Published online Nov 26, 2023. doi: 10.12998/wjcc.v11.i33.8078
Peer-review started: October 4, 2023
First decision: October 24, 2023
Revised: November 2, 2023
Accepted: November 17, 2023
Article in press: November 17, 2023
Published online: November 26, 2023
Processing time: 50 Days and 11.4 Hours
Hepatocellular carcinoma (HCC) is difficult to treat and has a high mortality rate, emphasizing the importance of early diagnosis and treatment. If characteristic radiologic findings and underlying liver disease are present, a diagnosis can be made without a biopsy. However, when HCC is accompanied by a liver abscess, diagnosis might be delayed by atypical radiologic findings. This case report aims to assist in the diagnosis of HCC, which can manifest in various forms.
A 75-year-old male presented to the Emergency Department with worsening fever and mental changes. He was diagnosed with liver cirrhosis six months earlier. Abdominal computed tomography (CT) raised our suspicion of an organized liver abscess. A follow-up CT scan after four weeks of antibiotic treatment showed a decrease in the liver lesion size. However, high fever recurred, and C-reactive protein increased to 14 mg/L. Aspiration of the liver lesion was performed, but no bacteria were identified. Blood culture revealed the presence of fungi. The patient received an additional four weeks of antibiotics and antifungal agents before being discharged. Approximately 10 mo later, a CT scan showed an increase in the lesion size, and biopsy was performed. The biopsy revealed an organized abscess with focal carcinomatous changes, for which surgery was performed. Postoperative histopathological examination revealed HCC, clear-cell variant. The nontumor liver tissue showed cirrhosis and an organized abscess.
Even if a liver abscess is suspected in a patient with cirrhosis, the possibility of HCC should be considered.
Core Tip: Hepatocellular carcinoma (HCC) is more difficult to treat and has a higher mortality rate than other carcinomas, emphasizing the importance of early diagnosis. Radiologic examination is crucial for diagnosing HCC. If characteristic findings and underlying liver disease are present, a diagnosis can be made, but when HCC is accompanied by a liver abscess, diagnosis may be delayed by atypical radiologic findings. The present patient was hospitalized for an organized liver abscess with calcification but was subsequently diagnosed with HCC. This case report aims to assist in the diagnosis of HCC, which can manifest in various forms.
- Citation: Ryou SH, Shin HD, Kim SB. Hepatocellular carcinoma presenting as organized liver abscess: A case report. World J Clin Cases 2023; 11(33): 8078-8083
- URL: https://www.wjgnet.com/2307-8960/full/v11/i33/8078.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i33.8078
Liver cancer ranks fifth in global cancer incidence and fourth in cancer-related death[1]. Over 80% of liver cancers are hepatocellular carcinoma (HCC), while intrahepatic cholangiocarcinoma accounts for 10%-15%[2]. The lower survival rate of liver cancer compared to other types of cancer is primarily due to the difficulty of curative treatment in advanced stages. Since HCC is often already advanced at the time of diagnosis, early diagnosis is crucial. This can be challenging when typical radiological findings are absent or when they are accompanied by other conditions. In particular, diagnosing HCC presenting as a liver abscess can be difficult, as the clinician may be unlikely to suspect hidden HCC in the presence of typical abscess symptoms such as fever, pain, and blood test findings. This case report describes a patient who was admitted with fever, sepsis, and acute pyelonephritis and displayed organized liver abscess findings with calcification in the liver. Initially, the liver abscess size decreased during treatment, but it later increased, leading to tissue biopsy and surgery, which confirmed the diagnosis of HCC. This report discusses our process of reaching the final diagnosis of HCC based on the patient's clinical course following the initial diagnosis of liver abscess.
A 75-year-old male visited the Emergency Department with worsening general weakness, loss of appetite, fever, and mental changes for 2-3 d.
General weakness, loss of appetite, and mild fever began 3 d earlier. The mental change that started 2 d prior prompted him visit the Emergency Department.
The patient had been admitted for general weakness six months prior, at which time he was diagnosed with liver cirrhosis (Child-Pugh Class A) based on abdominal ultrasound. The cause of the cirrhosis was unknown.
There was no history of malignancy or underlying liver disease in the family.
The patient's vital signs were as follows: Blood pressure 89/69 mmHg, respiratory rate 25 breaths/min, heart rate 112 beats/min and body temperature 38.2°C. As patient's consciousness was not clear at the time of admission to the Emergency Department, a proper physical examination could not be conducted. After the patient's consciousness improved, a physical examination was performed, during which the patient complained of discomfort and tenderness in the upper right abdomen.
Laboratory tests revealed white blood cell 13200/µL, hemoglobin 11.5 g/dL, platelet 57000/µL, C-reactive protein (CRP) 14 mg/L, aspartate aminotransferase/alanine aminotransferase 117/89 U/L, total bilirubin 2.3 mg/dL, albumin 3.1 g/dL, prothrombin time 15.7 S, blood urea nitrogen 34 mg/dL, creatinine 2.5 mg/dL, -fetoprotein (AFP) 2.8 ng/mL, protein induced by vitamin K absence II 18 mAU/mL, hepatitis B surface antigen/antibody (-/+), and anti- hepatitis C virus (-). Urinalysis showed nitrite (+) and many bacteria. Urine culture revealed extended-spectrum beta-lactamase-positive Escherichia coli.
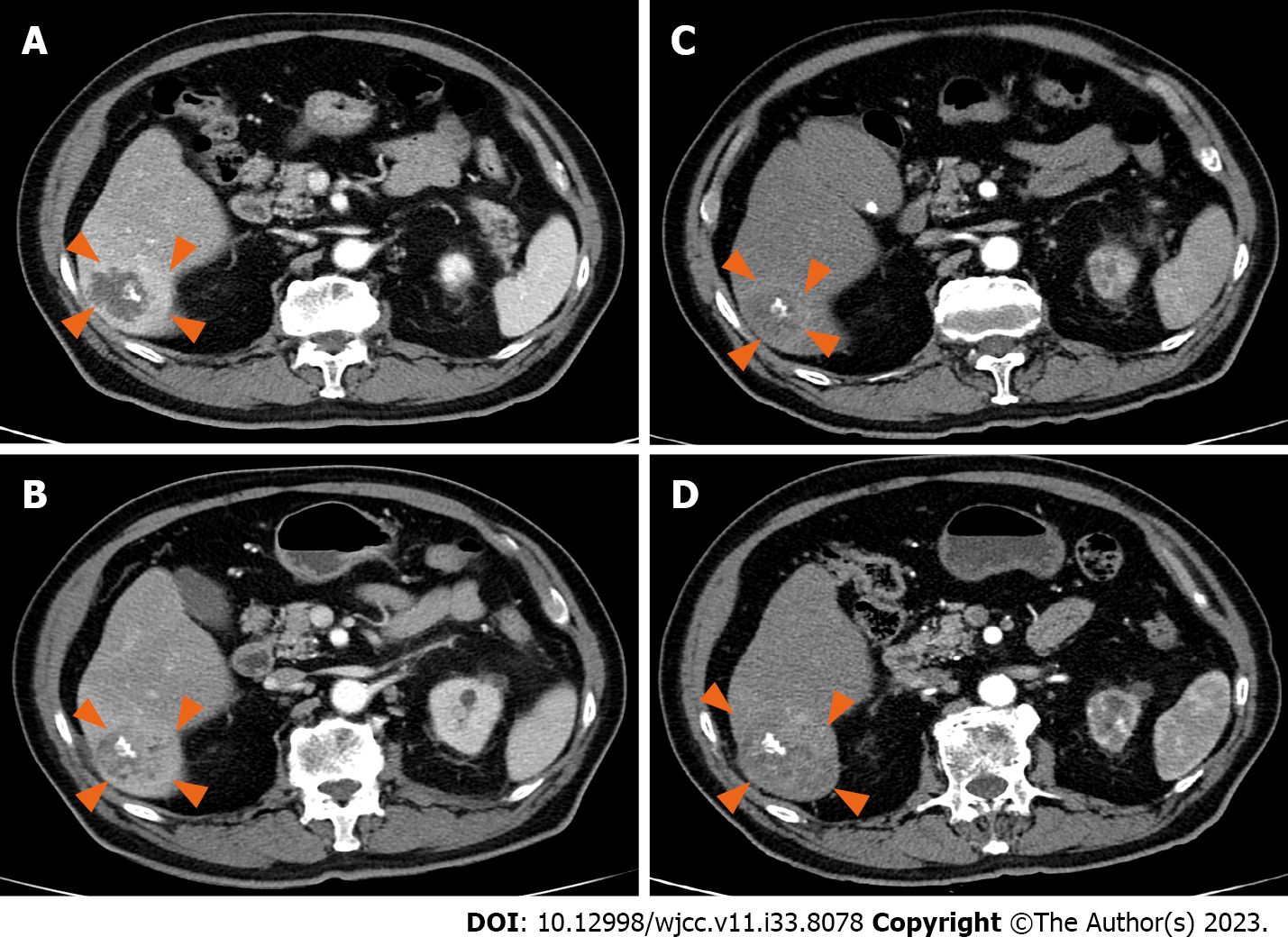
An abdominal CT performed in the Emergency Department revealed a lobulated, margined, multiseptated 3.9 cm cystic attenuating mass with central septal calcification and surrounding prolonged hyperemia in hepatic segment VI, raising our suspicion of an organized liver abscess (Figure 1A).
