Published online Apr 26, 2019. doi: 10.12998/wjcc.v7.i8.928
Peer-review started: January 31, 2019
First decision: March 10, 2019
Revised: March 22, 2019
Accepted: April 9, 2019
Article in press: April 9, 2019
Published online: April 26, 2019
Processing time: 87 Days and 1.5 Hours
Chronic total occlusion (CTO) is found in 18-31% of patients who undergo coronary angiography. Successful recanalization of CTOs is associated with reduced recurrent angina pectoris rates and increased long-term survival. Although the success rate of CTO percutaneous coronary intervention (CTO-PCI) has improved, CTO-PCI remains technically challenging. The Fielder XT guidewire was designed for CTO lesions. To validate whether the use of the guidewire increases the success rate, we compared the results of CTO-PCI with or without the guidewire. We hypothesized that the use of Fielder XT guidewire can increase the success rate of CTO-PCI.
To investigate whether the use of Fielder XT guidewire increases the final procedural success of CTO-PCI via the anterograde approach.
Between January 2013 and December 2015, a retrospective study was conducted on 1230 consecutive patients with CTO who received PCI via the anterograde approach at the General Hospital of Northern Theater Command. The patients were divided into an XT Group (n = 686) and a no-XT Group (n = 544) depending on whether Fielder XT guidewire was used. Both groups were compared for clinical parameters, lesion-related characteristics, procedural outcomes and in-hospital complications. The data were statistically analyzed using Pearson’s χ2 test for categorical variables, and Students’ t test was used to compare the quantitative data. Significant independent factors and a risk ratio with 95% confidence interval (CI) were assessed by multivariate logistic regression analysis.
In total, 1230 patients were recruited; 75.4% of the patients were male, and 55.8% of the patients were in the XT group. The overall success rate was 83.9%, with 87.8% in the XT group. Based on multivariate logistic regression analysis, factors positively associated with procedural success were the use of Fielder XT guidewire (P = 0.005, 95%CI: 1.172-2.380) and systolic blood pressure (P = 0.011, 95%CI: 1.003-1.022), while factors negatively associated with procedural success were blunt stump (P = 0.013, 95%CI: 1.341-11.862), male sex (P = 0.016, 95%CI: 0.363-0.902), New York Heart Association (NYHA) class (P = 0.035, 95%CI: 0.553-0.979), contrast amount (P = 0.018, 95%CI: 0.983-0.998) and occlusion time (P = 0.009, 95%CI: 0.994-0.999). No significant differences were found between the XT group and the no-XT group with respect to clinical parameters, lesion-related characteristics, coronary artery rupture [3 (0.4%) vs 8 (1.5%), P = 0.056], in-hospital death [2 (0.3%) vs 6 (1.1%), P = 0.079] or in-hospital target lesion revascularization [3 (0.4%) vs 7 (1.3%), P < 0.099]. However, there were significant differences between the groups with respect to success rate [602 (87.8%) vs 430 (79.0%), P < 0.001], procedure time [(74 ± 23) vs (83 ± 21), P < 0.001], stent length [(32.0 ± 15.8) vs (37.3 ± 17.6), P < 0.001], contrast amount [(148 ± 46) vs (166 ± 43), P < 0.001], post-PCI myocardial infarction [43 (6.3%) vs 59 (10.8%), P = 0.004], major adverse cardiovascular event [44 (6.4%) vs 57 (10.7%), P = 0.007], side branch loss [31 (4.5%) vs 44 (8.1%), P = 0.009], contrast-induced nephropathy [29 (4.2%) vs 40 (7.4%), P = 0.018] and no reflow [8 (1.2%) vs 14 (2.9%), P = 0.034].
The use of Fielder XT guidewire shortens the Procedure and increases the success rate of CTO-PCI, and is also associated with reduced complication rates.
Core tip: This retrospective study aimed to investigate whether the use of Fielder XT guidewire can increase the final procedural success of chronic total occlusion-percutaneous coronary intervention via the anterograde approach. We found that the use of Fielder XT guidewire was positively associated with procedural success based on multivariate logistic regression analysis. We found no significant differences between the XT group and the no-XT group with respect to clinical parameters, lesion-related characteristics, coronary artery rupture, in-hospital death or in-hospital target lesion revascularization. However, we found significant differences between the groups with respect to success rate, procedure time, stent length, contrast amount and in-hospital complications.
- Citation: Wang QC, Lin HR, Han Y, Dong H, Xu K, Guan SY, Chen ZH, Hao HX, Bin JP, Liao YL, Jing QM. Optimal use of fielder XT guidewire enhances the success rate of chronic total occlusion percutaneous coronary intervention. World J Clin Cases 2019; 7(8): 928-939
- URL: https://www.wjgnet.com/2307-8960/full/v7/i8/928.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i8.928
Coronary chronic total occlusion (CTO), defined as a lesion with total occlusion exhibiting thrombolysis in myocardial infarction (TIMI) grade 0 flow in a native vessel for more than 3 mo, is found in 18%-31% of patients who undergo invasive coronary angiography[1,2]. Successful recanalization of CTOs has been shown to be associated with reduced risks of death, coronary artery bypass grafting[3], recurrent angina pectoris[4] and increased long-term survival[5,6]. In addition, failure of CTO-percutaneous coronary intervention (CTO-PCI) is reported to be associated with higher subsequent mortality and more frequent major adverse cardiovascular events (MACE)[7]. Although experience and the introduction of new devices have improved the success rate of PCI[8], CTO-PCI is still technically challenging. The most common reason for CTO-PCI failure is the failure of the guidewire to cross the occlusion segment[9]. Recently, the Fielder XT guidewire was specifically designed for CTO lesions. It has a soft, tapered polymer-jacketed tip, and has been introduced and used worldwide.
To validate whether Fielder XT guidewire can increase the success rate of PCI in CTO lesions, we retrospectively compared data from 1230 consecutive patients with CTO who received PCI via the anterograde approach at our institution from January 2013 to December 2015. We hypothesized that the use of Fielder XT guidewire can increase the success rate of CTO-PCI via the anterograde approach.
Between January 2013 and December 2015, 1230 consecutive patients with CTO who received PCI via the anterograde approach at the General Hospital of Northern Theater Command. The study protocol was approved by the local ethics committee, and all procedures were performed according to current international guidelines[10,11]. All patients provided written informed consent. We conducted a retrospective analysis of these 1230 patients.
CTO was defined as a lesion with total occlusion exhibiting TIMI grade 0 flow in a native vessel for more than 3 mo. Estimation of the occlusion duration was based on the first onset of angina symptoms, prior history of myocardial infarction (MI) in the target vessel territory, or comparison with a prior angiogram. Procedural success was defined as angiographic success (final residual diameter stenosis < 20% and TIMI grade 3 flow following recanalization of the CTO). Clinical success was defined as successful PCI with the patient discharged alive.
Patients were candidates for intervention if they had sufficient cardiac function to lie in the supine position for at least 2 h. To minimize confounding factors, only patients undergoing primary anterograde CTO-PCI whose target vessel was ≥ 2.5 mm in diameter were included in this study. Patients were excluded if they had more than one CTO treated during the same PCI procedure, or if there was no clear evidence for CTO duration ≥ 3 mo.
Based on the use of Fielder XT guidewire, the patients were divided into two groups: the XT group (n = 686) and the no-XT group (n = 544). Both groups were compared for clinical parameters, lesion-related characteristics, procedural outcomes and in-hospital complications.
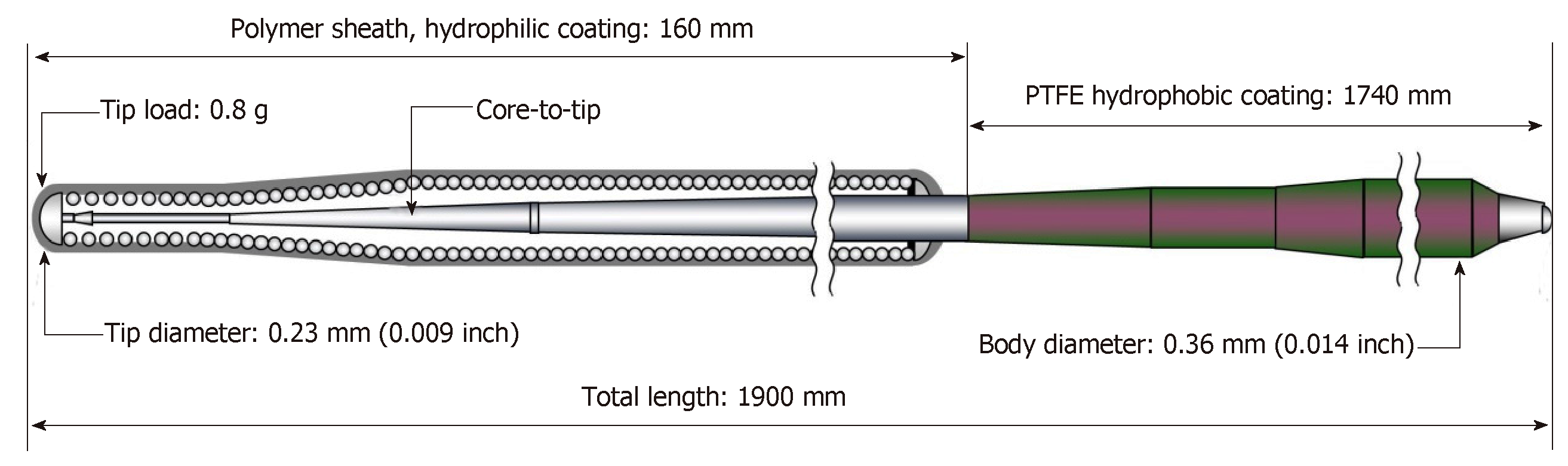
All interventional procedures were performed using standard techniques. The selection of arterial access depends on the characteristics of the target lesions. Generally, puncture of one of the right radial arteries or right femoral arteries was performed. If necessary, puncture of two arteries among the right radial artery, left radial artery, right femoral artery and left femoral artery were performed. We preferred the Amplatz Left guiding catheter when performing CTO-PCI of the right coronary artery, and we preferred the EBU or the Extra Backup guiding catheter when performing CTO-PCI of the left anterior descending (LAD) and left circumflex artery. The anterograde wire escalation (AWE) strategy was employed for anterograde crossing of the CTO. AWE was usually started with a soft (tip load = 0.8 g), tapered polymer-jacketed guidewire (such as Fielder XT, Asahi Intecc, Japan), a tapered polymer-jacketed guidewire (such as Pilot 50, Abbott, United States), a stiff guidewire (such as Miracle 6, Asahi Intecc), or a stiff, tapered guidewire (such as Conquest, Asahi Intecc).
AWE technique was always performed using an over-the-wire system (such as Finecross microcatheter, Terumo, Japan, or Corsair microcatheter, Asahi Intecc) to support the guidewire. A microcatheter allowed rapid exchange of guidewires, while maintaining wire position and improving guidewire torque response. Microcatheters also improve support and enable dynamic alterations of the penetration power of the guidewire by changing the distance between the microcatheter tip and wire tip. Some of the preferred wires are able to cross the CTO lesions either directly or with the support of the over-the-wire system. If the first soft wire entered the subintimal space of the occlusion segment and failed to cross the CTO lesion, we upgraded to a stiff, tapered wire for crossing using the parallel wires technique. If the first wire could not enter the proximal cap of the CTO lesion, we used a higher-tip-load tapered wire to puncture the proximal cap and then downgraded to a softer, tapered polymer-jacketed guidewire to cross the occlusion. If the CTO had tortuous vessels or unclear vascular anatomy, the knuckle wire technique was usually attempted with a polymer-jacketed guidewire (such as Fielder XT or Pilot 50). Other techniques including the buddy wire technique, multiwire plaque crushing, subintimal tracking and reentry, and balloon jailing were also employed as required. All PCI procedures were performed by experienced interventionists who handled at least 50 cases of CTO-PCI annually.
Continuous variables are presented as the mean ± SD, and categorical data are presented as numbers (proportions). The data were statistically analyzed using Pearson’s χ2 test for categorical variables, and Students’ t test was used to compare the quantitative data. Significant independent factors and risk ratio with 95% confidence interval (CI) were assessed by multivariate logistic regression analysis. Analyses were performed using SPSS software (version 21.0; SPSS Inc., Chicago, IL, United States), and P < 0.05 (2-sided) was considered statistically significant.
A total of 1230 patients aged from 31 to 88 years were enrolled, with 74.8% (898/1230) of the patients being male and 55.8% (686/1230) of the patients in the XT group. The overall success rate was 83.9% (1032/1230).
The right radial arterial access percentage is 38.4% (472/1230); the right femoral arterial access percentage is 6.3% (77/1230); the right and left radials arterial accesses percentage is 33.1% (407/1230); the right radial arterial and right femoral arterial accesses percentage is 17.1% (210/1230); the right and left femoral arterial accesses percentage is 5.2% (64/1230).
According to backward logistic regression analysis by Wald’s method, the following factors were positively correlated with successful CTO-PCI: Use of Fielder XT guidewire (P = 0.005, 95%CI: 1.172-2.380) and systolic blood pressure (P = 0.011, 95%CI: 1.003-1.022), while factors negatively associated with procedural success were blunt stump (P = 0.013, 95%CI: 1.341-11.862), male sex (P = 0.016, 95%CI: 0.363-0.902), New York Heart Association (NYHA) class (P = 0.035, 95%CI: 0.553-0.979), contrast amount (P = 0.018, 95%CI: 0.983-0.998) and occlusion time (P = 0.009, 95%CI: 0.994-0.999) (Table 1).
| β coefficient | Wald | Exp (β) | P-value | 95%CI of OR | |
| Clinical predictors | |||||
| Sex, male | -0.559 | 7.780 | 0.572 | 0.016 | 0.363~0.902 |
| Systolic blood pressure | 0.012 | 6.405 | 1.012 | 0.011 | 1.003~1.022 |
| NYHA class | -0.307 | 4.445 | 0.735 | 0.035 | 0.553~0.979 |
| Contrast amount | -0.009 | 5,555 | 0.991 | 0.018 | 0.983~0.998 |
| Lesion-related predictors | |||||
| Occlusion time | -0.003 | 6.848 | 0.997 | 0.009 | 0.994~0.999 |
| Blunt stump | -1.382 | 6.192 | 3.982 | 0.013 | 1.341~11.862 |
| Use of Fielder XT | 0.513 | 8.060 | 1.670 | 0.005 | 1.172~2.380 |
| Constant | -5.668 | 0.127 | 0.003 | 0.722 |
Based on the use of Fielder XT guidewire, the patients were divided into two groups: The XT group (n = 686; 55.8%) and the no-XT group (n = 544; 44.2%). When clinical characteristics from the two groups were compared, we found no significant differences based on male sex (P = 0.313), age (P = 0.062), height (P = 0.064), body weight (P = 0.645), body mass index (P = 0.112), systolic blood pressure (P = 0.146), diastolic blood pressure (P = 0.365), hypertension (P = 0.782), diabetes mellitus (P = 0.988), previous stroke (P = 0.521), old MI (P = 0.587), previous PCI (P = 0.431), previous renal insufficiency (P = 0.513), smoking (P = 0.325), alcohol drinking (P = 0.887), left ventricular ejection fraction (P = 0.587), left ventricular end-diastolic diameter (P = 0.559), serum creatinine (P = 0.577), cardiothoracic ratio (P = 0.089), NYHA heart function class (P = 0.643) or age ≥ 65 years (P = 0.585) (Table 2).
| Overall population, n = 1230 | XTgroup, n = 686 | No-XT group, n = 544 | P-value | |
| Sex, male | 928 (75.4) | 510 (74.3) | 418 (76.8) | 0.313 |
| Age, yr | 61.9 ± 10.3 | 62.4 ± 9.9 | 61.3 ± 10.8 | 0.062 |
| Height, cm | 169.5 ± 6.3 | 169.2 ± 6.3 | 169.9 ± 6.4 | 0.064 |
| Body weight, kg | 74.0 ± 10.0 | 74.4 ± 10.7 | 74.2 ± 10.0 | 0.645 |
| Body mass index, kg/m2 | 25.8 ± 3.2 | 26.0 ± 3.3 | 25.7 ± 3.1 | 0.112 |
| SBP, mmHg | 137.0 ± 20.8 | 137.7 ± 20.6 | 136.0 ± 21.0 | 0.146 |
| DBP, mmHg | 81.0 ± 12.9 | 81.3 ± 13.1 | 80.6 ± 12.7 | 0.365 |
| Hypertension | 765 (62.2) | 429 (62.5) | 336 (61.8) | 0.782 |
| Diabetes mellitus | 405 (32.9) | 226 (32.9) | 179 (32.9) | 0.988 |
| Previous stroke | 95 (7.7) | 50 (7.3) | 45 (8.3) | 0.521 |
| OMI | 408 (33.2) | 232 (33.8) | 176 (32.4) | 0.587 |
| Previous PCI | 328 (26.7) | 189 (27.6) | 139 (25.6) | 0.431 |
| PRI | 119 (9.7) | 63 (9.2) | 56 (10.3) | 0.513 |
| Smoking | 693 (56.3) | 378 (55.1) | 315 (57.9) | 0.325 |
| Alcohol drinking | 445 (36.2) | 247 (36.0) | 198 (36.4) | 0.887 |
| LVEF, % | 60.0 ± 9.0 | 60.0 ± 9.0 | 59.8 ± 8.6 | 0.587 |
| LVEDd, mm | 48.4 ± 6.3 | 48.5 ± 6.4 | 48.3 ± 6.2 | 0.559 |
| Serum creatinine, μmol/L | 73.0 ± 23.0 | 72.5 ± 23.9 | 71.8 ± 21.6 | 0.577 |
| Cardiothoracic ratio, % | 54.0 ± 6.0 | 53.8 ± 6.1 | 53.2 ± 6.0 | 0.089 |
| NYHA heart function class | 0.643 | |||
| Class I | 923 (75.0) | 510 (74.3) | 413 (75.9) | |
| Class II | 247 (20.1) | 144 (21.0) | 103 (18.9) | |
| Class III | 60 (4.9) | 32 (4.7) | 28 (5.1) | |
| Age ≥ 65 yr | 532 (43.3) | 292 (42.6) | 240 (44.1) | 0.585 |
The groups were further compared for lesion-related characteristics. The two groups did not differ significantly in terms of multivessel coronary artery disease (P = 0.609), lesion calcification (P = 0.423), tortuosity (P = 0.124), bridging collaterals (P = 0.665), blunt stump (P = 0.787), J-CTO score (P = 0.077), Rentrop class (P = 0.686), CTO vessel (P = 0.570), occlusion length (P = 0.876), or occlusion time (P = 0.796) (Table 3).
| Overall population, n = 1230 | XT group, n = 686 | No-XT group, n = 544 | P-value | |
| Multivessel CAD | 530 (43.1) | 300 (43.7) | 230 (42.3) | 0.609 |
| LC | 170 (13.8) | 90 (13.1) | 80 (14.7) | 0.423 |
| Tortuosity | 105 (10.2) | 57 (11.7) | 48 (8.8) | 0.124 |
| Bridging collaterals | 95 (7.7) | 55 (8.0) | 40 (7.4) | 0.665 |
| Blunt stump | 107 (8.7) | 61 (8.9) | 46 (8.5) | 0.787 |
| J-CTO score | 0.077 | |||
| 0 | 597 (48.5) | 332 (48.4) | 265 (48.7) | |
| 1 | 507 (41.2) | 282 (41.1) | 225 (41.4) | |
| 2 | 99 (8.0) | 50 (7.3) | 49 (9.0) | |
| 3 | 23 (1.9) | 19 (2.8) | 4 (0.7) | |
| 4 | 4 (0.3) | 3 (0.4) | 1 (0.2) | |
| Rentrop class | 0.686 | |||
| 0 | 233 (18.9) | 126 (18.4) | 107 (19.7) | |
| 1 | 220 (17.9) | 117 (17.1) | 103 (18.9) | |
| 2 | 434 (35.3) | 245 (35.7) | 189 (34.7) | |
| 3 | 343 (27.9) | 198 (28.9) | 145 (26.7) | |
| CTO vessel | 0.570 | |||
| LM | 1 (0.1) | 1 (0.1) | 0 (0) | |
| LAD | 545 (44.3) | 302 (44.0) | 243 (44.7) | |
| LCX | 173 (14.1) | 103 (15.0) | 70 (12.9) | |
| RCA | 511 (41.5) | 280 (40.8) | 231 (42.5) | |
| Occlusion length, mm | 21.6 ± 14.8 | 21.5 ± 15.1 | 21.7 ± 14.5 | 0.876 |
| Occlusion time, mo | 82.3 ± 27.1 | 45.9 ± 60.0 | 45.0 ± 50.9 | 0.796 |
When the procedural outcomes and in-hospital complications were compared between the two groups, there were no significant differences in coronary artery rupture [3 (0.4%) vs 8 (1.5%), P = 0.056], in-hospital death [2 (0.3%) vs 6 (1.1%), P = 0.079] or in-hospital target lesion revascularization (TLR) [3 (0.4%) vs 7 (1.3%), P < 0.099] (Table 4); however, there were significant differences with regard to success rate [602 (87.8%) vs 430 (79.0%), P < 0.001], procedure time [(74 ± 23) vs (83 ± 21), P < 0.001], stent length [(32.0 ± 15.8) vs (37.3 ± 17.6), P < 0.001], contrast amount [(148 ± 46) vs (166 ± 43), P < 0.001], post-PCI MI [43 (6.3%) vs 59 (10.8%), P = 0.004], MACE [44 (6.4%) vs 57 (10.7%), P = 0.007], side branch loss [31 (4.5%) vs 44 (8.1%), P = 0.009], contrast-induced nephropathy (CIN) [29 (4.2%) vs 40 (7.4%), P = 0.018] and no reflow [8 (1.2%) vs 14 (2.9%), P = 0.034] (Table 4).
| Overall population, n = 1230 | XTgroup, n = 686 | No-XT group, n = 544 | P-value | |
| Stent length, mm | 34.3 ± 16.8 | 32.0 ± 15.8 | 37.3 ± 17.6 | < 0.001 |
| Contrast amount, mL | 156.1 ± 45.6 | 148 ± 46 | 166 ± 43 | < 0.001 |
| Side branch loss | 75 (6.1) | 31 (4.5) | 44 (8.1) | 0.009 |
| CIN | 69 (5.6) | 29 (4.2) | 40 (7.4) | 0.018 |
| Coronary artery rupture | 11 (0.9) | 3 (0.4) | 8 (1.5) | 0.056 |
| No reflow | 22 (1.9) | 8 (1.2) | 14 (2.9) | 0.034 |
| Post-PCI MI | 102 (8.3) | 43 (6.3) | 59 (10.8) | 0.004 |
| In-hospital death | 8 (0.7) | 2 (0.3) | 6 (1.1) | 0.079 |
| TLR | 10 (0.8) | 3 (0.4) | 7 (1.3) | 0.099 |
| MACE | 101 (8.3) | 44 (6.4) | 57 (10.7) | 0.007 |
| Success rate | 1032 (83.9) | 602 (87.8) | 430 (79.0) | < 0.001 |
| Procedure time, min | 78 ± 23 | 74 ± 23 | 83 ± 21 | < 0.001 |
This retrospective study investigated the use of Fielder XT guidewire in CTO-PCI via the anterograde approach. We focused on the relationship between the use of Fielder XT guidewire and the success rate of CTO-PCI, and evaluated the occurrence of in-hospital complications in two groups. The main novel findings of this study are as follows: (1) The use of Fielder XT guidewire contributes to increasing the success rate of CTO-PCI via the anterograde approach; and (2) The use of Fielder XT guidewire is associated with reduced rates of in-hospital complications and stent implantations.
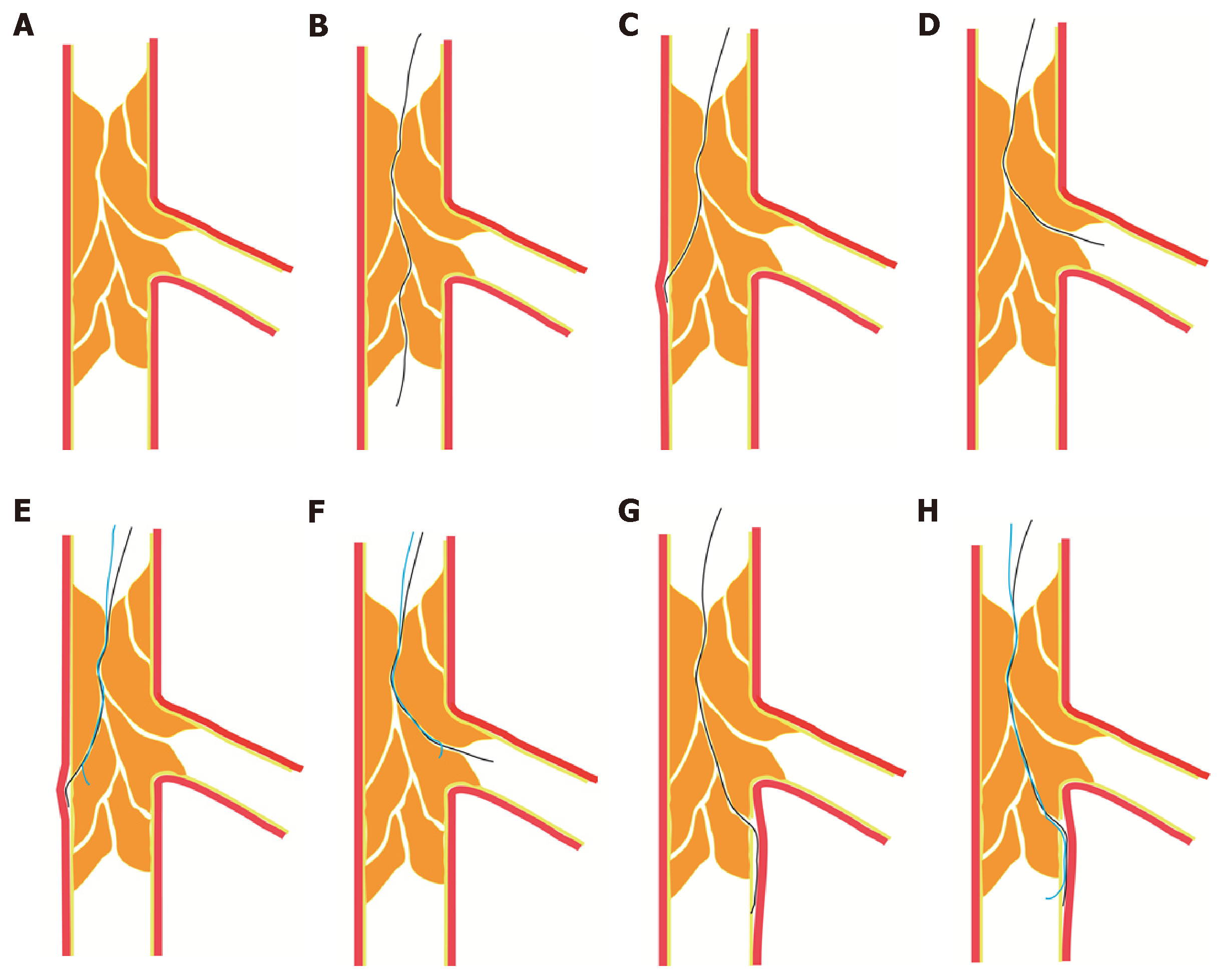
The AWE technique is the most common strategy for CTO-PCI, and polymer-jacketed guidewires are most frequently used to implement this strategy. Although Karatasakis et al[12] recently reported that the use of stiff polymer-jacketed guidewires results in a high CTO crossing rate without increasing the incidence of MACE or perforation[12], we found that a soft, tapered polymer-jacketed Fielder XT (Figure 1) guidewire was also effective in crossing the occlusion. Consistent with our results, the Euro-CTO club has recommended starting with a soft (tip load < 1 g), tapered polymer-jacketed guidewire, not only because of high success rates but also because of the low risk of distal vessel damage if the wire fails to cross the lesion[13]. The existence of microchannels, which partly or completely connect from the proximal cap to the distal end of CTO lesions[14] (Figure 2A), has also been reported to predict procedural success[15]. Single wiring displays a high success rate as the initial PCI strategy for CTO of the LAD, and is generally performed with a tapered guidewire such as Fielder XT[16] (Figure 2B). The diameter of the Fielder XT guidewire is 230 µm, while the diameters of the microchannels range from 160 to 230 µm[14]. Therefore, it is reasonable to select Fielder XT as the initial guidewire. Additionally, microchannels frequently end at the sidewall of the coronary artery or connect to the side branches far proximal to the distal end of the CTO lesion. Some of these microchannels may run longitudinally through the lesion from the proximal to the distal lumen for up to 85% of the total length of the CTO (Figure 2A). The initial soft, tapered polymer-jacketed guidewire can easily enter the proximal cap through microchannels, but the wire frequently goes into the sidewall of the coronary artery and results in forming intimal dissection (Figure 2C). It may also go into the side branches of the occlusion segment (Figure 2D). In such situations, the parallel wire technique, which is based on a middle-hard guidewire with a tapered tip, is the best approach to solve the problem. First, the initial guidewire in the false lumen or side branch is left both as a marker and to obstruct the false channel. Second, a second tapered guidewire is used to trace the exact path as the first wire. After the tip of the second guidewire reaches the point where the first guidewire appeared to divert from the true lumen, the tip of the second guidewire is intentionally directed into the true lumen (Figure 2E and F). In this case, the second guidewire usually has a high crossing rate and a low side branch occlusion rate. If the second guidewire fails to enter the true lumen, the AWE strategy for CTO will usually involve switching from a middle-hard guidewire with a tapered tip to a stiff guidewire with a tapered tip. If the initial guidewire had already crossed the occlusion segment and entered the subintimal region of the distal cap (Figure 2G), an anterograde dissection reentry (ADR) strategy can be employed. This is usually attempted to minimize the length of the dissection by reentry into the distal true lumen using a stiff guidewire with a tapered tip immediately after the distal cap of the occlusion segment (Figure 2H). If an initial stiff guidewire has been used to puncture the proximal cap, it is important to downgrade to a soft, tapered polymer-jacketed guidewire, such as Fielder XT, to reduce the risk of perforation and increase the chance of tracking the vessel[17].
In the present study, we found that a strategy based on the initial use of Fielder XT guidewire significantly increased the success rate of CTO-PCI via the anterograde approach. This may have been partially attributable to the existence of microchannels with a diameter of approximately 160-230 µm in the CTO lesions. The number of microchannels has been reported to decrease with CTO maturation[18]. Other studies have reported that these channels can exist in loose tissues extending from the proximal to distal fibrous caps in CTOs of any age[19]. Thus, successful tracking of microchannels in loose tissue may be possible, even in very old CTOs[20]. Consistent with these data, we found that the use of Fielder XT guidewire significantly increased the success rate of CTO-PCI, although there were no significant differences in occlusion time between the two groups.
Nevertheless, factors predicting the success or failure of CTO-PCI are context-dependent. In agreement with previous studies, we noted that blunt stump[21-24] was an independent predictor of the procedural success of CTO-PCI. In recent years, multiple scoring systems have been established to predict the procedural success, efficiency, and complications of CTO-PCI[21-26]. Both the multicenter CTO registry in Japan (J-CTO) and clinical- and lesion-related (CL) scores include blunt stump as the lesion-related predictor[21,23]. CTO with blunt stump is a major obstacle to successful intervention. If the proximal cap has a blunt morphology, the occlusion is often more mature[17]. Older occlusions usually have harder proximal caps and lack microchannels connected to the proximal cap, which prevent the initial soft, tapered polymer-jacketed guidewire from entering the proximal cap. Thus, the blunt stump of proximal cap is an obstacle to the procedural success of CTO-PCI[17]. In accordance with the results of previous studies, we also found that contrast amount, procedure time and cardiac function were independent predictors of procedural success. Algorithms also provide specific guidance, suggesting that operators should consider stopping a CTO procedure if the procedure time is > 3 h, or more than 3.7 mL × the estimated glomerular filtration rate of contrast has been used[17]. Systolic blood pressure is closely related to cardiac function, and systolic blood pressure was thus an independent predictor of procedural success in this study. Furthermore, females have lower J-CTO scores than males. The technical success rate is usually higher in females than in males[27], consistent with our observed outcomes.
In summary, we found in this study that the use of Fielder XT guidewire was associated with a relatively shorter procedure time and lower contrast amount, as Fielder XT guidewire could cross CTO lesions into the distal true lumen by microchannels. The amount of contrast media is closely related to the incidence of CIN, and several studies have shown that the volume of contrast media is an independent risk factor for the development of contrast-induced acute kidney injury[28-30]. We observed a similar outcome in which the volume of contrast media was positively associated with CIN incidence. We also found that the use of Fielder XT guidewire was associated with lower rates of in-hospital complications and stent implantation. Furthermore, the initial soft, tapered polymer-jacketed guidewire we used could cross the CTO lesion and reach the distal cap, with lower likelihoods of dissection and a smaller degree of hematoma than stiff guidewires. ADR based on the soft guidewire we used above could also ensure true lumen reentry once through the CTO segment, which decreased the length of the implanted stent and reduced side branch loss. Additionally, MI of perioperative caused by the occlusion of side branches after CTO-PCI was avoided.
In conclusion, the use of Fielder XT guidewire shortens the procedure and increases the success rate of CTO-PCI, and is also associated with reduced complication rates.
Chronic total occlusion (CTO) is found in 18%-31% of patients who undergo coronary angiography. Successful recanalization of CTOs has been shown to be associated with reduced recurrent angina pectoris rates and increased long-term survival. Although the success rate of CTO percutaneous coronary intervention (CTO-PCI) has improved, CTO-PCI remains technically challenging. The Fielder XT guidewire was designed for CTO lesions. To validate whether the use of the guidewire increases the success rate, we compared the results of CTO-PCI with or without the guidewire. We hypothesized that the use of Fielder XT guidewire can increase the success rate of CTO-PCI.
Although experience and the introduction of new devices have improved the success rates of PCI, CTO-PCI is still technically challenging. We thus wanted to validate whether the use of Fielder XT guidewire increases the success rate of CTO-PCI.
To investigate whether the use of Fielder XT guidewire increases the final procedural success of CTO-PCI via the anterograde approach.
Between January 2013 and December 2015, a retrospective study was conducted on 1230 consecutive patients with CTO who received PCI via the anterograde approach at the General Hospital of Northern Theater Command. The patients were divided into an XT Group (n = 686) and a no-XT Group (n = 544) depending on whether Fielder XT guidewire was used. Both groups were compared for clinical parameters, lesion-related characteristics, procedural outcomes and in-hospital complications. The data were statistically analyzed using a Pearson’s χ2 test for categorical variables, and a Students’ t test was used to compare the quantitative data. Significant independent factors and risk ratios with a 95% confidence interval (CI) were assessed by multivariate logistic regression analysis.
In total, 1230 patients were recruited; 75.4% of the patients were male, and 55.8% of the patients were in the XT group. The overall success rate was 83.9%, with 87.8% in the XT group. Based on multivariate logistic regression analysis, factors positively associated with procedural success were the use of Fielder XT guidewire (P = 0.005, 95%CI: 1.172-2.380) and systolic blood pressure (P = 0.011, 95%CI: 1.003-1.022), while factors negatively associated with procedural success were blunt stump (P = 0.013, 95%CI: 1.341-11.862), male sex (P = 0.016, 95%CI: 0.363-0.902), NYHA class (P = 0.035, 95%CI: 0.553-0.979), contrast amount (P = 0.018, 95%CI: 0.983-0.998) and occlusion time (P = 0.009, 95%CI: 0.994-0.999). No significant differences were found between the XT group and the no-XT group with respect to clinical parameters, lesion-related characteristics, coronary artery rupture [3 (0.4%) vs 8 (1.5%), P = 0.056], in-hospital death [2 (0.3%) vs 6 (1.1%), P = 0.079] or in-hospital target lesion revascularization [3 (0.4%) vs 7 (1.3%), P < 0.099]. However, there were significant differences between the groups with respect to success rate [602 (87.8%) vs 430 (79.0%), P < 0.001], procedure time [(74 ± 23) vs (83 ± 21), P < 0.001], stent length [(32.0 ± 15.8) vs (37.3 ± 17.6), P < 0.001], contrast amount [(148 ± 46) vs (166 ± 43), P < 0.001], post-PCI myocardial infarction [43 (6.3%) vs 59 (10.8%), P = 0.004], major adverse cardiovascular event [44 (6.4%) vs 57 (10.7%), P = 0.007], side branch loss [31 (4.5%) vs 44 (8.1%), P = 0.009], contrast-induced nephropathy [29 (4.2%) vs 40 (7.4%), P = 0.018] and no reflow [8 (1.2%) vs 14 (2.9%), P = 0.034].
The use of Fielder XT guidewire shortens the procedure and increases the success rate of CTO-PCI, and is also associated with reduced complication rates.
Larger multicenter studies are required to better understand the relationship between the use of Fielder XT series (such as Fielder XT, Fielder XT-R and Fielder XT-A) guidewires and the procedural success of CTO-PCI via anterograde, retrograde, or hybrid approaches.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abadi ATB, Aseni P, Elhamid SMA S-Editor: Ji FF L-Editor: Filipodia E-Editor: Wu YXJ
| 1. | Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, Gannot S, Samuel M, Weisbrod M, Bierstone D, Sparkes JD, Wright GA, Strauss BH. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59:991-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 473] [Cited by in RCA: 589] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 2. | Jeroudi OM, Alomar ME, Michael TT, El Sabbagh A, Patel VG, Mogabgab O, Fuh E, Sherbet D, Lo N, Roesle M, Rangan BV, Abdullah SM, Hastings JL, Grodin J, Banerjee S, Brilakis ES. Prevalence and management of coronary chronic total occlusions in a tertiary Veterans Affairs hospital. Catheter Cardiovasc Interv. 2014;84:637-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 175] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 3. | Warren RJ, Black AJ, Valentine PA, Manolas EG, Hunt D. Coronary angioplasty for chronic total occlusion reduces the need for subsequent coronary bypass surgery. Am Heart J. 1990;120:270-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Christakopoulos GE, Christopoulos G, Carlino M, Jeroudi OM, Roesle M, Rangan BV, Abdullah S, Grodin J, Kumbhani DJ, Vo M, Luna M, Alaswad K, Karmpaliotis D, Rinfret S, Garcia S, Banerjee S, Brilakis ES. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115:1367-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 189] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 5. | Ivanhoe RJ, Weintraub WS, Douglas JS, Lembo NJ, Furman M, Gershony G, Cohen CL, King SB. Percutaneous transluminal coronary angioplasty of chronic total occlusions. Primary success, restenosis, and long-term clinical follow-up. Circulation. 1992;85:106-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 207] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Suero JA, Marso SP, Jones PG, Laster SB, Huber KC, Giorgi LV, Johnson WL, Rutherford BD. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001;38:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 463] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 7. | Prasad A, Rihal CS, Lennon RJ, Wiste HJ, Singh M, Holmes DR. Trends in outcomes after percutaneous coronary intervention for chronic total occlusions: a 25-year experience from the Mayo Clinic. J Am Coll Cardiol. 2007;49:1611-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 237] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 8. | King SB, Yeh W, Holubkov R, Baim DS, Sopko G, Desvigne-Nickens P, Holmes DR, Cowley MJ, Bourassa MG, Margolis J, Detre KM. Balloon angioplasty versus new device intervention: clinical outcomes. A comparison of the NHLBI PTCA and NACI registries. J Am Coll Cardiol. 1998;31:558-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Sapontis J, Christopoulos G, Grantham JA, Wyman RM, Alaswad K, Karmpaliotis D, Lombardi WL, McCabe JM, Marso SP, Kotsia AP, Rangan BV, Christakopoulos GE, Garcia S, Thompson CA, Banerjee S, Brilakis ES. Procedural failure of chronic total occlusion percutaneous coronary intervention: Insights from a multicenter US registry. Catheter Cardiovasc Interv. 2015;85:1115-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS);. European Association for Percutaneous Cardiovascular Interventions (EAPCI), Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501-2555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1660] [Cited by in RCA: 1715] [Article Influence: 114.3] [Reference Citation Analysis (0)] |
| 11. | Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1654] [Cited by in RCA: 1744] [Article Influence: 124.6] [Reference Citation Analysis (0)] |
| 12. | Karatasakis A, Tarar MN, Karmpaliotis D, Alaswad K, Yeh RW, Jaffer FA, Wyman RM, Lombardi WL, Grantham JA, Kandzari DE, Lembo NJ, Moses JW, Kirtane AJ, Parikh M, Garcia S, Doing A, Pershad A, Shah A, Patel M, Bahadorani J, Shoultz CA, Danek BA, Thompson CA, Banerjee S, Brilakis ES. Guidewire and microcatheter utilization patterns during antegrade wire escalation in chronic total occlusion percutaneous coronary intervention: Insights from a contemporary multicenter registry. Catheter Cardiovasc Interv. 2017;89:E90-E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Sianos G, Werner GS, Galassi AR, Papafaklis MI, Escaned J, Hildick-Smith D, Christiansen EH, Gershlick A, Carlino M, Karlas A, Konstantinidis NV, Tomasello SD, Di Mario C, Reifart N; EuroCTO Club. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. 2012;8:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 271] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 14. | Katsuragawa M, Fujiwara H, Miyamae M, Sasayama S. Histologic studies in percutaneous transluminal coronary angioplasty for chronic total occlusion: comparison of tapering and abrupt types of occlusion and short and long occluded segments. J Am Coll Cardiol. 1993;21:604-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 127] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Baykan AO, Gür M, Acele A, Şeker T, Quisi A, Kıvrak A, Yıldırım A, Uçar H, Akyol S, Çaylı M. Predictors of successful percutaneous coronary intervention in chronic total coronary occlusions. Postepy Kardiol Interwencyjnej. 2016;12:17-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Nassar YS, Boudou N, Dumonteil N, Lhermusier T, Carrie D. Guidewires used in first intentional single wiring strategy for chronic total occlusions of the left anterior descending coronary artery. Heart Views. 2013;14:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Harding SA, Wu EB, Lo S, Lim ST, Ge L, Chen JY, Quan J, Lee SW, Kao HL, Tsuchikane E. A New Algorithm for Crossing Chronic Total Occlusions From the Asia Pacific Chronic Total Occlusion Club. JACC Cardiovasc Interv. 2017;10:2135-2143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 146] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 18. | Munce NR, Strauss BH, Qi X, Weisbrod MJ, Anderson KJ, Leung G, Sparkes JD, Lockwood J, Jaffe R, Butany J, Teitelbaum AA, Qiang B, Dick AJ, Wright GA. Intravascular and extravascular microvessel formation in chronic total occlusions a micro-CT imaging study. JACC Cardiovasc Imaging. 2010;3:797-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Galassi AR, Sianos G, Werner GS, Escaned J, Tomasello SD, Boukhris M, Castaing M, Büttner JH, Bufe A, Kalnins A, Spratt JC, Garbo R, Hildick-Smith D, Elhadad S, Gagnor A, Lauer B, Bryniarski L, Christiansen EH, Thuesen L, Meyer-Geßner M, Goktekin O, Carlino M, Louvard Y, Lefèvre T, Lismanis A, Gelev VL, Serra A, Marzà F, Di Mario C, Reifart N; Euro CTO Club. Retrograde Recanalization of Chronic Total Occlusions in Europe: Procedural, In-Hospital, and Long-Term Outcomes From the Multicenter ERCTO Registry. J Am Coll Cardiol. 2015;65:2388-2400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 180] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 20. | Sumitsuji S, Inoue K, Ochiai M, Tsuchikane E, Ikeno F. Fundamental wire technique and current standard strategy of percutaneous intervention for chronic total occlusion with histopathological insights. JACC Cardiovasc Interv. 2011;4:941-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 21. | Alessandrino G, Chevalier B, Lefèvre T, Sanguineti F, Garot P, Unterseeh T, Hovasse T, Morice MC, Louvard Y. A Clinical and Angiographic Scoring System to Predict the Probability of Successful First-Attempt Percutaneous Coronary Intervention in Patients With Total Chronic Coronary Occlusion. JACC Cardiovasc Interv. 2015;8:1540-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 120] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 22. | Opolski MP, Achenbach S, Schuhbäck A, Rolf A, Möllmann H, Nef H, Rixe J, Renker M, Witkowski A, Kepka C, Walther C, Schlundt C, Debski A, Jakubczyk M, Hamm CW. Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion: insights from the CT-RECTOR multicenter registry (Computed Tomography Registry of Chronic Total Occlusion Revascularization). JACC Cardiovasc Interv. 2015;8:257-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 126] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 23. | Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, Hiasa Y, Doi O, Yamashita T, Hinohara T, Tanaka H, Mitsudo K; J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 660] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 24. | Christopoulos G, Kandzari DE, Yeh RW, Jaffer FA, Karmpaliotis D, Wyman MR, Alaswad K, Lombardi W, Grantham JA, Moses J, Christakopoulos G, Tarar MNJ, Rangan BV, Lembo N, Garcia S, Cipher D, Thompson CA, Banerjee S, Brilakis ES. Development and Validation of a Novel Scoring System for Predicting Technical Success of Chronic Total Occlusion Percutaneous Coronary Interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. JACC Cardiovasc Interv. 2016;9:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 270] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 25. | Morino Y, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, Hiasa Y, Doi O, Yamashita T, Morimoto T, Abe M, Hinohara T, Mitsudo K; J-CTO Registry Investigators. In-hospital outcomes of contemporary percutaneous coronary intervention in patients with chronic total occlusion insights from the J-CTO Registry (Multicenter CTO Registry in Japan). JACC Cardiovasc Interv. 2010;3:143-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 204] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 26. | Galassi AR, Boukhris M, Azzarelli S, Castaing M, Marzà F, Tomasello SD. Percutaneous Coronary Revascularization for Chronic Total Occlusions: A Novel Predictive Score of Technical Failure Using Advanced Technologies. JACC Cardiovasc Interv. 2016;9:911-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 27. | Karatasakis A, Iwnetu R, Danek BA, Karmpaliotis D, Alaswad K, Jaffer FA, Yeh RW, Kandzari DE, Lembo NJ, Patel M, Mahmud E, Lombardi WL, Wyman RM, Grantham JA, Doing AH, Toma C, Choi JW, Uretsky BF, Moses JW, Kirtane AJ, Ali ZA, Parikh M, Karacsonyi J, Rangan BV, Thompson CA, Banerjee S, Brilakis ES. The Impact of Age and Sex on In-Hospital Outcomes of Chronic Total Occlusion Percutaneous Coronary Intervention. J Invasive Cardiol. 2017;29:116-122. [PubMed] |
| 28. | Nijssen EC, Rennenberg RJ, Nelemans PJ, Essers BA, Janssen MM, Vermeeren MA, van Ommen V, Wildberger JE. [Prophylactic hydration to protect renal function from intravascular iodinated contrast material in patients at high risk of contrast-induced nephropathy (AMACING): a prospective, randomised, phase 3, controlled, open-label, non-inferiority trial]. Ned Tijdschr Geneeskd. 2018;161:D1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 316] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 29. | Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 690] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 30. | Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, Singh M, Bell MR, Barsness GW, Mathew V, Garratt KN, Holmes DR. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259-2264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1212] [Cited by in RCA: 1213] [Article Influence: 52.7] [Reference Citation Analysis (0)] |