Published online Oct 26, 2019. doi: 10.12998/wjcc.v7.i20.3316
Peer-review started: July 1, 2019
First decision: August 2, 2019
Revised: August 12, 2019
Accepted: August 27, 2019
Article in press: August 27, 2019
Published online: October 26, 2019
Processing time: 119 Days and 13.4 Hours
In general, malignant tumors metastasize to the pancreas in < 1% of cases. Most patients miss the opportunity for further surgery due to distant metastases; however, for fibrosarcomas, aggressive surgery may be helpful even if distant metastases occur. Hence, we report such a case and share some valuable information about the disease.
A 45-year-old man was admitted with recurrent epigastric pain for 10 days. The abdominal pain was mainly related to bloating with nausea, but no other associated symptoms. No particular signs were found on abdominal examination or laboratory testing. In 2003, a local distal expanded resection of the primary fibrosarcoma in the left chest wall was performed. Then, a left pneumonectomy was performed in 2017 due to diffuse metastases from the fibrosarcoma to the left lung. Enhanced computed tomography (CT) and magnetic resonance imaging of the upper abdomen suggested multiple masses of different sizes involving the head and tail of the pancreas; no local lymph node enlargement was noted. The postoperative pathologic diagnosis revealed a fibrosarcoma of the pancreas. A CT re-examination 6 mo postoperatively showed no local recurrence or distant metastases.
A fibrosarcoma is a rare low-grade malignant tumor, and metastases to the pancreas are even rarer. Patients with a history of a fibrosarcoma should consider the possibility of metastasis when a pancreatic neoplasm is demonstrated. Surgical resection is the preferred treatment.
Core tip: The literature focusing on cutaneous fibrosarcoma metastases to the pancreas is extremely limited. We report a 45-year-old male patient who underwent a distal local dilation resection of a primary fibrosarcoma in the left chest wall in 2003 and a left pneumonectomy for left pulmonary fibrosarcoma metastases in 2017. Magnetic resonance imaging has specific characteristics, thus facilitating assessment of the extent of tumor invasion and whether or not there are peripheral lymph node metastases, which can help develop a reasonable treatment strategy for surgeons. Surgical excision is an effective treatment.
- Citation: Cai HJ, Fang JH, Cao N, Wang W, Kong FL, Sun XX, Huang B. Dermatofibrosarcoma metastases to the pancreas: A case report. World J Clin Cases 2019; 7(20): 3316-3321
- URL: https://www.wjgnet.com/2307-8960/full/v7/i20/3316.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i20.3316
A fibrosarcoma is a low-grade malignant tumor with a local recurrence rate of 60%[1]. The incidence of distant metastases is <1%[2,3]. When fibrosarcomas metastasize to the pancreas, there are no apparent clinical symptoms in the early stage; however, when the mass increases in size, there may be symptoms of compression, such as gastrointestinal obstruction, jaundice, and abdominal pain, as well as a series of clinical symptoms, such as cachexia, in the late stage. Generally speaking, pancreatic metastases of malignant tumors and primary pancreatic cancer have a higher degree of malignancy and often invade peripheral blood vessels, viscera, and other tissues, thus making radical surgery difficult. Palliative chemotherapy is often adopted clinically[4]; however, this case illustrates that aggressive radical surgery is beneficial to long-term survival due to the low malignant characteristics of fibrosarcomas. Pre-operative magnetic resonance imaging (MRI) can more accurately detect lesions and assess the extent of tumor invasion, thus enabling the development of a reasonable therapeutic schedule. At present, most of the treatment methods adopted involve surgical resection, while the effect of adjuvant chemotherapy is still uncertain. Due to the small number of cases, there is no universally recognized standard for imaging diagnosis and treatment. Hence, we report a case of a dermatofibrosarcoma with metastases to the pancreas with the imaging findings and treatment mode, in order to provide reference for scholars and clinicians.
A 45-year-old man was admitted to hospital due to recurrent epigastric pain for 10 d.
The 45-year-old male patient underwent a distal local dilation resection of a primary fibrosarcoma of the left chest wall in 2003, and a left pneumonectomy in 2017 for left pulmonary fibrosarcoma metastases.
The family history was unremarkable.
No obvious abnormalities were noted on physical examination with the exception of slight tenderness in the upper abdomen.
No abnormalities were found on laboratory testing, including routine blood testing, liver function, blood amylase, and tumor markers.
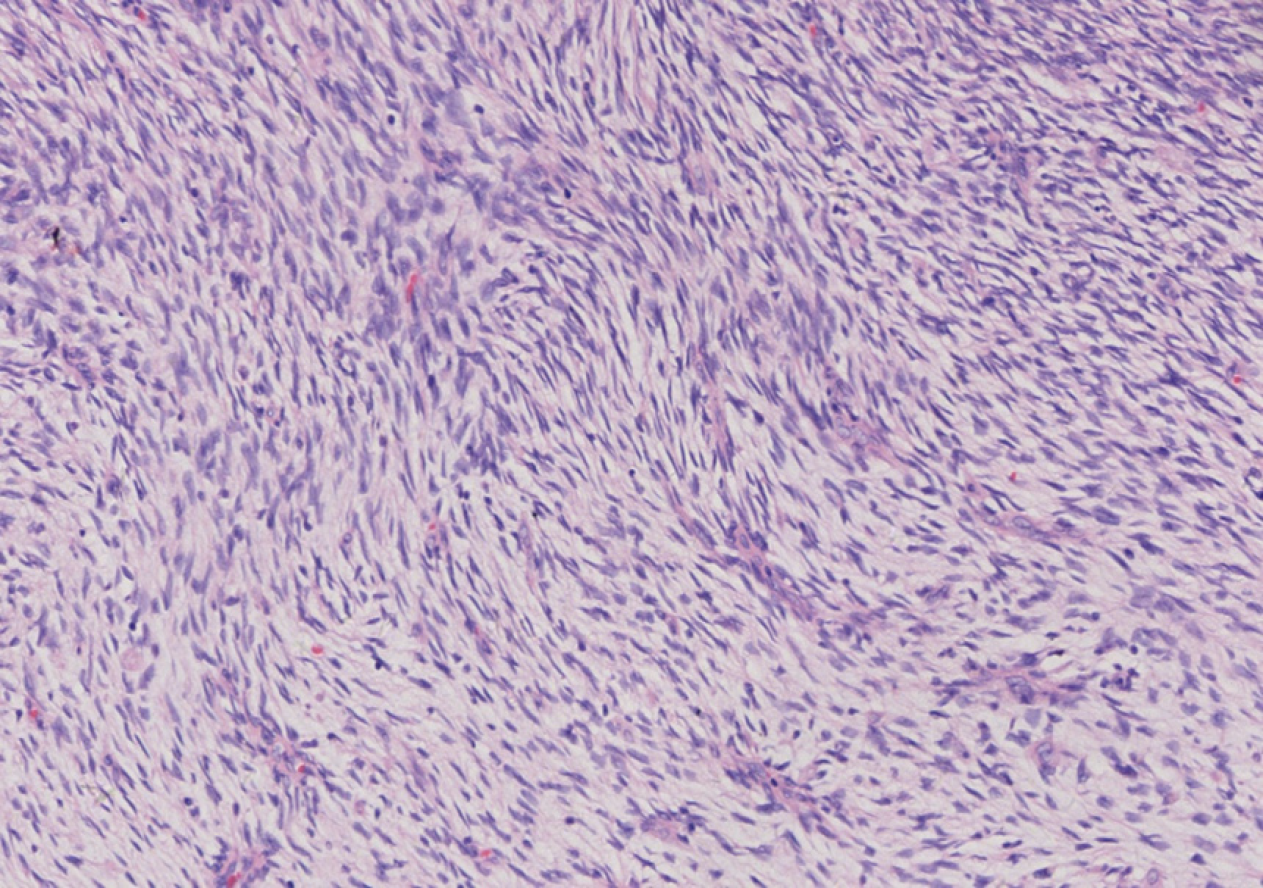
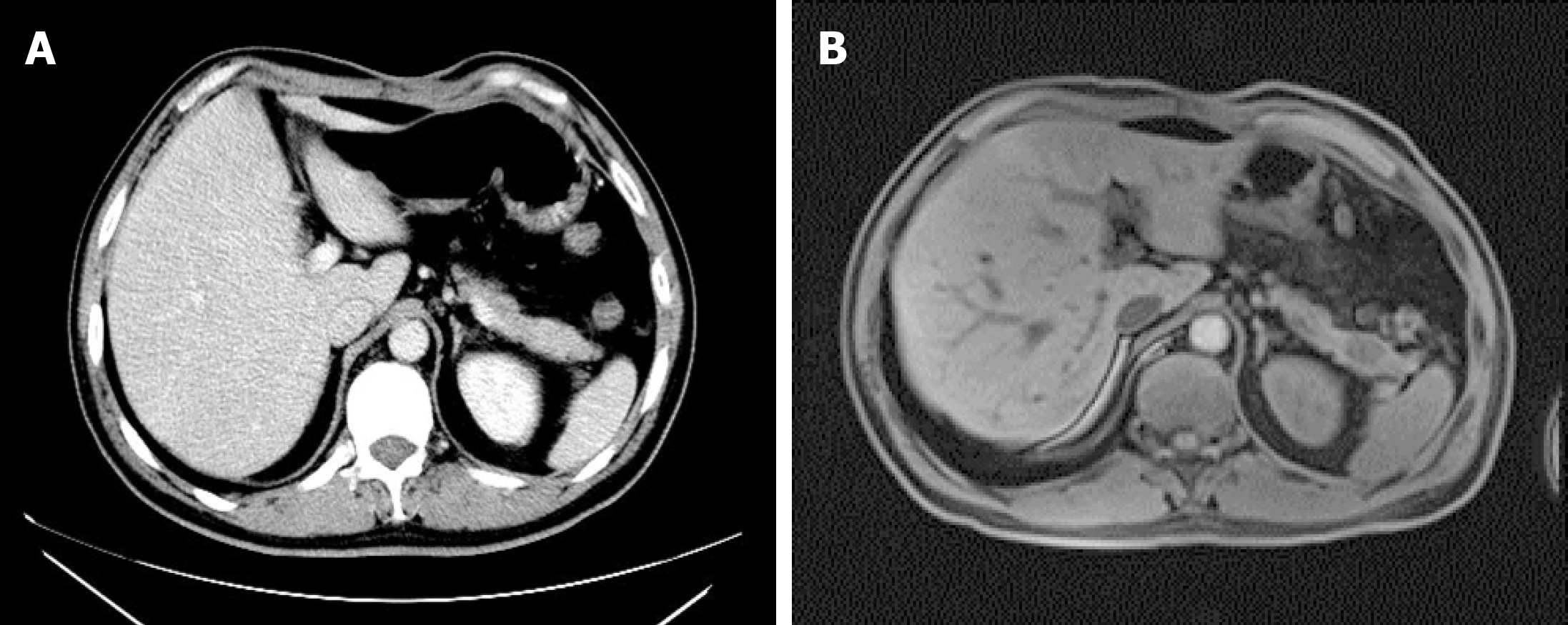
A computed tomography (CT) scan of the upper abdomen suggested a soft tissue mass, 4.8 cm × 3.0 cm in size, in the head of the pancreas, with an inhomogeneous density, unclear boundaries, and inhomogeneous enhancement (Figure 1A). Epigastric MRI showed that multiple masses of abnormal signals were visible in the pancreatic head and tail. The largest of which was located in the pancreatic head (approximately 4.8 cm in diameter), with an irregular shape that was hypointense on T1-weighted imaging (T1WI) (Figure 1B), slightly hyperintense on T2-weighted imaging (T2WI), and hyperintense on diffusion-weighted imaging (DWI) (Figure 1C). An enhanced MRI scan displayed progressive reinforcement at the edge of the mass, presenting spoke wheel-like enhancement (Figure 1D), and no significant expansion of the pancreatic duct. A CT scan and MRI revealed no local lymph node enlargement. The pathologic examination revealed that there were multiple fusiform interlobular tumors with abundant tumor cells interwoven within the matrix cells in the pancreas. The larger tumor (5 cm × 3 cm × 3 cm) was located in the pancreatic head. No tumor cells were found in the upper and lower margins or the bile duct margins. Immunohistochemical staining demonstrated the following in approximately 10% of tumor cells: Cytokeratin [-]; CD117 [-]; S-100 [-]; desmin [-]; smooth muscle actin [-]; CD34 [+]; vimentin [+]; and Ki-67 [+] (Figure 2). Thus, a final diagnosis of pancreatic fibrosarcoma was confirmed.
Pancreatic fibrosarcoma.
A Whipple's procedure and distal pancreatectomy with splenectomy were performed under general anesthesia. Multiple lesions were observed in the pancreas during the operation. The size of the mass in the head of the pancreas was 5 cm × 3 cm × 3 cm. The mass had a tough consistency with yellow liquid inside. The largest mass in the tail of the pancreas was 3 cm × 2 cm in size and invaded the capsule of the spleen. Intraoperative frozen section suggested a mesenchymal spindle cell tumor in the tail of the pancreas, consistent with metastatic fibrosarcoma. No obvious abnormality was found in the retroperitoneal lymph nodes. Considering that the left lung had been excised, the patient was transferred to intensive care unit (ICU) for observation.
After the Whipple's procedure and distal pancreatectomy with splenectomy were performed, the patient uneventfully recovered, without a local recurrence or distant transfer at the 6-mo follow-up.
A fibrosarcoma is a slow, soft tissue tumor with low malignant potential that makes up 10% of soft tissue sarcomas. Soft tissue sarcomas comprise only 1% of tumors. Fibrosarcomas mainly manifest in soft tissues, such as the limbs, the head and neck, and the abdominal cavity (mainly in the peritoneum)[5]. Dermatofibrosarcoma metastasis to the pancreas is extremely rare and was first reported by Atucha in 1960[6].
At present, the etiology of fibrosarcoma is unclear, but some scholars are of the opinion that this disease may be related to a history of the plague, trauma, radiation exposure, and a family history[7]. This disease occurs most often in the elderly, and the incidence between males and females is not significantly different. Pancreatic tumors, in the early stages, often have no obvious clinical symptoms; however, when the mass enlarges, it can compress local tissues and result in gastrointestinal obstruction, jaundice, and abdominal pain[8].
In the current case, MRI of the masses were hypointense on T1WI and slightly hyperintense on T2WI. They were mainly characterized by T2WI signals with spoke wheel-like enhancement at the edges of the masses. The spoke wheel-like enhancement of this case is consistent with the findings of Wang et al[9], who reported that such lesions usually exhibit peripheral enhancement and sometimes spoke wheel-like enhancement. The mechanism of enhancement has not been established. The enhancement may be related to the arrangement of collagen fibers within the tumor lesions, while the non-enhanced zone may be related to fibrous septations, cystic changes, or necrosis of the lesion. This disease should be distinguished from the following diseases. The first one is non-functional islet cell tumor (NFICE). Most NFICE patients have no clinical symptoms and are treated for compression. CT findings show that the tumor mass is large, at an average of 10 cm. The tumor density is not uniform, and liquefaction necrosis may occur, with some nodular calcification. MRI shows a sharp edge of the mass, hypointense on T1WI and hyperintense on T2WI, and obvious enhancement in the solid part of the mass. Solid false papilloma pseudopapillary tumor of the pancreas (SPTP) is also a differential diagnosis. SPTP, which is usually located in the head and tail of the pancreas, frequently occurs in young women. On CT, the mass presents a mixed density shadow, with hemorrhage and calcification within the tumor. MRI shows mixed signals in the mass, hypointense in the cystic part of T1WI, hyperintense in T2WI, and progressive moderate enhancement in the solid part. The third differential diagnosis is pancreatic cancer, which is a tumor with deficient blood supply. With CT enhancement, the tumor is not significantly strengthened and shows high malignancy and strong infiltration, and vague edges of the lesion, which often encroach on surrounding structures. It is worth mentioning that the enhanced CT scan of this case only showed irregular low-density masses in the head of pancreas, while the enhanced MRI suggested multiple signals of unequal soft tissue masses in the head and tail of the pancreas (Figure 3). Hence, MRI has a greater resolution of soft tissues. In the case of soft tissues, it is necessary to perform MRI enhancement before the operation. MRI enhancement provides more valuable information for surgeons to choose an optimal surgical approach. Although the spoke wheel-like enhancement of the mass is highly suggestive of a fibrosarcoma, it is ultimately confirmed by postoperative pathologic examination and immunochemical staining. The masses were generally not exquisite, having a fish-like appearance, in which the plane was pink and the cystic area was visible. The histologic characteristic was mainly the diffuse distribution of the tumor cells, which were interwoven with the matrix cells in which the blood vessels are abundant. At present, it is difficult to identify the sarcoma morphologically as a fibrosarcoma, but the expression of immunological markers, such as CD34, vimentin, and Ki-67, can help in the identification process.
CT and MRI enhancement in this case suggested a pancreatic malignancy without metastases to the lymph nodes. A Whipple's procedure and distal pancreatectomy with splenectomy were performed. Unlike pancreatic metastases from breast cancer[10], aggressive surgery for a resectable fibrosarcoma of the pancreas was indicated[11,12]. Debulking surgery prolongs long-term survival and controls local recurrence. Currently, radical surgery is considered the preferred treatment for localized fibrosarcomas[13].
When the tumor is transferred, it can be treated systemically, such as with chemotherapy and biological preparation; however, a fibrosarcoma is generally resistant to chemotherapy, the effect of which is still controversial, so that the patient does not receive further adjuvant chemotherapy. New research reveals that adjuvant chemotherapy may be beneficial[14], and the clinical trials of treatment, such as Oradin, have been shown to be effective. Based on phase 3 clinical trials, Oradin was a first-line treatment that has been classified by the United States as a high level or distant metastatic soft tissue sarcoma due to the good effect of Oradin combined with azithromycin in the second phase[15].
Generally, the severity of malignancy may be associated with the speed of metastasis. By comparison of the two metastatic events in this case, the second metastasis occurred faster. Hence, it is essential to have an increased clinical suspicion for a newly emerging fibrosarcoma. During the 6 months of follow-up, he recovered well without evidence of a local recurrence or newly distant metastases by abdominal CT re-evaluation; however, further long-term follow-up is needed.
Pancreatic fibrosarcoma is a rare malignant tumor of low malignant potential with a high local recurrence rate. It is essential to perform MRI enhancement before the operation and follow-up postoperatively. Surgery is the preferred treatment. Moreover, adjuvant chemotherapy also requires additional data for confirmation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fujino Y S-Editor: Gong ZM L-Editor: Wang TQ E-Editor: Liu MY
| 1. | Du K, Li J, Tang L, Lin X, Kong X, Liao X, Peng Q, Dong Y, He J, Huang Y, Zhang X, Lin F, Zhuang Q, Wu J. Role of postoperative radiotherapy in dermatofibrosarcoma protuberans: a propensity score-matched analysis. Radiat Oncol. 2019;14:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | van den Akker M, Angelini P, Taylor G, Chami R, Gerstle JT, Gupta A. Malignant pancreatic tumors in children: a single-institution series. J Pediatr Surg. 2012;47:681-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Llombart B, Serra C, Requena C, Alsina M, Morgado-Carrasco D, Través V, Sanmartín O. Guidelines for Diagnosis and Treatment of Cutaneous Sarcomas: Dermatofibrosarcoma Protuberans. Actas Dermosifiliogr. 2018;109:868-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Le DT, Picozzi VJ, Ko AH, Wainberg ZA, Kindler H, Wang-Gillam A, Oberstein P, Morse MA, Zeh HJ, Weekes C, Reid T, Borazanci E, Crocenzi T, LoConte NK, Musher B, Laheru D, Murphy A, Whiting C, Nair N, Enstrom A, Ferber S, Brockstedt DG, Jaffee EM. Results from a Phase IIb, Randomized, Multicenter Study of GVAX Pancreas and CRS-207 Compared with Chemotherapy in Adults with Previously Treated Metastatic Pancreatic Adenocarcinoma (ECLIPSE Study). Clin Cancer Res. 2019; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 167] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 5. | Colović R, Grubor N, Misev M, Jovanović M, Radak V. [Fibromyxoid sarcoma of the pancreas]. Srp Arh Celok Lek. 2008;136:158-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | ATUCHA. [Fibroblastic sarcoma of the pancreas]. Rev Esp Enferm Apar Dig Nutr. 1960;19:477-480. [PubMed] |
| 7. | Jo VY, Doyle LA. Refinements in Sarcoma Classification in the Current 2013 World Health Organization Classification of Tumours of Soft Tissue and Bone. Surg Oncol Clin N Am. 2016;25:621-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 8. | Miyazawa M, Naritaka Y, Miyaki A, Asaka S, Isohata N, Yamaguchi K, Murayama M, Shimakawa T, Katsube T, Ogawa K, Fujibayashi M. A low-grade myofibroblastic sarcoma in the abdominal cavity. Anticancer Res. 2011;31:2989-2994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Wang H, Nie P, Dong C, Li J, Huang Y, Hao D, Xu W. CT and MRI Findings of Soft Tissue Adult Fibrosarcoma in Extremities. Biomed Res Int. 2018;2018:6075705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Bednar F, Scheiman JM, McKenna BJ, Simeone DM. Breast cancer metastases to the pancreas. J Gastrointest Surg. 2013;17:1826-1831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Yokoyama Y, Murakami Y, Sasaki M, Morifuji M, Hayashidani Y, Kobayashi T, Sudo T, Sueda T. Pancreatic metastasis of dermatofibrosarcoma protuberans. J Gastroenterol. 2004;39:798-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Sperti C, Moletta L, Patanè G. Metastatic tumors to the pancreas: The role of surgery. World J Gastrointest Oncol. 2014;6:381-392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 100] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Madden C, Spector A, Siddiqui S, Mirkin G, Yim J, Hao X. Dermatofibrosarcoma Protuberans on Adult Toes: A Case Report and Review of the Literature. Anticancer Res. 2019;39:2105-2111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | ESMO/European Sarcoma Network Working Group. Soft tissue and visceral sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25 Suppl 3:iii102-iii112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 380] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 15. | Tap WD, Jones RL, Van Tine BA, Chmielowski B, Elias AD, Adkins D, Agulnik M, Cooney MM, Livingston MB, Pennock G, Hameed MR, Shah GD, Qin A, Shahir A, Cronier DM, Ilaria R, Conti I, Cosaert J, Schwartz GK. Olaratumab and doxorubicin versus doxorubicin alone for treatment of soft-tissue sarcoma: an open-label phase 1b and randomised phase 2 trial. Lancet. 2016;388:488-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 457] [Article Influence: 50.8] [Reference Citation Analysis (0)] |