A follow-up CT scan four weeks later showed a decrease in the liver lesion size to 3.3 cm (Figure 1B), and CRP dropped to 0.7 mg/L. However, the patient experienced recurrence of high fever, and CRP increased to 14 mg/L. Aspiration of the liver lesion was performed, but no bacteria were identified. Blood culture revealed the presence of Candida glabrata. The patient's fever subsided, and CRP decreased following fluconazole administration. The patient received an additional four weeks of antibiotics and antifungal agents (micafungin) before being discharged.
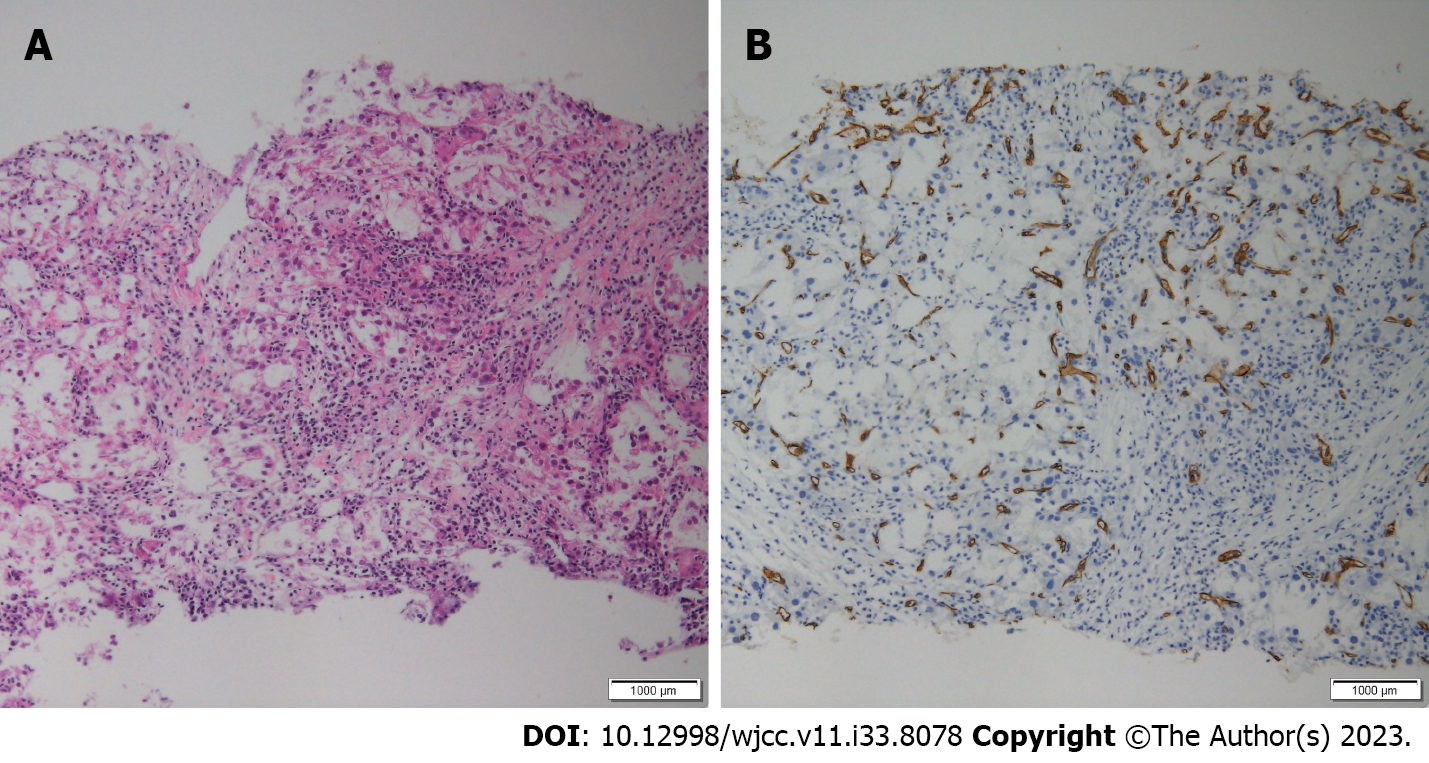
Six months later, the patient returned to the Emergency Department with left upper quadrant pain and decreased urine output. A CT scan revealed a ureter stone and a persistent 3.6 cm liver lesion (Figure 1C). Although biopsy was recommended, the patient's poor condition and lack of size change of the lesion led to a preference for follow-up. Liver magnetic resonance imaging could not be performed due to the patient's pacemaker insertion. Approximately 10 mo later, a CT scan showed an increase in the lesion size to 6 cm (Figure 1D), and biopsy was thus performed. The biopsy revealed an organized abscess with focal carcinomatous changes (Figure 2).
HCC presenting as organized liver abscess in patient with cirrhosis of unknown etiology.
Tumorectomy was performed given the patient’s performance and liver function.
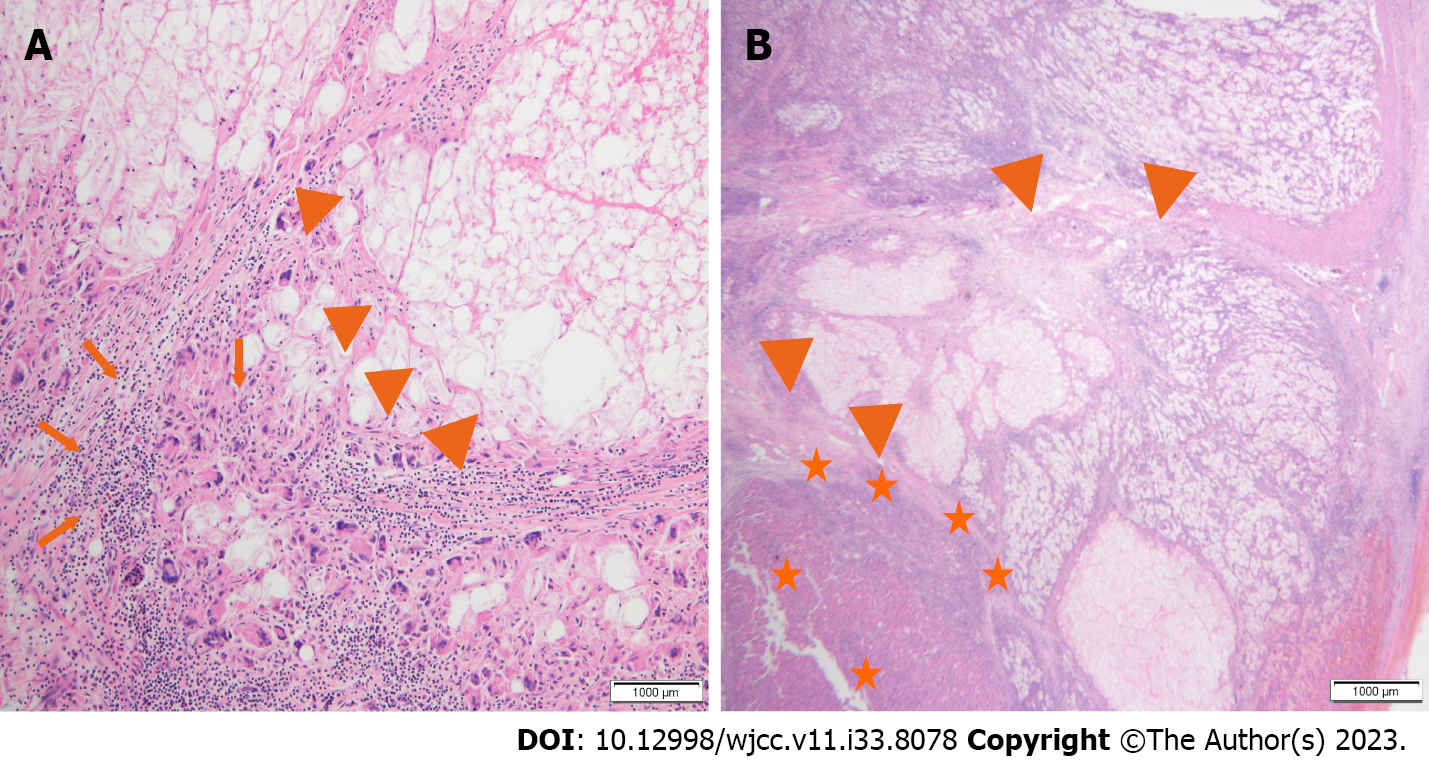
Postoperative histopathological examination revealed a tumor size of 6 cm 5 cm, and the diagnosis was HCC, clear-cell variant. The nontumor liver tissue showed hallmarks of both cirrhosis and abscess. This indicates that the abscess developed in HCC (Figure 3). The patient had multiple intense hypermetabolic enlarged lymph nodes in the common hepatic, portocaval, retrocaval, and SMA root areas on positron emission tomography CT scans performed during surgery. The Barcelona Clinic Liver Cancer stage was C. He is currently undergoing atezolizumab and bevacizumab treatment.
HCC is the fifth most common cancer worldwide, though its incidence is higher in countries such as South Korea, where the prevalence of chronic hepatitis B is high[1,2]. HCC ranks second only to lung cancer as a cause of cancer death in Korea, and it has the highest cancer mortality rate among people in their 40s and 50s. The high mortality rate can be attributed to the fact that HCC often occurs in patients with preexisting liver dysfunction, such as cirrhosis, leading to liver failure and death, or because it is diagnosed late because symptoms such as pain are often absent. Therefore, it is recommended that patients with chronic hepatitis or cirrhosis undergo ultrasound and blood tests every six months.
The diagnostic method of HCC varies slightly among countries, but it is mostly performed by radiological examinations. If a liver mass of 1 cm or larger is discovered in patients with chronic hepatitis, cirrhosis, or other underlying liver diseases and if dynamic liver CT or dynamic liver magnetic resonance imaging show arterial enhancement and early washout in the portal venous or venous phase, a diagnosis can be made without biopsy. In the past, AFP was included in the diagnostic criteria, but it is not included in recent guidelines[3-5]. In this case, the patient had underlying cirrhosis of unknown etiology. However, we did not initially consider HCC, as the findings were more indicative of a liver abscess. Notably, there was calcification inside the tumor in this case. When calcification is identified within a mass, it often leads to the assumption of a benign tumor. Unfortunately, this delayed diagnosis in this patient. It is difficult to find cases in which calcification is present within a mass.
In patients with HCC, fever and increased white blood cell counts can be present in 6%-54% of cases without infection[6-8]. However, the fever is usually low grade, and the increase in white blood cells is not severe. It is more accurate to attribute these symptoms to the tumor itself than to infection. Hypotheses have been put forward to explain these similarities, such as neoplasm-associated granulocytosis resulting from granulopoietin production by tumor cells and pyrogen production by malignant tumor cells or macrophages following tumor necrosis[9,10]. In cases such as this, where sepsis causes low blood pressure, severe leukocytosis, and elevated CRP, it is reasonable to suspect a liver abscess first, even if there is an underlying liver disease such as cirrhosis.
In cases in which a liver abscess is suspected, diagnosis of HCC can be delayed for several reasons. First, the infected necrotic cavities of HCC may appear similar to benign lesions, such as abscesses, on radiological examinations. Second, the presence of calcification in the liver suggests a benign lesion rather than a tumor. Third, if the size of the mass decreases and clinical symptoms improve after antibiotic treatment, the lesion may be a liver abscess, and treatment may continue. Fourth, even if liver biopsy is performed, HCC cells may not be detected due to necrosis or to the abscess, increasing the likelihood of dismissing HCC[11,12].
The mechanism by which HCC with liver abscess arises is thought to be similar to that of liver abscess alone. Bacteria that enter the liver through the blood or bile ducts can form a liver abscess inside the tumor. In cases such as this, where there is a systemic infection caused by urinary tract infection, it is highly likely that bacteria have infiltrated the HCC through the bloodstream. Furthermore, HCC has a rich blood supply and primarily receives blood from the hepatic artery, and thus an infection is more likely to be caused by bacteria from the blood. In such cases, careful attention should be given to the diagnosis of HCC through liver biopsy and other methods while treating liver abscesses. Moreover, even if biopsy results are negative, repeated biopsies may be necessary due to the possibility of false negatives.
Although HCC accompanied by liver abscess is rare, the overall prognosis is known to be poor[6,13]. This is due to both the delay in diagnosis, as in this case, and the fact that treating HCC is complicated when accompanied by a liver abscess. In other words, even if surgery is necessary, the postoperative mortality rate is high because of the accompanying infection, and although RFA and TACE can be performed, a cure is difficult to achieve because the tumor and abscess are mixed, and the risk of postoperative complications increases due to the infection. Therefore, the treatment method must be chosen by considering the patient's overall condition, the size of the tumor, and the state of the liver abscess.
When a liver mass is detected in a patient with an underlying liver disease, the possibility of HCC being accompanied by a liver abscess should be considered, even if a liver abscess is suspected or diagnosed. This case report might assist in the diagnosis and treatment of future cases of HCC accompanied by liver abscess.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maslennikov R, Russia; Pan Y, China S-Editor: Lin C L-Editor: A P-Editor: Lin C
| 1. | Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2838] [Cited by in RCA: 2962] [Article Influence: 370.3] [Reference Citation Analysis (0)] |
| 2. | Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2184] [Cited by in RCA: 2908] [Article Influence: 484.7] [Reference Citation Analysis (17)] |
| 3. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 6064] [Article Influence: 866.3] [Reference Citation Analysis (3)] |
| 4. | Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, Roberts LR, Heimbach JK. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2121] [Cited by in RCA: 3243] [Article Influence: 463.3] [Reference Citation Analysis (1)] |
| 5. | Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for management of chronic hepatitis B. Clin Mol Hepatol. 2022;28:276-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 81] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 6. | Yeh TS, Jan YY, Jeng LB, Chen TC, Hwang TL, Chen MF. Hepatocellular carcinoma presenting as pyogenic liver abscess: characteristics, diagnosis, and management. Clin Infect Dis. 1998;26:1224-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Kew MC, Geddes EW. Hepatocellular carcinoma in rural southern African blacks. Medicine (Baltimore). 1982;61:98-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 80] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Okuda K, Kondo Y, Nakano M, Kage M, Arakawa M, Kojiro M, Ohtsuki T, Shimokawa Y, Hirata M, Kohno K. Hepatocellular carcinoma presenting with pyrexia and leukocytosis: report of five cases. Hepatology. 1991;13:695-700. [PubMed] |
| 9. | Saar B, Kellner-Weldon F. Radiological diagnosis of hepatocellular carcinoma. Liver Int. 2008;28:189-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Smalley SR, Moertel CG, Hilton JF, Weiland LH, Weiand HS, Adson MA, Melton LJ 3rd, Batts K. Hepatoma in the noncirrhotic liver. Cancer. 1988;62:1414-1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Klotz SA, Penn RL. Clinical differentiation of abscess from neoplasm in newly diagnosed space-occupying lesions of the liver. South Med J. 1987;80:1537-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Takayama T, Makuuchi M, Kojiro M, Lauwers GY, Adams RB, Wilson SR, Jang HJ, Charnsangavej C, Taouli B. Early hepatocellular carcinoma: pathology, imaging, and therapy. Ann Surg Oncol. 2008;15:972-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Li C, Li G, Miao R, Lu X, Zhong S, Sang X, Mao Y, Zhao H. Primary liver cancer presenting as pyogenic liver abscess: characteristics, diagnosis, and management. J Surg Oncol. 2012;105:687-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |