Published online Feb 6, 2023. doi: 10.12998/wjcc.v11.i4.859
Peer-review started: August 30, 2022
First decision: December 9, 2022
Revised: January 2, 2023
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 6, 2023
Processing time: 159 Days and 17.1 Hours
A rectal neuroendocrine tumor (rNET) is a malignant tumor originating from neuroendocrine cells. Currently, tumor size is the primary basis for assessing tumor risk.
This article reports the case of a 46-year-old male patient who underwent a colonoscopy that found a 3 mm rectal polypoid bulge. The pathological exam
Despite the presence of lymphatic invasion and extremely small diameter rNETs in our case, this phenomenon may not imply a higher risk of distant lymph node and organ metastasis.
Core Tip: Due to the heterogeneity and atypical symptoms of rectal neuroendocrine tumors, in the process of clinical diagnosis and treatment, it is not sufficient to judge the risk of tumor metastasis based only on tumor size and lymphovascular invasion. Therefore, during treatment, it is necessary to formulate an individualized plan, undertake close follow-up observation, and try to improve the quality of life and disease prognosis of patients while reducing the burden of treatment.
- Citation: Ran JX, Xu LB, Chen WW, Yang HY, Weng Y, Peng YM. Is lymphatic invasion of microrectal neuroendocrine tumors an incidental event?: A case report. World J Clin Cases 2023; 11(4): 859-865
- URL: https://www.wjgnet.com/2307-8960/full/v11/i4/859.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i4.859
A rectal neuroendocrine tumor (rNET) is a rectal malignancy that originates from neuroendocrine cells with an insidious onset and a lack of specific first symptoms[1]. In recent years, with the extensive development of colon cancer screening programs and the improvement of endoscopic diagnosis and treatment techniques, the incidence of rNET has increased annually[2]. The incidence of rNET has increased nearly 10 times in the past 30 years, indicating that this type of tumor may not be uncommon[3]. Clinically, rNETs are usually found during endoscopy, the vast majority are 10 mm or less in diameter[4]. According to the European Neuroendocrine Tumor Society guidelines, tumor size greater than 20 mm is a risk factor for tumor invasion and metastasis, but vascular invasion, lymph node metastasis, and distant metastasis may also occur in the case of smaller tumors[5,6]. Currently, for rNETs with a tumor size of 10 mm or less, existing treatment guidelines recommend radical surgery and, in the presence of definite vascular invasion, additional lymph node dissection[7,8]. Here, we report a case of a 3 mm rNET located in the distal rectum with lymphatic invasion after endoscopic resection.
Polypoid bulge found on colonoscopy.
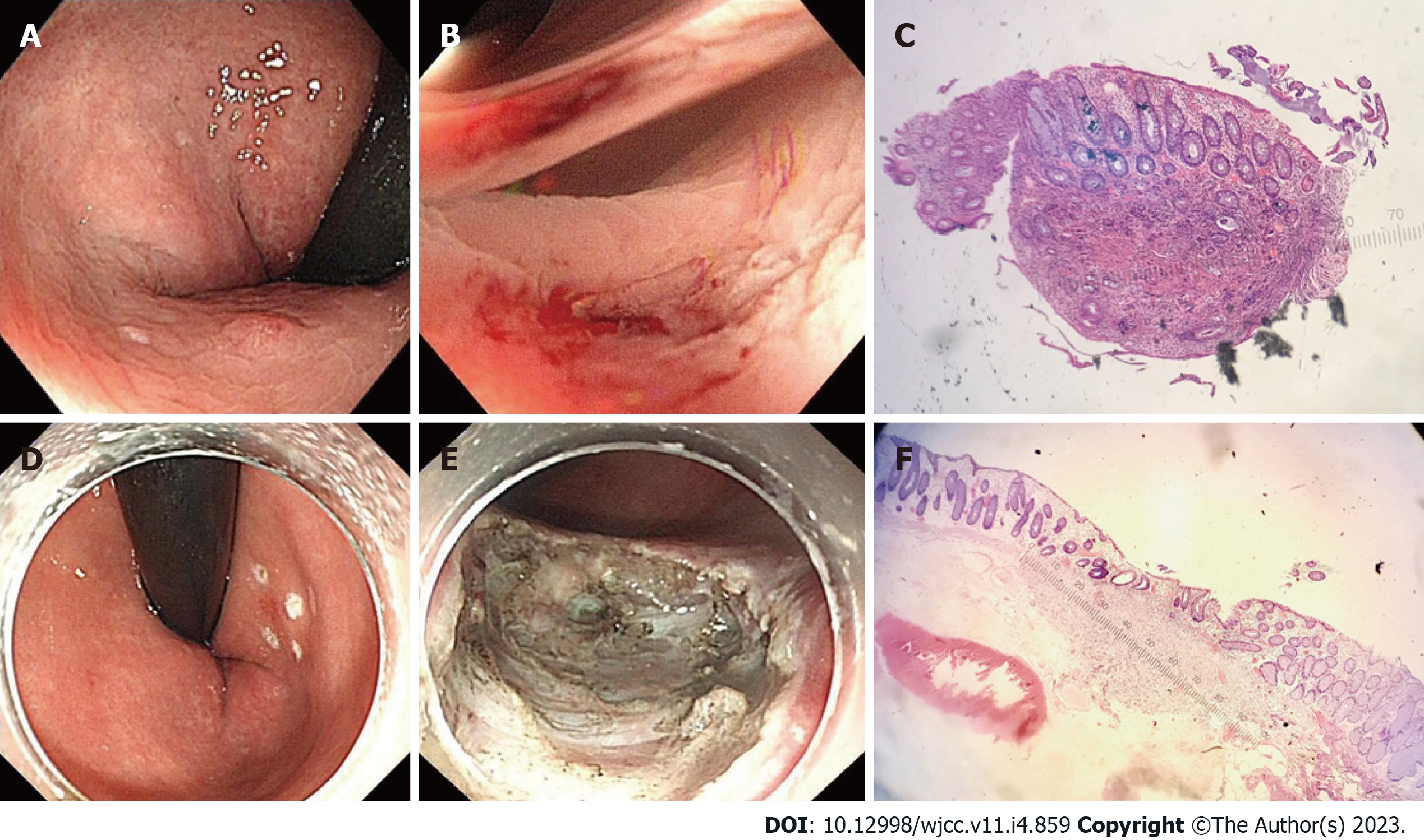
A 46-year-old male patient underwent colonoscopy and was found to have a 3-mm-sized polypoid bulge with a smooth surface in the rectum 3 cm from the anus. After sample collection with biopsy forceps, the pathological diagnosis was neuroendocrine tumor (NET) (Figure 1).
No special history of past illness.
The patient's father had a history of colon cancer. His Personal history has nothing notable.
No special.
No special.
Before endoscopic submucosal dissection (ESD), computed tomography (CT) showed no abnormalities in the enhancement of the chest and abdomen.
To clarify whether additional surgery was required, further assessment by 68Gallium labeled somatostatin analogues-positron emission tomography (68Ga-SSA-PET)/CT was used, but the results showed no abnormalities.
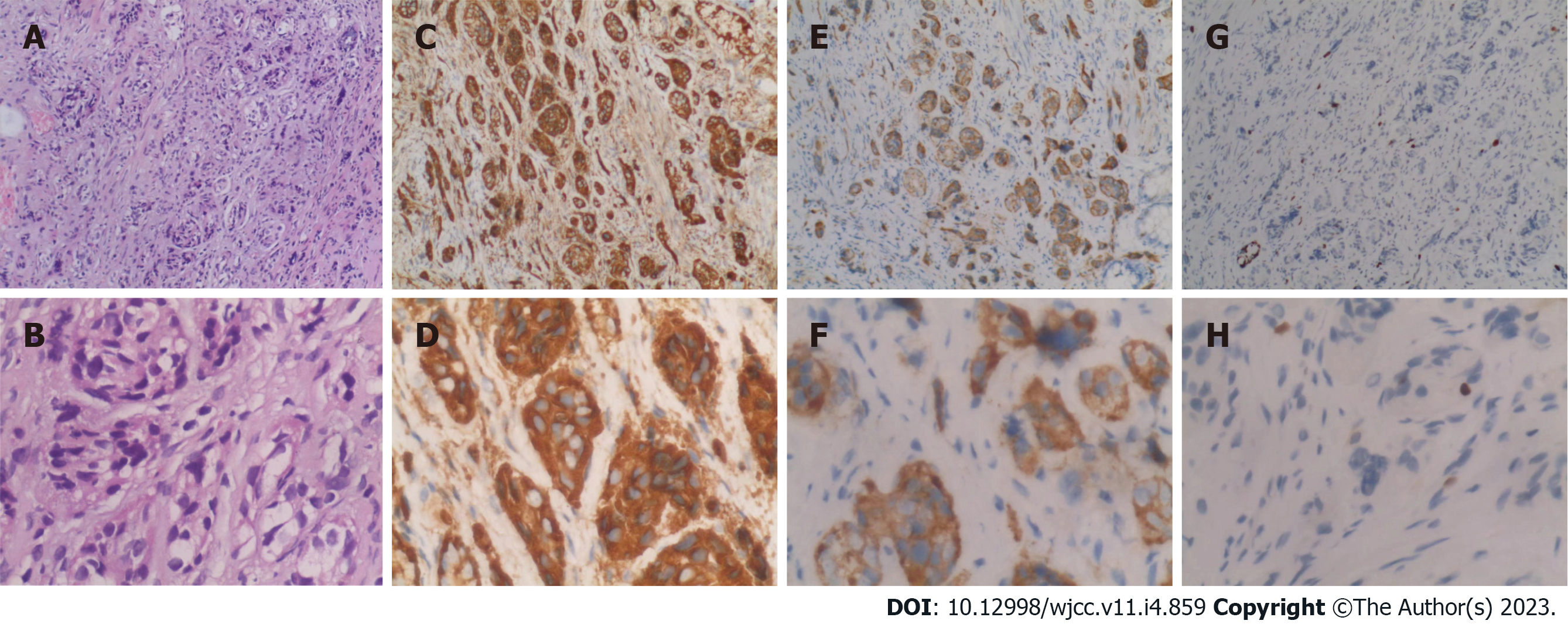
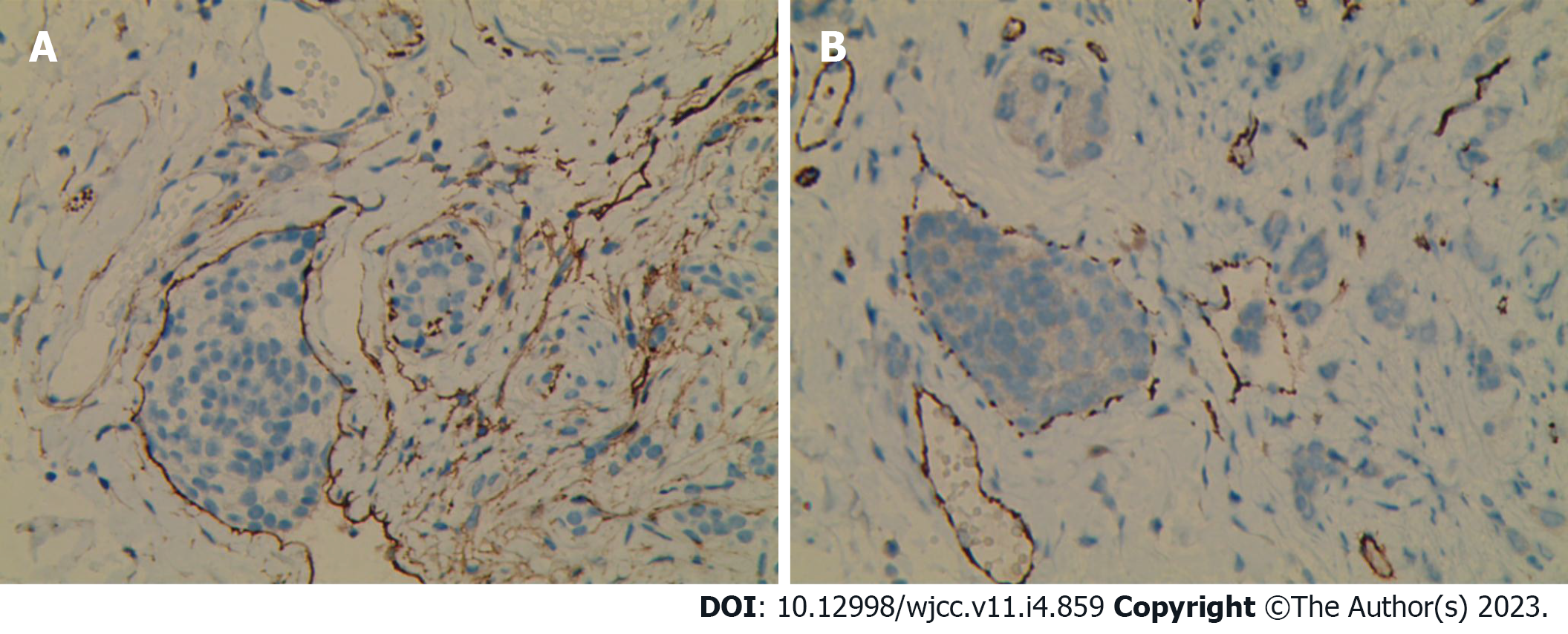
The pathological diagnosis of the specimen after ESD rescue therapy was rNET G1. The lesion infiltrated into the submucosa. The depth of submucosal infiltration was 1000 μm. The distance between the deepest infiltration of the lesion and the basal incision margin was 500 μm. The lesion size was 2550 μm. The horizontal and vertical resection margins were negative (Figure 1). Immunohistochemical (IHC) results were as follows: CK (weak +), Vim (-), Syn (+), CD56 (strong +), CgA (strong +), CK7 (-), CK20 (weak +), Villin (+), CEA (focal+), and Ki-67 (2%; Figure 2). The lymphatic invasion was confirmed by D2-40 and CD31 staining (Figure 3).
After the pathological examination of the biopsy clamped specimen suggested neuroendocrine tumor, the patient underwent multidisciplinary consultation with oncology, surgery and nuclear medicine, and finally decided to complete 68Ga-SSA-PET/CT, and no distant metastasis was found. Therefore, we decided to perform ESD after consulting the patient's consent and followed up regularly after the operation.
The pathological diagnosis of the specimen after ESD rescue therapy was rNET G1.
ESD salvage therapy was applied.
No tumor recurrence or distant metastasis was detected at 13 mo postoperative follow-up using endoscopy and CT-enhanced scans of the whole abdomen (including the pelvis).
Gastroenteropancreatic neuroendocrine tumors (GEP-NETs) are the most common type of NETs[9]. The rectum is the most common site for GEP-NETs in Asian populations[10]. In recent years, with the extensive development of colorectal cancer screening programs and the improvement of endoscopic diagnosis and treatment techniques, the incidence of rNET has continued to rise.
Lymphovascular invasion (LVI) refers to the presence of tumor cells in blood vessels and lymphatic channels. LVI is closely related to tumor metastasis in distant organs and lymph nodes. A meta-analysis found that LVI was associated with an increased risk of distant lymph node metastasis (LNM) after local resection of rNETs[11]. Therefore, LVI is a risk factor for LNM. Another meta-analysis found that, for small rNETs with a tumor size of 10 mm or less, even in the presence of LVI, the prognosis was good after endoscopic resection, with a 5-year follow-up recurrence rate of only 0.3%. In addition, tiny rNETs smaller than 5 mm had a lower incidence of LVI than rNETs with a tumor size of 5-10 mm[12].
In recent years, the detection rate of LVI in rNETs has increased significantly due to immunohistochemical detection methods[12-14]. This increasing trend is proportional to tumor size, even in the fraction of rNETs less than or equal to 5 mm, the detection rate is still about 50%[13]. One study reported that the detection rate of LVI by IHC staining (56.9%) was 6 times higher than that of hematoxylin and eosin (HE) staining alone (8.8%)[15]. This result suggests that the possibility of LVI in small rNETs was underestimated prior to using IHC staining. Both vascular and lymphatic invasion are included in LVI and usually need to be distinguished by IHC detection. Vascular invasion and lymphatic invasion have different effects on LNM. In small rNETs, vascular invasion may have a greater impact on LNM than lymphatic invasion[11].
In this rNET patient, the endoscopic tumor size was 3 mm with lymphatic invasion, the smallest rNET with LVI reporting in all existing research. At the same time, no instances of LNM or distant metastasis were found after the enhanced chest and total abdominal CT and 68G-SSA-PET/CT. During the 13-mo follow-up after ESD, we did not find tumor recurrence or distant metastasis using endoscopy at the 6-mo and 1-year postoperative follow-up. Whole abdominal CT-enhanced scans did not show tumor recurrence or distant metastasis. These findings suggest that, in small (< 10 mm) or even tiny (< 5 mm) rNETs, although there is lymphatic invasion, lymphatic invasion may not be a determinant of LNM.
A cohort study found that after 6 years of follow-up in patients with rNETs who underwent endoscopic resection, about 1% of the patients developed LNM or distant metastasis, and the tumor grades were G2. In contrast, patients with grade G1 rNETs whose tumor size was less than 20 mm and who underwent endoscopic resection did not develop lymph node or distant metastasis[16]. Therefore, the risk factors for lymph node and distant metastasis of rNETs with a tumor size less than 20 mm need further study.
Although this patient had lymphatic invasion, no lymph node or distant metastasis was found. Therefore, in the absence of a well-established correlation between LVI and LNM of rNETs with a tumor size less than 20 mm, additional surgery may not benefit all patients with LVI. The tumor grade, tumor size, LVI, and depth of invasion may still need to be comprehensively considered to determine whether to perform additional surgery. In addition, imaging studies and radionuclide scintigraphy can be considered when it is unclear whether additional surgery is required[15].
In this patient, the tumor surface was smooth, and endoscopy showed that the tumor size was small. The tumor was misdiagnosed as a hyperplastic polyp and was subjected to examination with biopsy forceps. The size of the lesion was 1500 μm. Residual lesions were found after ESD salvage surgery, in which the tumor size was found to be 1050 μm. These results indicated that simple biopsy forceps were insufficient for such rNETs, and ESD salvage was a suitable option. For hyperplastic polyps of the left colon and rectum with a tumor size of 5 mm or less, both the Japanese Society of Gastroenterology and the European Society for Gastrointestinal Endoscopy recommend endoscopic follow-up only[17,18]. The rectum is a high-incidence site of NETs. Therefore, we suggest that, if the lesions are smooth and bulging, especially when the margins of the lesions are not clear, the possibility of NETs should be considered. The possibility of NETs should be excluded by forceps and biopsy.
For this patient, to ensure his quality of life, we did not choose to conduct surgical intervention, but rather continued with follow-up observation. According to previous literature reports, the metastasis of rNETs can occur after more than 10 years[19,20]. Although no LNM and distant metastasis were found in the short-term follow-up of this patient, long-term follow-up is extremely important, especially for lymph node and liver metastasis. Therefore, this patient’s end point of follow-up should be at least 10 years. In the subsequent follow-up schedule, we will perform endoscopy and CT-enhanced scans of the whole abdomen (including the pelvis) once a year, with an additional 68Ga-SSA-PET/CT if abno
rNETs have heterogeneity and atypical symptoms. Therefore, it is not sufficient to judge the risk of tumor metastasis during clinical diagnosis and treatment based only on tumor size and LVI. Instead, during treatment, it is necessary to formulate an individualized plan, undertake close follow-up observation, and try to improve the quality of life and disease prognosis of patients while reducing the burden of treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cerwenka H, Austria; Haddadi S, Algeria S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Soga J. Carcinoids of the rectum: an evaluation of 1271 reported cases. Surg Today. 1997;27:112-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 113] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Tsikitis VL, Wertheim BC, Guerrero MA. Trends of incidence and survival of gastrointestinal neuroendocrine tumors in the United States: a seer analysis. J Cancer. 2012;3:292-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 138] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 3. | Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, Shih T, Yao JC. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017;3:1335-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1510] [Cited by in RCA: 2489] [Article Influence: 311.1] [Reference Citation Analysis (4)] |
| 4. | Scherübl H. Rectal carcinoids are on the rise: early detection by screening endoscopy. Endoscopy. 2009;41:162-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 5. | Hyun JH, Lee SD, Youk EG, Lee JB, Lee EJ, Chang HJ, Sohn DK. Clinical impact of atypical endoscopic features in rectal neuroendocrine tumors. World J Gastroenterol. 2015;21:13302-13308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Shinohara T, Hotta K, Oyama T. Rectal carcinoid tumor, 6 mm in diameter, with lymph node metastases. Endoscopy. 2008;40 Suppl 2:E40-E41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Ramage JK, De Herder WW, Delle Fave G, Ferolla P, Ferone D, Ito T, Ruszniewski P, Sundin A, Weber W, Zheng-Pei Z, Taal B, Pascher A; Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for Colorectal Neuroendocrine Neoplasms. Neuroendocrinology. 2016;103:139-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 232] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 8. | Expert Committee on Neuroendocrine Tumors; Chinese Society of Clinical Oncology. Expert consensus on gastroenteropancreatic neuroendocrine tumors in China. Linchuang Zhongliuxue Zazhi. 2016;21:927-946. [DOI] [Full Text] |
| 9. | Bornschein J, Kidd M, Malfertheiner P, Modlin IM. [Gastrointestinal neuroendocrine tumors]. Dtsch Med Wochenschr. 2008;133:1505-1510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Gastrointestinal Pathology Study Group of Korean Society of Pathologists; Cho MY, Kim JM, Sohn JH, Kim MJ, Kim KM, Kim WH, Kim H, Kook MC, Park DY, Lee JH, Chang H, Jung ES, Kim HK, Jin SY, Choi JH, Gu MJ, Kim S, Kang MS, Cho CH, Park MI, Kang YK, Kim YW, Yoon SO, Bae HI, Joo M, Moon WS, Kang DY, Chang SJ. Current Trends of the Incidence and Pathological Diagnosis of Gastroenteropancreatic Neuroendocrine Tumors (GEP-NETs) in Korea 2000-2009: Multicenter Study. Cancer Res Treat. 2012;44:157-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 172] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 11. | Kang HS, Kwon MJ, Kim TH, Han J, Ju YS. Lymphovascular invasion as a prognostic value in small rectal neuroendocrine tumor treated by local excision: A systematic review and meta-analysis. Pathol Res Pract. 2019;215:152642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Sekiguchi M, Sekine S, Sakamoto T, Otake Y, Nakajima T, Matsuda T, Taniguchi H, Kushima R, Ohe Y, Saito Y. Excellent prognosis following endoscopic resection of patients with rectal neuroendocrine tumors despite the frequent presence of lymphovascular invasion. J Gastroenterol. 2015;50:1184-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Kitagawa Y, Ikebe D, Hara T, Kato K, Komatsu T, Kondo F, Azemoto R, Komoda F, Tanaka T, Saito H, Itami M, Yamaguchi T, Suzuki T. Enhanced detection of lymphovascular invasion in small rectal neuroendocrine tumors using D2-40 and Elastica van Gieson immunohistochemical analysis. Cancer Med. 2016;5:3121-3127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Kwon MJ, Kang HS, Soh JS, Lim H, Kim JH, Park CK, Park HR, Nam ES. Lymphovascular invasion in more than one-quarter of small rectal neuroendocrine tumors. World J Gastroenterol. 2016;22:9400-9410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Carideo L, Prosperi D, Panzuto F, Magi L, Pratesi MS, Rinzivillo M, Annibale B, Signore A. Role of Combined [(68)Ga]Ga-DOTA-SST Analogues and [(18)F]FDG PET/CT in the Management of GEP-NENs: A Systematic Review. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 16. | Kuiper T, van Oijen MGH, van Velthuysen MF, van Lelyveld N, van Leerdam ME, Vleggaar FD, Klümpen HJ. Endoscopically removed rectal NETs: a nationwide cohort study. Int J Colorectal Dis. 2021;36:535-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | Tanaka S, Saitoh Y, Matsuda T, Igarashi M, Matsumoto T, Iwao Y, Suzuki Y, Nozaki R, Sugai T, Oka S, Itabashi M, Sugihara KI, Tsuruta O, Hirata I, Nishida H, Miwa H, Enomoto N, Shimosegawa T, Koike K. Evidence-based clinical practice guidelines for management of colorectal polyps. J Gastroenterol. 2021;56:323-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 18. | Ferlitsch M, Moss A, Hassan C, Bhandari P, Dumonceau JM, Paspatis G, Jover R, Langner C, Bronzwaer M, Nalankilli K, Fockens P, Hazzan R, Gralnek IM, Gschwantler M, Waldmann E, Jeschek P, Penz D, Heresbach D, Moons L, Lemmers A, Paraskeva K, Pohl J, Ponchon T, Regula J, Repici A, Rutter MD, Burgess NG, Bourke MJ. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017;49:270-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 766] [Article Influence: 95.8] [Reference Citation Analysis (0)] |
| 19. | Shigematsu Y, Kanda H, Konishi T, Takazawa Y, Inoue Y, Muto T, Ishikawa Y, Takahashi S. Recurrence 30 Years after Surgical Resection of a Localized Rectal Neuroendocrine Tumor. Intern Med. 2017;56:1521-1525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Kwaan MR, Goldberg JE, Bleday R. Rectal carcinoid tumors: review of results after endoscopic and surgical therapy. Arch Surg. 2008;143:471-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |