Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4114
Peer-review started: May 28, 2020
First decision: June 15, 2020
Revised: July 7, 2020
Accepted: August 29, 2020
Article in press: August 29, 2020
Published online: September 26, 2020
Processing time: 116 Days and 9.7 Hours
Schwannomas are rare, often benign, tumors deriving from Schwann cells that have low incidence in the retroperitoneal region (0.5% to 5%). Their diagnosis is hardly confirmed at early stage due to lack of specific features in signs, symptoms and imaging tests. Thus, it is necessary performing guided punch biopsy in order to identify it. Tumor removal is the treatment of choice due to its low sensitivity to radiation and chemotherapy.
Forty-seven years old female patient who was hospitalized for elective orthopedic procedure, without complications, evolved with severe pain in the lower limbs, thigh and gluteal region associated with neurogenic claudication. Persistent pain required magnetic resonance imaging (MRI) of the lumbar spine, which showed epidural collection with dural compression and massive heterogeneous perihepatic nodular lesion. The surgical team opted for draining the collection, as well as requested an MRI of the abdomen and pelvis, whose analysis showed expansive lesion in the retroperitoneum, in close contact with the inferior vena cava and with the right renal vein. A guided puncture was performed for diagnostic clarification, which showed immunohistochemical profile compatible with schwannoma. The selected treatment comprised retroperitoneum tumor resection in association with laparoscopic cholecystectomy. The patient was discharged and remained stable after 4-mo follow-up; she remains under follow-up to check the need of cancer investigations.
Schwannoma features requires surgical treatment based on laparoscopic resection, which often presents low relapse rates and optimistic prognosis.
Core Tip: Schwannomas are rare tumors deriving from Schwann cells, whose incidence in the retroperitoneal region is remarkably unusual (approximately 0.5% to 5%). Their diagnosis is hardly confirmed at early stage due to the lack of specific features in signs, symptoms and imaging tests. The diagnosis of primary retroperitoneal schwannoma in the herein reported case was incidental; it happened during the postoperative follow-up of a patient who had been subjected to an orthopedic procedure in the lumbosacral spine. Laparoscopic resection of the tumor was the treatment of choice; the patient did not present complications and remains under oncological follow-up.
- Citation: Ribeiro Jr MAF, Elias YGB, Augusto SS, Néder PR, Costa CTK, Maurício AD, Sampaio AP, Fonseca AZ. Laparoscopic resection of primary retroperitoneal schwannoma: A case report. World J Clin Cases 2020; 8(18): 4114-4121
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4114.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4114
Schwannomas are rare tumors deriving from Schwann cells found in peripheral nerve sheaths[1-8]; they are often diagnosed in patients’ head, neck and extremities[1-10]. Schwannoma incidence in the retroperitoneal region is quite rare; it accounts for only 0.5% to 5% of all cases of it[7]. Such incidence prevails among women, mainly in patients in the age group 20-60 years, although it can affect individuals at any other age[1-10].
Early schwannoma diagnosis is unusual due to lack of specific signs and symptoms capable of characterizing the disease and of leading patients to seek medical help[1-5,7,9-11]. In addition, findings of ultrasound images, computed tomography (CT) and magnetic resonance imaging (MRI) directly linked to the disease are poorly described. Thus, many cases are diagnosed incidentally during imaging exams. Advanced stage schwannomas can be associated with abdominal pain or palpable abdominal tumor, and even with atypical symptoms such as secondary hypertension, hematuria, renal colic and headache[1-7,9,11]. Schwannomas are often benign; however, they can lead to malignant tumor transformation when they are associated with Von Recklinghausen’s disease[1,2,4,6,7]. It is necessary performing CT- or ultrasound-guided punch biopsy, with anatomopathological report, in order to confirm the preoperative diagnosis and start treatment[1,2,6,7,11]. Surgical removal of the tumor is the treatment of choice, since schwannomas are not very sensitive to radiotherapy and/or che-motherapy[1-11].
The aims of the current study were to report the case of a primary retroperitoneal schwannoma incidentally diagnosed and to present a literature review on the topic.
Description of a retroperitoneal schwannoma case treated based on laparoscopic approach without complications, and review of similar cases described in the literature for the last 20 years.
A 47-year-old female patient was admitted to the orthopedics service to undergo elective decompression surgery and lumbosacral spine arthrodesis (L4, L5, S1).
The orthopedic procedure was performed without complications. On the first postoperative day, the patient presented severe pain in the anterior aspect of the thigh, bilateral burning in the gluteal region and lower limbs in shock with neurogenic claudication.
Patient’s comorbidities comprised type II Diabetes Mellitus and hypothyroidism. The patient used 500 mg Metformin twice a day and 50 μg Levothyroxine once a day, on a regular and continuous basis, and did not have allergies.
The patient was in good general condition; she was flushed, hydrated, eupneic, afebrile and presented obesity grade I. The physical examination of the chest and cardiovascular system did not present relevant findings. Patients’ abdomen was flaccid and painless; it presented normal noises and did not show visceromegaly or palpable masses. Her orthopedic surgical incision presented satisfactory appearance. She had been submitted to a specific spinal cord MRI prior to her orthopedic surgery.
Lumbar CT was requested and, since the patient presented persistent pain on the 5th postoperative day, MRI of the lumbar spine was also requested; results showed posterior epidural collection in L3 and L4 with dural and spinal canal compression, as well as massive heterogeneous nodular perihepatic lesion (of undetermined nature) anterior to the right kidney. There were no association between the collection and the Schwannoma. The patient was subjected to a new surgery to drain the 50 mL collection that caused dural sac compression; the procedure did not show complications.
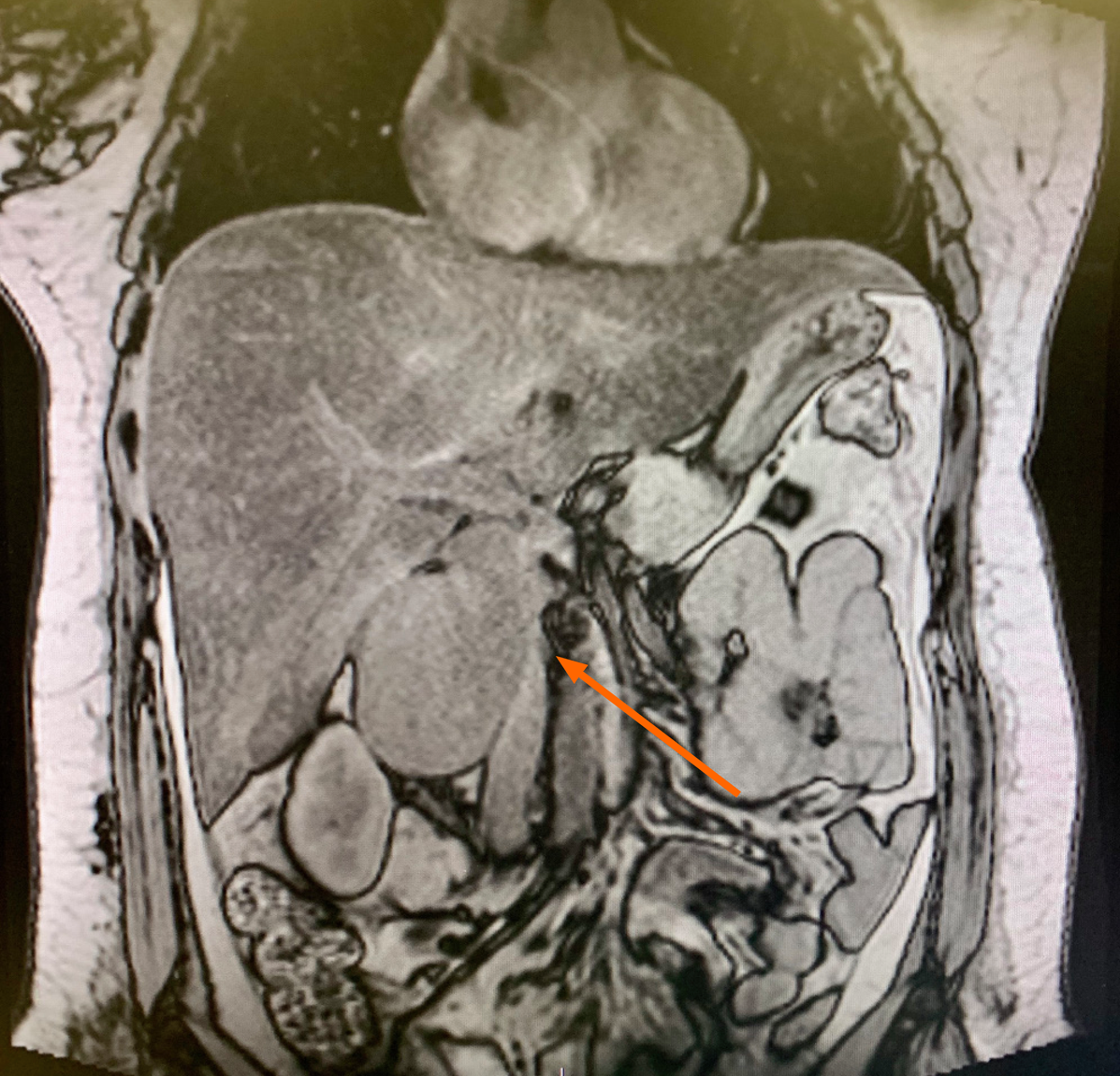
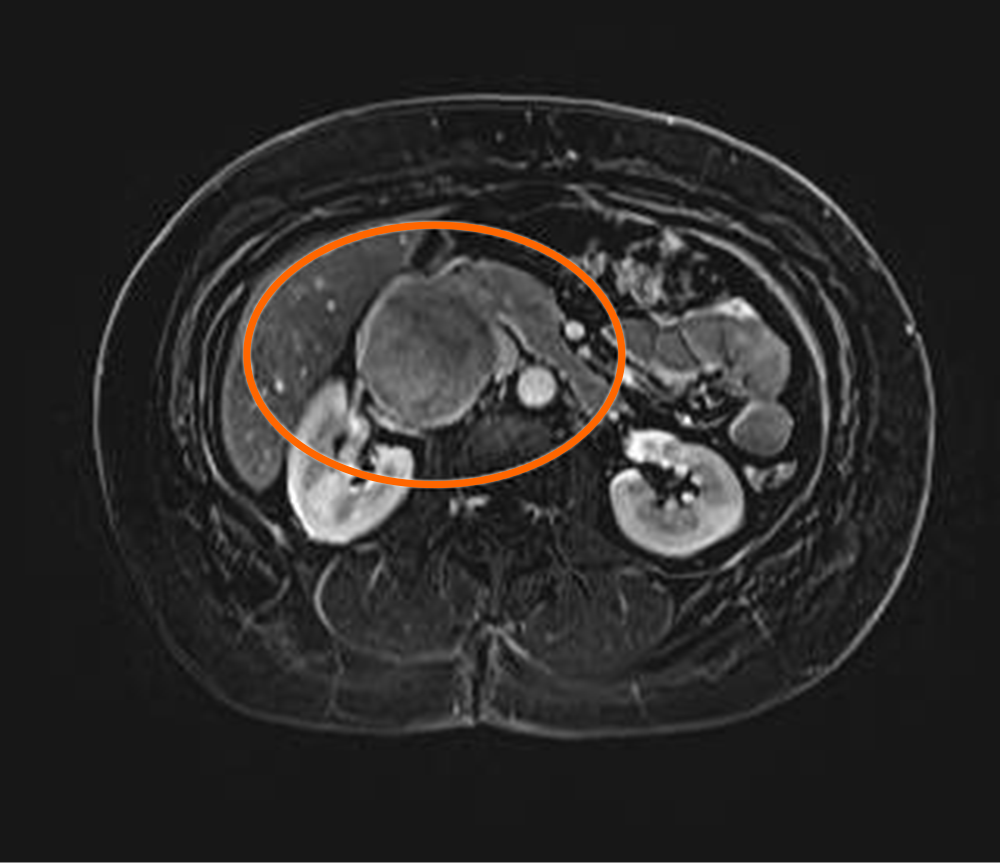
Given the heterogeneous mass found in front of the right kidney, which led to significant thinning of the inferior vena cava in lesion topography, the general surgery team was required to assess the patient, who had her pain stabilized and did not have new episodes of it. MRI of the abdomen and pelvis was requested by the general surgery team; results have shown undetermined, expansive, 7.2-cm retroperitoneal lesion on the right side of patient’s body – it was in close contact with the inferior vena cava and with the right renal vein, which caused a compression that extended toward the left renal vein (Figure 1 and 2). The patient did not present compressive symptoms associated with the lesion.
CT-guided puncture was performed to collect two biopsy fragments, which were subjected to anatomopathological analysis for diagnostic clarification purposes. Analysis results have shown fusiform neoplasia, with discrete nuclear atypia, interspersing more and lesser cellular areas. Mitosis and necrosis figures were not detected. The material was subjected to immunohistochemical profile analysis, which indicated its compatibility to schwannoma.
Primary retroperitoneal schwannoma was the final diagnosis of the herein reported case.
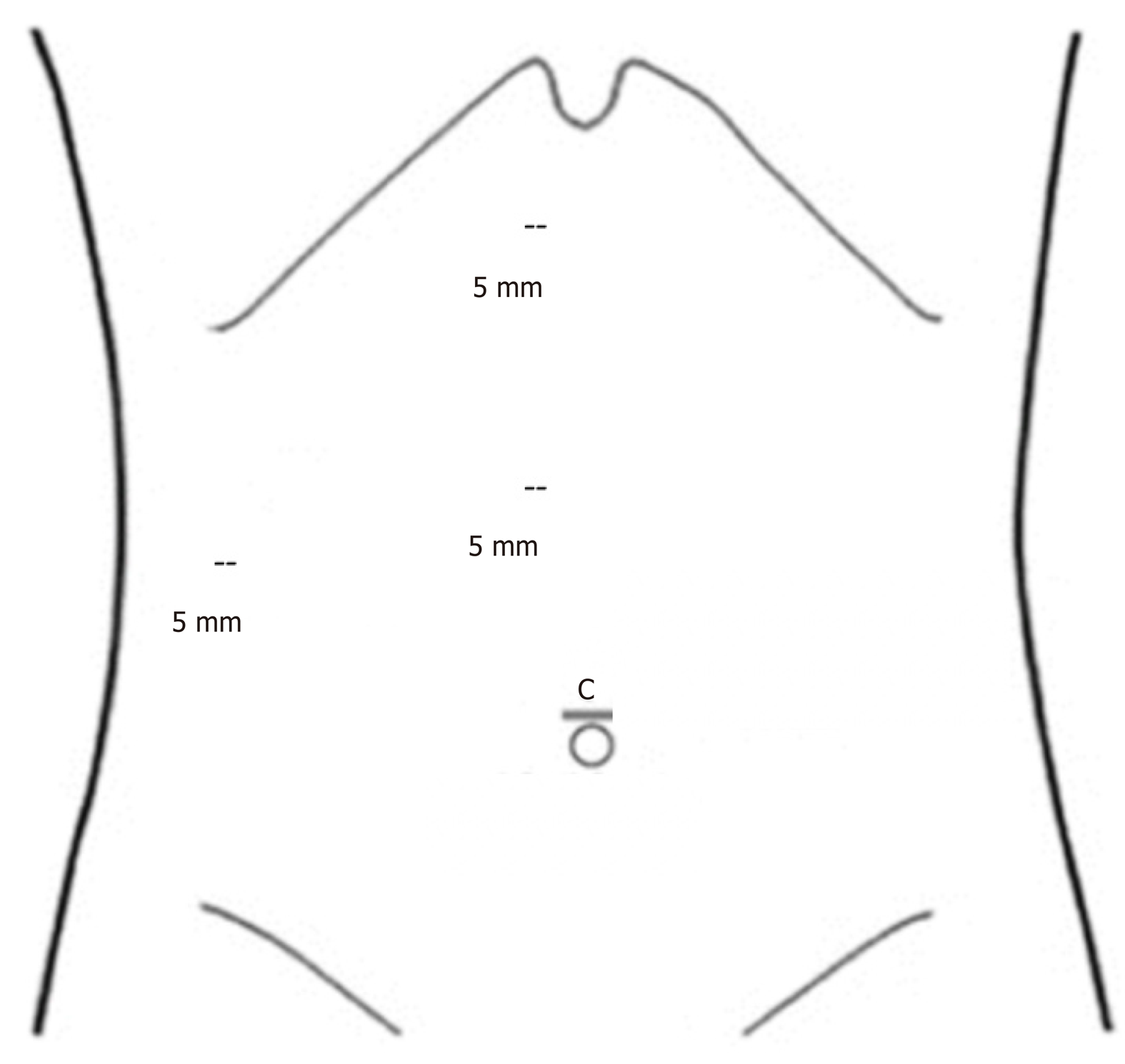
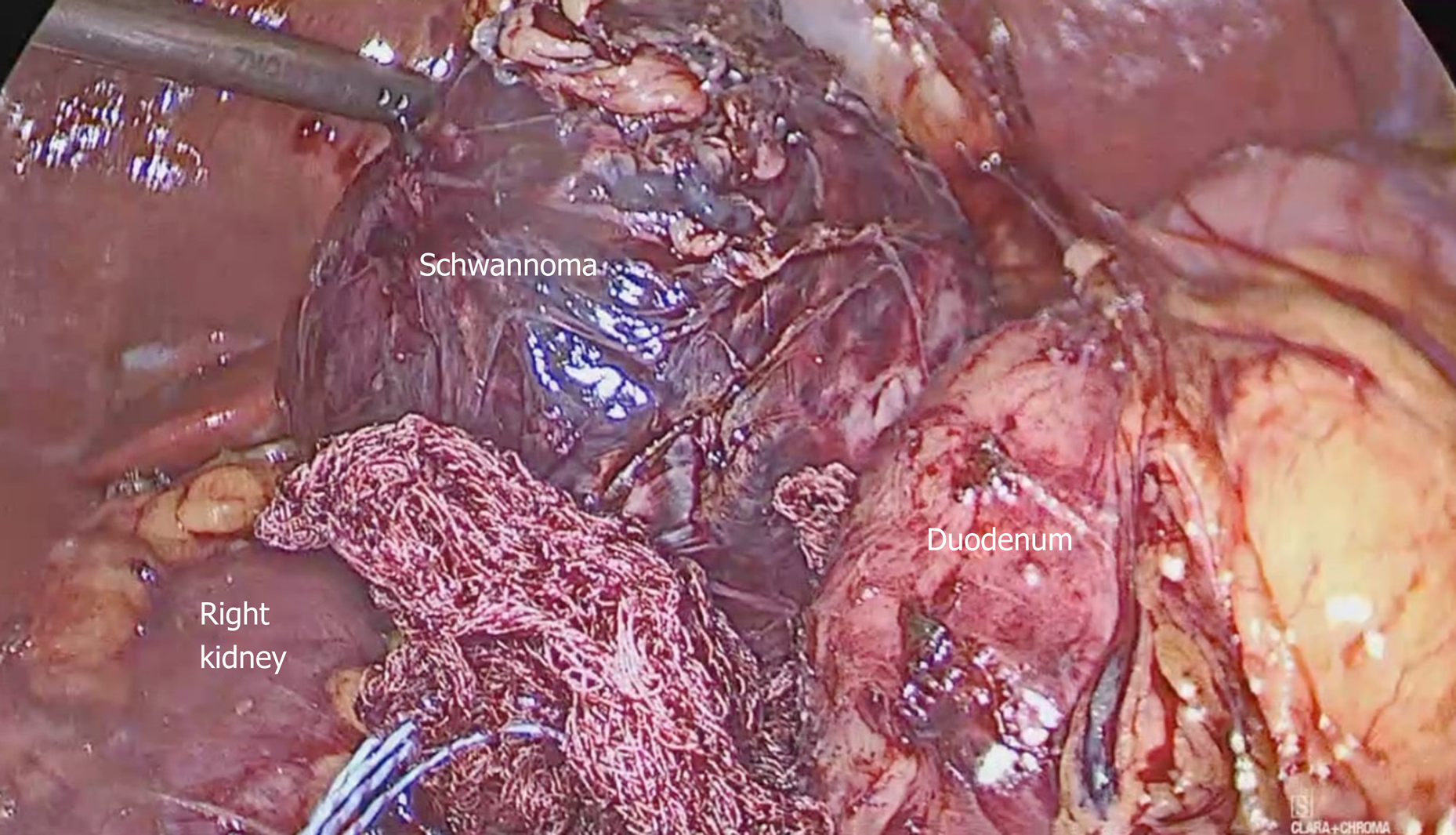
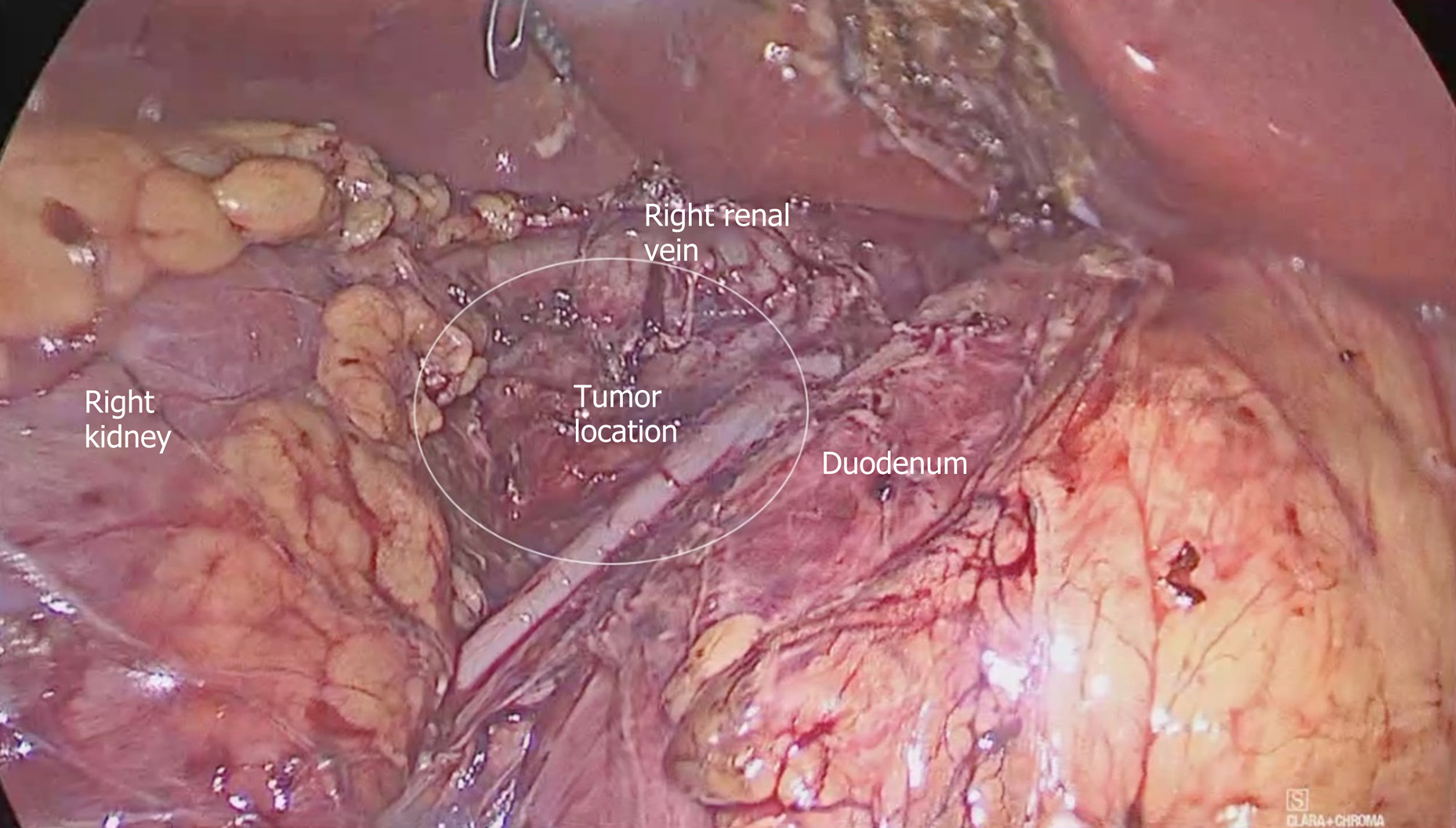
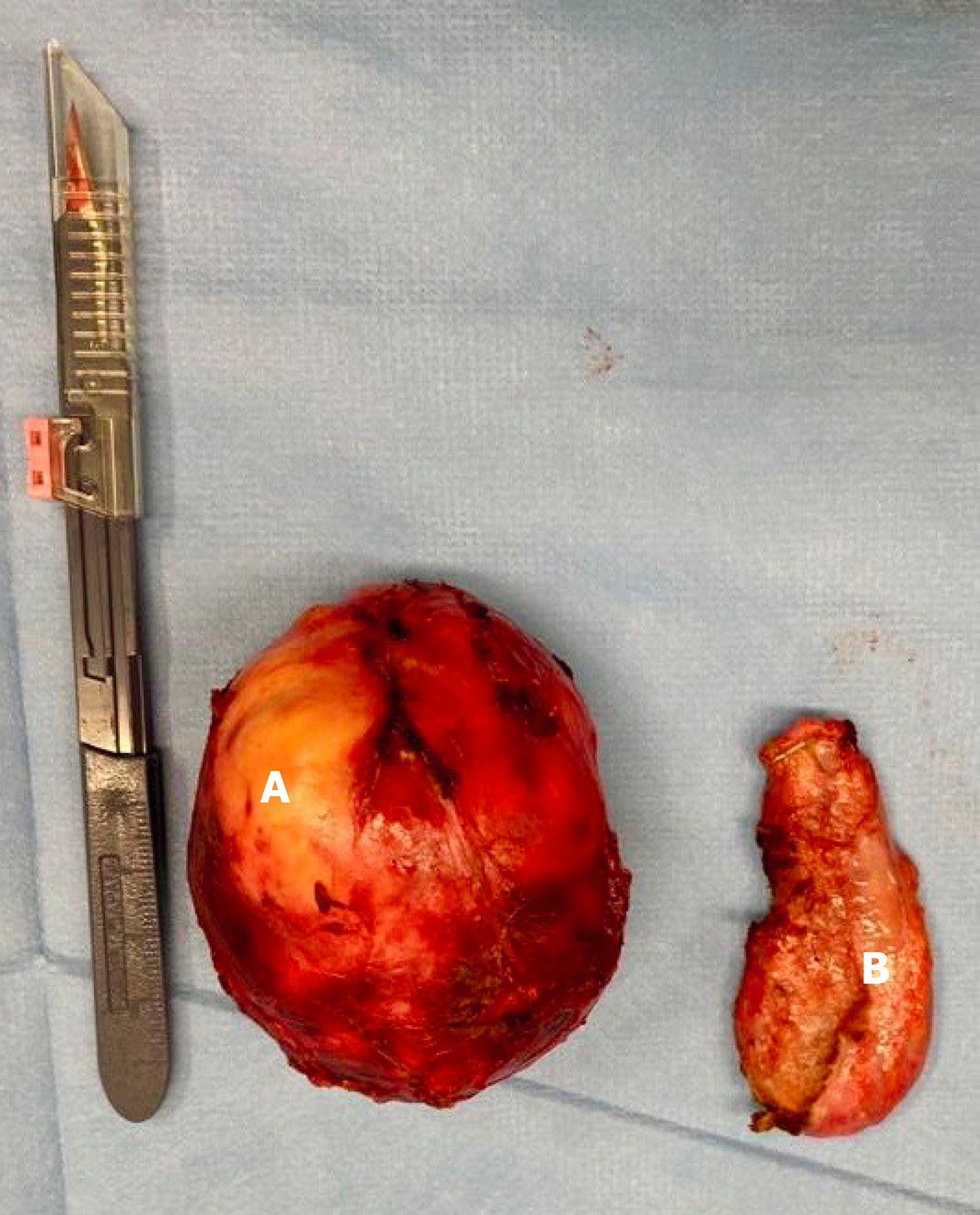
After the case was discussed with the tumor board and the patient, the surgical team opted for resecting the retroperitoneal tumor in association with cholecystectomy (the gallbladder was used to mobilize the liver) via laparoscopic approach. Port placement is shown in Figure 3. A large lesion was found in the retroperitoneum (zone II) during the procedure; it was adhered to patient’s duodenum, vesicle, kidney, right renal vein and inferior vena cava (Figure 4). An adequate cleavage plan for safe lesion resection was identified; although labor-intensive, the surgery was carried out safely and did not have intraoperative complications (Figure 5). The surgical specimen had nodular aspect and was covered by a thin brownish membrane (dimensions: 8.2 cm × 6.4 cm × 5.3 cm), as shown in Figure 6 and 7.
The immunohistochemical analysis applied to the specimen resected during surgery has shown the following results: Positive CD-56; positive CD-68; positive EMA; positive Ki-67 at 7%; strong and diffuse positive S-100. The final anatomopathological report has confirmed that the patient had non-malignant schwannoma; she was discharged on the 3rd postoperative day.
The patient remained stable, with no complications after 4 mo of the surgery.
Schwannomas, which are also known as neurinomas or neurilemmomas, affect women to a greater extent than men[1,2,4,5,7,10]. This tumor type accounts for approximately 0.5% to 12% of retroperitoneal tumors[2]. Symptoms, whenever present, are nonspecific and delayed due to great retroperitoneum flexibility. The course of the disease is often asymptomatic, and it is incidentally diagnosed at advanced stage[1,2,4,5,7,10] Table 1. The patient in the herein reported case was female and had nonspecific symptoms, such as headache and lower limb pain, which were in compliance with cases described in the literature. It is worth emphasizing that the patient was asymptomatic for retroperitoneal lesion, did not present any type of compressive symptom, neither in the digestive tract nor in the vascular system. Jankowski et al[9] have reported the case of a patient with history of low back pain and compression on the right side of the sciatic nerve, which led to displacement of the kidney, renal artery and vein, and vena cava, similar to the herein reported case. The aforementioned authors described symptoms such as increased pain at rest, muscle weakness and paresthesia, as seen in the present report before the arthrodesis surgery. Tumor expansion can cause extensive dorsal spine bone destruction, whereas tumor growth can lead to erosive pressure on adjacent bone structures. Schwannomas are often single, with firm and delimited consistency; they often change to form cysts and calcifications, and can present hemorrhages[2,3,5,7,8]. The described case was a single, well-defined lesion without local or remote invasive features, which corroborated previously presented data. In histological terms, its featuring was well described as the alternation of Antoni A (elongated and compact spindle cells with paler pattern) and Antoni B (loose cell arrangement in varying medium) areas. The alternation between two areas featured the benign pattern. Malignancy is often determined by the number of mitoses, as well as by vascular invasion and pleomorphism; tumor size is not relevant for such confirmation[1,2,3,5,7] and immunohistochemical analysis shows strong and diffuse S-100 protein mark in the cytoplasm of schwannoma cells[1,2,5,7,11]. This pattern is in compliance with the one observed in the analysis of the specimen during surgery. Preoperative imaging exams are of paramount importance to help defining tumor delimitations, although they do not complete the diagnosis in separate. The main manifestations observed in magnetic resonances of retroperitoneal schwannomas are hypointense on T1-weighted sequences and slightly hyperintense on T2-weighted ones; they also show varying enhancement in the presence of intravenous contrast. These patterns found in MRI can change depending on the arrangement of Antoni A and Antoni B areas; malignant schwannomas show intensity confluence in T1- and T2-weighted sequences. Although there are some features at the MRI, it cannot be used as specific standard to diagnose the disease[1-3,5,6,7,10,11]. Fibrosarcoma, liposarcoma and ganglioneuroma are differential diagnoses, which present similar pattern in CT and MRI[1,5]. Ultrasound- or CT-guided biopsy plays a key role in defining patients’ therapeutic plan in the preoperative period. Radio and/or chemotherapy are not recommended due to lack of tumor sensitivity to these treatments[1,2,4,6,7,11]. The only approach capable of confirming, and treating, patients’ condition lies on the surgical resection of the identified mass in order to subject it to reliable analysis, as well as to relief patients’ potential symptoms. The laparoscopic and robotic pathways are promising treatment alternatives depending on tumor location and size; they also depend on appropriate training in advanced procedures such as the management of vascular structures and anastomoses[1,2,5-7,8,10,11]. The patient in the current case report was subjected to laparoscopic procedure and did not have complications; however, the tumor was in close contact with noble structures such as duodenum, right renal vein and vena cava, which often require meticulous dissection to avoid iatrogenesis. Benign retroperitoneal schwannomas have good prognosis and low relapse rates. Nevertheless, it is necessary monitoring patients after tumor removal because malignant degeneration cases present higher relapse rates[2,7].
| Ref. | Year | Findings |
| Chan et al[10] | 2019 | Retroperitoneal benign schwannoma presenting as a pelvic tumor |
| Harada et al[3] | 2018 | Patient after retroperitoneal tumor surgery, returns with a bladder deviation, suspecting a malignant tumor. After pathological analysis there was evidence of a benign tumor - Schwannoma |
| Zhang et al[7] | 2018 | Retroperitoneal benign schwannoma with similar size |
| Ragu et al[8] | 2017 | Retroperitoneal benign schwannoma |
| Queiroz et al[5] | 2017 | Retroperitoneal benign schwannoma treated with left nephrectomy |
| D'Andrea et al[11] | 2016 | Retroperitoneal benign schwannoma abutting the IVC |
| Álvarez et al[1] | 2012 | Incidental retroperitoneal benign schwannoma |
| Chiang et al[4] | 2009 | Incidental retroperitoneal benign schwannoma in a patient with back pain |
| Cury et al[2] | 2007 | Benign retroperitoneal schwannoma misdiagnosed as an adrenal tumor |
Schwannoma is a rare retroperitoneal tumor that presents nonspecific features in signs, symptoms and imaging exams; this tumor is often diagnosed at advanced stage. It is highly recommended performing lesion biopsy to confirm schwannoma diagnos-is - before adopting the surgical approach - to help better understanding tumor delimitations and repercussions in adjacent organs. The final diagnosis is based on anatomopathological analysis, which requires immunohistochemical tests. The treatment is of the surgical type, as seen in the herein reported case, whose tumor was accessed and resected based on the laparoscopic approach. Schwannoma has low relapse rate and its prognosis is quite optimistic.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ito S, Sperti C S-Editor: Ma YJ L-Editor: A P-Editor: Zhang YL
| 1. | Alvarez Z C, Sanhueza P B, Ruiz F I, Castillo A J. [Retroperitoneal schwannoma. Report of one case]. Rev Med Chil. 2012;140:767-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Cury J, Coelho RF, Srougi M. Retroperitoneal schwannoma: case series and literature review. Clinics (Sao Paulo). 2007;62:359-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Harada TL, Nagao G, Aoyagi T, Kuroda I, Tokuyama N, Takahashi M, Takahashi Y, Morishita Y, Shinji S. Giant retroperitoneal schwannoma in a 52-year-old man. Radiol Case Rep. 2018;13:810-814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Chiang ER, Chang MC, Chen TH. Giant retroperitoneal schwannoma from the fifth lumbar nerve root with vertebral body osteolysis: a case report and literature review. Arch Orthop Trauma Surg. 2009;129:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Queiroz MR, Rocha PH, Félix PR, Landell GA, Gomes MP, Abud LG, Oliveira RGG. Schwannoma celular retroperitoneal. Medicina (Ribeirão Preto Online). 2017;50:182-187. [DOI] [Full Text] |
| 6. | Oliveira MLG, Lopes Filho GJ. Neurofibrossarcoma retroperitoneal primário. Rev Col Bras Cir. 2003;30:399-401. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Zhang L, Gao M, Zhang T, Chong T, Wang Z, Liu W, Li H. Surgical management of retroperitoneal schwannoma complicated with severe hydronephrosis: A case report. Medicine (Baltimore). 2018;97:e12528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Ragu R, Blanchard C, Meurette G. Robotic excision of large retroperitoneal Schwannoma (with video). J Visc Surg. 2017;154:297-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Jankowski R, Szmeja J, Nowak S, SokóÅ‚ B, Blok T. Giant schwannoma of the lumbar spine. A case report. Neurol Neurochir Pol. 2010;44:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 10. | Chan TS, Wong T, Pan NY. Primary pelvic retroperitoneal ancient schwannoma-a rare diagnosis of pelvic complex cystic lesion. Hong Kong Med J. 2019;25:160.e1-160.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | D'Andrea G, Sessa G, Picotti V, Raco A. One-Step Posterior and Anterior Combined Approach for L5 Retroperitoneal Schwannoma Eroding a Lumbar Vertebra. Case Rep Surg. 2016;2016:1876765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |