstruction are the key factors in obtaining the best prognosis[18,32,33]. Research by Lau et al[34] showed that the risk of arthritis depended on the quality of reduction; good reduction can reduce the risk by 18.2 times than that of normal or poor reduction. Research by Adib et al[35] found that arthritis occurred in 35% of patients with anatomical reduction compared with 80% of patients with non-anatomical reduction. The shortcoming of this study is that it was a single-center retrospective study; thus, there may be biases in collection and selection. Additionally, the number of cases was relatively small and the follow-up times were relatively short. There was only one surgical group without the comparison with a non-surgical group requiring future prospective randomized cohort studies to verify and establish a new classification method[36].
In conclusion, atypical Lisfranc joint complex injury is newly defined and included in Lisfranc injury, but the classification, surgical indications and treatment strategies for this type of injury require further study. In this retrospective study, open reduction and internal fixation for an atypical Lisfranc joint complex injury was performed. The results showed that the patients had a good prognosis and satisfactory functional recovery. The number of columns involved in a Lisfranc joint complex injury was related to the degree of violence, but the prognosis of the injury was not necessarily directly related to the severity of the injury. Combined with the results of other studies, we believe that anatomical reduction and stable fixation are the key factors in determining prognosis.
In the clinic, the incidence of Lisfranc injury is not high but the rate of missed diagnosis is high, especially for occult and atypical injuries. The definition, diagnosis and treatment criteria of such injuries remain controversial.
A new concept "atypical Lisfranc joint complex injury" is introduced in this study.
We hope that the introduction of such a new concept can prompt clinicians to pay attention to such injuries and that this study can make some contributions to further standardize the diagnosis and treatment of this type of injury.
This study used computed tomography and stress tests to diagnose and evaluate atypical Lisfranc joint complex injury, and active open reduction and internal fixation were performed to evaluate patients with joint instability.
In this retrospective analysis of 18 cases with atypical Lisfranc joint complex injury, the rate of excellent and good treatment reached 88.9%.
In this study, a new classification method was used to study the case data which proved that the classification method has good clinical utility for such injuries. From this study, it is concluded that atypical Lisfranc joint complex injury is newly defined and included in Lisfranc injuries, but the classification, surgical indications and treatment strategies for this type of injury require further study. The number of columns involved in the Lisfranc joint complex injury was related to the degree of violence, but the prognosis of the injury was not necessarily directly related to the severity of the injury.
Combining these results with those of other studies, we believe that anatomical reduction and stable fixation are the key factors in determining prognosis.
Thanks to all who made genuine contributions to the manuscript and endorsed the data and conclusions including: Fang Ye, Yi-Xiu Liu, Li-Qun Yang.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ashley S, Martelotto S S-Editor: Wang JL L-Editor: Webster JR P-Editor: Li X
| 1. | Hardcastle PH, Reschauer R, Kutscha-Lissberg E, Schoffmann W. Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br. 1982;64:349-356. [PubMed] |
| 2. | Stødle AH, Hvaal KH, Enger M, Brøgger H, Madsen JE, Ellingsen Husebye E. Lisfranc injuries: Incidence, mechanisms of injury and predictors of instability. Foot Ankle Surg. 2020;26:535-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Ren W, Li HB, Lu JK, Hu YC. Undisplaced subtle ligamentous Lisfranc injuries, conservative or surgical treatment with percutaneous position screws? Chin J Traumatol. 2019;22:196-201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Sivakumar BS, An VVG, Oitment C, Myerson M. Subtle Lisfranc Injuries: A Topical Review and Modification of the Classification System. Orthopedics. 2018;41:e168-e175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Krause F, Schmid T, Weber M. Current Swiss Techniques in Management of Lisfranc Injuries of the Foot. Foot Ankle Clin. 2016;21:335-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Lesko G, Altman K, Hogue G. Midfoot Degenerative Arthritis and Partial Fusion After Pediatric Lisfranc Fracture-Dislocation. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Teng AL, Pinzur MS, Lomasney L, Mahoney L, Havey R. Functional outcome following anatomic restoration of tarsal-metatarsal fracture dislocation. Foot Ankle Int. 2002;23:922-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Coss HS, Manos RE, Buoncristiani A, Mills WJ. Abduction stress and AP weightbearing radiography of purely ligamentous injury in the tarsometatarsal joint. Foot Ankle Int. 1998;19:537-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 88] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Wen Y, Feng P, Zhang H, Tu CQ. [Comparison between allogeneic tendon fixation and screw fixation in ligamentous Lisfranc injury: a biomechanical analysis]. Sichuan Da Xue Xue Bao Yi Xue Ban. 2013;44:222-225, 241. [PubMed] |
| 10. | Crates JM, Barber FA, Sanders EJ. Subtle lisfranc subluxation: results of operative and nonoperative treatment. J Foot Ankle Surg. 2015;54:350-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Stødle AH, Nilsen F, Molund M, Ellingsen Husebye E, Hvaal K. Open Reduction and Internal Fixation of Acute Lisfranc Fracture-Dislocation with Use of Dorsal Bridging Plates. JBJS Essent Surg Tech. 2019;9:e39.1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Chiodo CP, Myerson MS. Developments and advances in the diagnosis and treatment of injuries to the tarsometatarsal joint. Orthop Clin North Am. 2001;32:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Watson TS, Shurnas PS, Denker J. Treatment of Lisfranc joint injury: current concepts. J Am Acad Orthop Surg. 2010;18:718-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 14. | Eleftheriou KI, Rosenfeld PF, Calder JD. Lisfranc injuries: an update. Knee Surg Sports Traumatol Arthrosc. 2013;21:1434-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3199] [Cited by in RCA: 3115] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 16. | Pearce CJ, Calder JD. Surgical anatomy of the midfoot. Knee Surg Sports Traumatol Arthrosc. 2010;18:581-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Peicha G, Labovitz J, Seibert FJ, Grechenig W, Weiglein A, Preidler KW, Quehenberger F. The anatomy of the joint as a risk factor for Lisfranc dislocation and fracture-dislocation. An anatomical and radiological case control study. J Bone Joint Surg Br. 2002;84:981-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Stavlas P, Roberts CS, Xypnitos FN, Giannoudis PV. The role of reduction and internal fixation of Lisfranc fracture-dislocations: a systematic review of the literature. Int Orthop. 2010;34:1083-1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 19. | Desmond EA, Chou LB. Current concepts review: Lisfranc injuries. Foot Ankle Int. 2006;27:653-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 131] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 20. | Kaar S, Femino J, Morag Y. Lisfranc joint displacement following sequential ligament sectioning. J Bone Joint Surg Am. 2007;89:2225-2232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Raikin SM, Elias I, Dheer S, Besser MP, Morrison WB, Zoga AC. Prediction of midfoot instability in the subtle Lisfranc injury. Comparison of magnetic resonance imaging with intraoperative findings. J Bone Joint Surg Am. 2009;91:892-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 22. | Lin J, Huang JH, Wu K, Wang QG. Plantar avulsion fractures of the 2nd and 3rd metartasal base: high risk of occult Lisfranc injuries. Mil Med J S Chin. 2017;31:36-39. |
| 23. | Rammelt S, Schneiders W, Schikore H, Holch M, Heineck J, Zwipp H. Primary open reduction and fixation compared with delayed corrective arthrodesis in the treatment of tarsometatarsal (Lisfranc) fracture dislocation. J Bone Joint Surg Br. 2008;90:1499-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 24. | DeOrio M, Erickson M, Usuelli FG, Easley M. Lisfranc injuries in sport. Foot Ankle Clin. 2009;14:169-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Haapamaki V, Kiuru M, Koskinen S. Lisfranc fracture-dislocation in patients with multiple trauma: diagnosis with multidetector computed tomography. Foot Ankle Int. 2004;25:614-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Myerson MS. The diagnosis and treatment of injury to the tarsometatarsal joint complex. J Bone Joint Surg Br. 1999;81:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 57] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med. 2002;30:871-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 239] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 28. | Yu X, Pang QJ, Yang CC. Functional outcome of tarsometatarsal joint fracture dislocation managed according to Myerson classification. Pak J Med Sci. 2014;30:773-777. [PubMed] |
| 29. | Lau SC, Guest C, Hall M, Tacey M, Joseph S, Oppy A. Do columns or sagittal displacement matter in the assessment and management of Lisfranc fracture dislocation? An alternate approach to classification of the Lisfranc injury. Injury. 2017;48:1689-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Latoo IA, Wani IH, Farooq M, Wali GR, Kamal Y, Gani NU. Midterm functional outcome after operative management of midfoot injuries. Ortop Traumatol Rehabil. 2014;16:639-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Kuo RS, Tejwani NC, Digiovanni CW, Holt SK, Benirschke SK, Hansen ST, Sangeorzan BJ. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am. 2000;82:1609-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 278] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 32. | Lee CA, Birkedal JP, Dickerson EA, Vieta PA, Webb LX, Teasdall RD. Stabilization of Lisfranc joint injuries: a biomechanical study. Foot Ankle Int. 2004;25:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 83] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 33. | Richter M, Wippermann B, Krettek C, Schratt HE, Hufner T, Therman H. Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int. 2001;22:392-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 156] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 34. | Lau S, Howells N, Millar M, De Villiers D, Joseph S, Oppy A. Plates, Screws, or Combination? Radiologic Outcomes After Lisfranc Fracture Dislocation. J Foot Ankle Surg. 2016;55:799-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 35. | Adib F, Medadi F, Guidi E, Alami Harandi A, Reddy C. Osteoarthritis following open reduction and internal fixation of the Lisfranc injury. J Bone Joint Surg Br. 2012;94-B:5. |
| 36. | Lau S, Guest C, Hall M, Tacey M, Joseph S, Oppy A. Functional Outcomes Post Lisfranc Injury-Transarticular Screws, Dorsal Bridge Plating or Combination Treatment? J Orthop Trauma. 2017;31:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |