Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8247
Peer-review started: August 21, 2023
First decision: November 1, 2023
Revised: November 1, 2023
Accepted: December 1, 2023
Article in press: December 1, 2023
Published online: December 16, 2023
Processing time: 114 Days and 20.6 Hours
Anterior cruciate ligament (ACL) injury is one of the most common types of sports injuries. People’s need to participate in sports and desire for a high quality of life promotes the continuous development of ACL reconstruction technology. Arthroscopic ACL reconstruction has been recognized as an effective method for the treatment of ACL injuries. This review analyses and summarizes the advantages and limitations of each surgical procedure for arthroscopic ACL reconstruction reported in the relevant literature so as to promote the future development of more relevant techniques.
Core Tip: In the past 50 years, with the improvement of the understanding of knee anatomy and its injury mechanism, anterior cruciate ligament reconstruction surgery has developed rapidly. The fixation methods are reviewed in order to provide reference for the treatment of preclinical cruciate ligament injuries.
- Citation: Dai Y, Gao WJ, Li WC, Xiang XX, Wang WM. Research progress on preparation of lateral femoral tunnel and graft fixation in anterior cruciate ligament reconstruction. World J Clin Cases 2023; 11(35): 8247-8255
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8247.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8247
The anterior cruciate ligament (ACL) is one of the main anatomical structures of the knee joint and is commonly subjected to sports injury. More than 120000 ACL reconstructions are performed annually in the United States, and the relative risk of ACL rupture in female athletes is 2-9 times higher than that in male athletes[1]. In the past 50 years, improved understanding of the knee anatomy and its proneness to specific types of injury has led to the rapid development of ACL reconstruction surgery. The fixation methods are reviewed to provide a reference for the treatment of preclinical cruciate ligament injuries.
The tibial insertion of the ACL originates from the outer surface of the medial intercondylar ridge, assuming a fan-shaped configuration. On the other hand, the femoral insertion is attached to the intercondylar notch located behind the inner surface of the lateral femoral condyle and exhibits an oval shape with an extended fiber bundle[2]. It is widely accepted that the ACL consists of two fundamental functional bundles, namely, the anteromedial (AM) bundle and posterolateral (PL) bundle, which play a crucial role in maintaining both anteroposterior and rotational stability of the knee joint[3]. Giuliani et al[4] conducted anatomical studies on cadavers and discovered that ACL width ranged from 7-17 mm with an average measurement of 11 mm. Additionally, he found that AM bundle had an average length of 33 mm while PL bundle averaged at 18 mm[5,6]. The blood supply of the ACL is derived from the middle genicular artery, as well as the medial and lateral arteries below the knee. Mechanoreceptors, including Ruffini bodies, ring bodies, Golgi bodies, and free nerve endings, are also present in the ACL. These sensory endings indicate a proprioceptive function within the ACL that plays a crucial role in maintaining knee joint stability[7]. ACL injury is one of the most common sports injuries, with non-contact injuries accounting for 70% of cases. It occurs more frequently during activities involving sudden changes in direction such as deceleration, jumping or knee bending. This instability leads to secondary complications like meniscus and cartilage wear, increased joint effusion and reduced exercise capacity[8]. Furthermore, when combined with other structural injuries such as meniscal tears or collateral ligament damage (medial or lateral), it further exacerbates knee joint instability and increases the risk of secondary injuries[9].
Reijman et al[10] compared patients who underwent early ACL reconstruction vs those who had elective reconstruction after rehabilitation over a 2-year follow-up period. The results demonstrated significant improvements in symptom perception, knee joint function and exercise capacity among patients who underwent early reconstruction compared to those in the latter group. Herbst’s prospective comparative study revealed that patients who received early ACL reconstruction surgery had significantly lower rates of extension limitation between 3°-5° at 12 mo post-surgery. Therefore it is recommended for individuals with high activity demands or athletes to undergo ACL reconstruction within 48 h to prevent articular cartilage damage[11]. In cases where there is acute hematoma or limited knee motion due to early immobilization, it is advisable to perform elective ACL reconstruction once hematoma resolution and adhesion subsidence have occurred.
