Published online Jun 26, 2020. doi: 10.12998/wjcc.v8.i12.2590
Peer-review started: March 8, 2020
First decision: April 21, 2020
Revised: May 2, 2020
Accepted: May 26, 2020
Article in press: May 26, 2020
Published online: June 26, 2020
Processing time: 107 Days and 15.7 Hours
As the complex anatomy of maxillary first molars is one of the major challenges in endodontic therapy, knowledge of the complicated root canal anatomy and configuration is crucial to ensure the success of endodontic treatment and prognosis. This article presents an endodontically managed left maxillary first molar with an unusual palatal root morphology. The available literature on the anatomic variation of maxillary first molars is also reviewed.
A 36-year-old man with no medical history presented to the Stomatology Department of Peking University Third Hospital complaining of a toothache during mastication in the maxillary left posterior region for approximately 3 mo. He had a spontaneous and intermittent toothache that had worsened, particularly at night. The diagnosis based on clinical examination, X-ray imaging, and cone beam computed tomography (CBCT) was symptomatic irreversible pulpitis. Nonsurgical endodontic therapy was performed for the left maxillary first molar. Five root canals revealed by CBCT included a special palatal root canal (1-2-1-shaped), two mesiobuccal root canals, and one distobuccal root canal. Evaluation of the CBCT images confirmed the root canal morphology and the clinician performed more effective cleaning, obturation, and therapy. Finally, the tooth was restored using composite resin, and the patient was satisfied with the result.
CBCT and a complete review of the literature may be beneficial for investigating the root canal system to achieve a biological and functional therapeutic effect.
Core tip: A rare case of the left maxillary first molar with a special palatal root canal (1-2-1-shaped) is described in detail. The range of knowledge on the anatomy of root canals in the permanent maxillary first molar is extended. Cone beam computed tomography is an effective means for understanding complicated root canal anatomy and plays a significant role in the diagnosis and treatment of endodontic diseases.
- Citation: Zhang ZH, Yao HL, Zhang Y, Wang X. Endodontic management of the maxillary first molar with special root canals: A case report and review of the literature. World J Clin Cases 2020; 8(12): 2590-2596
- URL: https://www.wjgnet.com/2307-8960/full/v8/i12/2590.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i12.2590
The anatomical characteristics of permanent maxillary molars are complex and are generally described as teeth with three roots: Two buccal root canals and one palatal root canal[1]. In recent years, two palatal and two mesiobuccal root canals have been reported separately[2]. The incidence of a second mesiobuccal root canal (MB2) is 58.4% in Asians[3]. The incidence of a second distobuccal canal is between 1.6% and 9.5%[4]. The anatomy and morphology of roots in the permanent maxillary first molar and root canals vary greatly. Except for three roots, other variations include two[5], four[6], five[7], six[8], seven[9], and eight[10] root canals as well as O-shaped canals[11] within individual roots. Innumerable clinical studies and case reports of maxillary first molars have been reported on various root canal morphologies (Table 1).
| Ref. | Yr | No. of roots | No. of canals | Root canals anatomy | Country | Tooth | Sex | Age (yr) | Type of study | ||
| MB | DB | P | |||||||||
| Ferguson et al[7] | 2005 | 3 | 5 | 3 | 1 | 1 | United States | L | M | 18 | Case report |
| Kottoor et al[14] | 2010 | 3 | 7 | 3 | 2 | 2 | India | R | M | 37 | Case report |
| Kottoor et al[10] | 2011 | 3 | 8 | 3 | 3 | 2 | India | L | M | 30 | Case report |
| Shin et al[11] | 2013 | 1 | 1 | O-shaped | Korea | L | M | 39 | Case report, ex vivo study | ||
| Badole et al[9] | 2014 | 3 | 7 | 3 | 2 | 2 | India | L | M | 28 | Case report |
| Ahmad et al[31] | 2014 | 3 | 5 | 3-2, 3-3 | 1 | 1 | Germany | R | M | 28 | Case report |
| Asghari et al[2] | 2015 | 4 | 4 | 1 | 1 | 2 | Iran | R | W | 21 | Case report |
| Rodrigues et al[36] | 2017 | 3 | 7 | 3 | 2 | 2 | Brazil | R | W | 23 | Case report |
| Schryvers et al[6] | 2019 | 4 | 4 | 1 | 1 | 2 | Belgium | L | M | 44 | Case report |
| Liu et al[33] | 2019 | 2 | 2 | 1 | 1 | China | L, R | W, W | 63, 45 | Case report | |
The primary goal of endodontic treatment is not only identification, meticulous cleaning, and perfect shaping but also places vital importance on familiarity of the three-dimensional obturation of the entire root canal pattern[12]. Indeed, undetected extra roots and unusual canals can lead to endodontic failure[13]. Cone-beam computerized tomography (CBCT) is an objective analytical tool to ascertain complex root canal morphology[14], especially for maxillary molars[15], and such unusual morphology can be confirmed with the aid of CBCT. Among Asians, there is a prevalence of Vertucci type I (35.0%), Vertucci type II (15.0%), and type IV (45.0%) configurations[3]. The present case report discusses the successful endodontic management of a maxillary first molar presenting with five root canals consisting of double mesiobuccal root canals, one distobuccal root canal, and one 1-2-1-shaped palatal root canal by CBCT; the related literature is also reviewed.
A 36-year-old man with no medical history presented to the Stomatology Department of Peking University Third Hospital, Beijing, China, complaining of a toothache during mastication in the maxillary left posterior region for approximately 3 mo.
He had a history of spontaneous and intermittent toothache for the past month. The pain was spontaneous and severe, particularly at night.
The patient had a free previous medical history.
Clinical examination revealed a deep mesio-occlusal carious lesion on the left maxillary first molar (tooth 2.6). Palpation of the buccal and palatal aspects of the involved teeth did not reveal any tenderness. However, the left maxillary first molar exhibited tenderness to vertical percussion. The teeth were not mobile, and periodontal probing around the teeth was within physiological limits. Thermal testing of the involved tooth with heated gutta-percha and dry ice caused intense lingering pain; electronic pulp stimulation (Parkell Electronics Division, Farmingdale, NY, United States) showed pulpal vitality for the tooth.
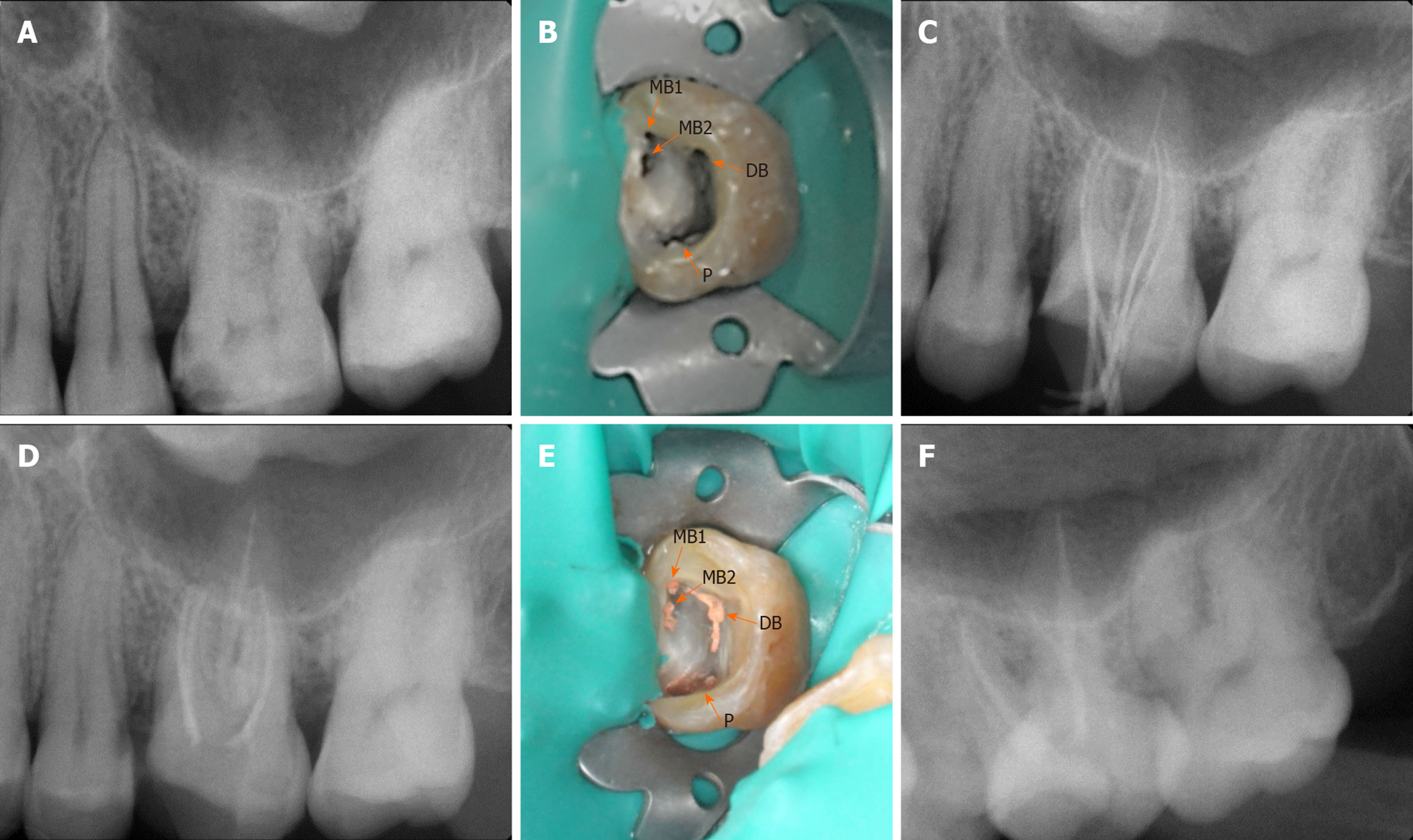
A preoperative X-ray radiograph revealed carious lesions closely approximating the pulp with a widened periodontal ligament adjacent to the mesiobuccal root with respect to the left maxillary first molar (Figure 1A).
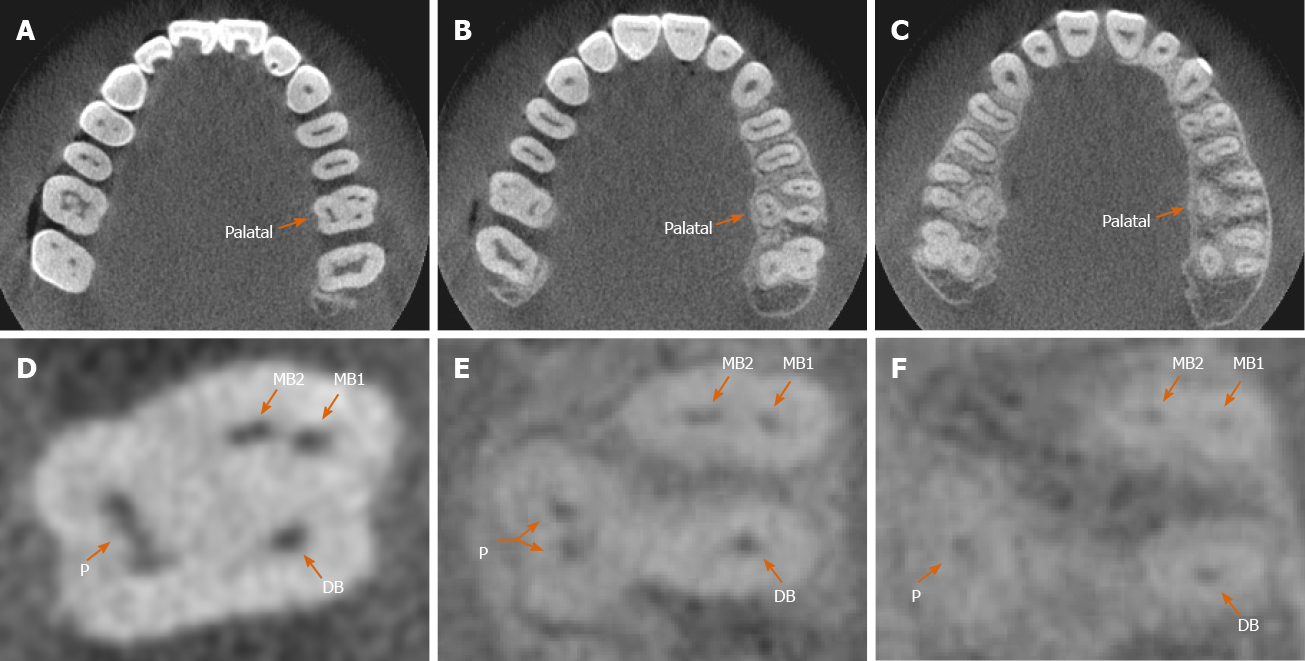
The medullary bottom could be explored with four root canal ports (Figure 1B). The root canal length was measured (PROPEX II, Densply Maillefer CH-1338 Ballaigues, Israel). CBCT images revealed two mesiobuccal root canals, one distobuccal root canal, and one 1-2-1-shaped palatal root canal for the left maxillary first molar (Figure 2A-F).
Endodontic therapy was proposed and accepted by the patient. Written informed consent was obtained from him. The tooth was isolated with a rubber dam after local infiltration anesthesia. After removing the crown pulp, the medulla chamber was found to be rectangular. Cleaning and shaping were performed using rotary instruments (X-SMART, Dentsply France SAS, 4, rue Michael Faraday, Japan) along with 17% EDTA gel (canal lubricant and chelating agent, Pulpdent Corporation, 80 Oakland St. Watertown, MA, United States); 3% sodium hypochlorite was used as the working solution. All the mesiobuccal and distobuccal canals were enlarged to size 30/0.04, whereas the palatal canal was enlarged to size 40/0.04.
Master cones (Dentsply Maillefer) were selected corresponding to the size and taper of the last file used to the working length, which was confirmed radiographically (Figure 1C). The canals were dried with absorbent paper points (Dentsply Maillefer, Ballaigues, Switzerland), and obturation was performed using gutta-percha (Dayading, Beijing, China). Final radiographs were taken to establish the quality of the obturation (Figure 1D). The postobturation clinical image is shown in Figure 1E. Then, the tooth was filled with resin sealer on the chamber.
The final diagnosis of the presented case was symptomatic irreversible pulpitis.
Nonsurgical endodontic therapy was performed with the aid of CBCT.
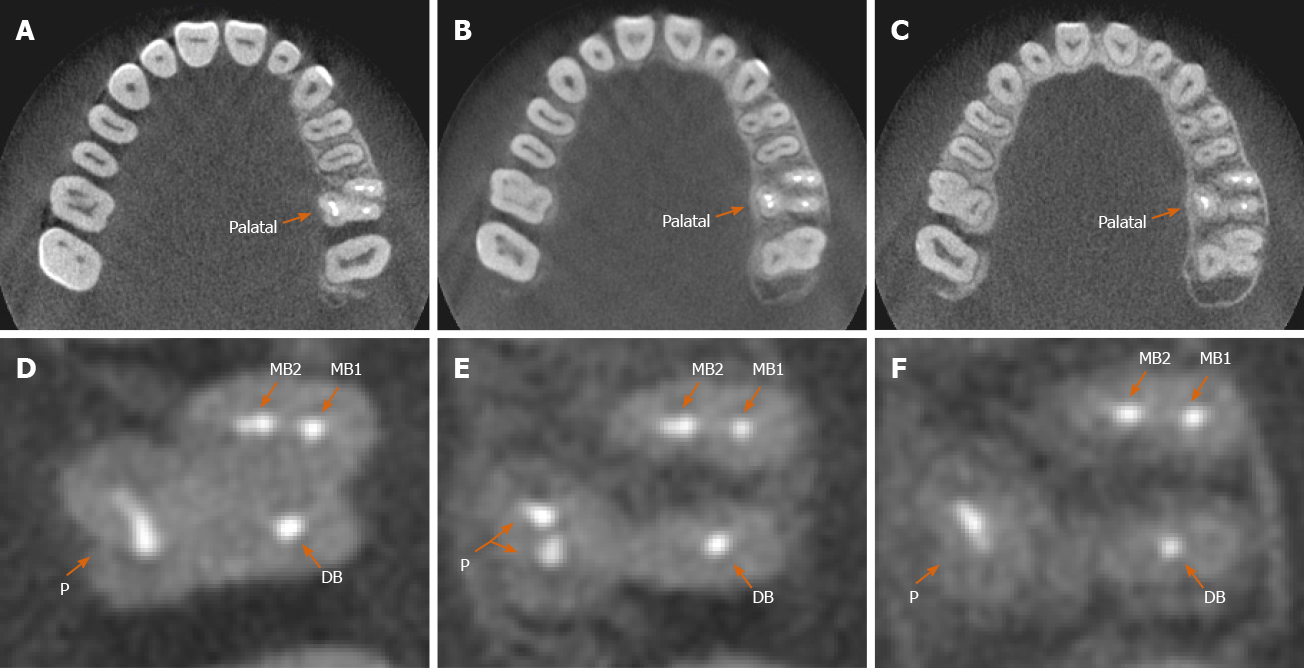
At 1 year, the patient remained asymptomatic during the follow-up period by X-ray radiograph (Figure 1F) and CBCT (Figure 3A-F). His discomfort disappeared, and he was satisfied with the results.
The most common morphology of the maxillary first molar is three roots and four canals. However, the mesiobuccal root of the maxillary first molar often contains a double root canal system, and the incidence of a second mesiobuccal canal (MB2) has been reported to be between 18.6% and 96.1%[16]. The presence of the MB2 root canal is 58.4% for maxillary first molars among Asians[17]. Accessory canals have been observed in the mesiobuccal root in 30.8% (MB1) and 5.6% (MB2), the distobuccal root in 15.1%, and the palatal root in 11.7% of maxillary molars[18]. The observed frequency of accessory canals in the distobuccal and palatal roots is similar[4,19]. We summarize the available case reports for a maxillary first molar with multifarious root canal anatomy (Table 1).
In the present case, Vertucci type IV mesiobuccal, Vertucci type I distobuccal, and Vertucci type III (1-2-1) palatal root canals were observed in the anatomical system. Among the different types of mesiobuccal roots of maxillary first molars[20-23], the highest prevalence is for Vertucci type I[24,25]. The root canal configuration type of the palatal root is reported in the literature, with even lower variations from Vertucci type I in the distobuccal root[19]. In addition, 33.3% of the palatal roots of the maxillary first molars have a V type configuration[26].
Anatomical variations occur frequently in maxillary molars, and CBCT scanning is used for a better understanding of the complex root canal anatomy. The morphological dimensions of a total of 1727 physiological foramina have been investigated by CBCT, with mean narrow and wide (to a high number, oval) diameters of the physiological foramen of 0.24 mm, 0.22 mm, and 0.33 mm and 0.33 mm, 0.31 mm, and 0.42 mm in mesiobuccal, distobuccal and palatal roots in maxillary first molars, respectively[27].
Understanding the anatomical variations of the root canal system is essential to the success of endodontic treatment[28-31]. The main goal of this treatment is to prevent apical pathosis and promote healing[4]. One reason for failure is the inability to clean, negotiate, or obturate all existing root canals[32]. Root canals may not be cleaned because the dentist fails to detect their presence.
Overall, variations in the anatomy of root canals have an important role in endodontic therapy[16,29,33]. The aim of treatment is to achieve a clean root canal system and fill it in all dimensions[34]. CBCT is a powerful tool for dental anomaly diagnosis and can provide significant clues for the success of root canal therapy[35,36]. The canals of fused roots are more complex than those of separate roots, which may increase the failure rate of root canal treatment. Careful location and negotiation of the canals should be carried out for successful management. This case highlights the ultimate importance of mastering the root canal anatomy of the maxillary molars in nonsurgical endodontic therapy. CBCT can be used as an important approach for completing satisfactory and efficient root canal treatment.
This case report discusses the endodontic management of an unusual case of a maxillary first molar with three roots and five canals and highlights the role of CBCT scanning as an objective analytic tool to ascertain 1-2-1 shaped anatomic variations in the palatal root.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pameijer CH S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Bornstein MM, Wasmer J, Sendi P, Janner SF, Buser D, von Arx T. Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: a comparative radiographic analysis using limited cone beam computed tomography. J Endod. 2012;38:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Asghari V, Rahimi S, Ghasemi N, Talebzadeh B, Norlouoni A. Treatment of a Maxillary First Molar with Two Palatal Roots. Iran Endod J. 2015;10:287-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 3. | Martins JNR, Gu Y, Marques D, Francisco H, Caramês J. Differences on the Root and Root Canal Morphologies between Asian and White Ethnic Groups Analyzed by Cone-beam Computed Tomography. J Endod. 2018;44:1096-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 93] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 4. | Sert S, Bayirli GS. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod. 2004;30:391-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 349] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 5. | Sharma S, Mittal M, Passi D, Grover S. Management of a maxillary first molar having atypical anatomy of two roots diagnosed using cone beam computed tomography. J Conserv Dent. 2015;18:342-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Schryvers A, Govaerts D, Politis C, Lambrechts P. Endodontic management of a maxillary first molar with two palatal roots: A case report. Aust Endod J. 2019;45:420-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ferguson DB, Kjar KS, Hartwell GR. Three canals in the mesiobuccal root of a maxillary first molar: a case report. J Endod. 2005;31:400-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | de Almeida-Gomes F, Maniglia-Ferreira C, Carvalho de Sousa B, Alves dos Santos R. Six root canals in maxillary first molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e157-e159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Badole GP, Warhadpande MM, Shenoi PR, Lachure C, Badole SG. A rare root canal configuration of bilateral maxillary first molar with 7 root canals diagnosed using cone-beam computed tomographic scanning: a case report. J Endod. 2014;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Kottoor J, Velmurugan N, Surendran S. Endodontic management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: a case report. J Endod. 2011;37:715-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Shin Y, Kim Y, Roh BD. Maxillary first molar with an O-shaped root morphology: report of a case. Int J Oral Sci. 2013;5:242-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006;39:921-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 674] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 13. | Smadi L, Khraisat A. Detection of a second mesiobuccal canal in the mesiobuccal roots of maxillary first molar teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e77-e81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Kottoor J, Velmurugan N, Sudha R, Hemamalathi S. Maxillary first molar with seven root canals diagnosed with cone-beam computed tomography scanning: a case report. J Endod. 2010;36:915-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Lee JH, Kim KD, Lee JK, Park W, Jeong JS, Lee Y, Gu Y, Chang SW, Son WJ, Lee WC, Baek SH, Bae KS, Kum KY. Mesiobuccal root canal anatomy of Korean maxillary first and second molars by cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Kulild JC, Peters DD. Incidence and configuration of canal systems in the mesiobuccal root of maxillary first and second molars. J Endod. 1990;16:311-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 179] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 17. | Vitalis A, Lip GY, Kay M, Vohra RK, Shantsila A. Ethnic differences in the prevalence of peripheral arterial disease: a systematic review and meta-analysis. Expert Rev Cardiovasc Ther. 2017;15:327-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Briseño-Marroquín B, Paqué F, Maier K, Willershausen B, Wolf TG. Root Canal Morphology and Configuration of 179 Maxillary First Molars by Means of Micro-computed Tomography: An Ex Vivo Study. J Endod. 2015;41:2008-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (1)] |
| 19. | al Shalabi RM, Omer OE, Glennon J, Jennings M, Claffey NM. Root canal anatomy of maxillary first and second permanent molars. Int Endod J. 2000;33:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Pérez-Heredia M, Ferrer-Luque CM, Bravo M, Castelo-Baz P, Ruíz-Piñón M, Baca P. Cone-beam Computed Tomographic Study of Root Anatomy and Canal Configuration of Molars in a Spanish Population. J Endod. 2017;43:1511-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Plotino G, Tocci L, Grande NM, Testarelli L, Messineo D, Ciotti M, Glassman G, D'ambrosio F, Gambarini G. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: a cone-beam computed tomography study in vivo. J Endod. 2013;39:1545-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 22. | Tzeng LT, Chang MC, Chang SH, Huang CC, Chen YJ, Jeng JH. Analysis of root canal system of maxillary first and second molars and their correlations by cone beam computed tomography. J Formos Med Assoc. 2020;119:968-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Silva EJ, Nejaim Y, Silva AI, Haiter-Neto F, Zaia AA, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod. 2014;40:173-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 24. | Tian XM, Yang XW, Qian L, Wei B, Gong Y. Analysis of the Root and Canal Morphologies in Maxillary First and Second Molars in a Chinese Population Using Cone-beam Computed Tomography. J Endod. 2016;42:696-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | Zhang R, Yang H, Yu X, Wang H, Hu T, Dummer PM. Use of CBCT to identify the morphology of maxillary permanent molar teeth in a Chinese subpopulation. Int Endod J. 2011;44:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 26. | Wasti F, Shearer AC, Wilson NH. Root canal systems of the mandibular and maxillary first permanent molar teeth of south Asian Pakistanis. Int Endod J. 2001;34:263-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Wolf TG, Paqué F, Sven Patyna M, Willershausen B, Briseño-Marroquín B. Three-dimensional analysis of the physiological foramen geometry of maxillary and mandibular molars by means of micro-CT. Int J Oral Sci. 2017;9:151-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Kottoor J, Hemamalathi S, Sudha R, Velmurugan N. Maxillary second molar with 5 roots and 5 canals evaluated using cone beam computerized tomography: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e162-e165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Pasternak Júnior B, Teixeira CS, Silva RG, Vansan LP, Sousa Neto MD. Treatment of a second maxillary molar with six canals. Aust Endod J. 2007;33:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Albuquerque DV, Kottoor J, Dham S, Velmurugan N, Abarajithan M, Sudha R. Endodontic management of maxillary permanent first molar with 6 root canals: 3 case reports. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e79-e83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Ahmad IA, Al-Jadaa A. Three root canals in the mesiobuccal root of maxillary molars: case reports and literature review. J Endod. 2014;40:2087-2094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | Thomas RP, Moule AJ, Bryant R. Root canal morphology of maxillary permanent first molar teeth at various ages. Int Endod J. 1993;26:257-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 87] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | Liu J, Que KH, Xiao ZH, Wen W. Endodontic management of the maxillary first molars with two root canals: A case report and review of the literature. World J Clin Cases. 2019;7:79-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Marceliano-Alves M, Alves FR, Mendes Dde M, Provenzano JC. Micro-Computed Tomography Analysis of the Root Canal Morphology of Palatal Roots of Maxillary First Molars. J Endod. 2016;42:280-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Kim SY, Choi SC, Chung YJ. Management of the fused permanent upper lateral incisor: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:649-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Rodrigues E, Braitt AH, Galvão BF, da Silva EJ. Maxillary first molar with 7 root canals diagnosed using cone-beam computed tomography. Restor Dent Endod. 2017;42:60-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |