Published online Nov 16, 2023. doi: 10.12998/wjcc.v11.i32.7761
Peer-review started: August 16, 2023
First decision: August 31, 2023
Revised: September 19, 2023
Accepted: November 8, 2023
Article in press: November 8, 2023
Published online: November 16, 2023
Processing time: 91 Days and 18.8 Hours
Perimenopausal is the period when women's ovarian function begins to decline before and after menopause. During this period, women experience a series of mental state changes, such as decreased hormone levels, decreased libido, and even female sexual dysfunction (FSD) in severe cases, which reduces their quality of life. Factors affecting the occurrence of FSD include physiological and non-physiological factors, among which physiological factors are uncontrollable. Therefore, it is particularly important to ascertain the related non-physiological factors that affect the occurrence of FSD for improving the quality of sexual life of perimenopausal women.
To investigate the mediating effect of depressive mood and body image on menopausal symptoms and sexual function in perimenopausal women.
A total of 186 perimenopausal women were enrolled between January 2019 and January 2021 and divided into the FSD (134 cases) and control (52 cases) groups based on the presence and absence of FSD. Clinical data were compared between the two groups. FSD-related factors were analyzed using logistic regression analysis. Hamilton Depression Scale (HAMD), Body Image Scale (BIS), and Menopause Rating Scale (MRS) scores were compared among women with different FSD scores. The correlation of the MRS score with the BIS and HAMD scores and the mediating effect of the BIS and HAMD scores on the MRS score and female sexual function index (FSFI) were analyzed.
The HAMD and BIS scores were higher in the FSD group than in the control group, and the difference in monthly income between the two groups was statistically significant (all P < 0.05). Monthly income of < 2000 yuan [odds ratio (OR) = 26.586, P = 0.000], BIS score (OR = 1.590, P = 0.000), and HAMD score (OR = 1.884, P = 0.000) were independent risk factors for FSD. MRS scores were positively correlated with BIS and HAMD scores (r = 0.358 and 0.244, P = 0.000 and 0.001, respectively) and negatively correlated with FSFI scores (r = -0.433, P = 0.000). Body image and depressive mood had partial mediating effects, accounting for 39.90% of the total effect.
Depression and body image play mediating roles between menopausal symptoms and sexual function in perimenopausal women.
Core Tip: Depressive mood and body image partially mediate the relationship between menopausal symptoms and sexual function in perimenopausal women, accounting for 39.90% of the total effect. Understanding these mediating factors can help inform interventions targeting sexual dysfunction in this population.
- Citation: Ling J, Wang YH. Association between depressive mood and body image and menopausal symptoms and sexual function in perimenopausal women. World J Clin Cases 2023; 11(32): 7761-7769
- URL: https://www.wjgnet.com/2307-8960/full/v11/i32/7761.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i32.7761
Perimenopause is the period before and after menopause, when a woman’s ovarian function begins to decline. During this period, women experience alterations in their mental state, hot flashes, sweating, excitement, and irritability[1,2], which is not conducive to physical and mental health. In addition to physical discomfort, a decrease in the hormone levels, genital tissue structure, and texture, as well as vaginal mucosal atrophy, may cause low sexual desire and difficulty in sexual arousal[3], and even worse, female sexual dysfunction (FSD), which is not good for the physical and mental health of women and is also detrimental to family harmony and quality of life[4].
Relevant studies have shown that women with severe menopausal symptoms are at higher risk of developing FSD. Besides physiological factors, the occurrence of FSD is associated with multiple non-physiological factors such as sexual health concepts, income levels, negative emotions, and body image[5,6]. Xiong et al[7] reported that 90% of FSD is caused by psychological factors and that body image is strongly associated with female sexual behavior[5], both of which play a non-negligible role in the mechanism of FSD. Nevertheless, there are few studies on the correlation among menopausal symptoms, depressive state, body image, and sexual function in perimenopausal women. Therefore, the present study investigated whether depressive state and body image play a mediating role between menopausal symptoms and sexual function to provide theoretical guidance for the improvement of sexual quality of life in perimenopausal women.
A total of 186 perimenopausal women were recruited between January 2019 and January 2021. The inclusion criteria were as follows: (1) Diagnosed perimenopausal women[8]; (2) signed informed consent; (3) married, spouse alive; (4) barrier-free communication and understanding of scale content; and (5) no history of mental illness before perimenopause. The exclusion criteria were as follows: (1) Mental disease; (2) estrogen replacement therapy; (3) heart, liver, kidney, and other vital organ disorders and severe chronic diseases; and (4) abnormal sexual function of the sexual partner, without sexual life for nearly four weeks. Women with a female sexual function index (FSFI) score < 26.55 were included in the FSD group (134 cases), and the rest were included in the control group (52 cases). Participants with a Menopause Rating Scale (MRS) score < 9 were included in the mild group, those with a score of 9-16 were included in the moderate group, and those with a score > 16 were included in the severe group. This study was approved by the Affiliated Hospital of Hunan Academy of Chinese Medicine.
Research methods: Baseline data such as age, spouse age, education level, and monthly income were collected and compared between the FSD and control groups to analyze FSD-related factors in perimenopausal women. Body image status and degree of depression [assessed using the Body Image Scale (BIS) and Hamilton Depression Scale (HAMD) scores, respectively] were compared among the mild, moderate, and severe groups. The correlation between the MRS score and BIS and HAMD scores were assessed. Additionally, the mediating effects of body image status and degree of depression on menopausal symptoms and sexual function were analyzed.
Assessment of sexual function and definition of FSD: FSFI[4] was used to measure sexual function and the scale was filled out independently by the patients. The scale contains 6 dimensions and 20 items, with 0-5 points for each dimension and 1-5 points for each item, and a total score of 36 points. The lower the score, the more severe the sexual dysfunction. FSD was defined by a total score of < 26.55.
Body image assessment: BIS[9] compiled by Hopwood et al was used to measure the body image of patients. The BIS scale was completed independently by patients. The scale contains 10 items with 0-3 points for each item. Zero, 1, 2, and 3 points represent “not at all,” “a little,” “quite a lot,” and “much”, respectively. The total score is 30 points, and the higher the score, the worse the body image.
Depression assessment: The HAMD[6] was used for depression assessment. The scale contains 21 items, with 0-4 scores for each item. A total score of 7-17, 17-24, and > 24 represents mild, moderate, and severe depression, respectively.
Assessment of the severity of menopausal symptoms: MRS was applied for the assessment of the severity of menopausal symptoms. The scale includes 11 items with physical, psychological, and genitourinary dimensions. Each item is scored as 0, 1, 2, 3, or 4 points for “asymptomatic,” “mild,” “moderate,” “severe,” and “very severe” symptoms, respectively. The total score is 44, with a score of < 4 for asymptomatic, 4-8 for mild, 9-16 for moderate, and 16-44 for severe symptoms.
Before the study, two medical staff members who guided participants in filling out the questionnaire were given uniform guidance language training, and the same guidance language was applied to all participants. The questionnaire was completed independently by patients in the outpatient department and issued and collected immediately.
Data were analyzed using SPSS 25.0 (IBM Corp., Armonk, NY, United States). Measurement data were expressed as mean ± SD. Differences between the groups were compared using the two-independent samples t-test. Count data were expressed as percentages [n (%)] and analyzed using the χ2 test. Analysis of variance (ANOVA) was used to compare differences among three or more groups. The Bonferroni method was used for the pairwise comparisons. The corrected P-value (P < 0.017) was used for the pairwise comparisons. Ranked data were analyzed using the rank-sum test to compare differences among groups. Multivariate logistic regression was used to analyze FSD-related factors in perimenopausal women. Pearson’s correlation analysis was used to analyze the correlation between the MRS score and the BIS and HAMD scores. A structural equation model of the correlation between menopausal symptoms, sexual function, body image, and depression was established to test the mediating effect of BIS and HAMD scores on the MRS score and FSFI. A mediating effect existed if the confidence interval was not 0. P < 0.05 was considered statistically significant.
The HAMD and BIS scores were higher in the FSD group than in the control group (P < 0.05). The difference in the monthly income between the two groups was significant (P < 0.05). There were no significant differences in the other data between the two groups (P > 0.05; Table 1).
| Factor | Control group (n = 52) | FSD group (n = 134) | t/χ2/Z | P value |
| Age (yr) | 47.78 ± 4.03 | 48.49 ± 3.65 | -1.156 | 0.249 |
| Spouse age (yr) | 51.14 ± 5.26 | 50.57 ± 4.80 | 0.707 | 0.480 |
| BMI (kg/m2) | 22.34 ± 2.75 | 22.86 ± 2.31 | -1.304 | 0.194 |
| Delivery times (time) | 2.64 ± 0.79 | 2.75 ± 0.92 | -0.760 | 0.448 |
| BIS score (point) | 9.33 ± 2.87 | 14.63 ± 4.52 | -7.856 | 0.000 |
| Education level, n (%) | ||||
| Junior high school and below | 34 (65.38) | 102 (76.12) | -1.542 | 0.123 |
| Senior middle school | 14 (26.92) | 27 (20.15) | ||
| College and above | 4 (7.69) | 5 (3.73) | ||
| Monthly income (yuan), n (%) | ||||
| < 2000 | 21 (40.38) | 100 (74.63) | -4.652 | 0.000 |
| 2000-5000 | 15 (28.85) | 23 (17.16) | ||
| > 5000 | 16 (30.77) | 11 (8.21) | ||
| HAMD score (point) | 7.83 ± 2.32 | 13.44 ± 3.65 | -10.296 | 0.000 |
| Retirement, n (%) | 24 (46.15) | 66 (49.25) | 0.144 | 0.704 |
Monthly income of < 2000 yuan [odds ratio (OR) = 26.586, P = 0.000], BIS score (OR = 1.590, P = 0.000), and HAMD score (OR = 1.884, P = 0.000) were all independent risk factors for FSD (Table 2).
| Factor | β value | Standard error | Wald | P value | Odds ratio | 95% confidence interval | |
| Monthly income | > 5000 yuan | 12.820 | 0.002 | 1.000 | |||
| < 2000 yuan | 3.280 | 0.942 | 12.117 | 0.000 | 26.586 | 4.193-168.579 | |
| 2000-5000 yuan | 1.854 | 0.977 | 3.603 | 0.058 | 6.387 | 0.941-43.341 | |
| BIS score | 0.464 | 0.107 | 18.941 | 0.000 | 1.590 | 1.290-1.959 | |
| HAMD score | 0.633 | 0.124 | 25.981 | 0.000 | 1.884 | 1.477-2.403 | |
A comparison of the clinical data in women with different degrees of menopausal symptoms is shown in Table 3. The BIS and HAMD scores were lower in the mild and moderate groups than in the severe group. The FSFI scores were higher in the mild and moderate groups than in the severe group (all P < 0.017). The MRS scores were positively correlated with the BIS and HAMD scores (r = 0.358 and 0.244, P = 0.000 and 0.001, respectively) and negatively correlated with the FSFI scores (r = -0.433, P = 0.000; Table 4).
| Factor | Mild group (n = 20) | Moderate group (n = 83) | Severe group (n = 83) | F/Z | P value |
| Age (yr) | 48.01 ± 1.54 | 48.62 ± 2.56 | 48.92 ± 2.09 | 1.336 | 0.265 |
| Spouse age (yr) | 49.30 ± 2.26 | 50.25 ± 3.80 | 50.17 ± 3.14 | 0.659 | 0.519 |
| Delivery times (time) | 2.24 ± 0.57 | 2.50 ± 0.96 | 2.58 ± 0.78 | 1.301 | 0.275 |
| Education level, n (%) | |||||
| Junior high school and below | 11 (55.00) | 65 (78.31) | 60 (71.29) | 4.484 | 0.106 |
| Senior middle school | 7 (35.00) | 14 (16.87) | 20 (24.10) | ||
| College and above | 2 (10.00) | 4 (4.82) | 3 (3.61) | ||
| Monthly income (yuan), n (%) | |||||
| < 2000 | 13 (65.00) | 51 (61.45) | 57 (68.67) | 1.468 | 0.480 |
| 2000-5000 | 5 (25.00) | 16 (19.28) | 17 (20.48) | ||
| > 5000 | 2 (10.00) | 16 (19.28) | 9 (10.84) | ||
| Retirement, n (%) | 9 (45.00) | 42 (50.60) | 48 (57.83) | 0.200 | 0.654 |
| BMI (kg/m2) | 22.06 ± 1.45 | 22.52 ± 2.23 | 22.73 ± 2.30 | 0.781 | 0.459 |
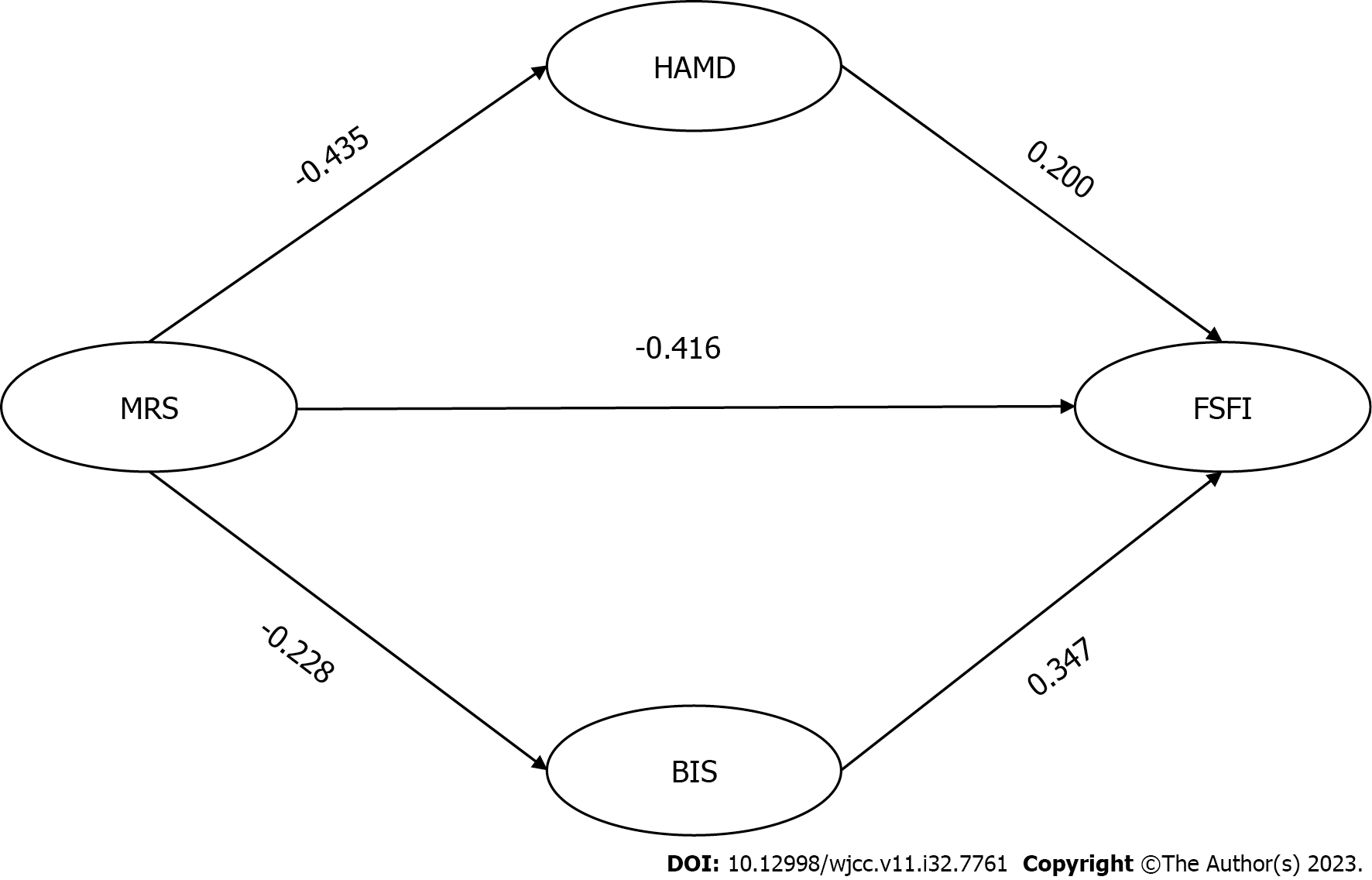
Body image and depressive mood were part of the mediating effect. The mediating effect accounted for 39.90% of the total effect (-0.166/-0.416), among which the HAMD and BIS score accounted for 20.91% and 18.99%, respectively (Figure 1 and Table 5).
| Effect | Effect | Standard error | t | P value | LLCI | ULCI | |
| Total effect | -0.416 | 0.064 | -6.524 | 0.000 | -0.542 | -0.290 | |
| Direct effect | -0.250 | 0.060 | -4.159 | 0.000 | -0.369 | -0.132 | |
| Mediating effect | HAMD score | -0.087 | 0.028 | -6.155 | 0.000 | -0.150 | -0.039 |
| BIS score | -0.079 | 0.025 | -3.623 | 0.000 | -0.138 | -0.036 | |
Perimenopause is a process involving ovarian dysfunction and sex hormone fluctuations. This stage is accompanied by symptoms of menopause, increased risk of various chronic diseases, and decline in reproductive function[10,11], causing varying degrees of negative changes to women’s physiological, psychological, and social relations. In addition to physical discomfort, another often-overlooked effect of perimenopause in women is FSD. A previous study showed that the incidence of FSD in perimenopausal women was as high as over 60%[3], which not only impacts mental health but also interferes with family harmony and stability. The occurrence of FSD cannot be separated from numerous independent risk factors. Besides physiological factors such as ovarian function decline, psychological factors also have a significant influence on the development of FSD[12]. Thus, our study investigated whether depression and body image play mediating roles.
Female sexual behavior is strongly associated with several social factors. In this study, there was a significant difference in the monthly income between the FSD and control groups. A monthly income < 2000 yuan was an independent risk factor for FSD. Jin et al[13] reported that age, menstruation, financial status, and hormone supplementation were related to female sexual function, which is consistent with previous results[14]. This may be because perimenopausal women with higher monthly income may have better living conditions and enthusiasm to seek medical treatment for menopausal symptoms[15], leading to a relatively lower incidence of FSD.
With increasing awareness of physical and mental diseases, the role of psychological factors in FSD has received considerable attention. The current study showed that the HAMD and BIS scores were higher in the FSD group than in the control group. Moreover, BIS and HAMD scores were independent risk factors for FSD. Body image and degree of depression are vital components of individual psychological factors. Body image is a complex experience mixed with the physical self, social self, and psychological self[16], while the degree of depression is a common negative emotion of perimenopausal women, and both affects women’s sexual behavior at a non-physiological level. Perimenopausal women are often accompanied by depression, irritability, and fatigue due to the fluctuation of sex hormones[17]. An Iranian study[18] demonstrated that depressed emotions were associated with a loss of interest, energy, and self-esteem among patients. Women in depressed states find it difficult to express their emotions and desires, which hinders their willingness to engage in sexual behaviors[18]. Simultaneously, depressive mood was an independent risk factor for FSD in perimenopausal women[19,20]. These findings are consistent with our results. Physical and psychological changes during perimenopause can diminish self-confidence and worsen body image in women. Negative self-body image contributes to resistance to sexual behavior and thus reduces sexual desire and response[21], thereby resulting in the occurrence of FSD.
Health management of menopausal women should not only address their physical condition but also their psychological needs. Our study showed that the MRS, BIS, and HAMD scores were lower in the mild and moderate groups than in the severe group. The MRS scores were positively correlated with the BIS and HAMD scores. Menopausal symptoms can affect psychological factors in perimenopausal women, and such women are often troubled by several physiological changes, such as hot flashes and sweating, insomnia, paresthesia, body shape change, and headache[10]. The discomfort induced by these menopausal symptoms can affect women’s mental states and attitudes toward menopause, ultimately aggravating negative evaluations of body image and depression. Hong et al[22] reported that menopausal symptoms are associated with body image, depression, and sexual communication, which mediates the correlation between menopausal symptoms and sexual function. It is also indicated that the effect of menopausal symptoms on sexual function in perimenopausal women includes both physiological and psychological factors.
Our data showed that the MRS score was negatively correlated with the FSFI, and body image and depressive mood had a partial mediating effect on menopausal symptoms and sexual function, accounting for 39.90% of the total effect, of which the HAMD and BIS scores accounted for 20.91% and 18.99%, respectively. Specifically, the MRS score negatively predicted the HAMD and BIS scores, whereas the HAMD and BIS scores positively predicted the FSFI score. These results reveal that menopausal symptoms affect sexual function, in part, through depressive mood and body image. This suggested that the improvement in sexual function of perimenopausal women could be achieved by improving body image and mood as well as self-cognition and negative emotions. Therefore, the sexual function of perimenopausal women can be improved from a multi-dimensional perspective. In addition to sex hormone replacement therapy and pelvic floor muscle training, the following is recommended to improve the sexual function of perimenopausal women: (1) Providing sexual health education to both spouses and strengthen sexual communication; (2) psychological intervention and antidepressant medication if necessary; (3) instructing women to exercise with body image as the target; and (4) advising family members and friends to support and tolerate perimenopausal women and encourage mutual communication. Furthermore, HAMD and BIS scores played a partial mediating role, suggesting that there may be other variables affecting sexual function, which will be the focus of future studies.
Nonetheless, this study has some limitations. The scales used are all filled out subjectively by the patients, and the samples needed to be expanded to reduce bias in the results. Moreover, there are only a handful of studies on this topic, which warrants further studies with larger sample sizes to validate our conclusions.
In summary, body image and the degree of depression in perimenopausal women have a partial mediating effect on menopausal symptoms and sexual function. In addition to the treatment of menopausal symptoms, close attention should also be paid to negative emotions and body image, to improve the sexual function in perimenopausal women.
Perimenopause is the period when women's ovarian function begins to decline before and after menopause. During this period, women experience a series of mental state changes, such as decreased hormone levels, decreased libido, and even female sexual dysfunction (FSD) in severe cases, which reduces their quality of life. Factors affecting the occurrence of FSD include physiological and non-physiological factors, among which physiological factors are uncontrollable. Therefore, it is particularly important to ascertain the related non-physiological factors that affect the occurrence of FSD for improving the quality of sexual life of perimenopausal women.
To observe the related non physiological factors that affect the occurrence of perimenopausal FSD, and to improve the quality of sexual life of perimenopausal women.
To investigate the mediating effect of depressive mood and body image on menopausal symptoms and sexual function in perimenopausal women.
Analysis of variance (ANOVA), Bonferroni method, rank-sum test, multivariate logistic regression, and Pearson correlation analysis.
The Hamilton Depression Scale (HAMD) and Body Image Scale (BIS) scores were higher in the FSD group than in the control group. Monthly income of < 2000 yuan, BIS score, and HAMD score were independent risk factors for FSD. The MRS scores were positively correlated with the BIS and HAMD scores and negatively correlated with the female sexual function index scores. Body image and depressive mood had partial mediating effects, accounting for 39.90% of the total effect.
Depression and body image play mediating roles between menopausal symptoms and sexual function in perimenopausal women.
This study shows that depression and body image play mediating roles between menopausal symptoms and sexual function in perimenopausal women, and reasonable countermeasures can be considered in clinic.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Griffiths M, United Kingdom; Mastrantonio E, Italy S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Willi J, Ehlert U. Assessment of perimenopausal depression: A review. J Affect Disord. 2019;249:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Khanna A, John F, Das S, Thomas J, Rao J, Maliakel B, Im K. Efficacy of a novel extract of fenugreek seeds in alleviating vasomotor symptoms and depression in perimenopausal women: A randomized, double-blinded, placebo-controlled study. J Food Biochem. 2020;44:e13507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Gordon JL, Halleran M, Beshai S, Eisenlohr-Moul TA, Frederick J, Campbell TS. Endocrine and psychosocial moderators of mindfulness-based stress reduction for the prevention of perimenopausal depressive symptoms: A randomized controlled trial. Psychoneuroendocrinology. 2021;130:105277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Martins WP, Lara LA, Ferriani RA, Rosa-E-Silva AC, Figueiredo JB, Nastri CO. Hormone therapy for female sexual function during perimenopause and postmenopause: a Cochrane review. Climacteric. 2014;17:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Mishra VV, Nanda S, Vyas B, Aggarwal R, Choudhary S, Saini SR. Prevalence of female sexual dysfunction among Indian fertile females. J Midlife Health. 2016;7:154-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Kucur Suna K, Ilay G, Aysenur A, Kerem Han G, Eda Ulku U, Pasa U, Fatma C. Effects of Infertility Etiology and Depression on Female Sexual Function. J Sex Marital Ther. 2016;42:27-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Xiong XT, Jin LJ. Research advance on the relationship between hypertension, antihypertensive drugs and female sexual function. Zhonghua Gaoxueya Zazhi. 2019;27:323-326. |
| 8. | Ruan XY, Yang X. Expert consensus on the diagnosis and treatment of perimenopausal abnormal uterine bleeding. Xiehe Yixue Zazhi. 2018;9:313-319. |
| 9. | Paterson CL, Lengacher CA, Donovan KA, Kip KE, Tofthagen CS. Body Image in Younger Breast Cancer Survivors: A Systematic Review. Cancer Nurs. 2016;39:E39-E58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 207] [Cited by in RCA: 183] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 10. | Culbert KM, Thakkar KN, Klump KL. Risk for midlife psychosis in women: critical gaps and opportunities in exploring perimenopause and ovarian hormones as mechanisms of risk. Psychol Med. 2022;52:1612-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Kanadys K, Wiktor-Stoma A, Lewicka M, Sulima M, Wiktor H. Predictors of the quality of life of women in peri-menopausal period. Ann Agric Environ Med. 2016;23:641-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Dombek K, Capistrano EJ, Costa AC, Marinheiro LP. Risk factors associated with sexual dysfunction in Brazilian postmenopausal women. Int J Impot Res. 2016;28:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Jin FY, Ruan XY, Mueck AO, Liu YL, Du J. Investigation on sexual dysfunction of female patients in hospital (analysis of 420 cases). Beijing Yixue. 2017;39:1135-1137. |
| 14. | Yisma E, Eshetu N, Ly S, Dessalegn B. Prevalence and severity of menopause symptoms among perimenopausal and postmenopausal women aged 30-49 years in Gulele sub-city of Addis Ababa, Ethiopia. BMC Womens Health. 2017;17:124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Li RX, Ma M, Xiao XR, Xu Y, Chen XY, Li B. Perimenopausal syndrome and mood disorders in perimenopause: prevalence, severity, relationships, and risk factors. Medicine (Baltimore). 2016;95:e4466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Chang SR, Yang CF, Chen KH. Relationships between body image, sexual dysfunction, and health-related quality of life among middle-aged women: A cross-sectional study. Maturitas. 2019;126:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Maki PM, Kornstein SG, Joffe H, Bromberger JT, Freeman EW, Athappilly G, Bobo WV, Rubin LH, Koleva HK, Cohen LS, Soares CN. Guidelines for the Evaluation and Treatment of Perimenopausal Depression: Summary and Recommendations. J Womens Health (Larchmt). 2019;28:117-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 112] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 18. | Yazdanpanahi Z, Nikkholgh M, Akbarzadeh M, Pourahmad S. Stress, anxiety, depression, and sexual dysfunction among postmenopausal women in Shiraz, Iran, 2015. J Family Community Med. 2018;25:82-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | Kucukdurmaz F, Inanc Y, Resim S. Sexual dysfunction and distress in premenopausal women with migraine: association with depression, anxiety and migraine-related disability. Int J Impot Res. 2018;30:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Gozuyesil E, Gokyildiz Surucu S, Alan S. Sexual function and quality-of-life-related problems during the menopausal period. J Health Psychol. 2018;23:1769-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Nazarpour S, Simbar M, Tehrani FR. Factors affecting sexual function in menopause: A review article. Taiwan J Obstet Gynecol. 2016;55:480-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 22. | Hong JH, Kim HY, Kim JY, Kim HK. Do psychosocial variables mediate the relationship between menopause symptoms and sexual function in middle-aged perimenopausal women? J Obstet Gynaecol Res. 2019;45:1058-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |