Published online Sep 16, 2016. doi: 10.12998/wjcc.v4.i9.302
Peer-review started: January 24, 2016
First decision: April 18, 2016
Revised: May 8, 2016
Accepted: July 14, 2016
Article in press: July 16, 2016
Published online: September 16, 2016
Processing time: 228 Days and 19 Hours
Gliosarcoma is rare central nervous system tumour and a variant of glioblastoma multiforme with bimorphic histological pattern of glial and sarcomatous differentiation. It occurs in elderly between 5th and 6th decades of life and extremely rare in children. It is highly aggressive tumour and managed like glioblastoma multiforme. A 12-year-old female child presented with complaints of headache and vomiting from 15 d and blurring of vision from 3 d. Magnetic resonance imaging of brain shows heterogeneous mass in right parieto-occipital cortex. A right parieto-occipito-temporal craniotomy with complete excision of mass revealed a primary glioblastoma on histopathological investigation. Treatment consists of maximum surgical excision followed by adjuvant radiotherapy. The etiopathogenesis, treatment modalities and prognosis is discussed. The available literature is also reviewed.
Core tip: We report a rare case of primary gliosarcoma right parieto-occipital cortex in a 12-year-old girl with review of available literature. The etiopathogenesis, treatment modalities and prognosis is discussed in view of the literature.
- Citation: Meena US, Sharma S, Chopra S, Jain SK. Gliosarcoma: A rare variant of glioblastoma multiforme in paediatric patient: Case report and review of literature. World J Clinical Cases 2016; 4(9): 302-305
- URL: https://www.wjgnet.com/2307-8960/full/v4/i9/302.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i9.302
Gliosarcoma was first time reported by Stroebe[1]. It is a rare cerebral tumour consist of bimorphic histological pattern of glial and sarcomatous differentiation. It is considered as grade 4 tumour according to WHO classification and variant of glioblastoma multiforme[2]. Incidence of gliosarcoma is 1.8%-2.8% of glioblastoma[3]. It usually affects elderly in 5th and 6th decades of life with slight male predominance and extremely rare in paediatric population[4]. So far only few cases of paediatric gliosarcoma have been reported. We report a case of primary gliosarcoma in 12-year-old girl.
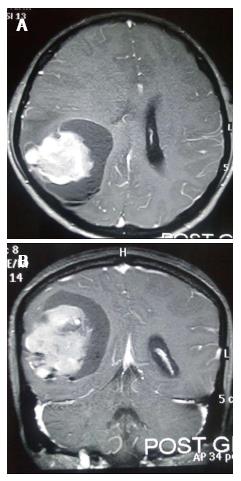
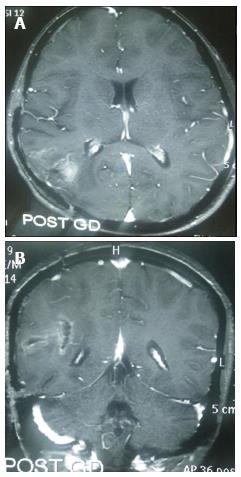
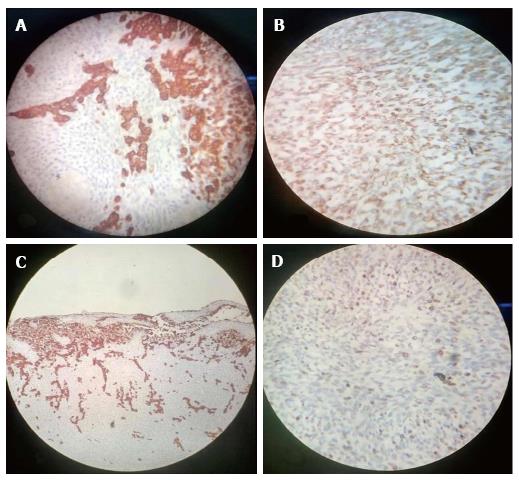
A 12-year-old girl was admitted in our institute with history of headache and vomiting from 15 d and blurring of vision from 3 d. Her general and systemic examination was unremarkable. Neurologically Glasgow coma scale was 15/15, pupil were equal and reactive bilaterally. Left side hemiparesis was present with 4/5 power in left upper and lower limb. CECT brain was done which shows large intra axial SOL in right parieto-occipital lobe with perifocal edema, producing mass effect, causing effaced adjacent sulci gyri and ipsilateral lateral ventricle. Lesion shows solid cystic component with intense enhancement after contrast. Midline shift of 8 mm to left side. MRI brain with GD shows similar findings (Figure 1). Antiedema measures were stared and early surgery was planned. She underwent right parieto-occipito-temporal craniotomy with complete excision of mass. Mass was greyish brown, avascular and firm in consistency. Post operative period was uneventful. Post operative MRI shows macroscopically complete excision of mass with reduction in mass effect and midline shift (Figure 2). Histopathological examination of the mass shows biphasic pattern comprising of alternating areas of mesenchymal and glial pattern. Mesenchymal component comprise of streaming spindle shape cells with nuclear atypia and many mitotic figures. At one focus pseudopalisading type of necrosis is also seen. In immunohistochemistry spindle shape cells show high MIB labelling index and vimentin positivity and glial cells shows GFAP positivity. Foci of reticulin-rich tumor cells also suggest sarcomatous component (Figure 3).
Patient was discharged on 7th post-operative day in good general and neurological condition with advice to attend radiotherapy clinic.
Gliosarcoma is a rare CNS tumour with incidence of 1.8%-2.8% of glioblastomas[3]. It usually occurs in elderly between 5th and 6th decades of life and extremely rare in paediatric population. Okami et al[5] reported eight cases of paediatric gliosarcoma, Sarkar et al[6] described three cases and Salvati et al[7] also reported three cases. Malde et al[8] reported one case of radiation induced gliosarcoma in literature.
Temporal lobe is most commonly involved followed by parietal and frontal lobe and can metastasize to extracranial structures like spinal cord, lung, pleura, liver, bone marrow and lymph nodes with increased frequency as compared to gliobastomas[7]. Pathogenesis of gliosarcoma is controversial topic and various studies have been proposed. The recent theory suggests monoclonal origin of gliosarcoma. The sarcomatous component originates from aberrant mesenchymal differentiation of the malignant glial cells during tumour progression[7]. Meis et al[9] laid down the criteria’s for the diagnosis of gliosarcoma on the basis of histological features: (1) the tumor should be bimorphic, and composed of two morphologically distinct populations of malignant cells (2) one component should be glial in nature with necrotic areas and must fulfil criteria adopted for defining glioblastoma (3) the sarcomatous component should resemble a spindle-cell sarcoma; and must fill one medium power field under (10 × objective with 10 × eyepiece).
The computed tomography findings of gliosarcoma is extremely variable and generally these lesions appear hyperdense mass with heterogeneous thick ring enhancement surrounded by intense peritumoural edema. On magnetic resonance imaging gliosarcoma appear as heterogeneous mass lesion in T1 and T2 weighted sequences with irregular contrast enhancement and intense peritumoural edema. Management of gliosarcoma consist of maximum surgical excision followed by adjuvant radiotherapy. The role chemotherapy in gliosarcoma is still poorly defined although Morantz et al[10] reported a slight improvement in survival. The average survival in gliosarcoma after diagnosis is less than one year (6 to 14.8 mo) with few case reports of long survivors[7,11]. Prognosis in gliosarcoma depends on histological and radiological features of mass lesion and is slightly better in lesions with predominant sarcomatous component along with meningioma like features in radiology[7].
In conclusion, Gliosarcoma is an aggressive tumor with propensity to recur and re-grow with poor outcome. Although it occurs more commonly in the 5th and 6th decades of life with temporal lobe predilection, but can occur in any age group or any region. Further studies are needed to understand the biphasic nature of these tumours.
Patient presented with h/o of headache, vomiting and blurring of vision.
She was conscious with left hemiparesis (4/5 power).
DD Includes malignant meningioma and central nervous system lymphoma and ruled out IHC marker studies.
All routine blood investigations (CBC, RFT, LFT and SE) were normal.
Contrast-enhanced computed tomography and magnetic resonance imaging GD Brain show heterogenous mass with intense contrast enhancement surrounded by peritumoural edema.
HPE shows biphasic pattern of mesenchymal(spindle cells) and glial cells. Glial cells show glial fibrilary acidic protein positivity while spindle cells shows vimentin positivity and high MIB index.
Microscopic complete excision of mass done. Patient was advised to attend radiotherapy clinic for adjuvant radiotherapy.
Salvati M, Lenzi J, Brogna C, Frati A, Piccirilli M, Giangaspero F, Raco A. Childhood’s gliosarcomas: pathological and therapeutical considerations on three cases and critical review of the literature. Childs Nerv Syst 2006; 22: 1301-1306; Gajendra Singh, Kuntal K. Das, Pradeep Sharma, B. Guruprasad, Sushila Jaiswal, Anant Mehrotra, Arun K. Srivastava, Rabi N. Sahu, Awadhesh K. Jaiswal, and Sanjay Behari:Cerebral gliosarcoma: Analysis of 16 patients and review of literature. Asian Journal Of Neurosurgery 2015; 10: 195-202.
Although it occurs more commonly in the 5th and 6th decades of life with temporal lobe predilection, but can occur in any age group or any region.
It is an interesting topic with only few case reports in literature.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Mocellin S, Yamagata M S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Stroebe H. Uber Entstehung und Bau der Gehirngliome. Beitr Pathol Anat Allg Pathol. 1895;18:405-486. |
| 2. | Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7079] [Cited by in RCA: 8038] [Article Influence: 446.6] [Reference Citation Analysis (0)] |
| 3. | Parekh HC, O’Donovan DG, Sharma RR, Keogh AJ. Primary cerebral gliosarcoma: report of 17 cases. Br J Neurosurg. 1995;9:171-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | di Norcia V, Piccirilli M, Giangaspero F, Salvati M. Gliosarcomas in the elderly: analysis of 7 cases and clinico-pathological remarks. Tumori. 2008;94:493-496. [PubMed] |
| 5. | Okami N, Kawamata T, Kubo O, Yamane F, Kawamura H, Hori T. Infantile gliosarcoma: a case and a review of the literature. Childs Nerv Syst. 2002;18:351-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Sarkar C, Sharma MC, Sudha K, Gaikwad S, Varma A. A clinico-pathological study of 29 cases of gliosarcoma with special reference to two unique variants. Indian J Med Res. 1997;106:229-235. [PubMed] |
| 7. | Salvati M, Lenzi J, Brogna C, Frati A, Piccirilli M, Giangaspero F, Raco A. Childhood’s gliosarcomas: pathological and therapeutical considerations on three cases and critical review of the literature. Childs Nerv Syst. 2006;22:1301-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Malde R, Jalali R, Muzumdar D, Shet T, Kurkure P. Gliosarcoma occurring 8 years after treatment for a medulloblastoma. Childs Nerv Syst. 2004;20:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Meis JM, Ho KL, Nelson JS. Gliosarcoma: a histologic and immunohistochemical reaffirmation. Mod Pathol. 1990;3:19-24. [PubMed] |
| 10. | Morantz RA, Feigin I, Ransohoff J. Clinical and pathological study of 24 cases of gliosarcoma. J Neurosurg. 1976;45:398-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 143] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Martin J, Devadoss P, Kannan K, Kumar Sundarraj S. Malignant pediatric gliosarcoma defies general survival data. Case Rep Med. 2014;2014:175679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |