Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3625
Peer-review started: January 14, 2023
First decision: January 30, 2023
Revised: February 14, 2023
Accepted: April 13, 2023
Article in press: April 13, 2023
Published online: May 26, 2023
Processing time: 131 Days and 14.8 Hours
Portal vein embolization (PVE) is an effective and relatively safe procedure performed prior to major hepatic resection to enhance future liver remnant. Non-target embolization during PVE is rare, and if it occurs, it usually affects the future liver remnant. Intrahepatic portosystemic venous fistulas are extremely rare in non-cirrhotic livers. We report a case of non-targeted lung embolization during PVE due to an unrecognized intrahepatic portosystemic fistula.
A 60-year-old male presented with metastatic colon cancer of the liver. The patient underwent preoperative right PVE. During the embolization procedure, a small amount of glue and lipiodol emulsion was embolized to the heart and lungs through an unrecognized intrahepatic portosystemic fistula. The patient remained clinically stable and underwent the planned hepatic resection after 4 wk, with an uneventful postoperative course.
Conventional portograms and careful evaluation prior to PVE are advisable to avoid such complications.
Core Tip: Portal vein embolization (PVE) is relatively safe procedure done prior to major hepatic resection to enhance the future remnant liver. Intrahepatic portosystemic venous fistula is very rare in non-cirrhotic liver. Non-target embolization is a rare complication of such a procedure. This is the first case report of non-target lung embolization during PVE through a portosystemic venous fistula. Failure of recognition of this rare vascular abnormality led to this rare complication. In our case, we emphasize on careful evaluation of conventional portogram prior to PVE to avoid such complication.
- Citation: Alharbi SR, Bin Nasif M, Alwaily HB. Non-target lung embolization during portal vein embolization due to an unrecognized portosystemic venous fistula: A case report. World J Clin Cases 2023; 11(15): 3625-3630
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3625.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3625
Preoperative portal vein embolization (PVE) is a standard procedure to enhance the size of the future remnant liver. It is a simple and relatively safe procedure, with a low complication rate. Non-target embolization (NTE) is a known, infrequent complication of PVE and usually involves embolization of the future remnant liver portal vein branches[1-3]. Non-targeted lung embolization during PVE has not been reported in the scientific English literature.
Intrahepatic vascular fistula and shunt are used as synonymous and are defined as intrahepatic abnormal vascular connections between the hepatic artery, hepatic vein, and the portal vein. Intrahe
Our objective with this case report is to describe this rare complication due to a rare vascular malformation and to reinforce the value of intraprocedural conventional portography for vascular abnormalities, even if contrast-enhanced computed tomography (CT) or magnetic resonance images appears normal.
A 60-year-old male patient with metastatic colon cancer of the liver was referred to interventional radiology for right PVE prior to major hepatic resection.
He was diagnosed with sigmoid colon cancer and underwent anterior resection surgery 6 mo back. He developed liver metastasis for which right liver lobe resection was planned by a hepatobiliary surgeon. Due to a small left liver lobe, preoperative right PVE is requested to enhance the volume of the residual left liver lobe.
He is a known case of diabetes mellitus Type 2 Stage 3 on insulin and metformin for 9 years.
His personal and family history is unremarkable.
General examinations did not reveal any abnormality. Abdominal examinations revealed surgical scars from previous laparoscopic surgery and a stoma. No others abnormality could be detected.
The laboratory results of routine hematological testing, blood sedimentation rate, and tumor-associated markers were within normal limits. Alpha-fetoprotein is 14 ng/mL. Carcinoembryonic antigen is 2.4 ng/mL. Carbohydrate antigen 19-9 is 19 U/mL.
