Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.1973
Peer-review started: February 5, 2020
First decision: March 18, 2020
Revised: April 3, 2020
Accepted: April 21, 2020
Article in press: April 21, 2020
Published online: May 26, 2020
Processing time: 110 Days and 7.2 Hours
Lymphangioma is a rare benign cystic tumor believed to be a proliferation of heterotopic lymphocytes. It is caused by congenital lymphatic dysplasia or other acquired factors related to surgery, trauma, infection, or cancer. In this article, we present the case of an adult patient who underwent multi-modal imaging and whose condition was finally confirmed to be multiple cystic lymphangiomas by pathological examination.
A 61-year-old man was referred to our hospital for having suffered from painless gross hematuria for 2 wk. Multiple masses rising from the retroperitoneum and pelvis were found incidentally by urinary ultrasonography. Contrast-enhanced abdominal-pelvic computed tomography showed multiple well-defined hypodense cystic lesions without enhancement. The lesions showed no uptake on F-18-fluorodeoxyglucose positron emission tomography/computed tomography images. Exploratory laparotomy was performed, and the case was confirmed as multiple cystic lymphangiomas.
When retroperitoneal and pelvic masses are found, clinicians should always consider cystic lymphangioma when making a differential diagnosis.
Core tip: Retroperitoneal and pelvic cystic lymphangioma, which is seldom seen in adults, has only rarely been reported. It is especially not often diagnosed by F-18-fluorodeoxyglucose (F-18 FDG) positron emission tomography/computed tomography (PET/CT). In addition, the features presented by F-18 FDG PET/CT are different. We here report an adult patient who underwent F-18 FDG PET/CT and was finally diagnosed with multiple cystic lymphangiomas, with an aim of improving the understanding of the disease.
- Citation: Sun MM, Shen J. Positron emission tomography/computed tomography findings of multiple cystic lymphangiomas in an adult: A case report. World J Clin Cases 2020; 8(10): 1973-1978
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/1973.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.1973
Lymphangioma is considered a benign proliferation of heterotopic lymphocytes caused by congenital lymphatic dysplasia or other acquired factors[1]. It is mostly found in the cervicofacial and axillary regions (95%) or in the thoracic, abdominal, or mesenteric region. However, it is seldom seen in the retroperitoneum or pelvic region[2,3]. It can be classified into three types based on its microscopic features: Simple, cavernous, and cystic[4]. Cystic lymphangioma, earlier referred to as hygroma, generally presents as a single multilocular mass and multiple cystic lymphangiomas are quite uncommon. The symptoms of cystic lymphangioma are nonspecific. This depends on the size, location, and the presence of complications. It occurs at an average age of 2 years. Cystic lymphangioma that can cause severe symptoms is seldom seen in adults. Ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI) are widely used. However, the diagnosis of lymphangioma by F-18-fluorodeoxyglucose (F-18 FDG) positron emission tomography/computed tomography (PET/CT) has not been explored in great detail, and the presentations are different. In this article, we present the case of an adult patient who underwent multi-modal imaging. The masses showed neither enhancement on CT nor uptake on fused PET/CT images. Differentiating these results from other retroperitoneal and pelvic tumors is difficult. This disease can only be identified essentially by putting the tissue under a microscope, and immunochemistry can be helpful in the further diagnosis. This patient was finally confirmed to have multiple cystic lymphangiomas by pathological examination.
A 61-year old man was referred to our hospital for having suffered from painless gross hematuria for 2 wk.
The patient had a history of hypertension going back more than 10 years. He had not undergone systematic treatment.
The patient had no special personal or family history.
The patient’s temperature was 35.6 °C, heart rate was 80 bpm, respiratory rate was 20 breaths per minute, and blood pressure was 121/74 mmHg. The clinical urological examination showed no abnormalities.
Routine blood examination, C reaction protein test, routine stool examination, and liver and kidney function were normal. Routine urine examination showed that the urine occult blood test was positive (+++). Neoplastic markers (CA153, CA199, CEA, AFP, NSE, and CA125) were negative (Table 1).
| Item | Data | Normal range |
| CA724 | < 1.5 U/mL | 0-6.9 |
| CEA | 1.72 ng/mL | 0-5.0 |
| AFP | 3.53 ng/mL | 0-7.0 |
| CYFRA | 2.61 ng/mL | 0-3.3 |
| NSE | 6.6 ng/mL | 0-16.3 |
| CA199 | 8.0 U/mL | 0-30 |
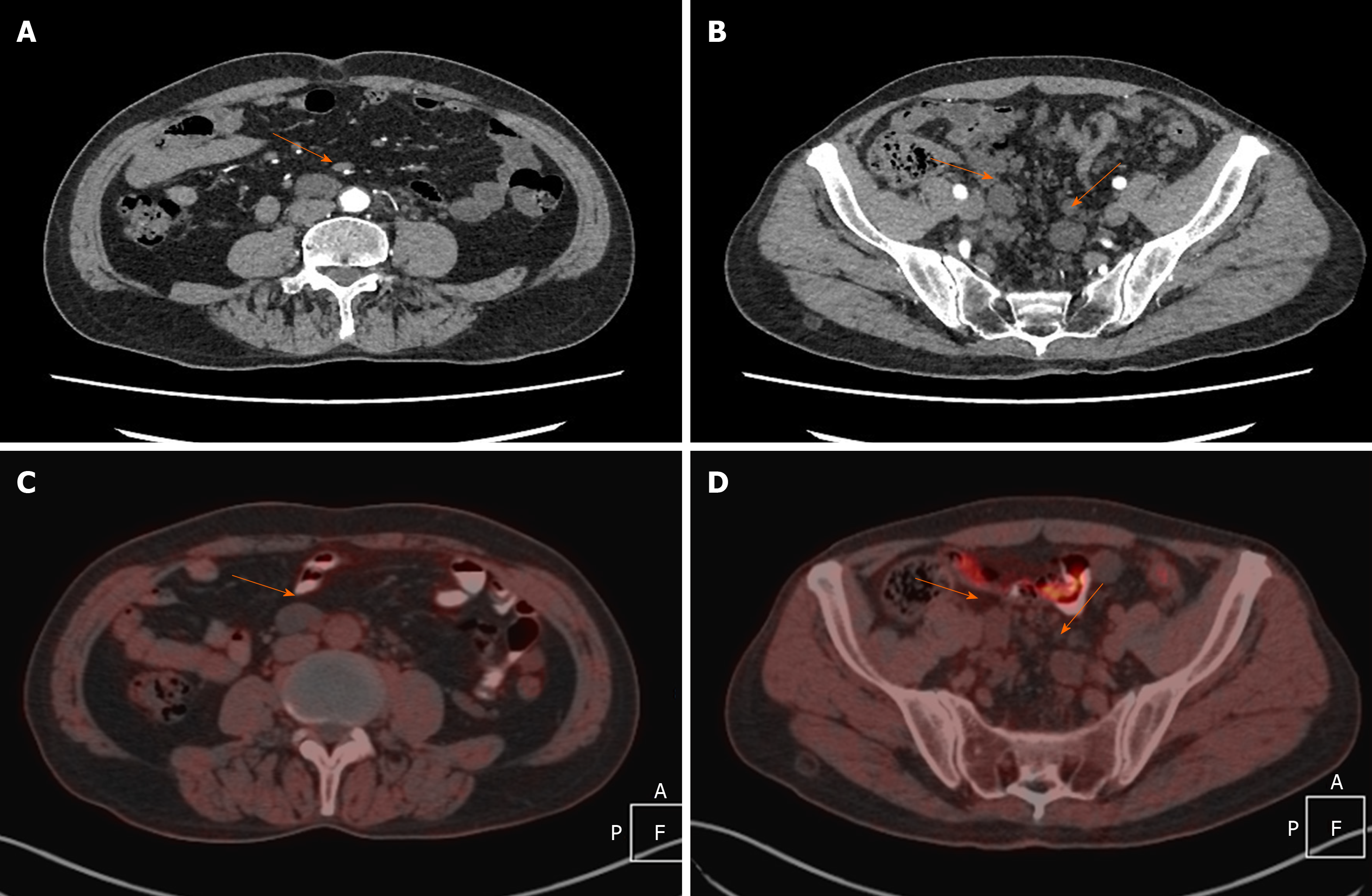
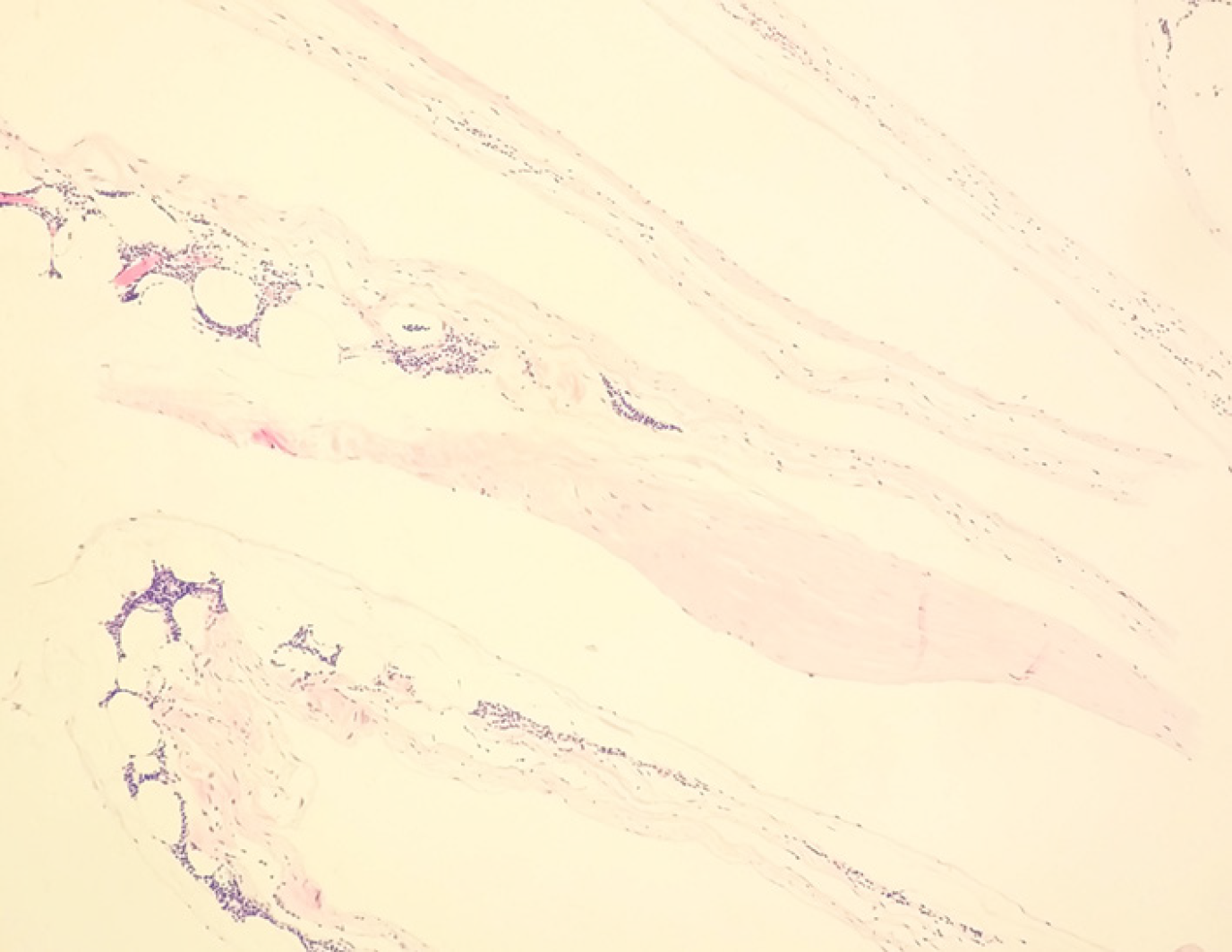
The patient was investigated by urinary ultrasonography initially, which showed ureteral calculus at the distal end of the right ureter. Besides, multiple masses rising from the retroperitoneum and pelvis were found incidentally. In order to identify the reason of hematuria as well as define the character of the tumor, contrast–enhanced CT was performed. The contrast-enhanced abdominal-pelvic CT revealed multiple well-defined hypodense cystic lesions arising from retroperitoneum and pelvic space without enhancement (Figure 1A and B). The lesions grew along the peritoneal interstitial space, the pelvic wall, and external iliac vascular deformation area, some of which showed shaping and suture-like changes. The largest one was 3.3 cm × 2.5 cm. Thus, a provisional diagnosis of multiple retroperitoneum and pelvic masses (the possibility of a malignancy cannot be ruled out) was made. To make a systematic evaluation of the general condition and a further diagnosis of the disease, F-18 FDG PET/CT was performed 1 h after injection of (10 mCi) 370 MBq of F-18 FDG. No uptake by the masses was observed on fused PET/CT images (Figure 1C and D). Combining the feature of morphology and the result of no F-18 FDG uptake, the conclusion of benign tumor was made. The ureteroscopic lithotripsy as well as exploratory laparotomy was performed at last. The stone was removed, and some of the tumor tissues were prepared into pathological sections where fibrous cystic wall-like tissues were observed under an optical microscope, with proliferated lymphoid tissue inside (Figure 2).
These findings confirmed the lesions to be multiple cystic lymphangiomas.
Based on the pathological examination, the lesions were confirmed to be cystic lymphangiomas (Figure 2). The patient declined complete excision and was discharged after conservative treatment.
Lymphangioma is a rare benign cystic tumor which is rarely reported in adults. The disease is a benign proliferation of heterotopic lymphocytes due to congenital lymphatic dysplasia or other acquired factors[1]. It is mostly found in the cervicofacial and axillary regions (95%) or in the thoracic, abdominal, or mesenteric region, but it is seldom seen in the retroperitoneum or pelvic region[2,3]. This disease can only be identified essentially by putting the tissue under a microscope. Histologically, it can be classified into three types based on its microscopic features: Simple, cavernous, and cystic[4]. Cystic lymphangioma, earlier referred to as hygroma, generally presents as a single multilocular mass. Multiple masses, presenting as our case, are quite uncommon. Immunohistochemistry can be helpful in the further diagnosis. The lymphatic endothelium, which adheres to the lymphatic tissue, could have a positive immunoreaction for the D2-40[5].
The clinical manifestations are usually nonspecific. They depend on the size, location, and the presence of complications. Progressive abdominal swelling and stomachache can occur if the mass originates from the retroperitoneum where histology is characterized by loose tissue and the tumor can grow unrestrictedly. The presence of acute symptoms is of significant importance when lymphangioma is associated with intestinal obstruction, infection, bleeding, and tumor torsion[6,7]. It usually occurs when the patient is 2 years old, and the type that can cause severe symptoms is seldom seen in adults.
US is usually regarded as the first choice among imaging modalities for examination. Typical features appear as fluid-filled cystic structure, with or without thin septa inside. Color Doppler US may show inner vascularity in the septa when infection occurs simultaneously[8]. A craniocaudal sliding movement, associated with the patient’s respiration, could be a specific feature of mesenteric lymphangioma[9]. CT mainly shows a single or multiple well-circumscribed cystic lesions whose attenuation value ranges from fat density (chyle) to liquid density. The septation could be inconspicuous if the lesion is not large enough. Retroperitoneal lymphangiomas usually present as large, slender lesions that span the adjacent organs[10,11]. The one occurring in the pelvic cavity is characterized by the presence of external iliac vessels along the pelvic wall[12]. However, the blood supply in the wall and septa of the lesion can be significantly increased in response to secondary infection, which appears as enhancement of the wall at a different level[13,14]. This can be a special sign for the diagnosis of cystic lymphangioma. In our case, CT showed multiple fluid-filled cystic lesions without septa. The lesions grew along the peritoneal interstitial space, the pelvic wall, and external iliac vascular deformation area with a clear boundary, some of which showed shaping and suture-like changes. The lesions and the wall were proved to be inhomogeneously enhanced on enhanced CT. MRI is an essential means of differentiating lymphangioma from other cystic lesions due to its excellent spatial resolution. Cystic lymphangioma typically shows a low signal in T1-weighted MR images and a high signal in T2-weighted MR images. However, the signal could be different if the ratio of the component within the cyst changes. Chemically selective fat-saturated and chemical shift MR images can show the fat content clearly, which cannot be found by CT and thus provide more useful information for diagnosis of the disease[15,16]. It is generally acknowledged that PET-CT is an effective means of discriminating between benign and malignant lesions. The use of an F-18 FDG PET/CT procedure in the diagnosis of lymphangioma has only rarely been reported, and the presentations are not common. Some patients have shown lymphangioma with mildly increased F-18 FDG uptake with an SUVmax of 3-3.8, mimicking a malignancy[17-20]. The results have shown that although lymphangioma is benign, it can still present as high-FDG-uptake lesions, which might be caused by lymphocytes and fluid joining the dilated lymphatic vessels. However, there are some reported cases[21,22] of lymphangioma without FDG uptake that are similar to what we found. This may be related to the absence of infection or granuloma formation[23,24]. In addition, 68Ga-NEB PET-CT and PET-MRI are also applied to evaluate lymphangioma in some research[22,25]. The novel radiotracer 68Ga-NEB is active in abnormal lymphoid tissue, which can provide more useful information for clinicians. Invasive examination such as cyst fluid fine-needle aspiration is also helpful in the differential diagnosis of benign and malignant tumors by analyzing cytological features and chemical composition[26,27].
Surgical resection is the most effective treatment for lymphangioma. However, it is reported that the recurrence rates of complete and incomplete resection are 12% and 53%, respectively. About 10% of asymptomatic patients show the phenomenon of pathological self-absorption[28]. A high complication rate and the possibility of incomplete excision also make patients wish to postpone treatment[29]. Noninvasive treatments, such as sclerotherapy, oral therapy, laser therapy, and radiofrequency ablation, are also confirmed to be effective and successful[30,31].
To our knowledge, this is the first report in the literature of findings of retroperitoneal and pelvic multiple cystic lymphangioma in an adult without 18-F FDG uptake by PET-CT. When retroperitoneal masses are found, clinicians should always consider cystic lymphangioma when performing a differential diagnosis.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Branch Association of Nuclear Medicine, Chinese Medical Association.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maurea S, Nag DS S-Editor: Ma YJ L-Editor: Wang TQ E-Editor: Qi LL
| 1. | Chung JC, Song OP. Cystic lymphangioma of the jejunal mesentery presenting with acute abdomen in an adult. Can J Surg. 2009;52:E286-E288. [PubMed] [DOI] [Full Text] |
| 2. | Torashima Y, Yamaguchi J, Taniguchi K, Fujioka H, Shimokawa I, Izawa K, Kanematsu T. Surgery for ileal mesenteric lymphangioma during pregnancy: case report and review of the literature. J Gastrointest Surg. 2004;8:616-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Nishino M, Hayakawa K, Minami M, Yamamoto A, Ueda H, Takasu K. Primary retroperitoneal neoplasms: CT and MR imaging findings with anatomic and pathologic diagnostic clues. Radiographics. 2003;23:45-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 163] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Rossi G, Iannicelli E, Almberger M, Innocenzi D, David V. Cystic lymphangioma of the upper extremity: US and MRI correlation (2004:11b). Eur Radiol. 2005;15:400-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Hanganu E, Gavrilescu SL, Trandafirescu MF, Chiforeanu AM, Mihăilă D, Florea ID, Anton-Păduraru DT, Burlea M. A histopathological diagnosis of mesenteric cystic lymphangioma, clinically misdiagnosed as simple mesenteric cyst - case report. Rom J Morphol Embryol. 2017;58:1525-1530. [PubMed] |
| 6. | Méndez-Gallart R, Solar-Boga A, Gómez-Tellado M, Somoza-Argibay I. Giant mesenteric cystic lymphangioma in an infant presenting with acute bowel obstruction. Can J Surg. 2009;52:E42-E43. [PubMed] |
| 7. | Tomsett AL, Addison RE, Hopkins JC, Courtney ED. Small intestinal and mesenteric lymphangioma in an adult: a rare cause of acute abdominal pain. Br J Hosp Med (Lond). 2016;77:603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 242] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 9. | Park SH, Moon SK, Sung JY. Sonographic findings in a case of scrotal lymphangioma. J Clin Ultrasound. 2014;42:234-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Naganuma H, Ishida H, Komatsuda T, Hakamada M, Sawada T, Satoyoshi R, Enomoto K, Miyauchi T. Sonographic findings in two cases of lymphangioma of the mesocolon in adults. J Clin Ultrasound. 2018;46:78-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Levy AD, Cantisani V, Miettinen M. Abdominal lymphangiomas: imaging features with pathologic correlation. AJR Am J Roentgenol. 2004;182:1485-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Wang H, Shen A, Duan S. CT and MRI diagnosis of postoperative pelvic lymphocyst in patients with gynecologic carcinoma. Yixue Yingxiangxue Zazhi. 2013;23:1272-1275. [DOI] [Full Text] |
| 13. | Katı Ö, Güngör Ş, Kandur Y. Mesenteric cystic lymphangioma. J Pediatr Surg Case Rep. 2018;35:26-28. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Jun BR, Yong HS, Kang EY, Woo OH, Choi EJ. 64-slice coronary computed tomography angiography using low tube voltage of 80 kV in subjects with normal body mass indices: comparative study using 120 kV. Acta Radiol. 2012;53:1099-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Yoo E, Kim MJ, Kim KW, Chung JJ, Kim SH, Choi JY. A case of mesenteric cystic lymphangioma: fat saturation and chemical shift MR imaging. J Magn Reson Imaging. 2006;23:77-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Ayyappan AP, Jhaveri KS, Haider MA. Radiological assessment of mesenteric and retroperitoneal cysts in adults: is there a role for chemical shift MRI? Clin Imaging. 2011;35:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Ji T, Kuang A. 18F-FDG PET/CT Findings in a Splenic Lymphangioma. Clin Nucl Med. 2015;40:e375-e377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Kwon SD, Chun KA, Kong EJ, Cho IH. Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography Findings of Post Traumatic Lymphangioma in a Young Adult Male. Vasc Specialist Int. 2016;32:137-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Dong A, Wang Y, Zuo C. F-18 FDG uptake in a retroperitoneal cystic lymphangioma mimicking malignancy. Clin Nucl Med. 2012;37:e154-e156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Wang X, Zhang J, Wang Y, Ding Q, Wang J. Imaging features of abdominal non-organi lymphangioma. Zhonghua Xiaohua Waike Zazhi. 2017;16:752-758. [DOI] [Full Text] |
| 21. | Hwang SS, Choi HJ, Park SY. Cavernous mesenteric lymphangiomatosis mimicking metastasis in a patient with rectal cancer: a case report. World J Gastroenterol. 2009;15:3947-3949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Hou G, Hou B, Jiang Y, Zhu Z, Long X, Chen X, Cheng W. 68Ga-NOTA-Evans Blue TOF PET/MR Lymphoscintigraphy Evaluation of the Severity of Lower Limb Lymphedema. Clin Nucl Med. 2019;44:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Zhang W, Yin J, Wang X, Zhang J, Li X, Ouyang X. 18F-FDG PET / CT findings in a small intestinal cavernous lymphangioma. Zhonghua Heyixue Yu Fenzi Yingxiang Zazhi. 2010;30:188. [DOI] [Full Text] |
| 24. | Eghtedari M, Sicklick J, Kono Y, Peterson MR, Santillan CS. Unusual imaging profile of a solitary splenic lymphangioma. Acta Radiol Short Rep. 2012;1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Zhang W, Wu P, Li F, Tong G, Chen X, Zhu Z. Potential Applications of Using 68Ga-Evans Blue PET/CT in the Evaluation of Lymphatic Disorder: Preliminary Observations. Clin Nucl Med. 2016;41:302-308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | DI Marco M, Grassi E, Vecchiarelli S, Durante S, Macchini M, Biasco G. Retroperitoneal lymphangioma: A report of 2 cases and a review of the literature regarding the differential diagnoses of retroperitoneal cystic masses. Oncol Lett. 2016;11:3161-3166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Abdelkader A, Hunt B, Hartley CP, Panarelli NC, Giorgadze T. Cystic Lesions of the Pancreas: Differential Diagnosis and Cytologic-Histologic Correlation. Arch Pathol Lab Med. 2020;144:47-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (1)] |
| 28. | Sah S, Nawal S, Gupta R, Kafle S. Benign cystic lymphangioma of sigmoid mesocolon presenting as abdominal catastrophe: an extremely rare entity. Health Renaissance. 2014;12:130-132. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Perkins JA, Manning SC, Tempero RM, Cunningham MJ, Edmonds JL, Hoffer FA, Egbert MA. Lymphatic malformations: review of current treatment. Otolaryngol Head Neck Surg. 2010;142:795-803, 803.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 148] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 30. | Amodeo I, Colnaghi M, Raffaeli G, Cavallaro G, Ciralli F, Gangi S, Leva E, Pignataro L, Borzani I, Pugni L, Mosca F. The use of sirolimus in the treatment of giant cystic lymphangioma: Four case reports and update of medical therapy. Medicine (Baltimore). 2017;96:e8871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Amodeo I, Cavallaro G, Raffaeli G, Colombo L, Fumagalli M, Cavalli R, Leva E, Mosca F. Abdominal cystic lymphangioma in a term newborn: A case report and update of new treatments. Medicine (Baltimore). 2017;96:e5984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |