Published online Jun 26, 2019. doi: 10.12998/wjcc.v7.i12.1444
Peer-review started: February 26, 2019
First decision: April 18, 2019
Revised: April 27, 2019
Accepted: May 2, 2019
Article in press: May 2, 2019
Published online: June 26, 2019
Processing time: 121 Days and 15.5 Hours
Currently, the findings about irisin as a novel myokine related to obesity are inconsistent in overweight/obese people. To our knowledge, no systematic analysis has been conducted to evaluate the relationship between irisin levels and overweight/obesity.
To evaluate the association between circulating irisin levels and overweight/obesity.
The Cochrane Library, MEDLINE, SCOPUS, and the ISI Web of Science were searched to retrieve all of the studies associated with circulating irisin levels and overweight/obesity. Standard mean difference values and 95% confidence intervals (CI) were estimated and pooled using meta-analysis methodology.
A total of 18 studies were included in our meta-analysis containing 1005 cases and 1242 controls. Our analysis showed that the circulating irisin level in overweight/obese people was higher than that in overall healthy controls (random effects MD = 0.63; 95%CI: 0.22-1.05; P = 0.003). In the subgroup analysis by ethnicity, the irisin level was higher in overweight/obesity people than that in controls in Africa (random effects MD = 3.41; 95%CI: 1.23-5.59; P < 0.05) but not in European, Asian, or American populations. In addition, in a subgroup analysis by age, the results showed that obese children exhibited a higher irisin level than controls (random effects MD = 0.86; 95%CI: 0.28-1.43; P < 0.05).
This meta-analysis provides evidence that circulating irisin is higher in obese individuals compared to healthy controls and it is important to identify the relationship between circulating irisin levels and overweight/obesity in predicting overweight/obesity.
Core tip: This study is the first meta-analysis that systematically assessed circulating irisin in overweight/obese people. This meta-analysis showed that circulating irisin levels were higher in obese individuals than in healthy controls. It also suggested that circulating irisin levels were higher in obese people in Africa than in controls. This meta-analysis further suggested that obese children exhibited a higher irisin level than controls.
- Citation: Jia J, Yu F, Wei WP, Yang P, Zhang R, Sheng Y, Shi YQ. Relationship between circulating irisin levels and overweight/obesity: A meta-analysis. World J Clin Cases 2019; 7(12): 1444-1455
- URL: https://www.wjgnet.com/2307-8960/full/v7/i12/1444.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i12.1444
The definition of obesity is the increase of fat mass which could cause serious health problems[1]. Guidelines of obesity treatment defined that body mass index (BMI) ≥ 25 is overweight and greater than 30 is obesity in adults. For children, age needs to be considered when defining overweight and obesity[2]. Over the past three decades, obesity has been a worldwide epidemic and a serious threat to human health for the steady rising of global obesity rate as well as no-declined prevalence rates[3]. Accumulating evidence suggests that overweight/obesity has been identified as an independent risk factor for chronic diseases, including metabolic syndrome, cardiovascular disease, and diabetes mellitus, leading to a negative effect on health-related quality of life and a heavy pressure on the health care system[4-6]. Hence, identification of overweight/obesity-oriented factors that are potential biomarkers that could be used to predict obesity and related complications is important.
It is well known that muscle tissues can secrete some cytokines and other peptides named myokines that are essential for maintaining metabolic homeostasis[7]. Irisin is a novel myokine produced by proteolytical cleavage of fibronectin type III domain-containing 5 (FNDC5) both in mice and humans, and it can also be secreted by adipose tissue and the liver in a small amounts[8]. Recent meta-analysis reported that circulating irisin levels were associated with polycystic ovary syndrome and coronary artery diseases[9,10], and it was considered a critical myokine related to body metabolism. Interestingly, irisin can promote white adipose tissue browning, which dissipates energy to produce heat and decreases the appearance of cellulite[11]. Recently, a growing number of studies suggested that circulating irisin levels in plasma or serum may be related to overweight/obesity in different groups of people[7]; however, this relationship remains controversial due to conflicting results that have been reported[12-18]. A clinical study involving 94 obese patients who participated in a weight loss program showed that obese subjects had a higher circulating irisin level than controls[12]. These findings are consistent with other studies[13-16]. Puzzlingly, although most studies support a role for irisin in forecasting obesity, several studies do not have a consistent trend and concluded that circulating irisin levels were lower in the obese group compared to the control group[17-19]. Moreover, in obese vs healthy children, boys, or girls, results regarding circulating irisin were also incompatible[20-22].
To our knowledge, no systematic analysis has been conducted to evaluate the relationship between irisin levels and overweight/obesity. As a result, the objective of this study was to analyze all of the available data to perform a quantitative assessment of the association and deepen our understanding of the role of circulating irisin levels in the development of obesity via a meta-analysis.
Databases including the Cochrane Library, PUBMED, and the ISI Web of Science were searched in English to identify studies published up to April 1, 2018, which addressed both irisin and overweight/obesity. Our overall search terms were irisin OR frcp2 OR fibronectin type III domain containing protein 5 OR fndc5 AND fat OR MS OR metabolic syndrome OR overweight/obesity. The reference lists of identified articles were also reviewed for more studies.
To be considered for the meta-analysis, the studies had to be case-control or cohort studies that reported irisin levels in overweight/obese patients compared with healthy controls regardless of age or gender. We incorporated overweight into the obese group. Conference abstracts were also included if they contained sufficient information to extract effect estimates. Literature reviews, articles of research on the drug, articles in which the mean and standard deviation (SD) could not be calculated, and studies with no healthy control group were excluded.
The titles and abstracts of all eligible studies were reviewed by two authors independently. To settle disagreements, a third author was consulted. The following information was collected from each study: The first author, publication year, study design, study location, numbers of cases and controls, age, BMI, types of blood sample, assays for irisin measurement, study quality, and circulating irisin levels (means and standard deviations).
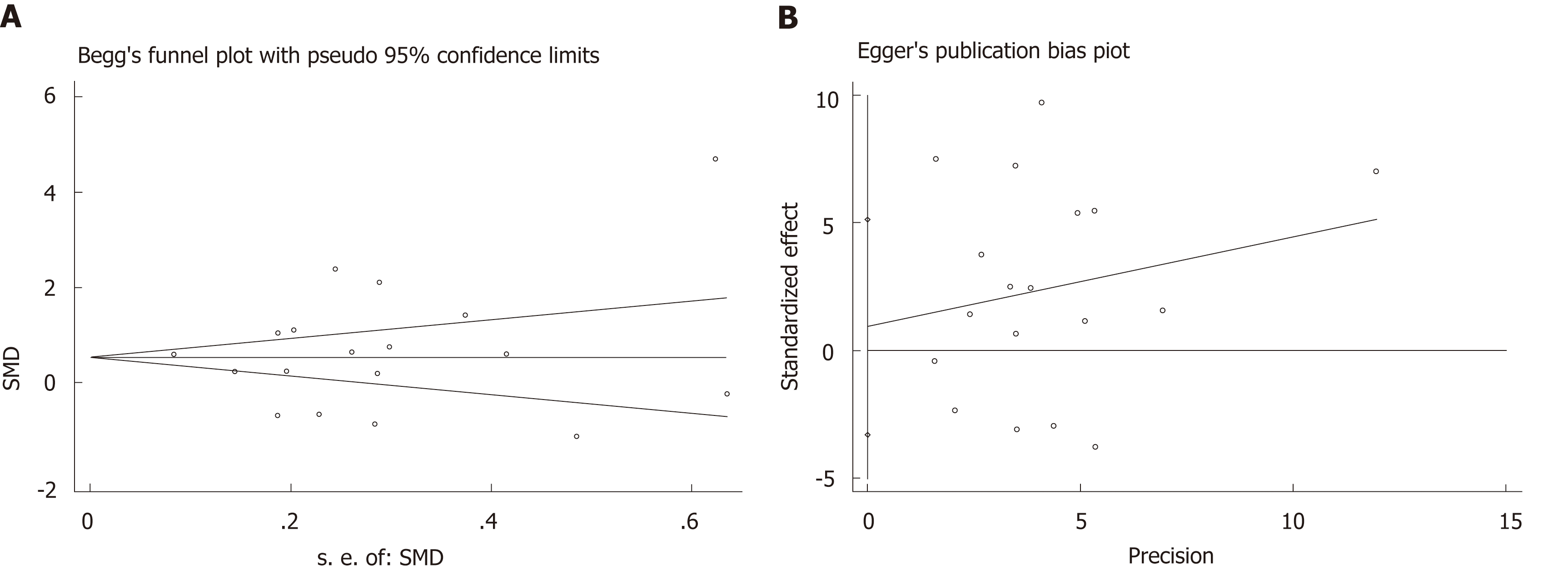
The primary variables, circulating irisin levels in patients with obesity, were reported as standard mean differences (SMD) and the corresponding 95% confidence intervals (CIs). The SMD for circulating irisin levels were calculated for all of the studies that were identified for the meta-analysis, and the results were combined using fixed- or random-effects modeling, as appropriate. Publication bias was assessed using Begg’s funnel plot and Egger’s test[22,23]. Heterogeneity in the results of the different studies was examined using χ2 tests for significance (a P-value < 0.1 was considered statistically significant) and the I2 test (I2 > 50%: significant heterogeneity; I2 < 25%: insignificant heterogeneity), which can be interpreted as the percentage of total variation across several studies owing to heterogeneity[24,25]. A sensitivity analysis was performed to assess whether the summary results had been significantly influenced by removing one study that investigated the association between circulating irisin levels and obesity. Subgroup analyses were conducted by geographic area and age. All statistical analyses were performed with Review Manager 5.2 and Stata version 11.0. P < 0.05 was considered statistically significant.
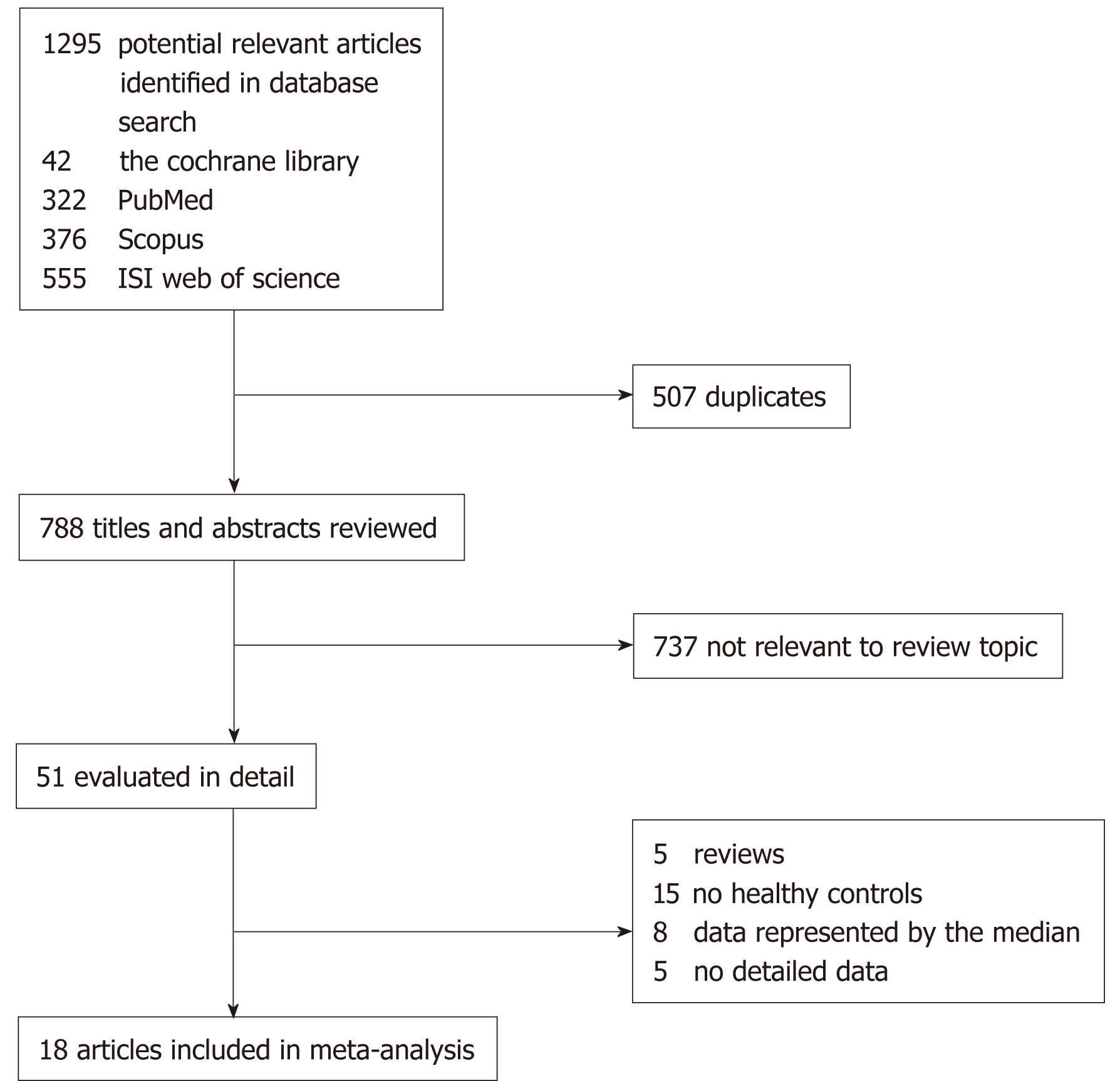
The literature search identified 1295 possible relevant articles. From these, 507 were duplicates, 788 were excluded after reading the title or abstract for obvious irrelevance, and 51 were finally included for further full-text evaluation. Of the 51 articles, five were excluded because they were reviews. Fifteen articles were excluded because they did not include healthy controls. Eight articles were excluded because data were represented by the median. Five articles were excluded because they did not contain detailed data. Finally, a total of 18 studies (1005 cases and 1242 controls) were included in our meta-analysis.
Figure 1 displays the flow chart describing the process of study inclusion/ex-clusion. Among the 18 studies, six were conducted in Europe, six in Asia, four in America, and two in Africa. The main characteristics of the included studies are presented in Table 1. Serum samples were used in 11 studies for irisin measurement, while plasma samples were used in the others. The sample size for each study ranged from 10 to 618. All of the irisin levels were measured with ELISA kits.
| Ref. | Country | Blood sample | Participants’ age, years (case-control) | Cases/controls, n | Irisin assay | BMI (kg/m2) (case-control) | ELISA kit |
| Moreno-Navarrete et al[7], 2013 | Spain | Plasma | 52.41 ± 10.99-47.28 ± 10.15 | 51/18 | ELISA | 28.98 ± 3.17-23.33 ± 1.2 | SK00170-01; Aviscera Bioscience Inc, Santa Clara, California |
| Stengel et al[13], 2013 | Germany | Plasma | 47.17 ± 11.91-48.5 ± 12.16 | 24/8 | ELISA | 50.63 ± 15.27-22.6 ± 2.55 | Phoenix Pharmaceuticals, Inc., Burlingame, CA, United States |
| Crujeiras et al[12], 2014 | Spain | Plasma | 49.4 ± 9.4-35.71 ± 8.8 | 94/48 | ELISA | 35.6 ± 4.5-22.9 ± 2.2 | Mercodia, AB (Uppsala, Sweden) |
| Hou et al[18], 2015 | China | Serum | 33 ± 9-31 ± 7 | 41/40 | ELISA | 30.8 ± 3.8-21.3 ± 1.8 | Phoenix Pharmaceuticals, Inc., Burlingame, CA, United States |
| Palacios-González et al[20], 2015 | Mexico | Serum | 9.07 ± 0.88-9.0 ± 0.86 | 60/25 | ELISA | -0.25 ± 0.67-2.11 ± 0.771 | CUSA-BIO BIOTECH |
| Viitasalo et al[26], 2016[26] | Finland | Plasma | 7.71 ± 0.4-7.6 ± 0.4 | 55/388 | ELISA | 20.21 ± 1.52-15.5 ± 1.3 | Phoenix Pharmaceuticals, Inc., Burlingame, CA, United States |
| Belviranli et al[17], 2016 | Turkey | Plasma | 34.40 ± 10.60-28.70 ± 6.82 | 10/10 | ELISA | 32.65 ± 3.04-23.00 ± 2.23 | BioVendor, Czech Republic |
| Chen et al[14], 2016 | China | Serum | 34.4 ± 7.6-32.8 ± 7.8 | 30/20 | ELISA | 33.3 ± 4.2-21.1 ± 2.0 | PHOENIX PHARMACEUTICAL |
| Fagundo et al[15], 2016 | Spain | Plasma | 44.49 ± 11.50-29.04 ± 6.22 | 65/49 | ELISA | 42.83 ± 6.63-21.61 ± 1.54 | EK-067-52; Phoenix Pharmaceuticals, INC, CA |
| Mehrabian et al[27], 2016 | Iran | Serum | 28.76 ± 4.67-29.23 ± 4.50 | 38/26 | ELISA | 22.26 ± 1.23-20.88 ± 1.28 | Biovendor, Laboratory Medicine, Modrice Czech Republic |
| Rizk et al[28], 2016 | Egypt | Serum | 45.45 ± 8.30-44.25 ± 10.46 | 20/20 | ELISA | 32.54 ± 1.80-22.85 ± 1.68 | BioVendor, Bmo, Czechrepublic (cat. No. RAG018R) |
| Shoukry et al[29], 2016 | Egypt | Serum | 47.06 ± 4.76-45.12 ± 4.72 | 119/31 | ELISA | 34.72 ± 5.68-23.27 ± 0.50 | BioVision, Milpitas, CA |
| Elizondo-Montemayor et al[21], 2017 | Mexico | Plasma | 8.0 (6–11)-8.5 (6-12) | 5/5 | ELISA | 98 (98-99)-66 (35-73) | Phoenix Pharmaceuticals, Inc., Burlingame, CA, United States |
| Jang et al[30], 2017 | South Korea | Serum | 13.7 ± 0.7-13.5 ± 0.5 | 248/370 | ELISA | 31.4 ± 3.8-19.4 ± 1.5 | Cat#EK-067-52; Phoenix, Pharmaceuticals, Belmont, CA |
| Liu et al[19], 2017 | China | Serum | 35.20 ± 6.51-35.01 ± 7.09 | 51/75 | ELISA | 27.80 ± 3.04-22.62 ± 2.52- | Bio Vision, Milpitas, CA95035, United States |
| Nigro et al[22], 2017 | Italy | Serum | 9.7 ± 2.7-8 ± 2.4 | 27/13 | ELISA | 2.7 ± 0.5-—0.46 ± 1.2 | Phoenix Pharmaceuticals, Belmont, CA, United States |
| Tibana et al[16], 2017 | Brazil | Serum | 66.5 ± 5.0-68.0 ± 6.2 | 26/23 | ELISA | 30.9 ± 3.1-24.3 ± 3.6 | MyBioSource Inc., San Diego, CA, United States |
| Sahin-Efe et al[31], 2018 | United States | Serum | 69.4 ± 8.6-69.5 ± 9.2 | 41/73 | ELISA | 30.5 (29.6–31.5)-24.0 (23.3–24.7) | CAT#EK-067-52; Phoenix Pharmaceuticals, Burlingame, CA |
There were nine studies utilizing irisin ELISA kits from Phoenix Pharmaceuticals (Burlingame, CA, United States), three from BioVendor (Brno, Czech Republic), two from Bio Vision (Milpitas, United States), and one each from CUSABIO Life Science (Wuhan, China), Bioscience (Santa Clara, California, United States), Mercodia AB (Uppsala, Sweden), and MyBioSource (San Diego, United States). The details of characteristics related to the included studies are shown in Table 1.
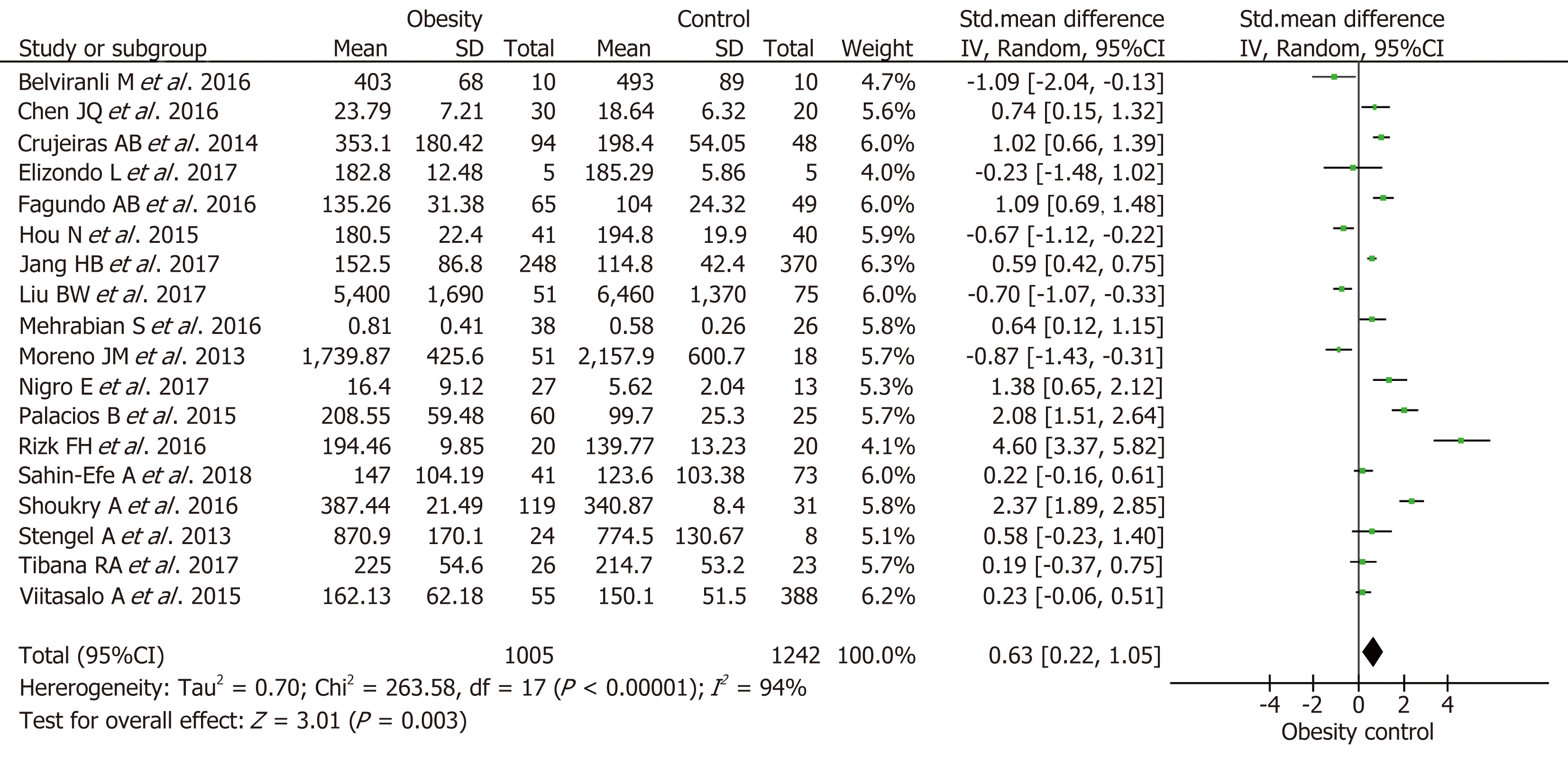
A meta-analysis of 18 studies involving a total of 2247 subjects (1005 cases and 1242 controls) was performed. Among them, four studies showed that obese individuals expressed lower irisin levels than healthy controls[7,17-19], while nine articles observed the opposite outcome where significantly higher irisin levels were exhibited in obese individuals compared to healthy controls. The results of the remaining four studies had no significance. Data were all described as the means ± SD. The P-value of heterogeneity between studies was significant (P < 0.05, Figure 2), so we used the random effects model and found that the overall effect was significant (random effects MD = 0.63; 95%CI: 0.22-1.05; P = 0.003). The effect size revealed that the irisin level was higher in obese people compared to healthy people.
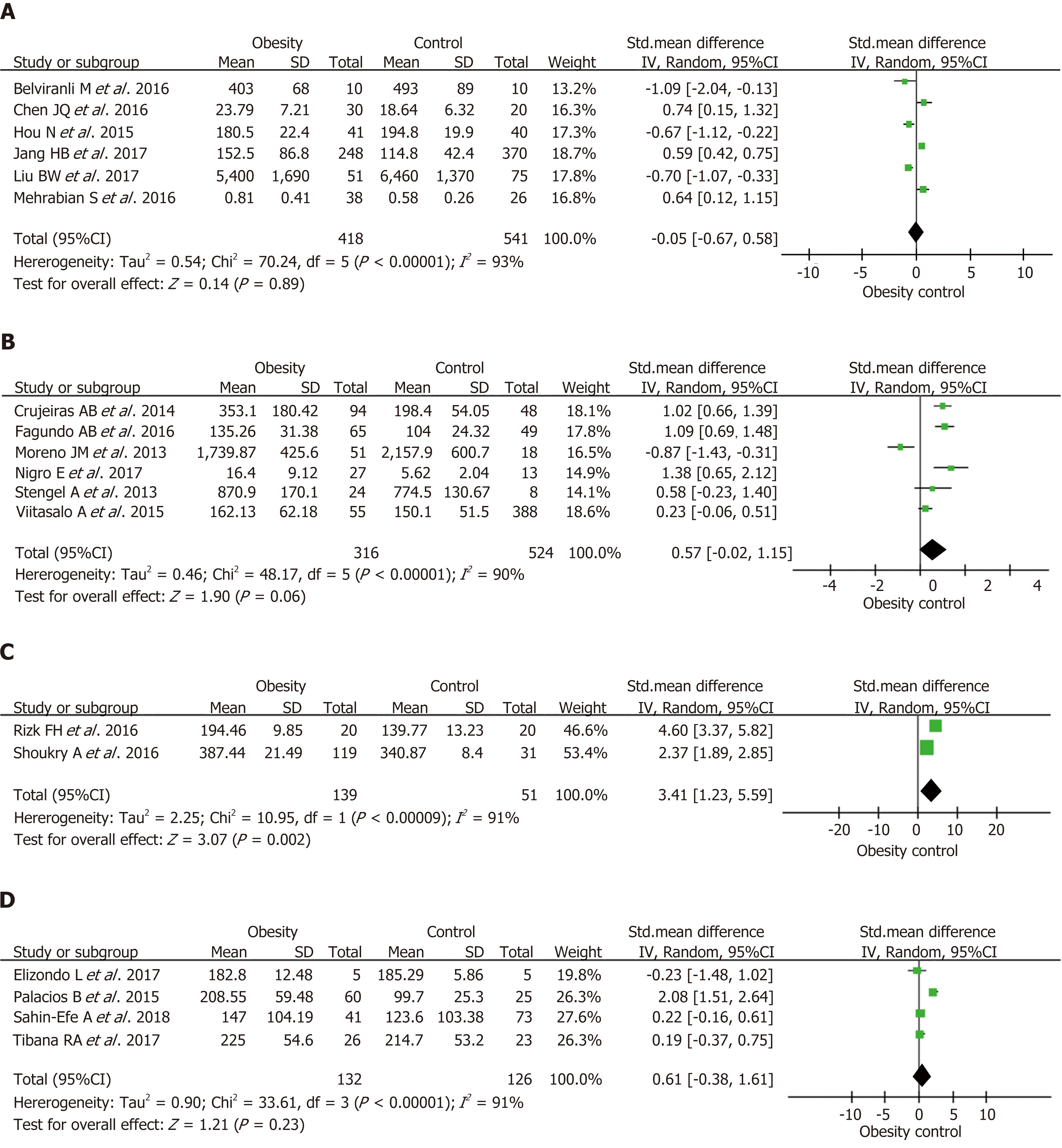
In the subgroup analysis by ethnicity, the irisin level was higher in obese people in Africa than in controls and the test for overall effect was significant (I2 = 91%; random effects MD = 3.41; 95%CI: 1.23-5.59; P < 0.05). While the irisin levels in European (I2 = 90%, random effects MD = 0.57; 95%CI: -0.02-1.15), Asian (I2 = 93%; random effects MD = -0.05; 95%CI: -0.67-0.58), and American populations (I2 = 91%; random effects MD = 0.61; 95%CI: -0.38-1.61) were not higher in obese individuals than in healthy controls, and the test for overall effect was not significant (P = 0.06, 0.89, and 0.31, respectively) (Figure 3).
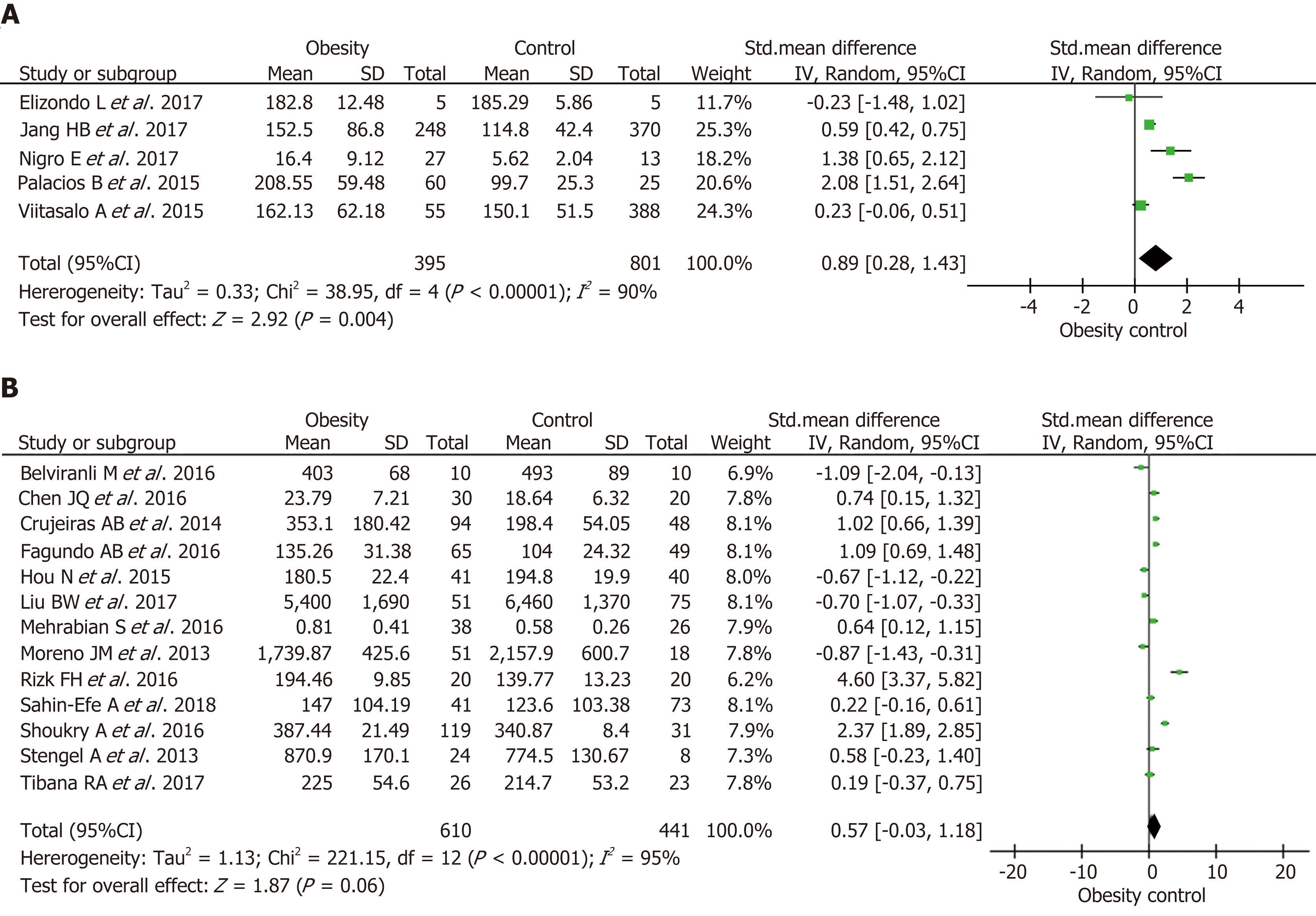
Furthermore, we performed a subgroup analysis by age. Five studies included children. Three of these studies suggested that obese children exhibited a higher irisin level than controls, and another two studies showed different outcomes. The P-value of heterogeneity between studies was significant (P < 0.05, Figure 4), then we used the random effects model and found that the overall effect was significant (random effects MD = 0.86; 95%CI: 0.28-1.43; P = 0.004). The effect size revealed that the irisin levels were higher in obese children than in controls. Conversely, the irisin levels in adult patients were not significantly different from controls and the total effect was not significant (I2 = 95%; random effects MD = 0.57; 95%CI: -0.03-1.18; P = 0.06) (Figure 4).
We omitted one study at a time and calculated the pooled SMD for the remainder of the studies to conduct a sensitivity analysis. There was no considerable change in the direction of the effect when omitting each of the studies.
We also conducted analyses by the Begg’s test and Egger’s test. Begg’s funnel plot had the expected funnel shape (Figure 5). Begg’s test (Z = 0.61, P = 0.544) and Egger’s test for publication bias (t = 0.46, P = 0.65) indicated that there was no publication bias in our analysis.
This meta-analysis showed that circulating irisin levels in obese individuals were higher than those in overall healthy controls. It also suggested that circulating irisin levels were higher in obese people than in healthy controls in Africa, while studies in other regions showed a negative result. This meta-analysis further suggested that obese children exhibited higher irisin levels than controls.
First, the overall result of this meta-analysis is positive that circulating irisin levels increased in obesity compared with health controls, although some studies did not draw the same conclusion. When it comes to underlying mechanisms, it is speculated that the rising circulating irisin level in obesity is an accommodative compensatory response to obesity-induced metabolic dysfunction, such as a decline of insulin levels or “irisin resistance”[32] as has already been established for leptin or insulin in obesity. Second, the results suggest that age may be a factor for the increasing circulating irisin levels in obese children compared to controls. It is deduced that diet habits and lifestyle are also related factors. Due to their growth and development needs, children differ from adults in the above-mentioned factors. In addition, there are other differences such as exercise and underlying diseases[33-37]. Recent studies explored that baseline irisin levels were lower in the old compared to the young participants for age-related decline in muscle function[38,39]. Third, in the subgroup analysis by ethnicity, the irisin level was only higher in obese individuals than in controls in Africa, while there were no significant differences in European, Asian, or American populations. These results indicate that genetic differences can influence specific hormone levels such as those of irisin. Weight stratification in the Asian population based on different BMI criteria from other regions may also lead to no significance of the subgroup analysis. Besides the above, gender is another interesting aspect. Murawska-Cialowicz et al[38] found that the level of irisin at baseline was higher in men than in women and after a 3-mo CrossFit training program, the changes of irisin level between women and men did not have a uniform trend[38], while in obese children, there was no evidence for differences of irisin levels between genders[37].
To our knowledge, this study is the first meta-analysis that systematically assessed circulating irisin in obese people, yet some limitations should be noted. First, in the above articles, how to choose the criteria to judge obesity is still in question. Although most studies chose to use BMI as the criterion of obesity, Mehrabian et al[27] suggested that body fat percentage is a better indicator of total adiposity compared to BMI for some individuals with normal weight obesity. Second, due to different methods, we cannot analyze whether the quality of serum or plasma samples has a decisive impact on the test results. For human FNDC5 does not have a canonical ATA translation start and some reports questioned that many human irisin antibodies used in commercial ELISA kits may lack necessary specificity[40], it is hard to determine the reliability of the results detected with the kits of many brands, although mass spectrometry has clearly demonstrated the existence of human irisin. Third, there were differences in the number of research subjects in different regions or countries; the majority of those surveyed were in Asia and Europe, while relatively few were in Africa. A larger sample survey is needed in the future for a more reliable result. Additionally, influences of the intensity and time of exercise on circulating irisin levels are also of interest, since irisin is a myokine associated with exercise. Future studies are required to investigate whether circulating irisin could predict the risk of obesity. Moreover, studies on the effects of exercise, lifestyle, and weight loss on the irisin level and related prospective studies are also needed.
In conclusion, our meta-analysis provides evidence that circulating irisin is higher in obese individuals compared to healthy controls and that circulating irisin levels seem to be affected by ethnicity and age. More investigations are necessary to clarify the association between the circulating irisin levels and overweight/obesity.
Overweight/obesity has been a global health challenge and irisin as a novel myokine is reported to play an important role in the development of metabolism dysfunction and obesity, however, the exact relationship between irisin and overweight/obesity remains unclear.
Many studies on the results of circulating irisin levels in overweight/obesity people are incon-sistent, which has puzzled us in confirming the role of irisin in overweight/obesity, thus, it is necessary to do such an analysis to clarify the relationship between them.
The main objective was to extract available data from studies and clarify the relationship between irisin and overweight/obesity.
We searched Cochrane Library, MEDLINE, SCOPUS, and the ISI Web of Science to retrieve all of the studies associated with circulating irisin levels and overweight/obesity. We estimated standard mean difference values and 95% confidence intervals and used meta-analysis methodology to get final results.
A total of 18 studies were included in this meta-analysis containing 1005 cases and 1242 controls. The overall analysis showed that the circulating irisin level in overweight/obese people was higher than that in overall healthy controls. In the subgroup analysis by ethnicity, the irisin level was higher in overweight/obese people than that in controls in Africa. In addition, in a subgroup analysis by age, the results showed that obese children exhibited a higher irisin level than controls. Studies of larger population samples are needed to better explore the relationship between irisin and overweight/obesity.
This study integrated the existing data to show that the circulating irisin levels in over-weight/obese people was higher than those in healthy controls overall, and explored the potential of irisin as a predictive factor for overweight/obesity.
More studies on the effects of exercise, lifestyle, and weight loss on the irisin level and related prospective studies are needed.
ORCID number: Jue Jia (0000-0003-1871-5015); Fan Yu (0000-0003-2009-3702); Wei-Ping Wei (0000-0002-2774-0354); Ping Yang (0000-0003-3555-847X); Ren Zhang (0000-0003-4783-5243); Yue Sheng (0000-0002-4001-6993); Yong-Qin Shi (0000-0002-7334-3130).
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Avtanski D, Hosseinpour-Niazi S S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Liu JH
| 1. | van der Klaauw AA, Farooqi IS. The hunger genes: pathways to obesity. Cell. 2015;161:119-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 266] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 2. | Ryan DH, Kahan S. Guideline Recommendations for Obesity Management. Med Clin North Am. 2018;102:49-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 117] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 3. | Kushner RF, Kahan S. Introduction: The State of Obesity in 2017. Med Clin North Am. 2018;102:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | El-Lebedy DH, Ibrahim AA, Ashmawy IO. Novel adipokines vaspin and irisin as risk biomarkers for cardiovascular diseases in type 2 diabetes mellitus. Diabetes Metab Syndr. 2018;12:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Polyzos SA, Anastasilakis AD, Efstathiadou ZA, Makras P, Perakakis N, Kountouras J, Mantzoros CS. Irisin in metabolic diseases. Endocrine. 2018;59:260-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 167] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 6. | Park KH, Zaichenko L, Brinkoetter M, Thakkar B, Sahin-Efe A, Joung KE, Tsoukas MA, Geladari EV, Huh JY, Dincer F, Davis CR, Crowell JA, Mantzoros CS. Circulating irisin in relation to insulin resistance and the metabolic syndrome. J Clin Endocrinol Metab. 2013;98:4899-4907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 366] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 7. | Moreno-Navarrete JM, Ortega F, Serrano M, Guerra E, Pardo G, Tinahones F, Ricart W, Fernández-Real JM. Irisin is expressed and produced by human muscle and adipose tissue in association with obesity and insulin resistance. J Clin Endocrinol Metab. 2013;98:E769-E778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 518] [Cited by in RCA: 566] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 8. | Polyzos SA, Kountouras J, Anastasilakis AD, Geladari EV, Mantzoros CS. Irisin in patients with nonalcoholic fatty liver disease. Metabolism. 2014;63:207-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 159] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 9. | Cai X, Qiu S, Li L, Zügel M, Steinacker JM, Schumann U. Circulating irisin in patients with polycystic ovary syndrome: a meta-analysis. Reprod Biomed Online. 2018;36:172-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Guo W, Zhang B, Wang X. Lower irisin levels in coronary artery disease: a meta-analysis. Minerva Endocrinol. 2017;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 11. | Boström P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, Rasbach KA, Boström EA, Choi JH, Long JZ, Kajimura S, Zingaretti MC, Vind BF, Tu H, Cinti S, Højlund K, Gygi SP, Spiegelman BM. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481:463-468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3682] [Cited by in RCA: 3492] [Article Influence: 268.6] [Reference Citation Analysis (0)] |
| 12. | Crujeiras AB, Pardo M, Arturo RR, Navas-Carretero S, Zulet MA, Martínez JA, Casanueva FF. Longitudinal variation of circulating irisin after an energy restriction-induced weight loss and following weight regain in obese men and women. Am J Hum Biol. 2014;26:198-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Stengel A, Hofmann T, Goebel-Stengel M, Elbelt U, Kobelt P, Klapp BF. Circulating levels of irisin in patients with anorexia nervosa and different stages of obesity--correlation with body mass index. Peptides. 2013;39:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 288] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 14. | Chen JQ, Fang LJ, Song KX, Wang XC, Huang YY, Chai SY, Bu L, Qu S. Serum Irisin Level is Higher and Related with Insulin in Acanthosis Nigricans-related Obesity. Exp Clin Endocrinol Diabetes. 2016;124:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Fagundo AB, Jiménez-Murcia S, Giner-Bartolomé C, Agüera Z, Sauchelli S, Pardo M, Crujeiras AB, Granero R, Baños R, Botella C, de la Torre R, Fernández-Real JM, Fernández-García JC, Frühbeck G, Rodríguez A, Mallorquí-Bagué N, Tárrega S, Tinahones FJ, Rodriguez R, Ortega F, Menchón JM, Casanueva FF, Fernández-Aranda F. Modulation of Irisin and Physical Activity on Executive Functions in Obesity and Morbid obesity. Sci Rep. 2016;6:30820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Tibana RA, da Cunha Nascimento D, Frade de Souza NM, de Souza VC, de Sousa Neto IV, Voltarelli FA, Pereira GB, Navalta JW, Prestes J. Irisin Levels Are not Associated to Resistance Training-Induced Alterations in Body Mass Composition in Older Untrained Women with and without Obesity. J Nutr Health Aging. 2017;21:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Belviranli M, Okudan N, Çelik F. Association of Circulating Irisin with Insulin Resistance and Oxidative Stress in Obese Women. Horm Metab Res. 2016;48:653-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Hou N, Han F, Sun X. The relationship between circulating irisin levels and endothelial function in lean and obese subjects. Clin Endocrinol (Oxf). 2015;83:339-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Liu BW, Yin FZ, Qi XM, Fan DM, Zhang Y. The Levels of Serum Irisin as a Predictor of Insulin Resistance in Han Chinese Adults with Metabolically Healthy Obesity. Clin Lab. 2017;63:881-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Palacios-González B, Vadillo-Ortega F, Polo-Oteyza E, Sánchez T, Ancira-Moreno M, Romero-Hidalgo S, Meráz N, Antuna-Puente B. Irisin levels before and after physical activity among school-age children with different BMI: a direct relation with leptin. Obesity (Silver Spring). 2015;23:729-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 21. | Elizondo-Montemayor L, Silva-Platas C, Torres-Quintanilla A, Rodríguez-López C, Ruiz-Esparza GU, Reyes-Mendoza E, Garcia-Rivas G. Association of Irisin Plasma Levels with Anthropometric Parameters in Children with Underweight, Normal Weight, Overweight, and Obesity. Biomed Res Int. 2017;2017:2628968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Nigro E, Scudiero O, Ludovica Monaco M, Polito R, Schettino P, Grandone A, Perrone L, Miraglia Del Giudice E, Daniele A. Adiponectin profile and Irisin expression in Italian obese children: Association with insulin-resistance. Cytokine. 2017;94:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10586] [Cited by in RCA: 12127] [Article Influence: 404.2] [Reference Citation Analysis (0)] |
| 24. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 40242] [Article Influence: 1437.2] [Reference Citation Analysis (2)] |
| 25. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46193] [Article Influence: 2099.7] [Reference Citation Analysis (3)] |
| 26. | Viitasalo A, Ågren J, Venäläinen T, Pihlajamäki J, Jääskeläinen J, Korkmaz A, Atalay M, Lakka TA. Association of plasma fatty acid composition with plasma irisin levels in normal weight and overweight/obese children. Pediatr Obes. 2016;11:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Mehrabian S, Taheri E, Karkhaneh M, Qorbani M, Hosseini S. Association of circulating irisin levels with normal weight obesity, glycemic and lipid profile. J Diabetes Metab Disord. 2016;15:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Rizk FH, Elshweikh SA, Abd El-Naby AY. Irisin levels in relation to metabolic and liver functions in Egyptian patients with metabolic syndrome. Can J Physiol Pharmacol. 2016;94:359-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Shoukry A, Shalaby SM, El-Arabi Bdeer S, Mahmoud AA, Mousa MM, Khalifa A. Circulating serum irisin levels in obesity and type 2 diabetes mellitus. IUBMB Life. 2016;68:544-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 30. | Jang HB, Kim HJ, Kang JH, Park SI, Park KH, Lee HJ. Association of circulating irisin levels with metabolic and metabolite profiles of Korean adolescents. Metabolism. 2017;73:100-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 31. | Sahin-Efe A, Upadhyay J, Ko BJ, Dincer F, Park KH, Migdal A, Vokonas P, Mantzoros C. Irisin and leptin concentrations in relation to obesity, and developing type 2 diabetes: A cross sectional and a prospective case-control study nested in the Normative Aging Study. Metabolism. 2018;79:24-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 32. | Perakakis N, Triantafyllou GA, Fernández-Real JM, Huh JY, Park KH, Seufert J, Mantzoros CS. Physiology and role of irisin in glucose homeostasis. Nat Rev Endocrinol. 2017;13:324-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 423] [Article Influence: 52.9] [Reference Citation Analysis (0)] |
| 33. | Kim HJ, Lee HJ, So B, Son JS, Yoon D, Song W. Effect of aerobic training and resistance training on circulating irisin level and their association with change of body composition in overweight/obese adults: a pilot study. Physiol Res. 2016;65:271-279. [PubMed] |
| 34. | Pathak K, Woodman RJ, James AP, Soares MJ. Fasting and glucose induced thermogenesis in response to three ambient temperatures: a randomized crossover trial in the metabolic syndrome. Eur J Clin Nutr. 2018;72:1421-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Daneshi-Maskooni M, Keshavarz SA, Mansouri S, Qorbani M, Alavian SM, Badri-Fariman M, Jazayeri-Tehrani SA, Sotoudeh G. The effects of green cardamom on blood glucose indices, lipids, inflammatory factors, paraxonase-1, sirtuin-1, and irisin in patients with nonalcoholic fatty liver disease and obesity: study protocol for a randomized controlled trial. Trials. 2017;18:260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 36. | Hron BM, Ebbeling CB, Feldman HA, Ludwig DS. Hepatic, adipocyte, enteric and pancreatic hormones: response to dietary macronutrient composition and relationship with metabolism. Nutr Metab (Lond). 2017;14:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Blüher S, Panagiotou G, Petroff D, Markert J, Wagner A, Klemm T, Filippaios A, Keller A, Mantzoros CS. Effects of a 1-year exercise and lifestyle intervention on irisin, adipokines, and inflammatory markers in obese children. Obesity (Silver Spring). 2014;22:1701-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 38. | Murawska-Cialowicz E, Wojna J, Zuwala-Jagiello J. Crossfit training changes brain-derived neurotrophic factor and irisin levels at rest, after wingate and progressive tests, and improves aerobic capacity and body composition of young physically active men and women. J Physiol Pharmacol. 2015;66:811-821. [PubMed] |
| 39. | Kim HJ, So B, Choi M, Kang D, Song W. Resistance exercise training increases the expression of irisin concomitant with improvement of muscle function in aging mice and humans. Exp Gerontol. 2015;70:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 120] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 40. | Jedrychowski MP, Wrann CD, Paulo JA, Gerber KK, Szpyt J, Robinson MM, Nair KS, Gygi SP, Spiegelman BM. Detection and Quantitation of Circulating Human Irisin by Tandem Mass Spectrometry. Cell Metab. 2015;22:734-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 411] [Article Influence: 41.1] [Reference Citation Analysis (0)] |