The transtibial drilling technique involves establishing a femoral tunnel through the tibial tunnel, initially utilized for isometric reconstruction of the ACL under arthroscopy with the knee joint flexed at 90° during surgery. This approach simplifies femoral tunnel placement, reduces operation time, and ensures graft isometry. However, the success of the femoral approach heavily relies on the direction of the tibial tunnel, primarily determined by the origin of the external tibial ostium. Kopf et al[12] employed a 3D computed tomography model to visualize and quantify femoral and tibial tunnel positions in patients after ACL reconstruction using 32 transtibial techniques (TTs). When compared to anatomical reference data for tunnel positioning, results indicated that while the tibial tunnel was located medially in an anatomically PL position, both AM and PL tunnels had their respective femoral tunnels positioned anteriorly from their anatomical locations. Conventional tibial tunnels typically reach a maximum height of only 4 mm above the center of femoral insertion, resulting in a mere 50% to 60% overlap with respect to femoral footprint[13]. As this non-anatomically positioned femoral tunnel passes through the tibia, its internal opening becomes excessively high and deep while also causing an overly vertical graft angle ultimately leading to inadequate recovery of rotational stability within the knee joint[14]. Long-term studies have additionally revealed that non-anatomic reconstructions can contribute to earlier postoperative cartilage degeneration in knees[15]. Furthermore, when flexed, instead of rotating around a fixed center point within itself as intended; it has been observed that movement occurs between the tibia plateau and femur during knee joint motion resulting in relatively equal graft length achievement only. Modified TT techniques have demonstrated comparable effectiveness to other approaches for ACL reconstruction. Bhatia et al[16] positioned the modified tibial tunnel at the proximal entry point with a minimum tunnel size of 9 mm to ensure achieving anatomical positioning of the femur using a 7 mm femoral offset guide. The guide pin was placed at the natural insertion point on the condyle wall, while alternative placements included distal and anterior or posterior positions relative to the natural insertion on the condylar wall. Sim et al[17] employed a robotic testing system for ACL reconstruction, demonstrating that both the modified TT technique, AM technique, and outside-in (OI) technique were viable in restoring normal knee motion biomechanics.
The AM technique is an arthroscopic AM approach that focuses on anatomical reconstruction, aiming to restore the normal function of the knee joint to its maximum extent and prevent excessive tension of the graft by reconstructing the anatomical insertion point of the ACL femur at a flexion angle of 120°[18,19]. Unlike the TT method, which has limitations based on the position of the tibial tunnel, AM allows for independent preparation of the femoral tunnel, providing more flexibility and easier positioning within the anatomical footprint area. A meta-analysis revealed that compared to AM, TT resulted in a significantly more vertical femoral tunnel orientation and obvious anterior displacement of tibia relative to femur, leading to poor postoperative joint stability[20]. In contrast, AM offers a deeper and lower placement with more precise positioning. This enables faster recovery and improved rotational stability in reconstructed knees[21-23]. Studies demonstrated that as inclination increases in AM-prepared femoral tunnels, their length decreases[24,25], which was also supported by experimental results from Osti et al[22]. Consequently, there was a higher proportion of femoral tunnels shorter than 25 mm in length within the AM group. While this may affect graft healing and increase risk for bursting through posterior femoral cortex, it also reduces postoperative “wiper effect” caused by traction loop swinging[26]. However, no statistically significant difference was observed in Koos scores between TT and AM groups; all patients reported successful return to sports activities and work following both procedures[27].
The OI technique is based on anatomical reconstruction, employing an ACL locator inserted into the AM femoral entrance to precisely locate the internal opening of the femoral tunnel. Simultaneously, an arthroscope is introduced through the anterolateral entrance to adjust the position of the femoral tunnel. This unique drilling technique offers considerable variability without necessitating knee joint flexion for intra-articular tissue protection. In cases where patients have a narrow intercondylar notch space, combined operations such as disability protection can be considered, reducing reliance on femoral drilling. Moreover, compared to the AM method[22,28], cortical fracture risk is less restrictive in this approach. Osti et al[22] confirmed that both AM and OI surgical techniques surpass TT technique in terms of ACL femoral tunnel positioning and reproduction of anatomical insertion while exhibiting comparable prognostic outcomes.
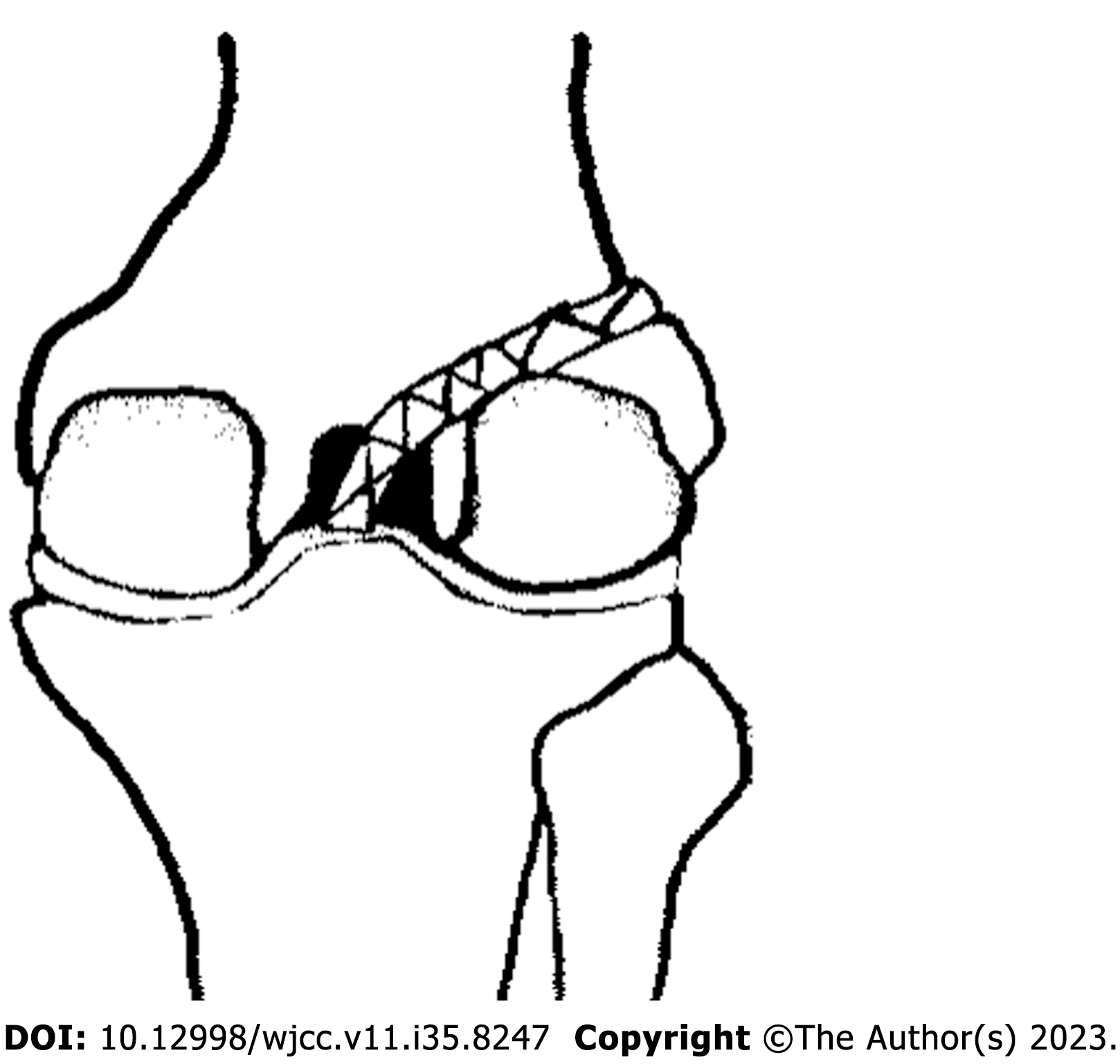
The study reported an over-the-top (OTT) technique in which the graft was secured above the lateral femoral condyle[29]. Girgis et al[30] proposed that the overtop area is an arc-shaped region located at the junction of the posterior aspect of the femoral shaft and the most proximal part of the lateral femoral condyle, with its innermost side representing the location of OTT. During knee motion, soft tissue loading rather than bone tunnel loading occurs on the graft, significantly reducing wear at the opening of the femoral tunnel[31]. Two studies have continuously refined OTT by creating a groove on the lateral femoral condyle to enhance graft fixation and maintain optimal balance between graft isometricity and anatomical alignment[32,33]. Due to its avoidance of femoral tunnel preparation and protection of femoral epiphysis, OTT is applicable for revision patients with excessive or improperly positioned tunnels as well as adolescent patients with growth potential. Furthermore, combining OTT with retaining graft stump technique can better preserve ACL proprioceptors and integrity[34,35]. The advantages and disadvantages of the above techniques are summarized in Table 1. The OTT technology diagram is shown in Figure 1.
| Technique | Advantages | Disadvantages |
| Transtibial | Less surgical trauma; few complications[17] | Poor rotational stability of the knee joint; cartilage degeneration occurred earlier after surgery[14] |
| Anteromedial | The femoral tunnel was accurately positioned; better rotational stability[18,19] | The femoral tunnel is short; breaking the femoral cortex; a risk of injury to the common peroneal nerve[24,25] |
| Outside-in | Larger tendon-bone interface contact area[22] | Add auxiliary incision |
| Over-the-top | Reduce femoral inlet graft wear | Need to practice the technique[32,33] |
Śmigielski et al[36] proposed the ribbon-like theory in the article, the anatomical structure of the ACL is a flat, ribbon-like structure with a bundle, and the reason why the ACL is double-bundled is that it is twisted. A number of anatomical studies on the ACL have shown that the femoral attachment point is oval or semicircular and the tibial attachment point is oval or “C”-shaped. Therefore, Noh et al[37] suggested creating an oval bone tunnel to better reproduce the anatomical attachment point[2]. Some studies have shown that compared to the circular tunnel group, the Tegner score, pivot shift test and early graft maturity were better in the oval tunnel group than in the circular group[38,39]. The oval tunnel, which resembles the natural ACL footprint, is closer to the shape of the physiologic attachment point, wear of the graft and bone tunnel increases the contact area, prolongs graft life, increases nutrient exchange between the synovial fluid, and promotes healing of the tendon on the bone[40]. The oval tunnel not only maintains the tensile strength of double-bundle reconstruction, but also has the advantage of reducing bone loss in single-bundle reconstruction, which is a promising reconstruction technique.
In 1836, the Weber[41] described the division of the ACL into two functional bundles, and a cadaver study[42] found that the in situ force of the AM was significantly higher than that of the PL at full extension of the knee, whereas the in situ forces are highest in the PL bundle and decrease with increasing flexion. The single-bundle ACL reconstruction technique mainly restores the function of the AM bundle, which limits but does not maintain well the anterior translation of the tibia during knee flexion. Rotational stability of the knee joint[43]. Kyung et al[44] believe that reconstruction with one bundle can restore the footprint of the original ACL more accurately, but it cannot restore the inclination angle of the original ACL in the coronal plane, while reconstruction with two bundles can restore the normal inclination of the two ACL bundles. The normal kinematics of the original ACL is better restored. The literature reports that, compared to reconstruction with one bundle, the incidence of graft fractures and osteoarthritis is significantly lower after reconstruction with two bundles, the anatomical structure of the ligaments can be better restored, the contact surface of the bone tract is large and the initial strength is high. A biomechanical in-vitro study has shown that stabilization of the knee with two bundles is superior to reconstruction with one bundle[45-47]. However, the technical requirements are higher than for reconstruction with one bundle and the operation time is longer, which increases the risk of the operation. Compared to reconstruction with one bundle, reconstruction with two bundles requires a larger space for the patient’s intercondylar notch. If the intercondylar notch is less than 12 mm wide, the graft is very likely to impinge, and the preparation of four bone tunnels results in a large loss of bone mass, and the indications are limited. Studies have shown no difference in clinical scores, knee stability, and magnetic resonance imaging (MRI) appearance between patients who underwent single-bundle reconstruction and those who underwent double-bundle reconstruction, but patients who underwent double-bundle reconstruction had a longer recovery time. Two studies found that anterior tibial displacement was closer to the intact knee joint in double-bundle reconstruction compared with single-bundle reconstruction, and the incidence of cartilage degeneration and meniscal injury to the knee was lower[48,49]. However, they pointed out that anatomical double-bundle reconstruction is not significantly better than single-bundle reconstruction when using individualized ACL reconstruction techniques.
With the confirmation of the ligament theory and the many problems that the reconstruction of double bundles has revealed, the reconstruction of single bundles has come into people’s focus. The most important aspect of single-bundle reconstruction is the selection of the femoral insertion point. Pearle et al[50] proposed the IDEAL theory to place the tunnel in the femoral footprint area, i.e., isometric, direct insertion, eccentrically located, anatomic, and low tension. The main surgical options for single-bundle reconstruction are the traditional anatomic single-bundle reconstruction and the total internal technique. The conventional total tibial tunnel technique uses a hanging cortical fixation on the femoral side and interfering screws on the tibial side. In all-inside reconstruction (all-inside), the cortical bone is suspended, retrogradely drilled and a bone socket is prepared instead of a tunnel to reserve bone for later revision surgery. Some studies suggest that the all-inside technique may also reduce tunnel expansion by preventing the flow of synovial fluid into the socket. In addition, the all-inside technique reduces damage to the cortex and periosteum and reduces posto
In 1979, Norwood and Cross[52] described that the ACL is divided into three bundles - AM, intermediate and PL. Otsubo et al[53] identified the attachment areas of the three ACL bundles, while Fujie et al[54] and Kato et al[55] explained the biomechanical function of each bundle in detail. Dissecting three-bundle ACL reconstruction with two double-ring grafts performed with two femoral tunnels and one tibial tunnel to simulate three bundles within the native ACL[56-58], ATB viewed through secondary arthroscopy. The grafts show a fan-shaped tibial insertion, that better mimics the original triangular tibial footprint[56]. Compared with double-bundle or single-bundle ACL reconstruction, ATB ACL reconstruction requires only lower initial graft tension to maintain anterolateral stability[59]. Uchida et al[58] indicated that after reconstruction of the triple-bundled ACL with a hamstring autograft, the patient achieved satisfactory results in terms of objective stability of the knee joint after surgery. This technique still has many limitations. First, there are currently no studies showing that the triple-bundle reconstruction technique can reduce the graft failure rate. Secondly, the area of the femoral tunnel hole in triple-bundle ACL reconstruction is more than twice that of the single-bundle technique, while the area of the tibial tunnel hole is three times that of the single-bundle technique. Excessive bone loss leads to an increased risk of secondary revision[60]. In addition, three-bundle reconstruction surgery is more complicated, and the long operation time increases the risk of intraoperative and postoperative complications, and the cost of surgical treatment is higher.
Depending on their material, interface screws can be divided into metal screws and screws made of bioresorbable material[61]. Metal screws can provide greater strength to the graft in the initial phase, but there is graft incision and postoperative pain, and the metal material interferes with postoperative MRI and other imaging studies, which hinders the assessment of postoperative graft healing[62]. Screws made of bioabsorbable material have better tissue compatibility and can be degraded and resorbed. They are excellent at controlling tendon gliding and the degree of incision of the grafted tendons is easier than with metal screws. The disadvantages are high cost, incomplete control of the degradation rate of the screw, some immune reactions and greater expansion of the bone tunnel. In addition, clinical complications such as local osteolysis and cysts may occur[63-66]. A meta-analysis concluded that resorbable screws have the same clinical effect compared to metal screws and that they do not need to be removed by a second surgical procedure, which is convenient for assessing the effect of postoperative graft healing, but the incidence of knee joint effusions is higher[67].
Cortical suspension fixation utilizes an Endo-button with loops, which is designed in the form of a button plate. Currently, in clinical practice, two types of loops are commonly utilized: Fixed-length loops and adjustable-length loops. The aforementioned products exhibit user-friendly characteristics and possess a notable level of initial fixation strength. The fixation point is located at a considerable distance from the anatomical insertion point, resulting in a gap between the graft and the fixation device. This gap leads to relative movement, thereby increasing the likelihood of postoperative complications such as the bungee effect and wiper effect. Additionally, the graft is unable to completely conform to the bone tunnel, significantly impacting the healing process of both the tendon and bone. Speed can also result in the enlargement of the bone tunnel, thereby increasing the likelihood of revision[68,69]. Although the utilization of adjustable-length loops has been proposed as a potential solution to decrease the gap and minimize complications, Bressy et al[70] discovered that the tibial graft’s stability is not optimal when relying solely on the button plate with adjustable-length loops for fixation.
Currently, the Rigidfix fixation system is the most commonly employed transverse nail in clinical practice. The utilization of transverse nail fixation offers several advantages. Firstly, it enhances the stability of the graft within the bone tunnel. Additionally, it increases the contact area between the tendon and bone, thereby promoting the healing process of the graft. The utilization of degradable absorbing material simplifies and expedites the operation process. Additionally, it allows for the distribution of resistance at the interface between the fixation material and the bone, thereby reducing the likelihood of posterior femoral cortical fracture. The drawback of this approach is the potential for breakage of absorbable transversal nails, which can result in the dissociation of fragments within the joint cavity. This can cause damage to the articular surface cartilage and meniscus, ultimately necessitating secondary surgery[9,71]. The advantages and disadvantages of several fixed methods are summarized in Table 2.
| Technique | Advantages | Disadvantages |
| Aperture fixation | High fixation strength[67] | Meta obstructing postoperative evaluation; the degradation rate of absorbable materials is not completely controllable[63-66] |
| Cortical suspension fixation | Adjustable length is easy to use | The probability of complications such as bungee jumping effect and wiper effect increased; bone tunnel enlargement[68,69] |
| Transverse nail fixation | More tendon-bone contact area; uniform resistance distribution[9,71] | Risk of nail breakage |
The femoral end fixation of the ACL in OTT reconstruction is unique. One suture rivet is positioned at the interface between the lateral epicondyle of the femur and the posterior femoral cortex. Two non-absorbable sutures are affixed to the distal end of the rivet. Two strands were inserted into the coil created by the traction wire at the femoral end of the grafted tendon and secured with a single knot. The two strands of suture were passed through the grafted tendon, folded, and subsequently tied individually to achieve the fixation of the femoral end. No matter the type of fixation device employed, it is imperative to select a fixation method that can offer adequate strength based on the patient's specific circumstances in order to minimize the rate of ACL revision.
Arthroscopic ACL reconstruction has become the primary surgery for ACL reconstruction. A large amount of clinical experience and data have been accumulated. Surgical concepts are constantly being updated. However, methods to better reconstruct the isometric, anatomical and proprioceptive properties of the graft and restore the function of the knee joint have yet to be discovered. In addition to the abovementioned introductions to surgical methods and graft selection, there are also a large number of biological experiments on the promotion of the ACL tendon-bone healing process, explaining ACL reconstruction at the molecular level. With the development of sports medicine and an in-depth understanding of the ACL reconstruction process, microscopic joint ACL reconstruction will develop more rapidly, and patients will have a better prognosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oommen AT, India S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 2. | Fujimaki Y, Thorhauer E, Sasaki Y, Smolinski P, Tashman S, Fu FH. Quantitative In Situ Analysis of the Anterior Cruciate Ligament: Length, Midsubstance Cross-sectional Area, and Insertion Site Areas. Am J Sports Med. 2016;44:118-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Sasaki N, Ishibashi Y, Tsuda E, Yamamoto Y, Maeda S, Mizukami H, Toh S, Yagihashi S, Tonosaki Y. The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy. 2012;28:1135-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 107] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 4. | Giuliani JR, Kilcoyne KG, Rue JP. Anterior cruciate ligament anatomy: a review of the anteromedial and posterolateral bundles. J Knee Surg. 2009;22:148-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 218] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 6. | Kopf S, Musahl V, Tashman S, Szczodry M, Shen W, Fu FH. A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc. 2009;17:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 170] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 7. | Georgoulis AD, Pappa L, Moebius U, Malamou-Mitsi V, Pappa S, Papageorgiou CO, Agnantis NJ, Soucacos PN. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001;9:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 125] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Krosshaug T, Nakamae A, Boden BP, Engebretsen L, Smith G, Slauterbeck JR, Hewett TE, Bahr R. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 716] [Cited by in RCA: 757] [Article Influence: 42.1] [Reference Citation Analysis (0)] |
| 9. | Freedman KB, D'Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 567] [Cited by in RCA: 514] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 10. | Reijman M, Eggerding V, van Es E, van Arkel E, van den Brand I, van Linge J, Zijl J, Waarsing E, Bierma-Zeinstra S, Meuffels D. Early surgical reconstruction versus rehabilitation with elective delayed reconstruction for patients with anterior cruciate ligament rupture: COMPARE randomised controlled trial. BMJ. 2021;372:n375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 11. | Lie MM, Risberg MA, Storheim K, Engebretsen L, Øiestad BE. What's the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019;53:1162-1167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 126] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 12. | Kopf S, Forsythe B, Wong AK, Tashman S, Anderst W, Irrgang JJ, Fu FH. Nonanatomic tunnel position in traditional transtibial single-bundle anterior cruciate ligament reconstruction evaluated by three-dimensional computed tomography. J Bone Joint Surg Am. 2010;92:1427-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 185] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 13. | Piasecki DP, Bach BR Jr, Espinoza Orias AA, Verma NN. Anterior cruciate ligament reconstruction: can anatomic femoral placement be achieved with a transtibial technique? Am J Sports Med. 2011;39:1306-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36:1275-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 116] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 15. | Izawa T, Okazaki K, Tashiro Y, Matsubara H, Miura H, Matsuda S, Hashizume M, Iwamoto Y. Comparison of rotatory stability after anterior cruciate ligament reconstruction between single-bundle and double-bundle techniques. Am J Sports Med. 2011;39:1470-1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Bhatia S, Korth K, Van Thiel GS, Frank RM, Gupta D, Cole BJ, Bach BR Jr, Verma NN. Effect of tibial tunnel diameter on femoral tunnel placement in transtibial single bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Sim JA, Gadikota HR, Li JS, Li G, Gill TJ. Biomechanical evaluation of knee joint laxities and graft forces after anterior cruciate ligament reconstruction by anteromedial portal, outside-in, and transtibial techniques. Am J Sports Med. 2011;39:2604-2610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20:1015-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 396] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 19. | Tashman S, Araki D. Effects of anterior cruciate ligament reconstruction on in vivo, dynamic knee function. Clin Sports Med. 2013;32:47-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Dong Z, Wang L, Ma YH, Hu F, Ma GP, Wang FF. [Arthroscopic anterior cruciate ligament reconstruction through transtibial and anteromedial approaches: a Meta-analysis]. Chinese J Tissue Engineering Res. 2015;19:8352-8358. [DOI] [Full Text] |
| 21. | Noh JH, Roh YH, Yang BG, Yi SR, Lee SY. Femoral tunnel position on conventional magnetic resonance imaging after anterior cruciate ligament reconstruction in young men: transtibial technique versus anteromedial portal technique. Arthroscopy. 2013;29:882-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Osti M, Krawinkel A, Ostermann M, Hoffelner T, Benedetto KP. Femoral and tibial graft tunnel parameters after transtibial, anteromedial portal, and outside-in single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2250-2258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | Azboy I, Demirtaş A, Gem M, Kıran S, Alemdar C, Bulut M. A comparison of the anteromedial and transtibial drilling technique in ACL reconstruction after a short-term follow-up. Arch Orthop Trauma Surg. 2014;134:963-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Chang CB, Choi JY, Koh IJ, Lee KJ, Lee KH, Kim TK. Comparisons of femoral tunnel position and length in anterior cruciate ligament reconstruction: modified transtibial versus anteromedial portal techniques. Arthroscopy. 2011;27:1389-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 25. | Chang CB, Yoo JH, Chung BJ, Seong SC, Kim TK. Oblique femoral tunnel placement can increase risks of short femoral tunnel and cross-pin protrusion in anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38:1237-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 26. | Zhang L, Jiang B, Sun J, Ma J, Zhang S, Liu X. [A comparative study of arthroscopic anterior cruciate ligament reconstruction via transtibial and transportal techniques]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1077-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Stone AV, Chahla J, Manderle BJ, Beletsky A, Bush-Joseph CA, Verma NN. ACL Reconstruction Graft Angle and Outcomes: Transtibial vs Anteromedial Reconstruction. HSS J. 2020;16:256-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Wang H, Han X, Wang J, Wang W. Femoral tunnels of outside-in method versus anteromedial portal technique in anterior cruciate ligament reconstruction. Chinese J Joint Surg (Electronic Edition). 2015;. |
| 29. | Luo MD. The anterior cruciate ligament: Over-the-top repair. J Bone Joint Surg. 1974;52. |
| 30. | Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;216-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1147] [Cited by in RCA: 948] [Article Influence: 19.0] [Reference Citation Analysis (1)] |
| 31. | Montgomery RD, Milton JL, Terry GC, McLeod WD, Madsen N. Comparison of over-the-top and tunnel techniques for anterior cruciate ligament replacement. Clin Orthop Relat Res. 1988;144-153. [PubMed] |
| 32. | Melhorn JM, Henning CE. The relationship of the femoral attachment site to the isometric tracking of the anterior cruciate ligament graft. Am J Sports Med. 1987;15:539-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 61] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Penner DA, Daniel DM, Wood P, Mishra D. An in vitro study of anterior cruciate ligament graft placement and isometry. Am J Sports Med. 1988;16:238-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 120] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 34. | Lee DH, Kim HJ, Ahn HS, Bin SI. Comparison of femur tunnel aperture location in patients undergoing transtibial and anatomical single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:3713-3721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Mei S, Li R, Xiang X, Wang W. [Research progress of anterior cruciate ligament reconstruction with over-the-top technique]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36:1166-1171. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 36. | Śmigielski R, Zdanowicz U, Drwięga M, Ciszek B, Williams A. The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J. 2016;98-B:1020-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 37. | Noh JH, Yang BG, Roh YH, Kim SW, Kim W. Anterior cruciate ligament reconstruction using 4-strand hamstring autograft: conventional single-bundle technique versus oval-footprint technique. Arthroscopy. 2011;27:1502-1510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Zhang J, Hu X, Liu Z, Zhao F, Ma Y, Ao Y. Anatomical single bundle anterior cruciate ligament reconstruction with rounded rectangle tibial tunnel and oval femoral tunnel: a prospective comparative study versus conventional surgery. Am J Transl Res. 2019;11:1908-1918. [PubMed] |
| 39. | Suzuki T, Shino K, Otsubo H, Suzuki D, Mae T, Fujimiya M, Yamashita T, Fujie H. Biomechanical comparison between the rectangular-tunnel and the round-tunnel anterior cruciate ligament reconstruction procedures with a bone-patellar tendon-bone graft. Arthroscopy. 2014;30:1294-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Nakase J, Toratani T, Kosaka M, Ohashi Y, Numata H, Oshima T, Takata Y, Tsuchiya H. Technique of anatomical single bundle ACL reconstruction with rounded rectangle femoral dilator. Knee. 2016;23:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 42. | Ma Y, Ao YF, Yu JK, Dai LH, Shao ZX. Failed anterior cruciate ligament reconstruction: analysis of factors leading to instability after primary surgery. Chin Med J (Engl). 2013;126:280-285. [PubMed] [DOI] [Full Text] |
| 43. | Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 452] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 44. | Kyung BS, Kim JG, Chang M, Jang KM, Lee SS, Ahn JH, Wang JH. Anatomic double-bundle reconstruction techniques result in graft obliquities that closely mimic the native anterior cruciate ligament anatomy. Am J Sports Med. 2013;41:1302-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 45. | Järvelä S, Kiekara T, Suomalainen P, Järvelä T. Double-Bundle Versus Single-Bundle Anterior Cruciate Ligament Reconstruction: A Prospective Randomized Study With 10-Year Results. Am J Sports Med. 2017;45:2578-2585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 46. | Sun R, Chen BC, Wang F, Wang XF, Chen JQ. Prospective randomized comparison of knee stability and joint degeneration for double- and single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23:1171-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 47. | Ebert A, Frosch KH. Anterior Cruciate Ligament Reconstruction - Does the Surgeon Risk Worsening of the Clinical Outcome During the Learning Curve if He Switches from Single Bundle Technique to Double Bundle Technique? Z Orthop Unfall. 2016;154:449-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 48. | Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS. Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc. 2015;23:640-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 130] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 49. | Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 784] [Cited by in RCA: 671] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 50. | Pearle AD, McAllister D, Howell SM. Rationale for Strategic Graft Placement in Anterior Cruciate Ligament Reconstruction: I.D.E.A.L. Femoral Tunnel Position. Am J Orthop (Belle Mead NJ). 2015;44:253-258. [PubMed] |
| 51. | Kouloumentas P, Kavroudakis E, Charalampidis E, Kavroudakis D, Triantafyllopoulos GK. Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg Sports Traumatol Arthrosc. 2019;27:3592-3598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 52. | Norwood LA, Cross MJ. Anterior cruciate ligament: functional anatomy of its bundles in rotatory instabilities. Am J Sports Med. 1979;7:23-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 126] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 53. | Otsubo H, Shino K, Suzuki D, Kamiya T, Suzuki T, Watanabe K, Fujimiya M, Iwahashi T, Yamashita T. The arrangement and the attachment areas of three ACL bundles. Knee Surg Sports Traumatol Arthrosc. 2012;20:127-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 54. | Fujie H, Otsubo H, Fukano S, Suzuki T, Suzuki D, Mae T, Shino K. Mechanical functions of the three bundles consisting of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19 Suppl 1:S47-S53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 55. | Kato Y, Ingham SJ, Maeyama A, Lertwanich P, Wang JH, Mifune Y, Kramer S, Smolinski P, Fu FH. Biomechanics of the human triple-bundle anterior cruciate ligament. Arthroscopy. 2012;28:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 56. | Tanaka Y, Shino K, Horibe S, Nakamura N, Nakagawa S, Mae T, Otsubo H, Suzuki T, Nakata K. Triple-bundle ACL grafts evaluated by second-look arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2012;20:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 57. | Otsubo H, Akatsuka Y, Takashima H, Suzuki T, Suzuki D, Kamiya T, Ikeda Y, Matsumura T, Yamashita T, Shino K. MRI depiction and 3D visualization of three anterior cruciate ligament bundles. Clin Anat. 2017;30:276-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 58. | Uchida R, Shino K, Iuchi R, Tachibana Y, Yokoi H, Nakagawa S, Mae T. Anatomical Triple Bundle Anterior Cruciate Ligament Reconstructions With Hamstring Tendon Autografts: Tunnel Locations and 2-Year Clinical Outcomes. Arthroscopy. 2021;37:2891-2900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 59. | Mae T, Shino K, Matsumoto N, Yoneda K, Yoshikawa H, Nakata K. Immediate postoperative anterior knee stability: double- versus triple-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2013;29:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 60. | Kinugasa K, Hamada M, Yoneda K, Matsuo T, Mae T, Shino K. Cross-sectional area of hamstring tendon autograft after anatomic triple-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:1219-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 61. | Gruen RL, Weeramanthri TS, Knight SE, Bailie RS. Specialist outreach clinics in primary care and rural hospital settings. Cochrane Database Syst Rev. 2004;2003:CD003798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 100] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 62. | Julien TP, Ramappa AJ, Rodriguez EK. Femoral condylar fracture through a femoral tunnel eleven years after anterior cruciate ligament reconstruction: a case report. J Bone Joint Surg Am. 2010;92:963-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 63. | Harvey A, Thomas NP, Amis AA. Fixation of the graft in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2005;87:593-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 64. | Konan S, Haddad FS. The unpredictable material properties of bioabsorbable PLC interference screws and their adverse effects in ACL reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2009;17:293-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 65. | Givissis PK, Stavridis SI, Papagelopoulos PJ, Antonarakos PD, Christodoulou AG. Delayed foreign-body reaction to absorbable implants in metacarpal fracture treatment. Clin Orthop Relat Res. 2010;468:3377-3383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 66. | Stener S, Ejerhed L, Sernert N, Laxdal G, Rostgård-Christensen L, Kartus J. A long-term, prospective, randomized study comparing biodegradable and metal interference screws in anterior cruciate ligament reconstruction surgery: radiographic results and clinical outcome. Am J Sports Med. 2010;38:1598-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 67. | Tao B, Zhao JM, Ding XF, Wei QJ, Liu JT. Bioabsorable interference screws versus metal interference screws in anterior cruciate ligament reconstruction: A systematic review. J Clin Rehabilitative Tissue Engineering Res. 2011;15:9817-9822. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 68. | Tajima T, Yamaguchi N, Nagasawa M, Morita Y, Nakamura Y, Chosa E. Early weight-bearing after anterior cruciate ligament reconstruction with hamstring grafts induce femoral bone tunnel enlargement: a prospective clinical and radiographic study. BMC Musculoskelet Disord. 2019;20:274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 69. | Wise BT, Patel NN, Wier G, Labib SA. Outcomes of ACL Reconstruction With Fixed Versus Variable Loop Button Fixation. Orthopedics. 2017;40:e275-e280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 70. | Bressy G, Brun V, Ferrier A, Dujardin D, Oubaya N, Morel N, Fontanin N, Ohl X. Lack of stability at more than 12 months of follow-up after anterior cruciate ligament reconstruction using all-inside quadruple-stranded semitendinosus graft with adjustable cortical button fixation in both femoral and tibial sides. Orthop Traumatol Surg Res. 2016;102:867-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 71. | Wang J, Fan HQ, Dai W, Li HD, Fu YP, Liu Z, Huang CM, Shi Z. Safety of the application of Rigidfix cross-pin system via different tibial tunnels for tibial fixation during anterior cruciate ligament reconstruction. BMC Musculoskelet Disord. 2020;21:736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |