Published online Jan 6, 2024. doi: 10.12998/wjcc.v12.i1.180
Peer-review started: October 7, 2023
First decision: November 22, 2023
Revised: November 29, 2023
Accepted: December 14, 2023
Article in press: December 14, 2023
Published online: January 6, 2024
Processing time: 87 Days and 1.6 Hours
Dilaceration is a rare dental developmental anomaly characterized by an abrupt deviation along the longitudinal axis of the root in which an angulation forms between the root and the crown. Here, we report on dilacerated bilateral maxi
A 10-year-old girl presented with a chief complaint of unerupted central incisors. An oral examination and radiography provided the basis for a diagnosis of dilaceration of the maxillary central incisors. After surgical exposure of the impacted teeth, a button with an attached chain was applied to the palatal surface of teeth 11 and 21. After 8 mo, a button was bonded to the labial surface of the crown to fix an elastic chain and move the teeth toward the maxillary arch. Finally, a fixed appliance was applied to tooth alignment to Class 1 malocclusion using a 0.019 × 0.025-inch nickel-titanium wire. After 3 years of follow-up, the clinical findings and radiographic assessment showed that the roots had developed with vital dental pulp and healthy periodontium, were acceptable aesthetically, and showed no resorption.
The rare occurrences of dilacerated bilateral maxillary central incisors can be successfully treated through surgical exposure and orthodontics.
Core Tip: Here, we report on a rare case of maxillary bilateral central incisors with severe root dilaceration in mixed dentition that we treated by surgical exposure followed by orthodontic treatment. The dilacerated teeth were successfully moved into the proper position with an aesthetically acceptable outcome at the three-year follow-up assessment. We also discuss the timing of and prognosis for treating dilacerated teeth.
- Citation: Wang JM, Guo LF, Ma LQ, Zhang J. Labial inverse dilaceration of bilateral maxillary central incisors: A case report. World J Clin Cases 2024; 12(1): 180-187
- URL: https://www.wjgnet.com/2307-8960/full/v12/i1/180.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i1.180
Dilaceration is a dental deformity characterized by an abrupt change in the axial angulation between the crown and the root of a tooth that may appear both in deciduous and permanent dentition. It causes severe aesthetic and subsequent psychological concerns for patients during the mixed dentition period[1,2]. The suspicion of dilacerated teeth is usually based on radiographic images, while treating a dilacerated tooth poses great challenges for clinicians due to its difficult positioning and abnormal root. The criteria for identifying root dilaceration in the recent literature vary. Some authors defined the longitudinal axis of the tooth to form an angle equal or greater than 90 degrees between the crown and the root, whereas others were inclined to define a deviation from the normal axis of 20 degrees or more in the apical part of the root[3].
The possible etiological factors for dilaceration include traumatic injury, developmental disturbances, and developmental syndromes. In preschool children, acute facial trauma is the most common cause. Thus, the impact of a blow can transfer vertically up to the unerupted germ, which displaces the calcifying part of the permanent germs and makes them angle with the rest of the germs[4]. The incisal edge of the successor tooth becomes displaced in the labial direction while the Hertwig’s epithelial root sheath continues to develop in its original place[5]. Finally, the crown of the permanent central incisor moves labially with root development. The extent of the disorder depends on the age of the patient suffering the trauma, the stage of development of the tooth, and the range of root resorption.
This paper reports a rare case of maxillary bilateral central incisors with severe root dilaceration in mixed dentition that we treated by surgical exposure followed by orthodontic treatment. The dilacerated teeth were successfully moved into the proper position with an aesthetically acceptable outcome at the three-year follow-up assessment. We also discuss the timing of and prognosis for treating dilacerated teeth.
A 10-year-old girl was brought to the Department of Endodontics at Anhui Medical University in China with a chief complaint of unerupted bilateral maxillary central incisors.
The patient presented to the Department of Endodontics, Anhui Medical University, China, with a chief complaint of unerupted central incisors.
The patient reported that she suffered maxillofacial trauma from a fall at the age of 5 years. The deciduous incisor underwent severe luxation, but no dental treatment was performed at the time.
The patient had a noncontributory personal and family history. Her general physical condition was healthy.
An intraoral examination showed the absence of tooth 11 and that tooth 21 presented with mesiolabial migration while the primary central incisors were present. Radiography revealed the germ of tooth 11 and that tooth 21 with root dilaceration and the crown pointed to the nasal cavity. Again, the patient’s general health condition was good, and she presented mixed dentition with Class I malocclusion.
The patient's blood test results were all normal.
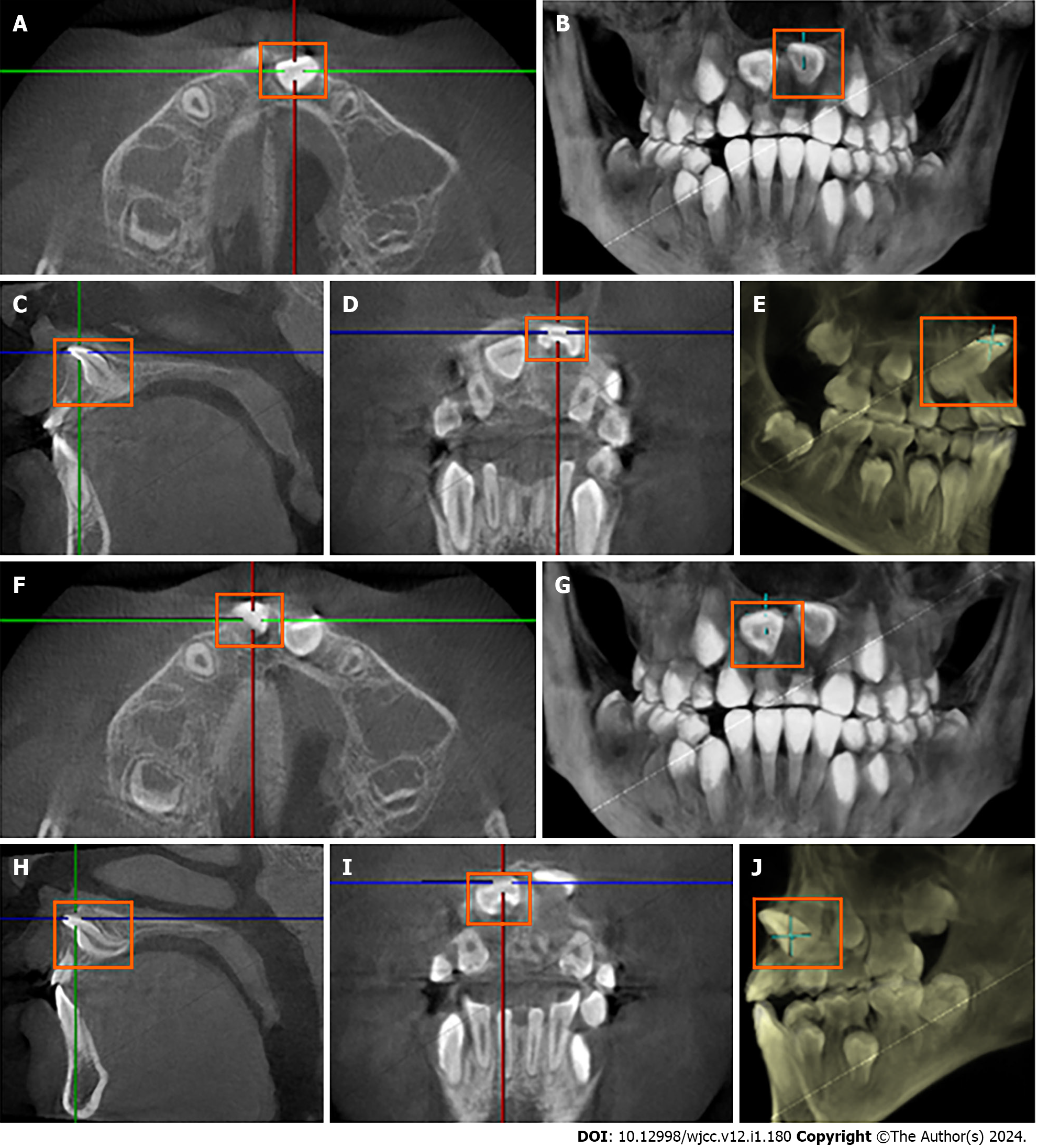
To assess the detailed three-dimensional positioning of the root, a cone-beam computed tomography (CBCT) scan was performed, which revealed that the roots of teeth 11 and 21 were positioned horizontally, with the crowns in the transverse position (Figure 1). The roots were dilacerated and the crowns were directed toward the nasal cavity. The root development was Nolla stage 9.
A diagnosis of severe dilacerated maxillary incisors was made.
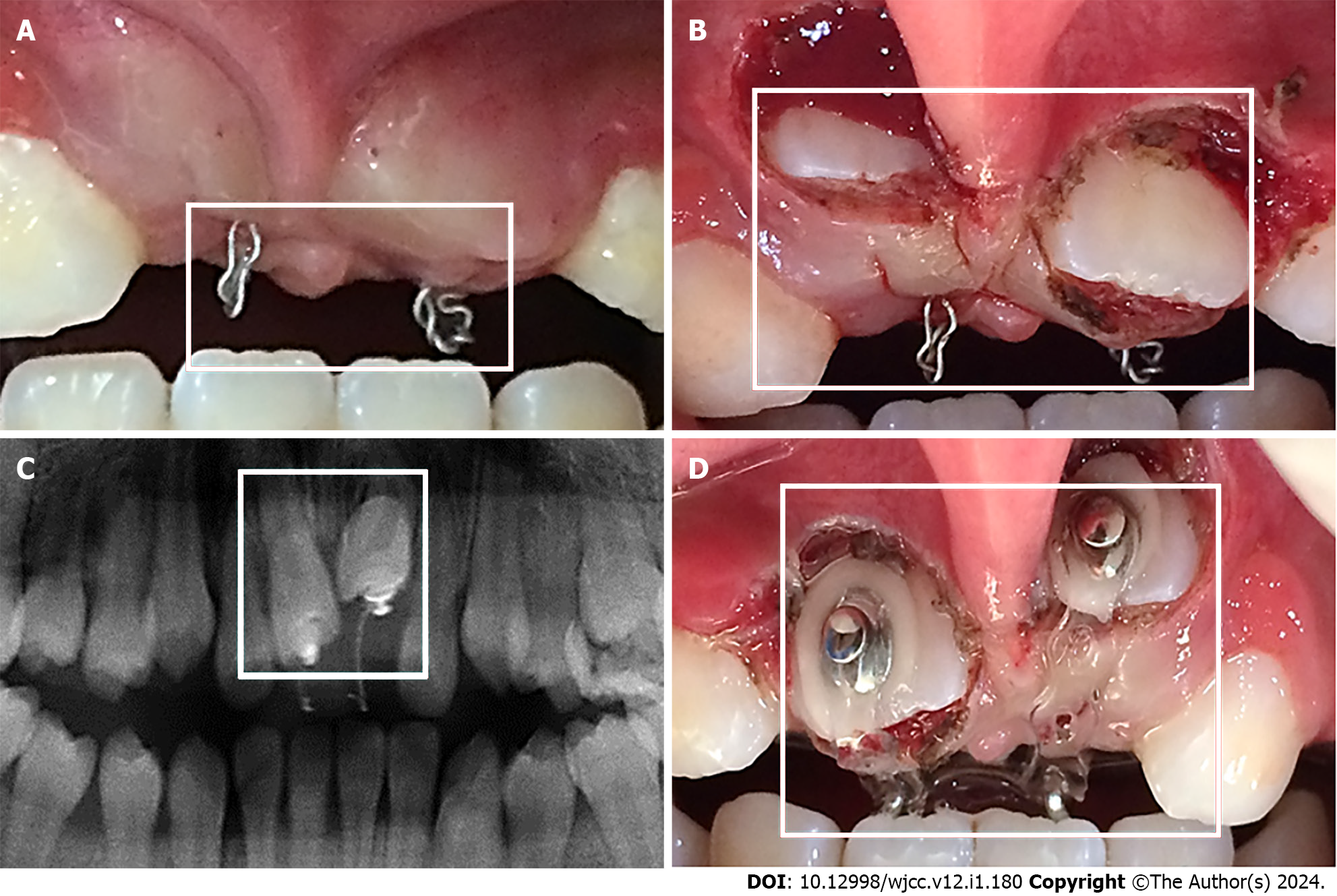
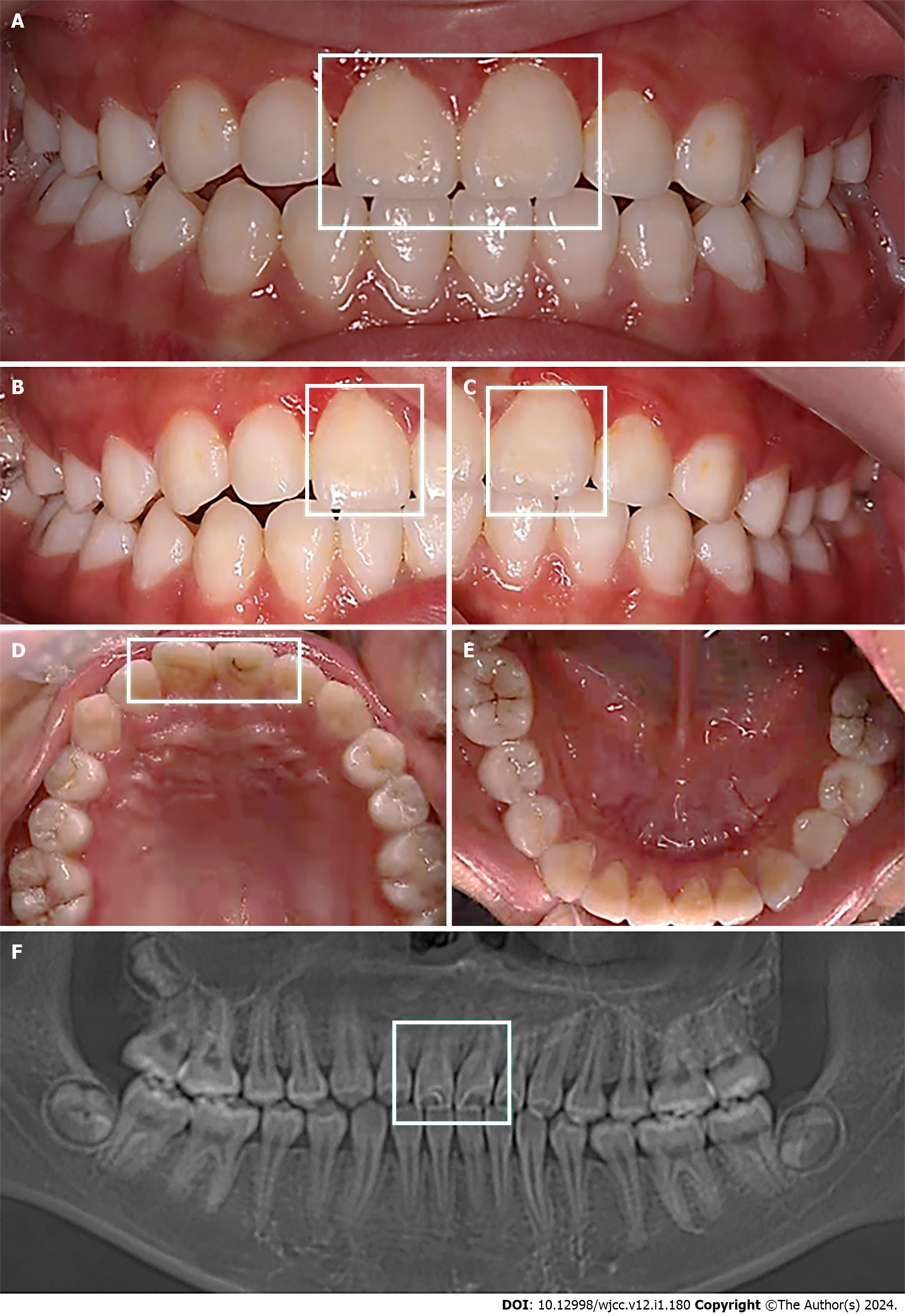
Because the patient’s parents refused extraction and strongly desired to preserve the teeth, surgical traction and orthodontic surgical treatment were selected as the method for correcting the axes of teeth 11 and 21. The parents were informed of the treatment plan, the risk of failure, and the possible complications. After the extraction of the primary incisors, a full-thickness triangular mucoperiosteal flap was raised to expose the palatal side of the dilacerated tooth while the patient was under local anesthesia. As shown in Figure 2A, a button with an attached chain was attached to the palatal surface of teeth 11 and 21. The elastic chain was secured to the maxillary arch and changed every month. The flap was repositioned and sutured with absorbable synthetic surgical sutures. After 8 mo, when the incisal edges of teeth 11 and 21 were transparent through the alveolar mucosa, the second surgery was performed (Figure 2B). A full-thickness flap was again made while the patient was under local anesthesia, and a button was bonded to the labial surface of the crown to fix an elastic chain (Figure 2C and D). The elastic chain was secured to the maxillary arch. The traction continued for 8 mo, during which the incisors were guided to the proper arch. A final fixed appliance was applied to the tooth alignment using a 0.019 × 0.025-inch nickel-titanium wire, and the patient was provided with a retainer and placed on a routine maintenance schedule at 3- to 6-mo intervals. The bilateral maxillary central incisors, which were impacted, have been correctly aligned with an acceptable gingival contour following crown exposure surgery and orthodontic traction. A significant improvement in the occlusal relationship was observed after debonding, as shown in Figure 3.
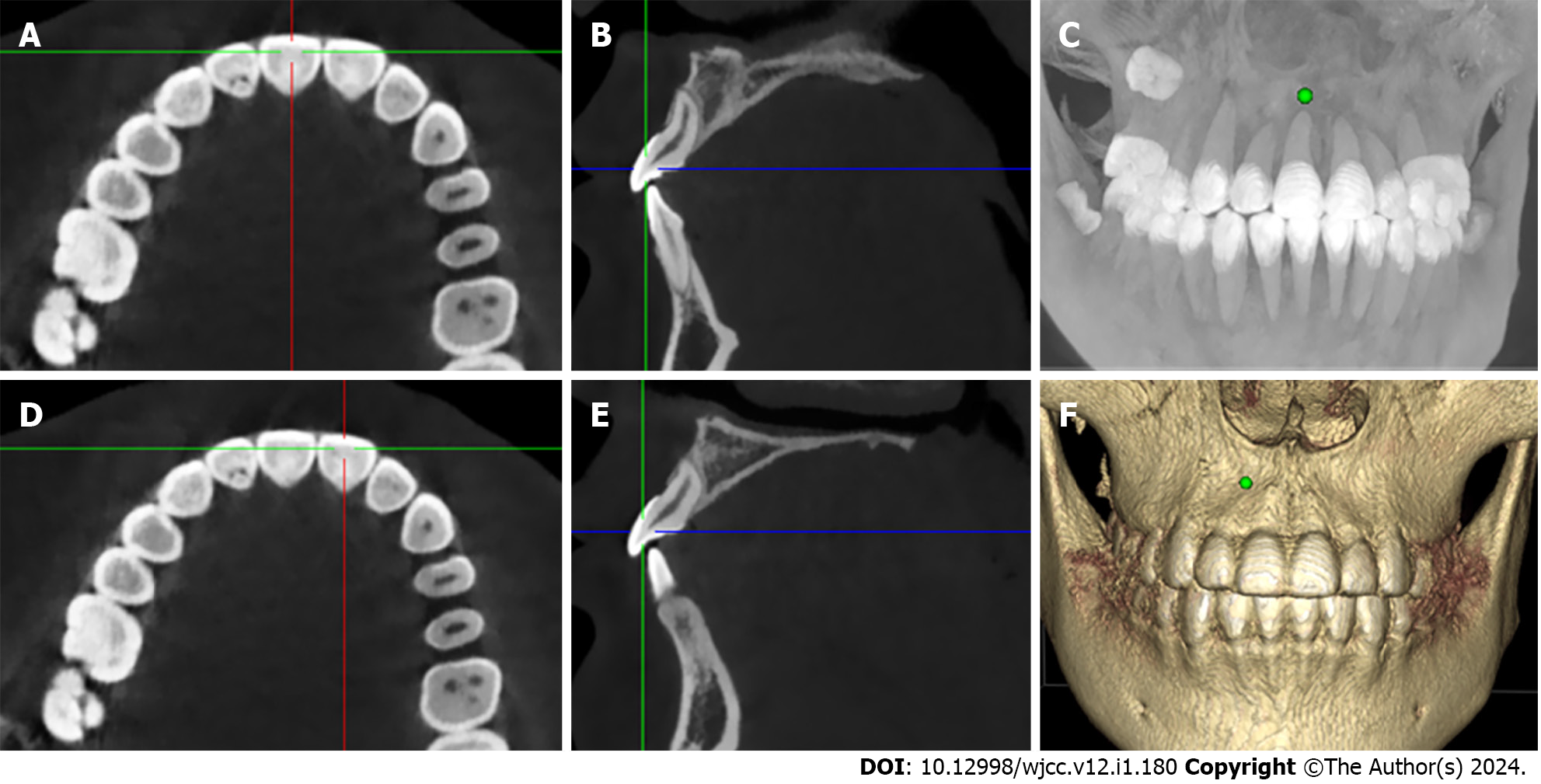
At the 3-year recall evaluation, the impacted bilateral maxillary central incisors were successfully positioned into properly aligned with an aesthetically acceptable gingival contour through the two-stage crown exposure surgery and orthodontic traction (Figure 4). Tipped molars and Class I malocclusion have been corrected, with no observable adverse effects. The final appearance of the teeth was aesthetically acceptable, and they functioned properly. No adverse effects were observed concerning pulp vitality, color change, or mobility. A CBCT scan showed that the closure apices of teeth 11 and 21 and the crowns were properly aligned and that the ideal overbite, overjet, and resolution of the insufficient incisal space had been achieved. There was proper alignment of the incisor root and normal lengths of the adjacent teeth. The dilacerated incisor root continued to mature during the post-treatment phase. The exposed incisor after completed treatment presented an acceptable gingival contour and attached gingiva after the completion of the treatment.
Crown dilacerations with palatal angulation are more prevalent in upper incisors. Hohayeb reported that upper incisors have a dilaceration frequency as high as 98%[6]. The etiological factors contributing to dilaceration are not fully understood. Traumatic dental injury frequently occurs before the eruption of the permanent teeth and is a widely accepted etiology for dilaceration of the anterior teeth among preschool children[7]. Approximately 1/4 (22.7%) of children has oral injuries before the age of 6 years[8]. The maxillary incisor bud, which is located palatally to the apex of the primary incisor, moves gradually upward and forward in a vestibular direction accompanied by resorption of the primary incisor root. The fibrous connective tissue between the primary maxillary incisor and the succedaneous tooth is less than 3 mm in thickness[9]. The narrow anatomical relationship can easily result in severe dilaceration when the primary tooth suffers an axial traumatic injury. Further, the axial impact results in permanent tooth crown displacement while the Hertwig’s epithelial sheath remains unaltered, maintaining its initial direction[1]. Therefore, an angle formed between the crown and the root. One study reported no gender difference in the prevalence of root dilaceration[2] while another reported a male-to-female ratio of 6:1[4]. Other researchers have found dilaceration in the posterior teeth, and this finding is inconsistent with the view that trauma is the major etiological factor[3]. Stewart studied 41 cases of dilacerated incisors and found that only 22% of the patients had a history of injury[10]. Idiopathic developmental disorder, facial clefting, and/or hereditary factors are suggested as potential factors when there is no clear evidence of traumatic injury[11].
If the roots bend mesially or distally, the dilaceration is evident on a periapical radiograph. However, if the dilaceration is towards the labial/buccal or palatal/lingual direction, the X-ray is difficult for diagnosis of root dilaceration. Besides, dilacerated root is difficult to differentiate from fused roots, condensing osteitis, or a dense bone island by X-ray. Therefore, CBCT is strongly recommended to evaluate the root toward palatal/lingual direction and assess the three-dimensional images of the root clearly. In addition, CBCT is benefit for assessing the thickness of the cortical and cancellous bone, and thus helps the dentist to choose the optimum treatment and prevent complications[12]. The radiation dose from CBCT is much lower than that of conventional CT[13]. Therefore, CBCT scans from a variety of angles are recommended to aid in the diagnosis, which can help to determine the exact location and angulation of the dilaceration.
The treatment of dilacerated incisors requires a multidisciplinary approach involving two main therapies beginning with the extraction of the affected teeth followed by prosthetic restoration. Alternatively, when the parents of preschool children reject extraction because of the emotional problems associated with the loss of the anterior teeth, successful treatment of impacted central incisors with surgical exposure followed by orthodontic traction has been demonstrated in previous studies by Bayram et al[14] and Pinho et al[15]. No consensus has emerged among researchers in this regard, with many preferring to preserve the impacted permanent tooth and achieving satisfactory results in cases in which this approach is appropriate. Hu et al[16] evaluated 12 patients with inversely maxillary immature central incisors and found continuous development of the impacted teeth with the same roots, with the length and apical size being the same as normally erupted contralateral incisors and no further alveolar bone loss in the 24-mo follow-up period[16].
The success rate for the combined surgical-orthodontic treatment of dilacerated teeth depends largely on the maturity of the root, the position and inclination of the impacted tooth, and the adequate space for the infected tooth[17,18]. Most frequent complications resulting from forced extraction of impacted teeth with dilacerated root and inverted or horizontal crown were as follows: Ankylosis, loss of attachment, external root resorption, pulp necrosis, pulp canal obliteration, crown discoloration, root exposure, and unaesthetic gingival margin[17,19,20].
During the treatment, the excessive bending angle may affect the adjacent lateral incisor or penetrate the labial mucosa and damage the periodontal tissue[21]. McNamara et al[22] emphasized that the integrity of the Hertwig’s epithelial sheath is decisive, playing a crucial role in the continuous development of and prognosis for a dilacerated tooth[22]. The prognosis is relatively good for a dilacerated tooth with an immature root apex, obtuse angulation, and a more occlusal position in the alveolar crest[18]. The treatment period increases with the patient’s age; thus, late mixed and full permanent dentition requires lengthy surgical-orthodontic treatment. Therefore, early orthodontic intervention treatment is recommended to create more space for root formation and enhance the benefits of further treatment. Its treatment poses great challenges in terms of restoring the aesthetic appearance aspect without damaging the adjacent teeth or periodontal tissue.
The present case study demonstrated the successful treatment of bilateral maxillary central incisors with severe root dilaceration through surgical exposure and orthodontic treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Domínguez AI, Mexico S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Yu HG
| 1. | Salek F, El Idrissi I, El Alloussi M, Zaoui F, Azaroual MF. Corono-radicular dilaceration of a maxillary central incisor: A case report. Int Orthod. 2019;17:606-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Shi X, Sun X, Wang X, Zhang C, Liu Y, Quan J, Zheng S. The effect of the root dilaceration on the treatment duration and prognosis of unilateral impacted immature maxillary central incisors. Am J Orthod Dentofacial Orthop. 2023;163:79-86. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Jafarzadeh H, Abbott PV. Dilaceration: review of an endodontic challenge. J Endod. 2007;33:1025-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Topouzelis N, Tsaousoglou P, Pisoka V, Zouloumis L. Dilaceration of maxillary central incisor: a literature review. Dent Traumatol. 2010;26:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Qutieshat A, Al Harthy N, Javanmardi S, Singh G, Chopra V, Aouididi R, Al Hanashi O, Al Arabi A. Prevalence of mesio-distal dilaceration in patients presenting for initial orthodontic care: A retrospective study. J Orthod Sci. 2023;12:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Chohayeb AA. Dilaceration of permanent upper lateral incisors: frequency, direction, and endodontic treatment implications. Oral Surg Oral Med Oral Pathol. 1983;55:519-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Mo SE, Kim JG, Yang YM, Lee DW. Impaction of multiple dilacerated primary incisors: a case report. J Clin Pediatr Dent. 2023;47:104-110. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Day PF, Flores MT, O'Connell AC, Abbott PV, Tsilingaridis G, Fouad AF, Cohenca N, Lauridsen E, Bourguignon C, Hicks L, Andreasen JO, Cehreli ZC, Harlamb S, Kahler B, Oginni A, Semper M, Levin L. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent Traumatol. 2020;36:343-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 9. | Walia PS, Rohilla AK, Choudhary S, Kaur R. Review of Dilaceration of Maxillary Central Incisor: A Mutidisciplinary Challenge. Int J Clin Pediatr Dent. 2016;9:90-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | de Amorim CS, Americano GCA, Moliterno LFM, de Marsillac MWS, Andrade MRTC, Campos V. Frequency of crown and root dilaceration of permanent incisors after dental trauma to their predecessor teeth. Dent Traumatol. 2018;34:401-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Stewart DJ. Dilacerate unerupted maxillary central incisors. Br Dent J. 1978;145:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Nallanchakrava S, Mettu S, Reddy NG, Jangam K. Multidisciplinary Approach for the Management of Dilacerated Permanent Maxillary Incisor: A Case Report. Int J Clin Pediatr Dent. 2020;13:725-728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Chaushu S, Becker T, Becker A. Impacted central incisors: factors affecting prognosis and treatment duration. Am J Orthod Dentofacial Orthop. 2015;147:355-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Bayram M, Ozer M, Sener I. Bilaterally impacted maxillary central incisors: surgical exposure and orthodontic treatment: a case report. J Contemp Dent Pract. 2006;7:98-105. [PubMed] [DOI] [Full Text] |
| 15. | Pinho T, Neves M, Alves C. Impacted maxillary central incisor: surgical exposure and orthodontic treatment. Am J Orthod Dentofacial Orthop. 2011;140:256-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Hu H, Hu R, Jiang H, Cao Z, Sun H, Jin C, Sun C, Fang Y. Survival of labial inversely impacted maxillary central incisors: A retrospective cone-beam computed tomography 2-year follow-up. Am J Orthod Dentofacial Orthop. 2017;151:860-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Uematsu S, Uematsu T, Furusawa K, Deguchi T, Kurihara S. Orthodontic treatment of an impacted dilacerated maxillary central incisor combined with surgical exposure and apicoectomy. Angle Orthod. 2004;74:132-136. [PubMed] [DOI] [Full Text] |
| 18. | Chew MT, Ong MM. Orthodontic-surgical management of an impacted dilacerated maxillary central incisor: a clinical case report. Pediatr Dent. 2004;26:341-344. [PubMed] |
| 19. | Kuvvetli SS, Seymen F, Gencay K. Management of an unerupted dilacerated maxillary central incisor: a case report. Dent Traumatol. 2007;23:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Bhikoo C, Xu J, Sun H, Jin C, Jiang H, Hu R. Factors affecting treatment duration of labial inversely impacted maxillary central incisors. Am J Orthod Dentofacial Orthop. 2018;153:708-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Kim KA, Hwang HS, Chung KR, Kim SH, Nelson G. Recovery of multiple impacted maxillary teeth in a hyperdivergent Class I patient using Temporary Skeletal Anchorage Devices and augmented corticotomy. Angle Orthod. 2018;88:107-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | McNamara T, Woolfe SN, McNamara CM. Orthodontic management of a dilacerated maxillary central incisor with an unusual sequela. J Clin Orthod. 1998;32:293-297. [PubMed] |