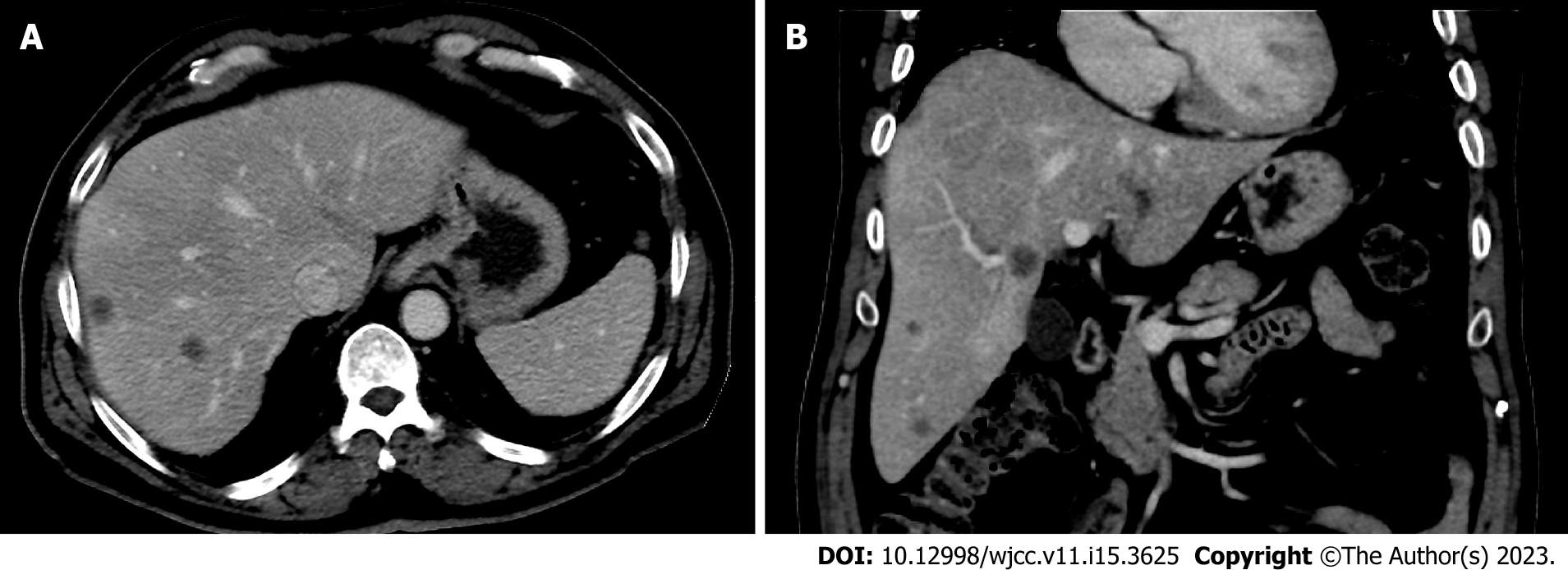
He underwent contrast-enhanced CT, which showed multiple right hepatic metastasis, small left hepatic lobe, and a normal patent portal venous system with a standard anatomy (Figure 1).
He was diagnosed with metastatic colon cancer to the liver. Secondary diagnosis is diabetes mellitus Type 2 Stage 3 on insulin and metformin. Management strategy is to prevent complications and the hemoglobin A1c goal is less than 7%.
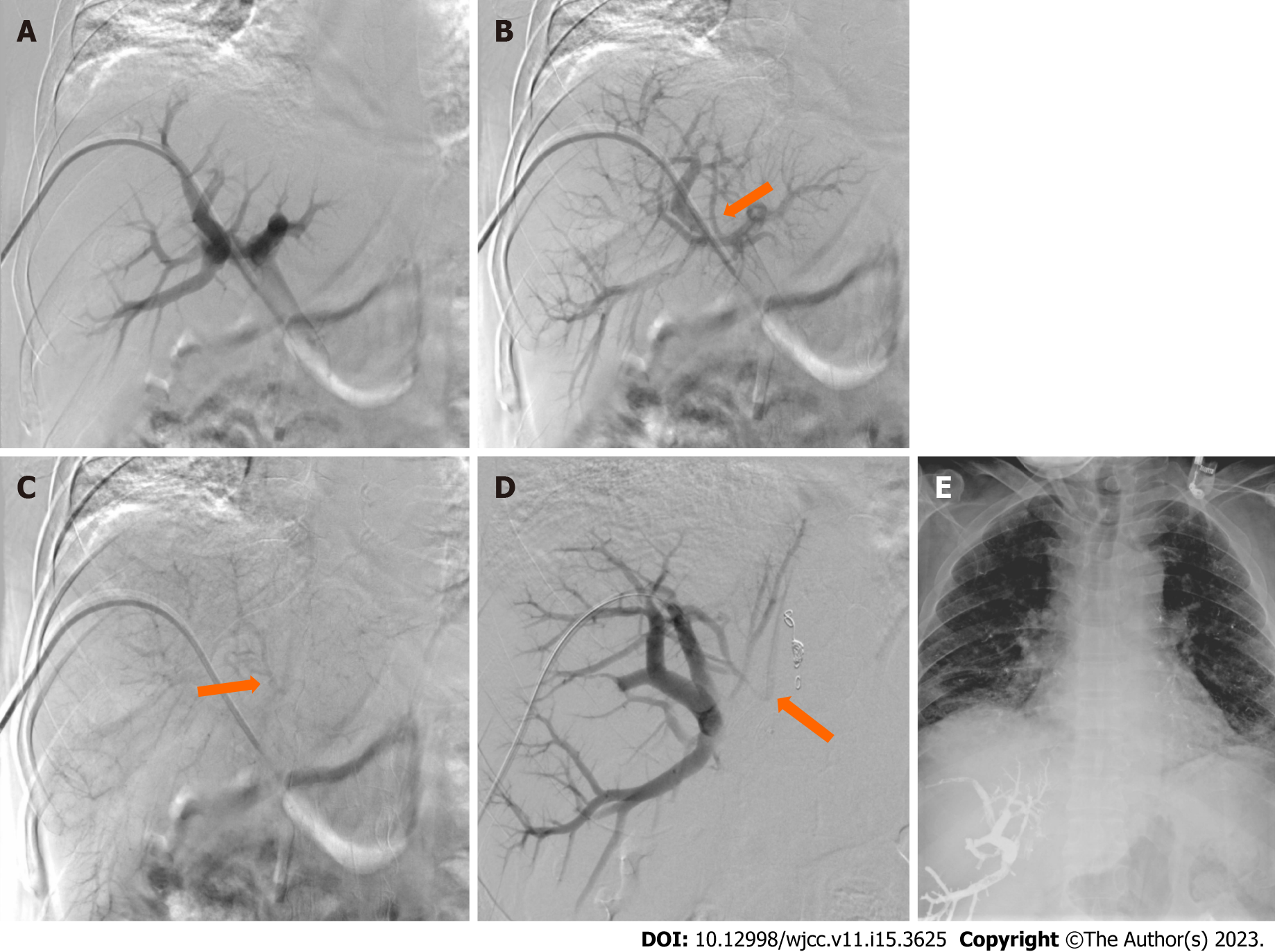
Patient underwent right PVE with intention to increase the volume of the future liver remanent. During the procedure, the ipsilateral right portal vein approach was used, and a portogram was carried out. Subsequently, right PVE was performed using an Amplatzer vascular plug, followed by glue and lipiodol emulsion injection in 1-8 ration and total amount is 9 mL. During glue and lipiodol emulsion injection, a small amount of emulsion flowed into the heart and the lungs bilaterally through a small intrahepatic portosystemic venous shunt/fistula creating a communication between the right portal vein and the inferior vena cava (IVC) (Figure 2). The patient’s condition remained clinically stable. His oxygen saturation remained 92% on room air. A supplementary oxygen vial nasal cannula was given, and patient was monitored for 2 h then shifted to patient ward in same stable condition. Conservative management and observation for the asymptomatic NTE to his lungs was decided after discussion with primary team and interventional radiologist.
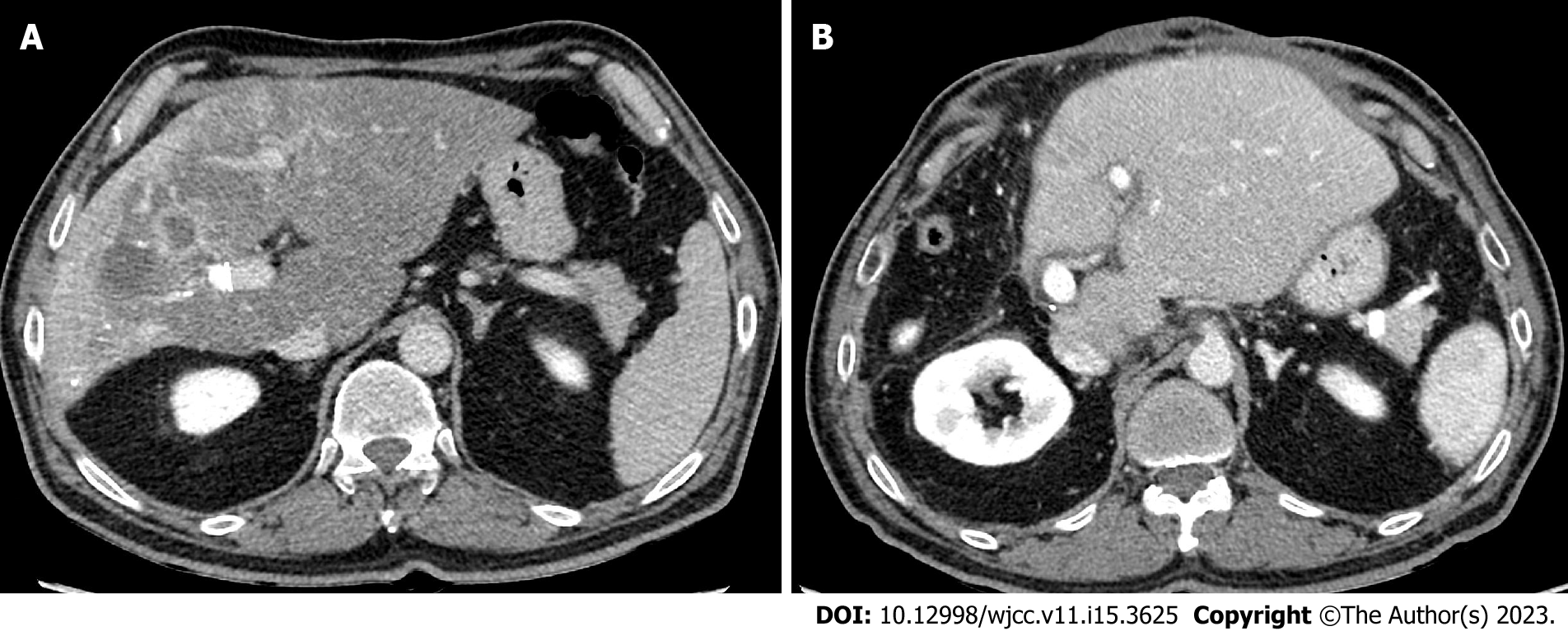
After four weeks, the patient underwent imaging which confirmed successful right PVE and adequate hypertrophy of left hepatic lobe. He underwent the planned right hepatectomy and had an uneventful postoperative course (Figure 3).
PVE is a known and effective procedure with a few contraindications, including portal vein thrombus and portal hypertension. Most patients do not experience serious postpreparative complications, and minor complications can occur in up to 12% of patients, some of which might potentially lead to non-resectability[2,3,6]. PVE complications include hematoma formation, vascular injury, infection, and NTE of the future liver remnants and other organs in the body[6,7]. While there may be no evidence of this during intraprocedural imaging, NTE is a highly recognized potential complication during all embolization procedures. NTE occurs when the embolic material migrates outside the desired area of treatment, leading to different consequences, the severity of which depends on the location of the reflux, functional status of the organ, amount and type of embolic material used, and general condition of the patient[8,9].
Intrahepatic portosystemic venous shunts and fistulas are rare disorders that describe an abnormal connection between the portal and systemic veins[10]. Most portosystemic shunts are congenital and asymptomatic, whereas acquired portosystemic shunts are secondary to cirrhosis, trauma, and surgery[11,12]. Intrahepatic portosystemic vascular malformations are rare in non-cirrhotic livers[13]. Radiological evaluation of portosystemic fistula is performed using color Doppler ultrasonography, CT, and magnetic resonance imaging[4].
Four morphological types of congenital intrahepatic portosystemic venous shunts have been described in the literature; the most common is Type I, which consists of a single vessel that directly connects the right portal vein to the IVC. Type II shunts involve one hepatic segment and consist of either a single communication or multiple communications between peripheral portal and hepatic venous branches. Type III of shunt involves direct communication between peripheral portal and hepatic venous branches through an aneurysmal segment. Type IV involves more than one hepatic segment and consists of multiple communicating peripheral portal and hepatic venous branches[5].
Although most of the cases are asymptomatic and incidentally discovered on imaging, hepatic encephalopathy, hepatopulmonary syndrome, and pulmonary hypertension are well-known clinical manifestations. Observation and monitoring are acceptable options for asymptomatic adult patients and treatment depends in occurrence and severity of symptoms[11].
There is no standards treatment protocol exist. Interventional radiology management by mean of coils or vascular plugs embolization is the least invasive and the preferred option. Surgical ligation, hepatic resection or liver transplantation are more invasive options and are preserved for extrahepatic or large multifocal intrahepatic shunts that are not amenable for embolization[11].
In our case, a portosystemic venous fistula Type 1 was unrecognized. If it is recognized early, it is preferable to embolize it first and then continue with PVE, based on our clinical experience.
Although intrahepatic portosystemic venous fistula is rare in non-cirrhotic livers, careful evaluation of portal vein anatomy, especially with conventional portography, is mandatory before PVE to avoid NTE.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bains L, India; Liu S, China S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY
| 1. | Narula N, Aloia TA. Portal vein embolization in extended liver resection. Langenbecks Arch Surg. 2017;402:727-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Di Stefano DR, de Baere T, Denys A, Hakime A, Gorin G, Gillet M, Saric J, Trillaud H, Petit P, Bartoli JM, Elias D, Delpero JR. Preoperative percutaneous portal vein embolization: evaluation of adverse events in 188 patients. Radiology. 2005;234:625-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Ganeshan DM, Szklaruk J. Portal vein embolization: cross-sectional imaging of normal features and complications. AJR Am J Roentgenol. 2012;199:1275-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Ulus S, Ertan Akan G, Erol C. Aneurysm of Portosystemic Fistula: A Case Report and Review of Literature. Euroasian J Hepatogastroenterol. 2017;7:178-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Bayona Molano MDP, Krauthamer A, Barrera JC, Luna C, Castillo P, Swersky A, Bhatia S. Congenital intrahepatic portosystemic venous shunt embolization: A two-case experience. Clin Case Rep. 2020;8:761-766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Yeom YK, Shin JH. Complications of Portal Vein Embolization: Evaluation on Cross-Sectional Imaging. Korean J Radiol. 2015;16:1079-1085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Denys A, Prior J, Bize P, Duran R, De Baere T, Halkic N, Demartines N. Portal vein embolization: what do we know? Cardiovasc Intervent Radiol. 2012;35:999-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Ingraham CR, Johnson GE, Nair AV, Padia SA. Nontarget embolization complicating transarterial chemoembolization in a patient with hepatocellular carcinoma. Semin Intervent Radiol. 2011;28:202-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Pardo Moreno P, Ruiz Villaverde G, Ciampi Dopazo JJ, Navarro VP. Novel reflux-control microcatheter: an alternative to maximize the effect of superselective embolization. Intervencionismo. 2020;20:126-133. [DOI] [Full Text] |
| 10. | Tsitouridis I, Sotiriadis C, Michaelides M, Dimarelos V, Tsitouridis K, Stratilati S. Intrahepatic portosystemic venous shunts: radiological evaluation. Diagn Interv Radiol. 2009;15:182-187. [PubMed] |
| 11. | Papamichail M, Pizanias M, Heaton N. Congenital portosystemic venous shunt. Eur J Pediatr. 2018;177:285-294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (1)] |
| 12. | Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A. Congenital and acquired anomalies of the portal venous system. Radiographics. 2002;22:141-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 175] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Tsai CW, Kuo CC, Huang CC. Spontaneous, non-cirrhotic, intrahepatic porto-systemic shunt presenting as acute encephalopathy. Liver Int. 2014;34:1603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |