Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.1832
Peer-review started: February 6, 2020
First decision: February 26, 2020
Revised: April 1, 2020
Accepted: April 21, 2020
Article in press: April 21, 2020
Published online: May 26, 2020
Processing time: 109 Days and 0.2 Hours
Facial defect coverage is a common subject in the field of reconstructive surgery. There are many methods for facial defect reconstruction, and reconstructive surgeons should choose the most appropriate method on a case-by-case basis to achieve both functional and aesthetic improvement. Among various options for facial reconstruction, the local flap technique is considered the best reconstructive modality to provide good tissue matches of color and texture, which is consistent with the ideal goal of reconstruction (replacement of like-with-like). Keystone design perforator island flap (KDPIF), devised by Behan in 2003, has been applied to various fields of reconstructive surgery in the past decade due to its design simplicity, robust vascular supply, and reproducibility. Several studies have reported KDPIF reconstruction of facial defects, such as large parotid defects, small-to-moderate nasal defects, and eyelid defects. However, KDPIF has been used relatively less in facial defects than in other body regions, such as the trunk and extremities. The purpose of this review is to provide an organized overview of facial KDPIF reconstruction including the classification of KDPIF, modifications, physiology, mechanism of flap movement, consideration of facial relaxed skin tension lines and aesthetics, surgical techniques, clinical applications, and precautions for successful execution of KDPIF reconstruction.
Core tip: To obtain improved aesthetic and functional results in facial reconstruction using local flaps, facial relaxed skin tension lines and facial aesthetic unit principles should both be considered. In this article, we review the keystone perforator island flap, which is a simple and easy local flap technique, and investigate facial keystone perforator island flap reconstruction, taking into account both facial relaxed skin tension lines and facial aesthetic subunits, which can achieve promising results and ideal outcomes without difficulty in covering facial defects in both central and peripheral facial units.
- Citation: Lim SY, Yoon CS, Lee HG, Kim KN. Keystone design perforator island flap in facial defect reconstruction. World J Clin Cases 2020; 8(10): 1832-1847
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/1832.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.1832
Facial defects are usually encountered in the field of reconstructive surgery[1]. Even though facial defects are rarely life-threatening and defect sizes are not extensive, reconstruction can be complex and significantly impact a patient’s face both functionally and aesthetically[2]. Reconstruction of facial defects has two main objectives: it should correct dysfunctions and restore or improve the aesthetics of the face. Operations to maintain or improve function are not feasible without incisions and the subsequent formation of scars. Function and aesthetics can sometimes contradict each another in reconstructive plastic surgery. Therefore, facial reconstructive surgery requires experience, detailed knowledge, and careful planning to achieve the intended improvement of function with a minimal loss of aesthetics. Obviously, aesthetics play an essential role, especially when the face is involved. Various reconstructive methods for facial defect coverage, such as skin grafts, local flaps, and free flaps, have been developed, and each technique has certain advantages and disadvantages[1]. Thus, reconstructive surgeons should choose the appropriate method on a case-by-case basis[3]. Skin grafts, especially full-thickness skin grafts, can be restrictively indicated for partial thickness facial defects with intact underlying musculatures[1]. Free flaps can be a good reconstructive modality for larger facial defects[1]; however, both skin grafts and free flaps may lead to mismatches of color and texture, and donor site morbidities[1,3]. Furthermore, free flaps may reflect overtreatment for smaller facial defects[1], and can be limited by the lack of skilled microsurgery experts and the inability of centers to perform microsurgical operations[3].
Local flaps have been considered as the best reconstructive modality for small-to-moderate-sized facial defects because they provide good tissue matches of color and texture, which is consistent with the ideal goal of reconstruction (replacement of like-with-like)[1]. Various local flaps, such as the rotation flap, rhomboid flap, bilobed flap, Limberg flap, V-Y advancement flap, perforator propeller flap, and perforator island flap have been used for facial defect reconstruction[1]. Among perforator flaps, the keystone design perforator island flap (KDPIF) has gained popularity in various fields of reconstructive surgery over the past decade[1,3-8]. Since Behan devised the KDPIF in 2003[4], several studies have presented KDPIF reconstruction of facial defects of various sizes and locations, which included small nasal defects to large parotid defects[6,9,10]. However, facial reconstruction using KDPIF has been reported relatively less than KDPIF reconstruction of other body regions, such as the trunk, lower extremities, and upper extremities[3,11-14]. The authors speculate that the reason for fewer reports of facial KDPIF reconstruction may result from less interest in the application of a new local flap technique as various reliable local flaps, based on the abundant vascular supply in face, have already been devised and used for a long period of time. Furthermore, many plastic and reconstructive surgeons tend to be in awe of flaps containing microsurgical techniques (microsurgical vessel anastomosis, microsurgical pedicle dissection), such as the free flap, perforator propeller flap, and perforator island flap; therefore, the KDPIF technique, which does not require a microsurgical technique, may be belittled. The lack of concern, associated apprehension, and a potential lack of knowledge may have blunted the incorporation of KDPIF in facial reconstruction[15].
In this review, we provide novice plastic and reconstructive surgeons with an in-depth perception of facial KDPIF reconstruction including the classification of KDPIF, modifications, physiology, mechanism of flap movement, consideration of the facial relaxed skin tension lines (RSTLs) and facial aesthetic unit concept, surgical techniques, clinical applications, and precautions for successful execution of KDPIF reconstruction.
The KDPIF is a curvilinear-shaped trapezoidal design flap comprising two conjoined end-to-side V-Y flaps[4]. Behan named this flap “Keystone flap” because its design resembled the architectural shape of the keystone (a way of locking the arch through gravity) in Roman arches[4]. As the keystone architecturally locks the other stones in place and allows for weight bearing, the KDPIF locks into the defect and provides structural advantages over other flap closure designs[15].
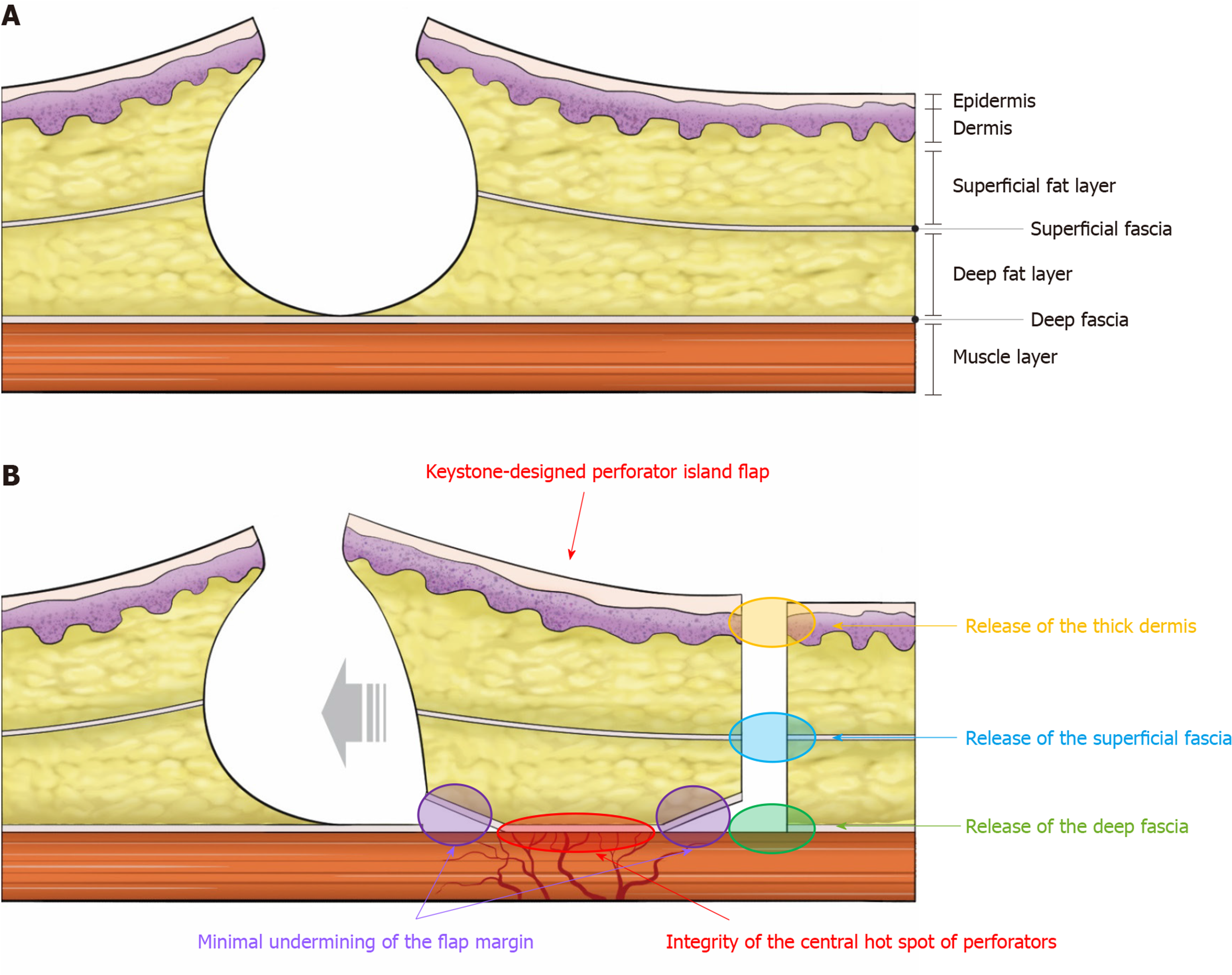
The KDPIF consists of two opposing V-Y flaps joined together[4]. The initial advancement of the V-Y at the corner of the flap towards the flap center provides some residual laxity within the flap, which allows for movement of the KDPIF in the horizontal axis into the defect[4]. The KDPIF is originally designed over dermatome segments with a flap width at a 1:1 ratio to the elliptical defect, and the limbs of the flap from the traditional design are symmetrically drawn at 90 degrees to the longitudinal axis of the defect[4]. The longitudinal axis of the flap is parallel to the defect[4]. A skin incision followed by blunt dissection of the surrounding tissues is performed to advance the flap to facilitate wound approximation[4]. Careful teasing of the circumferential tissues without any flap undermining is traditionally emphasized by Behan to preserve the integrity of perforators[4]. In addition, where possible, all subcutaneous longitudinal venous and neural structures that support the flap should be retained within the limits of the surgical procedure[4]. The deep fascia is left intact for smaller defects up to 2 cm; however, circumferential release of the deep fascia is necessary to achieve increased mobilization for larger defects[4].
There are original four subtypes of KDPIF according to Behan’s classification (Figure 1A-1E) based on the amount of tissue used, and the depth and extent of dissection: Type I (skin incision only), type II (A, division of the deep fascia along the outer curvilinear line; B, division of the deep fascia and skin graft to the secondary defect), type III (opposing keystone flaps designed to create a double-keystone flap), and type IV (keystone flap with undermining of up to 50% of the flap subfascially)[4].
There have been various modified operative techniques in KDPIF. We describe several representative modifications as follows.
First, the flap-to-defect ratio could be extended greater than 1:1 ratio (originally described by Behan) dependent on the surrounding tissue laxity (up to 5:1)[7]. Greater flap-to-defect ratios are material to defects with surrounding tissues undermined, inflamed, and irradiated to recruit well-vascularized tissue for durable and stable coverage without significant tension[7].
Second, asymmetric design of limbs and angles compared with traditional symmetric limbs drawn at 90 degrees to the longitudinal axis of the defect could be used to avoid crossing of joint lines, exposure of critical structures, and deliberate incision into lymphatic basins[7].
Third, circumferential division of the deep fascia is performed in a stepwise approach for necessary advancement[7], although Behan Type IIA KDPIF is the division of deep fascia along the outer curvilinear line. Namely, progressive release of the deep fascia could provide more flap movement and tension-less wound closure, except in Type I KDPIF.
Fourth, a certain undermining of the flap margins away from hot spots of perforators (vs originally no undermining) after teasing of the circumferential tissues could be necessary to achieve further flap movement including greater advancement, rotation, and transposition, which can provide even greater versatility of the flap[1,7,10,14]. We consider that this minimal undermining is the important concept of KDPIF in terms of adding flap movement whilst maintaining flap stability[1,10,14].
Fifth, the Ω-variant KDPIF (defect closure with fish-mouth fashion) could provide further flap movement via additional rotational movement and further tension reduction without sacrificing normal tissues in wound closure (Figure 1F)[16]. In contrast to traditional KDPIF, further undermining of the flap with preservation of the central hot spot of the perforators is necessary in this modification. Then, instead of advancing and expanding the skin paddle of the flap as in traditional KDPIF, the two apices and margins adjacent to the wound were conjoined to cover the defect[17].
Sixth, SMU (Sydney Melanoma Unit) modification involves maintenance of a skin bridge along the greater arc of the KDPIF, allowing additional vascularity, preserving subdermal lymphatics to reduce the risk of pin cushioning, and reducing time spent suturing the wounds (Figure 1G)[18].
Through these modifications, KDPIF could be more widely adopted for from smaller to larger defects in various anatomical locations.
KDPIF is basically a multi-perforator-based advancement flap based on a random pedicle arising from musculocutaneous or fasciocutaneous perforators[15]. The longitudinal axis of the flap should correspond to the maximal axiality of vascular flow and should be oriented to maximally capture the dominant perforators and linking vessels within the flap design to maximize flap perfusion[15]. Namely, the center of the flap should be located near hot spots of perforators, which can be easily identified using a hand-held ultrasound Doppler device[3,15]. Checking for hot spots with a hand-held ultrasound Doppler device is necessary for KDPIF reconstruction in upper and lower extremities[3]. However, we consider that it may not be essential to locate the perforators in KDPIF reconstruction for perforator-rich areas, such as the face, back, and buttocks, because there are enough perforators that have plenty of vascular connections resulting in reliable vascular perfusion for KDPIF reconstruction in these areas[1,14]. Of course, centering the flap over hot spots is the underlying basis of KDPIF, guaranteeing flap viability and allowing for more aggressive undermining away from the perforators when greater flap movement is necessary[15].
The flap appears hyperemic perhaps due to vasodilation after it is initially islanded[4]. It is surmised that this may be a sympathetic response and that a sympathectomy is being performed to the small vessels via blunt dissection[4]. In this regard, Behan described “the red dot sign” at a suture point where arterial blood oozed on the surface on the flap[4]. This vascular flare is seen consistently in KDPIFs in which the circulation is based on vertically-orientated perforators and dispenses with the sub-dermal plexus, which may be relative to an increase in angiogenesis in the flaps[4].
KDPIF movement is fundamentally provoked by three main factors (Figure 2)[14]. The first factor is the release of the skin layer (especially the dermis layer); the second is the release of the superficial fascia (subcutaneous tissue layer); and the last is the release of the deep fascia above the muscle layer[14]. During flap dissection, surgeons can clinically observe and feel a gradual slack in the tension surrounding the flap owing to this sequential release of the skin layer, followed by that of the superficial and deep fascia[14]. Performing minimal flap undermining of the flap margin provides additional flap movement whilst preserving the integrity of the central hot spots of the perforators[1,14].
The principle of recruitment of laxity is a crucial basis of KDPIF reconstruction, where a soft tissue defect in an area without surrounding tissue laxity is exchanged for a secondary defect in an adjacent area having sufficient laxity to enable primary closure[19]. The V-Y advancement flaps in either end of the KDPIF facilitate this recruitment of laxity, and therefore, the skin tension is redistributed perpendicular to the line of advancement[19]. In this point of view, KDPIF should be designed on the defect’s edge of greater tissue laxity, allowing distribution of the tension required for closure throughout the periphery[14].
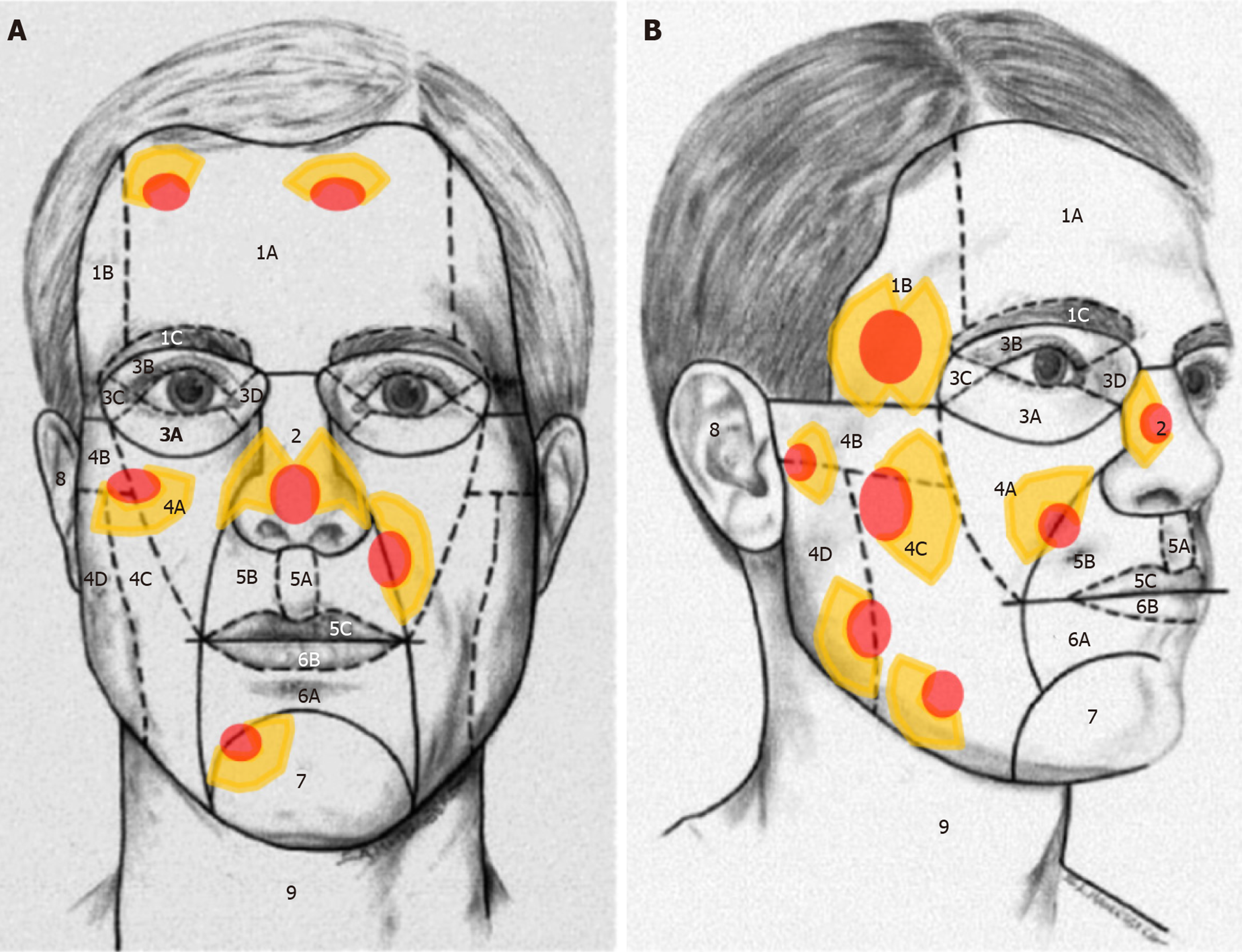
The local flap technique in facial reconstruction can readily achieve ideal reconstructive goals (replace like-with-like), as mentioned above. To obtain better aesthetic and functional results in facial reconstructions using local flaps, both facial RSTLs and facial aesthetic unit principles should be considered[1,20-22]. When designing the flaps, it is essential to respect the RSTLs and the wrinkle lines of the skin[1]. Skin incisions on the face should correspond to the direction of the RSTL to achieve less wound tension, rapid wound healing, and minimal scar formation, or follow the wrinkle lines to hide the scar within the skin crease when creases are present[1,14,21].
The facial aesthetic unit concept was first devised by Gonzales-Ulloa in 1956[23]. He described the original 14 facial aesthetic units including the forehead, right and left cheeks, nose, right and left upper lids, right and left lower lids, right and left ears, upper lip, lower lip, mental region, and neck[23]. He emphasized that superior surgical results could be obtained in complex facial reconstruction by replacing lost skin with grafts or flaps of similar histology, thickness, and texture[21,23]. To do so, surgeons should make an effort to hide the surgical margins within the natural border of each facial unit[21,23]. Menick et al[20] modified the facial aesthetic units to devise the facial subunit theory, which implied that if a suture line is matched to the shape of a particular subunit, the natural appearances of light and shadow are restored, thereby allowing the reconstruction to be imperceptible because the scars are perceived as a part of the normal facial topography.
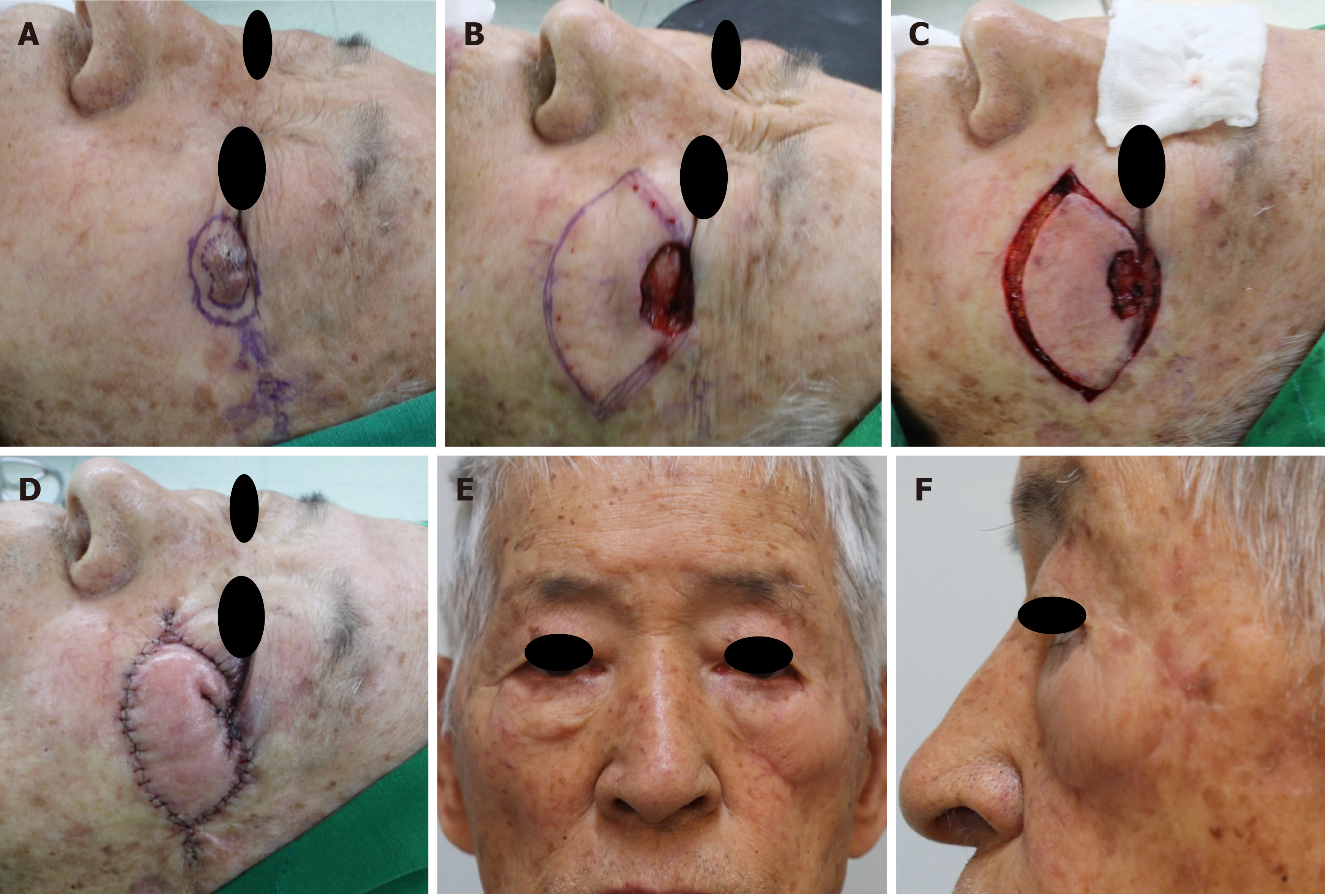
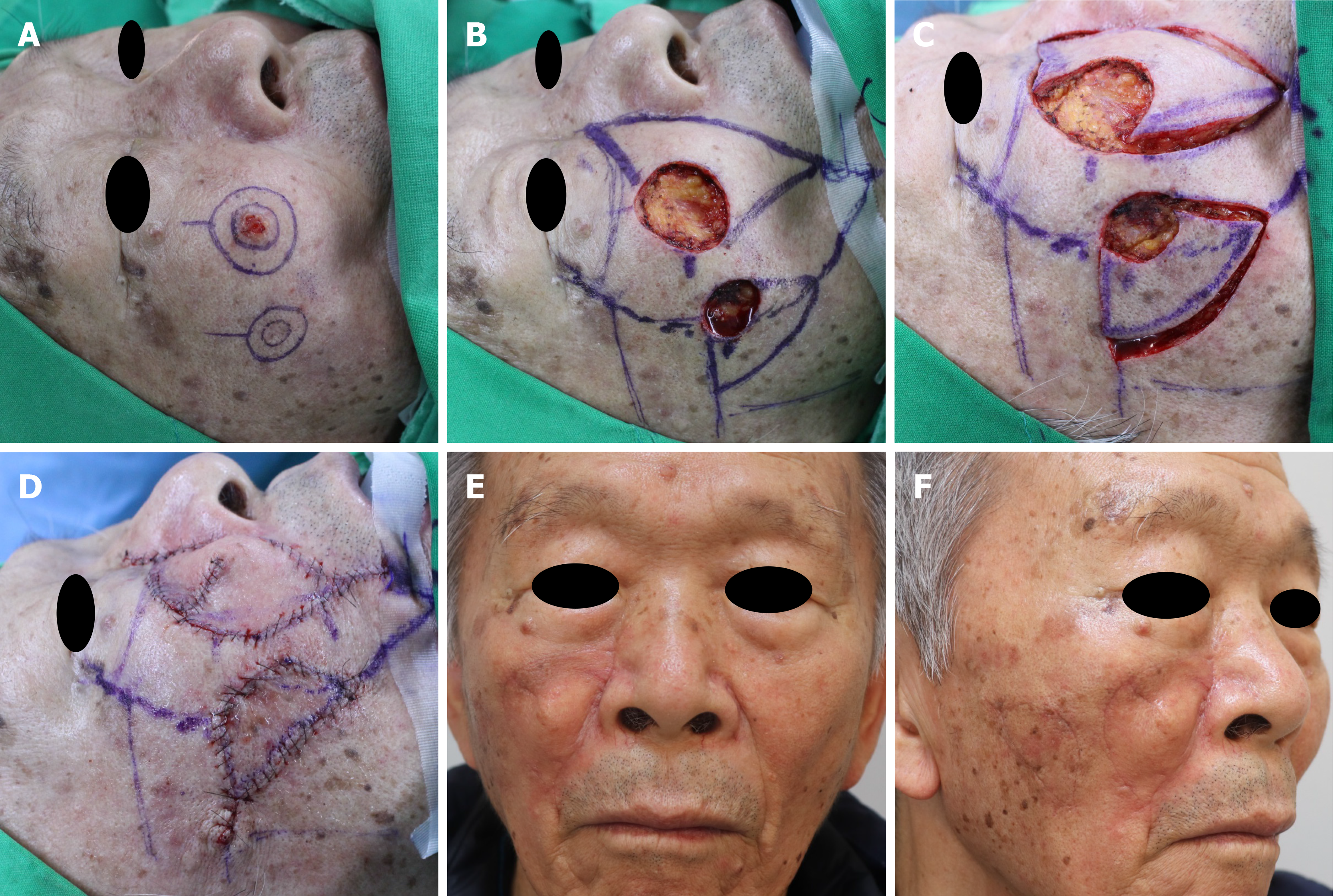
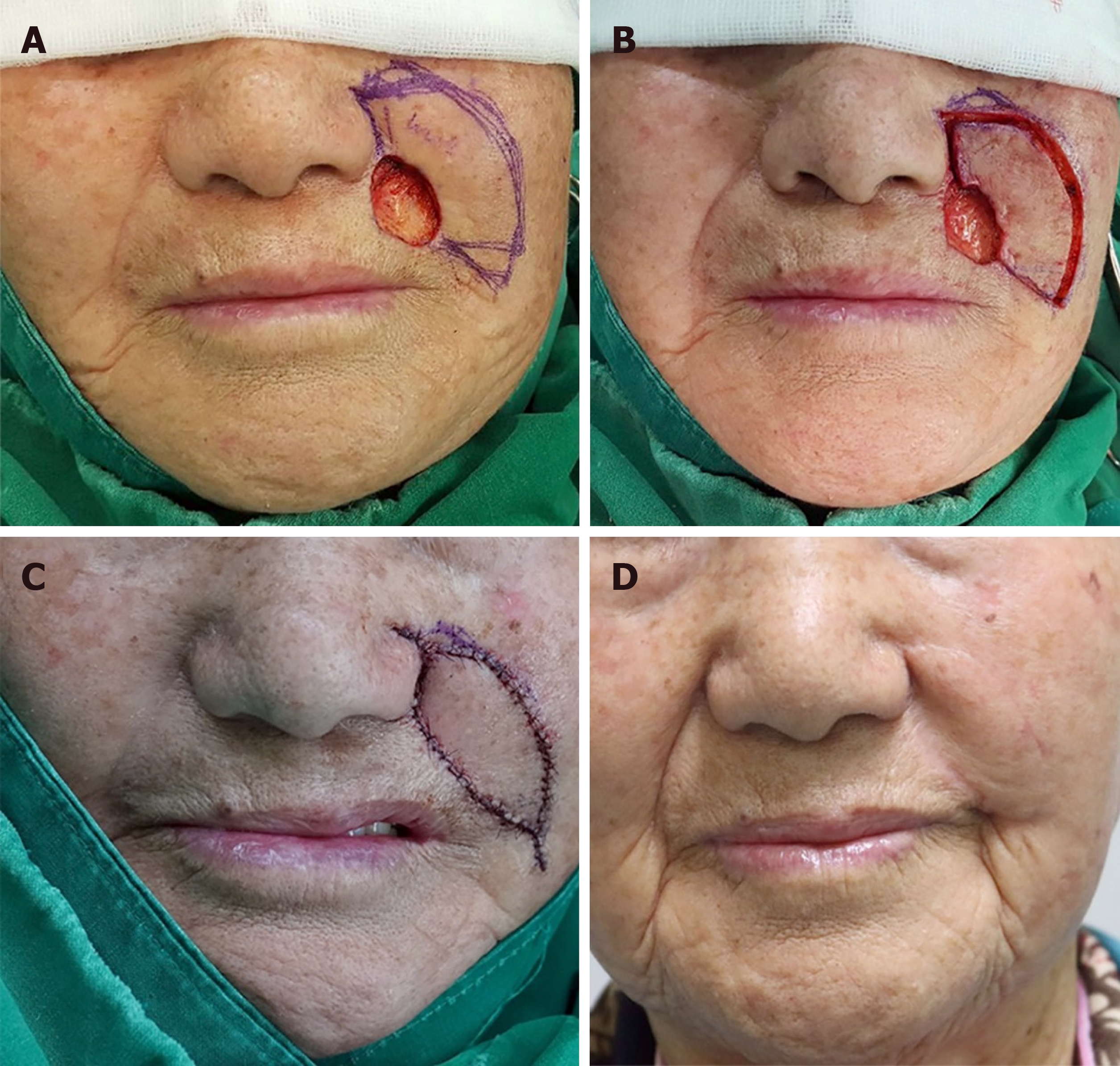
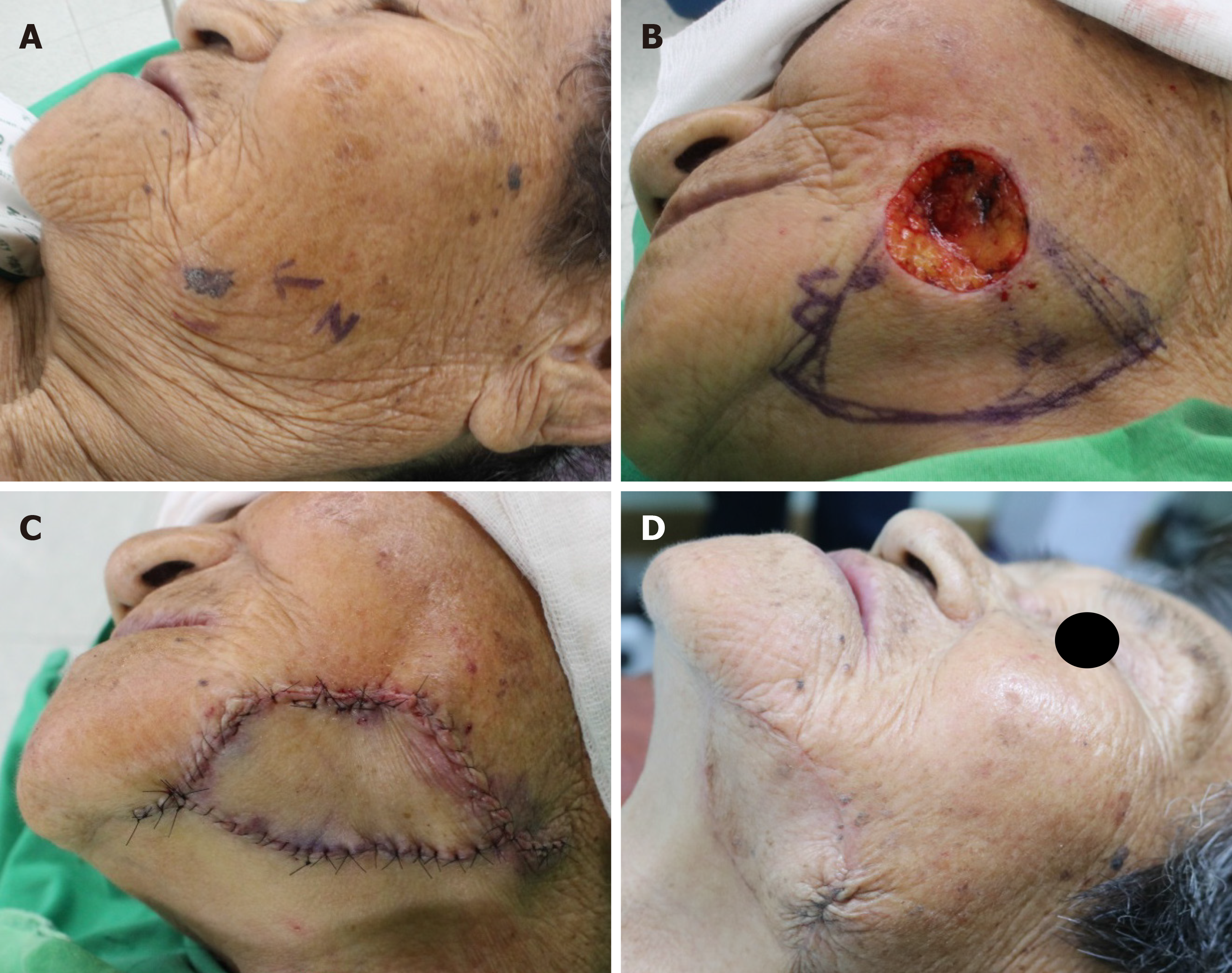
Behan presented KDPIF reconstruction in large facial defects around the parotid gland, and highlighted the KDPIF in accordance with the facial angiotome concept as a single-stage reconstructive option for covering large parotid defects[6]. Angiotome means a vascularized segment that can be extended in size by its communications with adjacent vessels with an axial input[24]. Behan demonstrated the importance of the linking vessels adjacent to the axial vascular systems in improving vascularity in island flap designs and that the axiality of flow mirrored dermatomal segments[4,24]. Although the face is one of the perforator-rich areas, as mentioned above, it is important to take the facial angiotome into account for KDPIF design in order to guarantee vascular perfusion of the flap, especially in the case of larger-sized flaps[6]. For covering small-to-moderate facial defects, surgeons should be concerned about facial RSTL and aesthetic subunits along with the facial angiotome in KDPIF reconstruction[1]. Facial aesthetic units can be divided into central facial units (nose, lips, and eyelids) and peripheral facial units (cheeks, forehead, and chin)[22]. The reconstructed requirements of the central facial units, which have complex and subtle contours and are seen in the primary gaze with their contralateral normal unit available for visual comparison, should KDPIF have the highest priority in reconstruction[22]. Previous studies have presented reconstruction in nose and medial canthal area, which emphasized consideration of the subunit principle to achieve superior aesthetic results[9,10,25]. Meanwhile, the units of the facial periphery are a lesser focus of attention, and the facial aesthetic unit principles are less appropriate in the reconstruction of these units[22]. However, our senior author (Kyu N Kim) presented the RSTL-oriented KDPIF reconstruction technique in consideration of the facial aesthetic subunit concept for covering small-to-moderate defects in both central and peripheral facial units (Figures 3 and 4)[1]. In our previous study, we mentioned that reconstructive surgeons should consider the aesthetic aspects of the peripheral facial units, which gather a smaller focus of attention and tend to be of secondary visual interests[1]. Namely, surgeons should attempt to transfer the flap to the periphery (boundary) of each facial subunit along the RSTLs as much as possible due to the off-center location of peripheral facial unit reconstruction; therefore, the scars would be concealed by the natural skin creases[1].
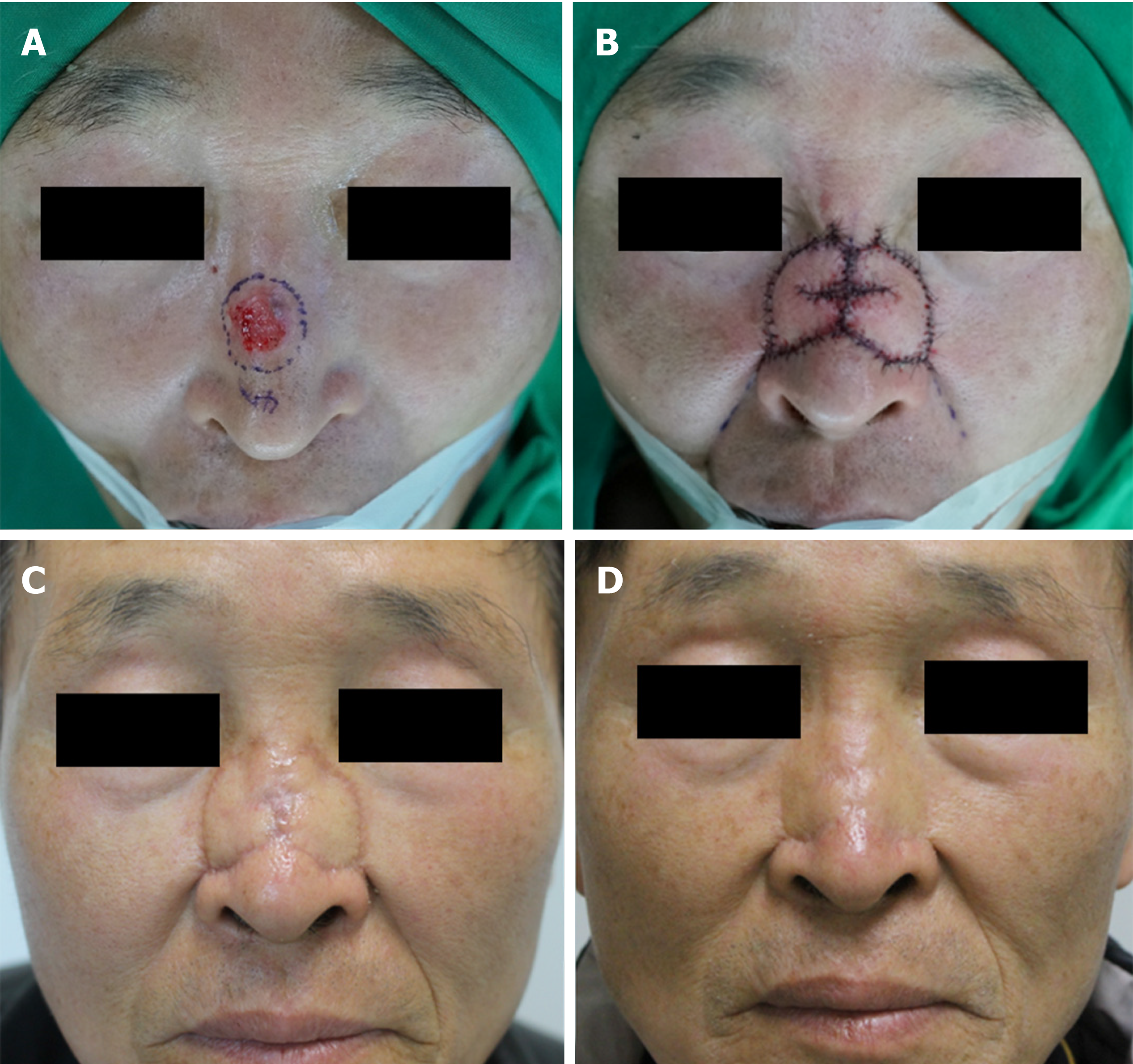
After excision or debridement of the lesion in the face, KDPIF reconstruction is performed in consideration of facial RSTLs and the facial aesthetic subunits[1]. When designing the flap in accordance with each defect, several points should be considered[1]. First, the width of the flap is designed to be larger than the width of the defect according to surrounding tissue laxity, especially in the nose, forehead, and periocular region[1]. Second, double-opposing KDPIF (Type III) is designed for larger defects that cannot be covered by single KDPIF or midline-crossing defects[1]. In this case, the width of each flap is designed to be slightly smaller than the width of the defect[1]. Third, the long axis of the flap is made as parallel to the facial RSTLs as possible to minimize wound tension and scar formation[1]. Fourth, an asymmetrical design of flap limbs and angles[7] is made along facial RSTLs or boundaries of facial aesthetic subunits as much as possible so incisions are located within and along each facial aesthetic subunit, which allows for distraction from the final postoperative scars, creating the illusion of normal skin architecture[1]. Once the skin incision is made along the flap, dissection proceeds from the subcutaneous layer to the deep fascia, which is the superficial muscular aponeurotic system layer on the face[1]. During this process, either a mono-polar or bipolar device is useful to release the fibrous septa and deep fascia until the flap can be moved freely from the surrounding tissues[1]. The surgeon determines what type and modification of KDPIF is applied intraoperatively, not preoperatively, taking laxity, elasticity, and movement of surrounding tissues into consideration. After the island-shaped flap is created, minimal undermining of the flap margin with preservation of the vascularity of the central hot spot of perforators is performed to achieve further flap movement, which may be necessary in most cases[1]. Meanwhile, during release of the fibrous septa, division of the deep fascia, and minimal undermining of the flap, the superficial veins and sensory nerves should be preserved as much as possible to maintain flap vascularity and sensation[4,15]. After meticulous hemostasis is achieved, flap inset is first performed at its central portion on the defect side, then on both ends, which are aligned in a V-Y apposition[1,4]. The donor site is closed in a primary fashion, and a mild compressive dressing is applied[1].
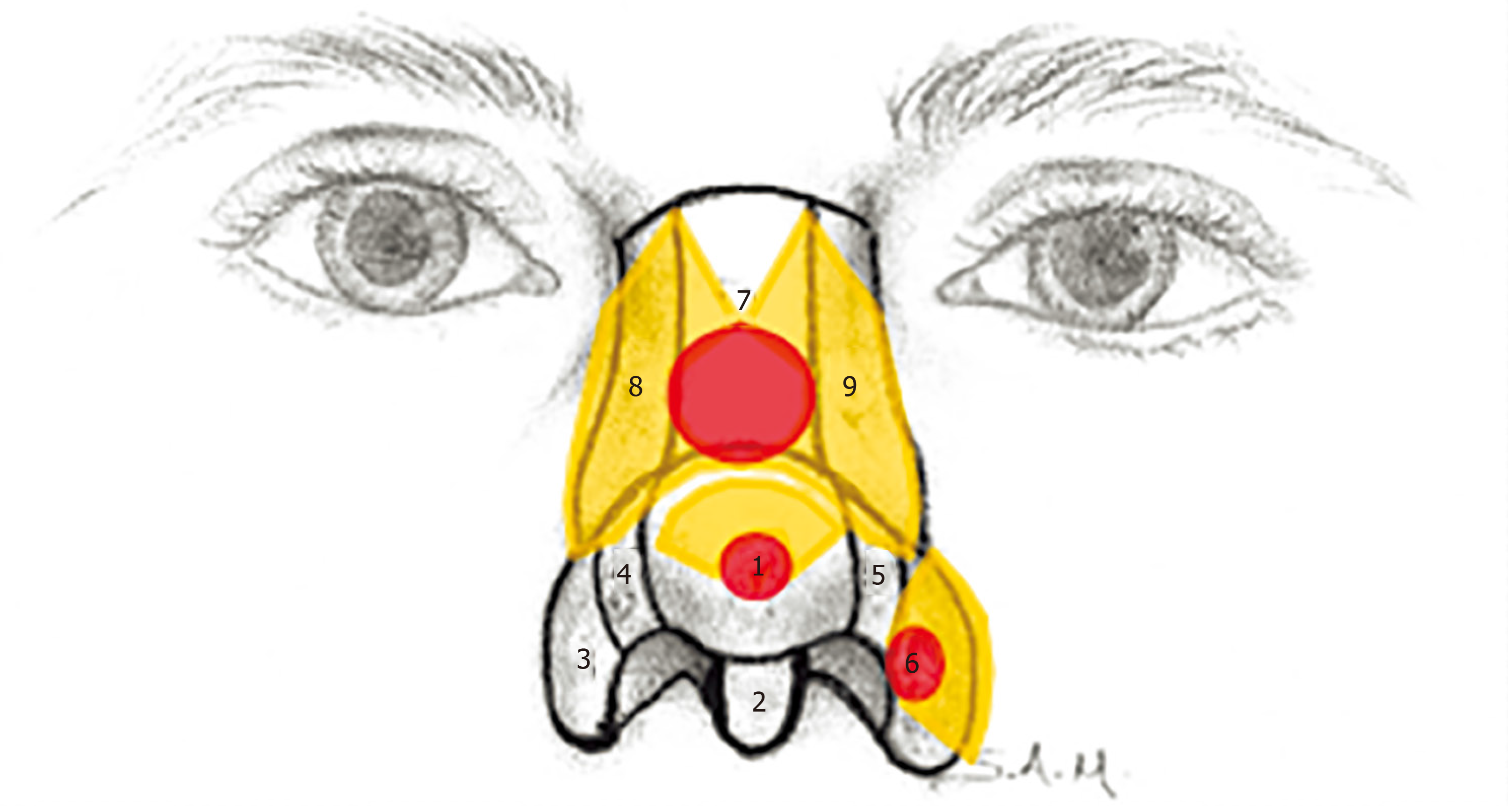
The nose is included in the central facial unit and has its own complex surface consisting of convex and concave regions[1]. In KDPIF reconstruction of nasal defects, the flaps are designed along facial RSTLs or boundaries of nasal aesthetic subunits as much as possible for incisions and final scars to be located within and along each facial aesthetic subunit, as aforementioned[1]. Kostopoulos et al[9,10] reported that KDPIF could be used to cover nasal defects up to 2 cm in diameter and partial thickness alar defects up to 1.5 cm in diameter. They used Type I KDPIF to cover nasal lateral side wall defects and Type III KDPIF to cover defects in nasal tip and dorsum[9]. Furthermore, they used Type I KDPIF to cover nasal ala defects with a diameter < 1 cm and Type IV KDPIF to cover nasal ala defects with a diameter ≥ 1 cm[10]. In addition, they did not recommend KDPIF reconstruction of nasal defects with a diameter > 2 cm due to lack of ability for flap advancement[9]. Meanwhile, our previous study presented the successful coverage of larger nasal defects up to 3 cm; we could cover a 3 cm sized defect in the dorsal subunit of the nasal unit with the Ω-variant Type III KDPIF from each dorsal side wall subunit[1]. Furthermore, we acquired further flap movement via additional rotational movement using the Ω-variant KDPIF[1]. In nasal ala defects, we consider that defects with a diameter ≥ 1.5 cm can be covered by KDPIF from other adjacent facial subunits such as the medial subunit of the cheek and the lateral subunit of the upper-lip unit. Figures 5-7 show representative cases with clinical photographs to help understand KDPIF reconstruction of nasal and ala defects, respectively.
Reconstruction of eyelid unit defects has been focused on both filling the defects and maintaining normal eyelid appearance. Loh et al[26] presented KDPIF reconstruction of the lower eyelid defects secondary to either skin cancer ablation or ectropion release. They designed the flap along the boundary of the lower-lid subunit; therefore, lateral V–Y closures aided the advancement of tissues into the defect[26]. Their technique demonstrated the recruitment of tissue laxity and the redistribution of wound tension in KDPIF reconstruction. They suggested that the KDPIF could offer the ability to preserve aesthetic subunits, hide scars in natural skin crease lines, and preserve function with preservation of local tissue, innervations, and vasculature, which are principles that are highly appropriate for lower eyelid reconstruction[26]. Kostopoulos et al[25] presented medial canthal reconstruction using a modified croissant-like KDPIF with a fibromuscular bridge of the procerus[25]. They emphasized that specific characteristics of the medial canthal area, which is located at the boundaries of different anatomic structures, involve tissues of different qualities and an inner concavity. In view of the facial aesthetic subunit concept, they covered the medial canthal subunit defect with a KDPIF from the central subunit of the forehead unit, and the dorsal side wall subunit of the nasal unit. Their technique modified the original KDPIF with a croissant-like design and addition of a fibromuscular bridge to achieve more adjustment of inner concavity in the defect and allow for better mobilization of the flap[25]. Furthermore, their final scars were almost parallel to facial RSTLs and well hidden by facial wrinkles. Based on these previous studies, KDPIF should be considered a useful option to cover eyelid unit defects[25,26]. Figures 8 and 9 show representative cases with clinical photographs to help understand the KDPIF reconstruction of eyelid unit defects.
Behan proposed that the basic overall design of any flaps seems to fit accurately within dermatomes, and recommended using dermatomes (angiotomes) as a road map in flap design because the axiality of flow mirrored the dermatomal segments[24]. He reported that larger lateral cheek, parotid, and preauricular defects could be successfully reconstructed using a Type IV KDPIF on the C2 and C3 dermatome based on the submental, posterior auricular, and occipital artery perforators[6]. Meanwhile, Behan described that smaller facial defects in the cheek, forehead, and chin could be reconstructed using KDPIFs based on trigeminal angiotomes[24]. We consider that it is possible to design the flap more freely in facial KDPIF reconstruction because the face is rich in perforators that have plenty of vascular connections, resulting in reliable vascular perfusion[1]. Thus, facial RSTLs and facial aesthetic subunits would be preferentially considered in the design of facial KDPIFs on the basis of Behan’s trigeminal angiotome concept[1]. As mentioned above, it is important to attempt to transfer the flap to boundaries of each facial subunit along the RSTLs as much as possible in the reconstruction of a peripheral facial unit defect[1]. Figures 10-13 show representative cases with clinical photographs to help understand the KDPIF reconstruction of the cheek, nasolabial fold, forehead, and chin defects, respectively.
There are some precautions to the application of the KDPIF in facial reconstruction. Care should be taken when applying the KDPIF reconstruction in areas with less skin laxity and higher tension, such as the central subunit of the forehead unit and subunit of the nasal unit, and irradiated areas[7,13,15]. In KDPIF reconstruction of these areas, it is being recommended that the flap-to-defect ratio is extended greater than 1:2, Type III KDPIF is used, and the Ω-variant KDPIF is used for achieving further flap movement and tension reduction[1,7,15].
Defects related with either traumatic wounds or wounds with an inflammatory state should be carefully applied with KDPIF reconstruction because the surrounding tissues tend to be under the zone of injury and wound healing complications occur at a higher rate[3,13-15]. Thus, wound preparation and stabilization before flap coverage is indispensable to the reconstruction of defects related with trauma and an inflammatory condition[3,14]. Wound preparation and stabilization include serial debridement of unhealthy tissues, wound dressing, and intravenous antibiotic treatment[3,14].
Using the KDPIF reconstruction, an extension of the operative scars is inevitable compared to the linear scar that occurs following primary closure with undermining or imbrication[14]. The KDPIF presents longer incisions compared to other local flaps, such as rhomboid flap and Limberg flap. Moreover, dog-ear deformity in both ends of the flap and cone deformity in the Ω-variant KDPIF can lead to complications in aesthetic perspective[27]. Therefore, a thorough explanation of the possibility of scarring should be preoperatively given to each patient to impress the necessity for prolonged postoperative scar management[14].
Although the KDPIF technique is a good modality of facial reconstruction, previous other local flap techniques can also achieve favorable results according to each circumstances; therefore, surgeons are not required to insist on performing KDPIF for facial reconstruction at all times. It is important to choose a method that can attain the best outcome for each case.
The KDPIF technique has distinct advantages, including its simple defect-adaptive design, easy reproducibility, robust vascular supply, short operative time, and minimal donor site morbidity[1,3,15]. KDPIF reconstruction in consideration of both facial RSTLs and facial aesthetic subunits can achieve promising results and ideal outcomes without difficulty in covering facial defects in both central and peripheral facial units[1].
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Member of the Korean Society of Plastic and Reconstructive Surgeons.
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Long X, Yoshimoto S S-Editor: Ma YJ L-Editor: A E-Editor: Liu MY
| 1. | Yoon CS, Kim HB, Kim YG, Kim H, Kim KN. Relaxed skin tension line–oriented keystone–designed perforator island flaps considering the facial aesthetic unit concept for the coverage of small to moderate facial defects. Medicine (Baltimore). 2019;98:e14167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Kretlow JD, McKnight AJ, Izaddoost SA. Facial soft tissue trauma. Semin Plast Surg. 2010;24:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Yoon CS, Kim SI, Kim H, Kim KN. Keystone-designed perforator island flaps for the coverage of traumatic pretibial defects in patients with comorbidities. Int J Low Extrem Wounds. 2017;16:302-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Behan FC. The keystone design perforator island flap in reconstructive surgery. ANZ J Surg. 2003;73:112-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 240] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 5. | Behan FC, Sizeland A, Glimour F, Hui A, Seel M, Lo CH. Use of the keystone island flap for advanced head and neck cancer in the elderly–a principle of amelioration. J Plast Reconstr Aesthet Surg. 2010;63:739-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Behan FC, Lo CH, Sizeland A, Pham T, Findlay M. Keystone island flap reconstruction of parotid defects. Plast Reconstr Surg. 2012;130:36e-41e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Mohan AT, Rammos CK, Akhavan AA, Martinez J, Wu PS, Moran SL, Sim FH, Behan F, Mardini S, Saint-Cyr M. Evolving concepts of keystone perforator island flaps (KPIF): principles of perforator anatomy, design modifications, and extended clinical applications. Plast Reconstr Surg. 2016;137:1909-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Abraham JT, Saint-Cyr M. Keystone and pedicle perforator flaps in reconstructive surgery: new modifications and applications. Clin Plast Surg. 2017;44:385-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Kostopoulos E, Casoli V, Agiannidis C, Konofaos P, Drimouras G, Dounavis A, Champsas G, Frangoulis M, Papadopoulos O. The keystone perforator island flap in nasal reconstruction: an alternative reconstructive option for soft tissue defects up to 2 cm. J Craniofac Surg. 2015;26:1374-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Kostopoulos E, Agiannidis C, Konofaos P, Kotsakis I, Champsas G, Frangoulis M, Papadopoulos O, Casoli V. Keystone perforator island flap as an alternative reconstructive option for partial thickness alar defects up to 1.5 centimeters. J Craniofac Surg. 2016;27:1256–1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Huang J, Yu N, Long X, Wang X. A systematic review of the keystone design perforator island flap in lower extremity defects. Medicine (Baltimore). 2017;96:e6842-6845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Khouri JS, Egeland BM, Daily SD, Harake MS, Kwon S, Neligan PC, Kuzon WM. The keystone island flap: use in large defects of the trunk and extremities in soft tissue reconstruction. Plast Reconstr Surg. 2011;127:1212-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Lanni MA, Van Kouwenberg E, Yan A, Rezak KM, Patel A. Applying the keystone design perforator island flap concept in a variety of anatomic locations: a review of 60 consecutive cases by a single surgeon. Ann Plast Surg. 2017;79:60-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Yoon CS, Kim HB, Kim YG, Kim H, Kim KN. Keystone-design perforator island flaps for the management of complicated epidermoid cysts on the back. Sci Rep. 2019;9:14699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Riccio CA, Chang J, Henderson JT, Hassouba M, Ashfaq F, Kostopoulos E, Konofaos P. Keystone flaps: physiology, types, and clinical applications. Ann Plast Surg. 2019;83:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Behan FC, Rozen WM, Lo CH, Findlay M. The omega –Ω– variant designs (types A and B) of the keystone perforator island flap. ANZ J Surg. 2011;81:650-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Byun IH, Kim CW, Park TH. The modified keystone flap for pressure ulcers: a modification of the keystone flap with rotation and advancement. Ann Plast Surg. 2019;82:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Moncrieff MD, Bowen F, Thompson JF, Saw RP, Shannon KF, Shannon KF, Quinn MJ, Stretch JR. Keystone flap reconstruction of primary melanoma excision defects of the leg–the end of the skin graft? Ann Surg Oncol. 2008;15:2867-2873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Shayan R, Behan FC. Re: the ‘keystone concept’: time for some science. ANZ J Surg. 2013;83:499-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Menick FJ. Artistry in aesthetic surgery. Aesthetic perception and the subunit principle. Clin Plast Surg. 1987;14:723-735. [PubMed] |
| 21. | Fattahi TT. An overview of facial aesthetic units. J Oral Maxillofac Surg. 2003;61:1207-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 72] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Mureau MA, Hofer SO. Maximizing results in reconstruction of cheek defects. Clin Plast Surg. 2009;36:461-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Gonzales-Ulloa M. Restoration of the face covering by means of selected skin in regional aesthetic units. Br J Plast Surg. 1956;9:212-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 141] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Behan FC. The fasciocutaneous island flap: an extension of the angiotome concept. ANZ J Surg. 1992;62:874-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Kostopoulos E, Agiannidis C, Konofaos P, Kotsakis I, Hatzigianni P, Georgopoulos G, Papadatou Z, Konstantinidou C, Champsas G, Papadopoulos O, Casoli V. Changing the paradigm in medial canthal reconstruction: the bridge principle and the croissant-like keystone island perforator flap as an alternative for medium size soft tissue defects in internal canthus reconstruction. J Craniofac Surg. 2018;29:e455-e459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Loh IW, Rozen WM, Behan FC, Crock J. Eyelid reconstruction: expanding the applications of the keystone perforator island flap concept. ANZ J Surg. 2012;82:763-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Ettinger KS, Fernandes RP, Arce K. Keystone flap. Atlas Oral Maxillofac Surg Clin North Am. 2020;28:29-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |