Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.2981
Peer-review started: November 12, 2022
First decision: January 30, 2023
Revised: February 10, 2023
Accepted: March 31, 2023
Article in press: March 31, 2023
Published online: May 6, 2023
Processing time: 164 Days and 0.4 Hours
Cardiovascular disease is the most prevalent disease worldwide and places a great burden on the health and economic welfare of patients. Cardiac surgery is an important way to treat cardiovascular disease, but it can prolong mechanical ventilation time, intensive care unit (ICU) stay, and postoperative hospitalization for patients. Previous studies have demonstrated that preoperative inspiratory muscle training could decrease the incidence of postoperative pulmonary complications.
To explore the effect of preoperative inspiratory muscle training on mechanical ventilation time, length of ICU stay, and duration of postoperative hospitalization after cardiac surgery.
A literature search of PubMed, Web of Science, Cochrane Library, EMBASE, China National Knowledge Infrastructure, WanFang, and the China Science and Technology journal VIP database was performed on April 13, 2022. The data was independently extracted by two authors. The inclusion criteria were: (1) Randomized controlled trial; (2) Accessible as a full paper; (3) Patients who received cardiac surgery; (4) Preoperative inspiratory muscle training was implemented in these patients; (5) The study reported at least one of the following: Mechanical ventilation time, length of ICU stay, and/or duration of postoperative hospitalization; and (6) In English language.
We analyzed six randomized controlled trials with a total of 925 participants. The pooled mean difference of mechanical ventilation time was -0.45 h [95% confidence interval (CI): -1.59-0.69], which was not statistically significant between the intervention group and the control group. The pooled mean difference of length of ICU stay was 0.44 h (95%CI: -0.58-1.45). The pooled mean difference of postoperative hospitalization was -1.77 d in the intervention group vs the control group [95%CI: -2.41-(-1.12)].
Preoperative inspiratory muscle training may decrease the duration of postoperative hospitalization for patients undergoing cardiac surgery. More high-quality studies are needed to confirm our conclusion.
Core Tip: For cardiac surgery patients, the use of inspiratory muscle training could reduce the incidence of postoperative pulmonary complications according to previous research. Our study demonstrated that it could shorten the duration of postoperative hospitalization and thus may decrease overall costs. More research is needed to explore the effect of inspiratory muscle training on mechanical ventilation time and length of intensive care unit stay.
- Citation: Wang J, Wang YQ, Shi J, Yu PM, Guo YQ. Effect of preoperative inspiratory muscle training on postoperative outcomes in patients undergoing cardiac surgery: A systematic review and meta-analysis. World J Clin Cases 2023; 11(13): 2981-2991
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/2981.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.2981
Cardiovascular disease (CVD) has a high incidence rate and high mortality worldwide. CVD has been one of the most prevalent causes of death in the United States since 1975, accounting for 25% of all deaths[1]. The World Health Organization reported that in 2015 CVD caused an estimated 17.7 million deaths globally, making CVD the most prevalent cause of death worldwide. The economic burden of CVD is greater than that of Alzheimer’s disease and diabetes, with calculated indirect costs of $237 billion per year and a projected increase to $368 billion by 2035[2]. A study reported a national economic loss of $8.8 trillion from 2012 to 2030 due to CVD in China[3]. Cardiac surgery is an important treatment for coronary heart disease and other structural heart diseases. Due to the complex surgical procedures, surgical trauma, and long surgery time, patients often need postoperative mechanical ventilation and intensive care unit (ICU) admission for observation and further treatment. Meanwhile, postoperative pulmonary complications (PPCs) are one of the major causes of prolonged hospitalization and death[4,5]. Indeed, pulmonary complications following coronary artery bypass graft (CABG) operation were reported to be associated with significantly longer hospital stays (8.2 d vs 10.0 d, 95% confidence interval [CI]: 0.3-3.3)[6]. The incidence of PPCs prolongs the hospitalization length and thus increases the hospitalization expenses. Vonlanthen et al[7] performed a cost analysis of 1200 patients undergoing major surgery and revealed that costs increased with the severity of postoperative complications. This increase in costs is up to 5 times that of a similar surgery without complications. Thompson et al[8] included 618495 patients who underwent an intra-abdominal surgery. They found that postoperative hospital-acquired pneumonia increased the mean hospitalization length by 11 d, which translated to a mean increase in total hospital charges of $31000 (study performed in the year 2000). Other studies have also demonstrated that postoperative complications can increase the expense of surgery[9-11].
Preoperative inspiratory muscle training (IMT) has attracted increasing attention from doctors. Previous studies demonstrated that preoperative IMT can reduce the incidence of PPCs. Hulzebos et al[12] reported that preoperative IMT reduced the incidence of PPCs and the postoperative stay in hospital in patients at high risk of developing pulmonary complications after CABG surgery. Katsura et al[13] found evidence that preoperative IMT was associated with a reduction in postoperative atelectasis, pneumonia, and duration of hospital stay in adults after cardiac and major abdominal surgery. Fagevik Olsén et al[14] reported that preoperative physiotherapy education and training sessions can reduce PPC incidence in patients receiving open major abdominal surgery. Boden et al[15] confirmed the findings in their trial in 2017. However, there are few studies reporting the effects of preoperative IMT on length of mechanical ventilation, length of ICU stay, and duration of postoperative hospitalization. Our study aimed to answer the following questions: (1) Does preoperative IMT shorten the time of mechanical ventilation and ICU stay; and (2) Does preoperative IMT reduce the duration of postoperative hospitalization and thus save money for patients?
We searched the English literature databases, which included PubMed, Web of Science, Cochrane Library, and EMBASE, and Chinese literature databases, which included China National Knowledge Infrastructure, WanFang, and China Science and Technology journal VIP. Our search strategies were composed of: (1) Patients (experimental: Cardiac surgery/heart surgery); (2) Intervention (preoperative IMT/preoperative respiratory muscle training); (3) Control (-); and (4) Outcome (mechanical ventilation/MV/intensive care unit/ICU/postoperative stay in hospital/duration of postoperative hospitalization). We searched the databases through April 13, 2022. Two researchers independently assessed the eligibility of papers by title and abstract. When there was insufficient information to judge the qualification of the study in the title and abstract, the whole paper was assessed. When the two researchers disagreed, a third researcher was consulted to reach consensus.
The inclusion criteria were: (1) Randomized controlled trial; (2) Accessible as full paper; (3) Cardiac surgery patient(s); (4) Preoperative IMT; (5) Data on at least one of the following: Mechanical ventilation time, length of ICU stay, and/or duration of postoperative hospitalization; and (6) In English language.
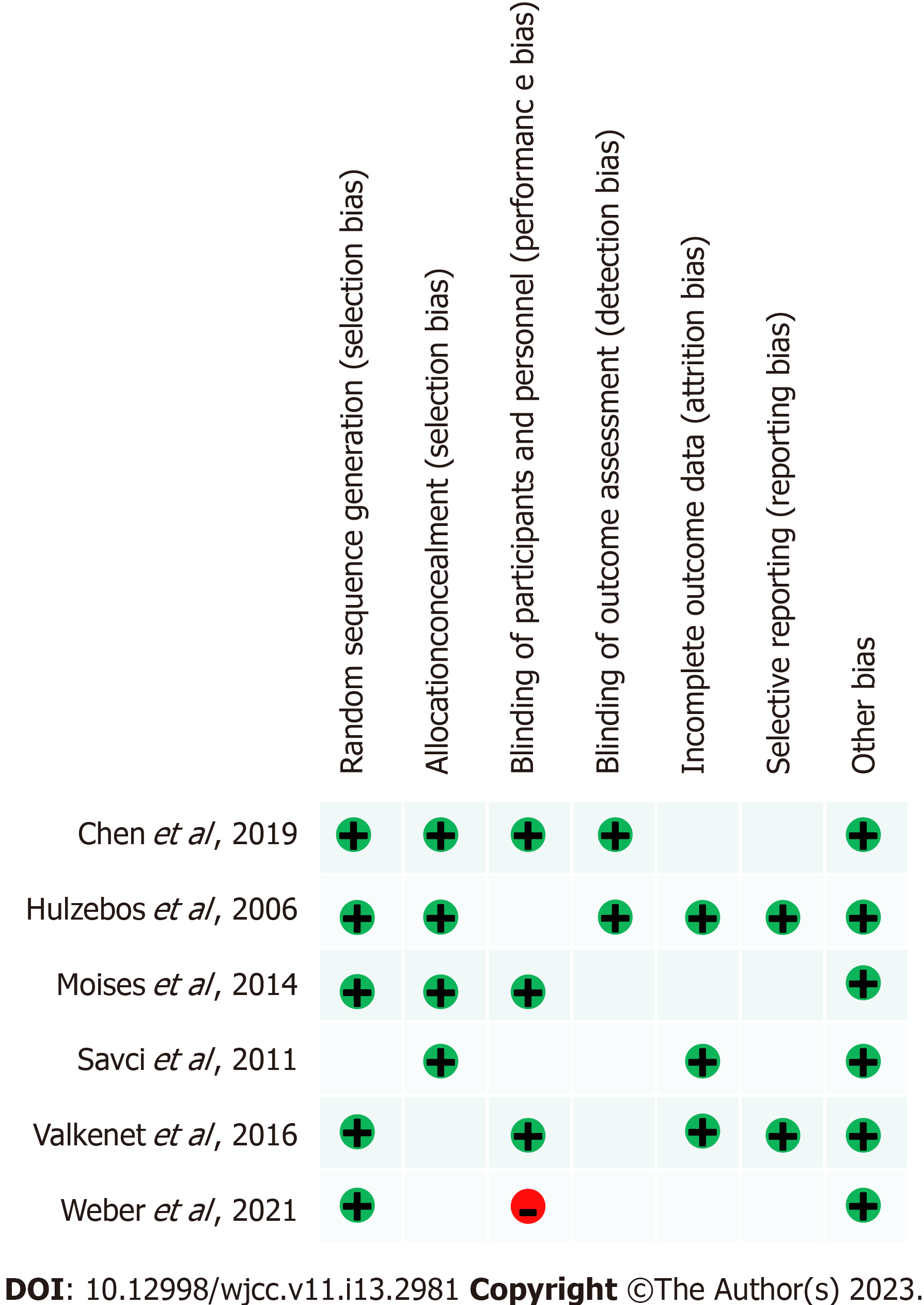
We used the Cochrane bias risk assessment tool in Review Manager (RevMan) computer program version 5.4, which is a reliable tool for the assessment of the risk of bias in randomized controlled trials in systematic reviews, to assess the bias risk of the included studies[16].
Data on author, year, journal, and country of the studies were obtained. Data on patient age, patient sex, type of surgery, intervention (including strength, frequency, time), and outcomes (mechanical ventilation time, length of ICU stay, and duration of postoperative hospitalization) were collected. The data were collected from tables or from the main text. For example, we collected the duration of postoperative hospitalization from the study by Hulzebos et al[12] and from the main text in the study by Valkenet et al[6]. However, some data were reported in ranges or interquartile ranges, such as those in the study of Hulzebos et al[12]. For these studies, we used the tool on the website (http://www.math.hkbu.edu.hk/~tongt/papers/median2mean.html) to estimate the sample mean and standard deviation from the sample size, median, range, and/or interquartile range. The data were independently extracted by two authors (Wang J and Wang YQ).
This meta-analysis aimed to evaluate the effect of IMT on mechanical ventilation time, length of ICU stay, and postoperative hospitalization in cardiac surgery patients. RevMan5.4 and Stata statistical software (Release 14; StataCorp LP, College Station, TX, United States) were used to perform the statistical analyses; of note, the results obtained from each program were the same. We chose the randomized effects model to analyze the data. The principal summary measurement used was the pooled mean difference (95%CI). We provided forest plots for every outcome.
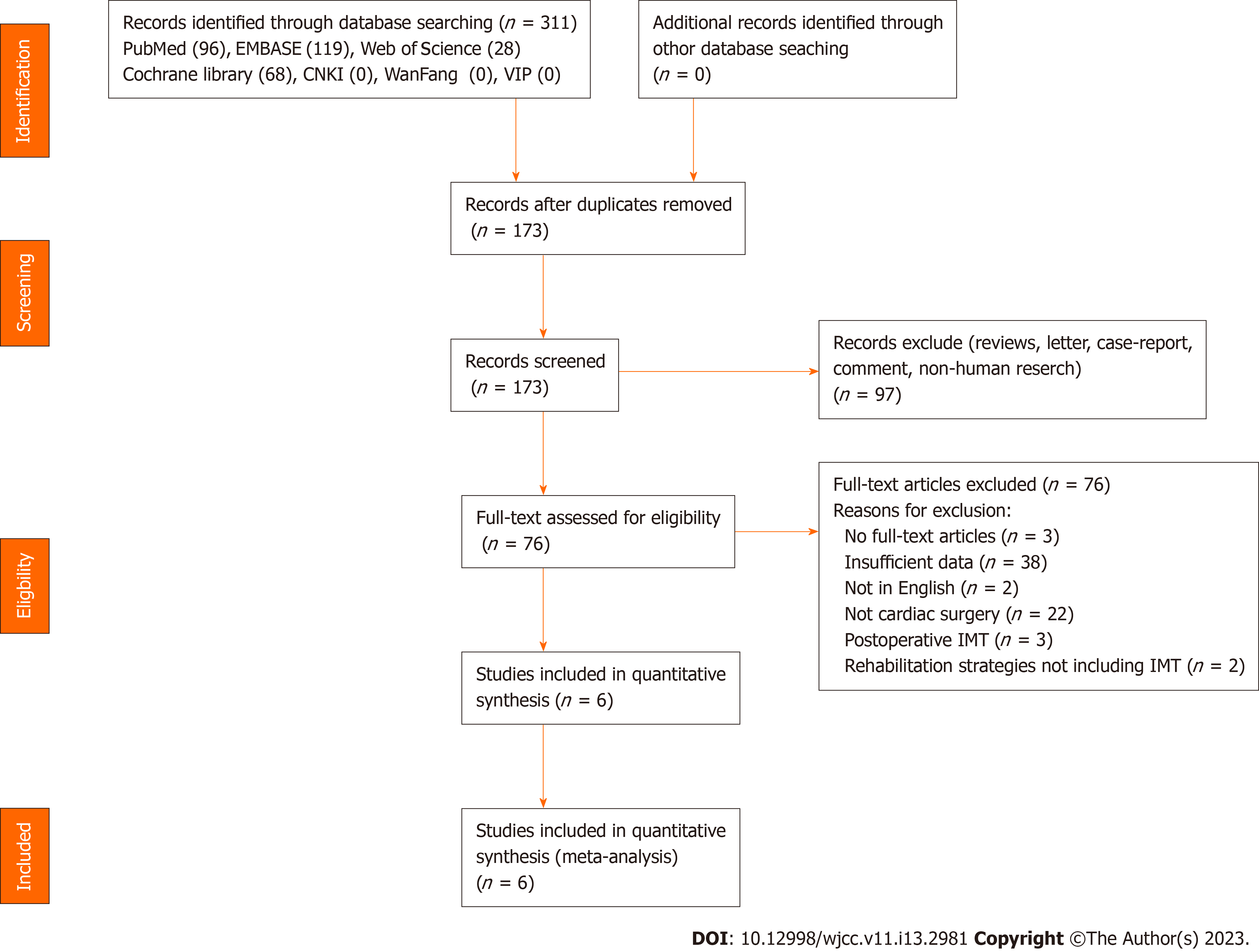
The flowchart of selected studies is presented in Figure 1. After the initial search, 311 citations were selected. After a review of abstracts and full-text articles, six trials[6,12,17-20] met the inclusion criteria. The risk of bias assessment of the included studies is presented in Figure 2.
The characteristics of the included trials are presented in Table 1. A total of 925 participants were involved in the six included studies. The sample sizes of the included trials ranged from 43 to 276, consisting primarily of male participants. The integrated age was 66.97 years, and the sex ratio in every study showed no significant effect. The intervention strategies and control methods were similar in each trial (Table 2). There was no significant difference in the type of operation. Most patients received CABG, and some of them received valve surgery [including transcatheter aortic valve replacement (TAVR)].
| No. | Ref. | Country | Intervention | Control | Intervention group | Control group | ||||
| Patients (male: female) | Mean age | Surgery type | Patients (male: female) | Mean age | Surgery type | |||||
| 1 | Hulzebos et al[12], 2006 | Netherlands | Threshold IMT + incentive spirometry + education in an active cycle of breathing techniques + forced expiration techniques | Usual care (i.e. instruction on deep breathing maneuvers, coughing, and early mobilization) + postoperative incentive spirometry, chest physical therapy, and mobilization scheme | 139 (108:31) | 66.5 (9.0) | CABG: 139 | 137 (107:30) | 67.3 (9.2) | CABG: 137 |
| 2 | Savci et al[17], 2011 | Turkey | Threshold IMT + mobilization + active exercises of upper and lower limbs + breathing exercises + coughing techniques | Usual care (mobilization, active exercises of upper and lower limbs, breathing exercises, and coughing techniques) | 22 (19:3) | 62.82 (8.69) | CABG: 22 | 21 (19:2) | 57.48 (11.48) | CABG: 21 |
| 3 | Moises et al[18], 2014 | Brazil | Threshold IMT + breathing exercises + postoperative physical therapy | Guidelines ward routine + postoperative physical therapy | 35 (23:12) | 58.90 ± 9.53 | CABG: 35 | 35 (29:6) | 61.40 ± 8.43 | CABG: 35 |
| 4 | Valken et al[6], 2016 | Netherlands | Threshold IMT + incentive spirometry + education (deep breathing maneuvers, coughing, and early mobilization) | Postoperative deep breathing maneuvers, coughing, and early mobilization incentive spirometry and chest physical therapy | 119 (93:26) | 66 (9.2) | CABG: 99; CABG + valve:20 | 116 (93:23) | 67.5 (9.7) | CABG: 87; CABG + valve: 29 |
| 5 | Chen et al[19], 2019 | China | Threshold IMT + usual care (education coughing, and early mobilization) and abdominal breathing training + postoperative chest physical therapy and mobilization scheme | Threshold IMT [the intensity was fixed at the minimum load of the device (9 cmH2O)] + usual care (education coughing and early mobilization) and abdominal breathing training + postoperative chest physical therapy and mobilization scheme | 98 (73:25) | 61.68 ± 8.12 | CABG: 69; valve: 18; CABG + valve: 11 | 99 (68:31) | 61.68 ± 7.73 | CABG: 70; valve: 21; CABG + valve: 8 |
| 6 | Weber et al[20], 2021 | Germany | Threshold IMT + walking below the threshold of subjective exhaustion + mobilization protocol and individual physiotherapy | Postoperative physiotherapy | 58 (27:31) | 82.2 ± 5.8 | TAVR: 58 | 50 (26:24) | 81.7 ± 5.0 | TAVR: 50 |
| No. | Ref. | Length | Frequency | Duration | Supervision | Intensity |
| 1 | Hulzebos et al[12], 2006 | ≥ 2 wk preoperatively | Once a day | 20 mins | 6 times a week without supervision and once a week with supervision | 30% of MIP. Resistance increases incrementally, based on the RPE scored on the Borg scale |
| 2 | Savci et al[17], 2011 | 5 d preoperatively + 5 d postoperatively | Twice a day | 30 mins | Each session was under the supervision of a physical therapist | 15% of MIP. The resistance was increased incrementally between 15% and 45% based on patient’s tolerance in the following days |
| 3 | Moises et al[18], 2014 | Preoperative (length not mentioned) | Once a day | 20 mins | Each session was under supervision | 40% of MIP. Intensity increase not mentioned |
| 4 | Valkenet et al[6], 2016 | Not mentioned | Once a day | 20 min | 6 times a week without supervision and once a week with supervision | 30% of MIP. Increased incrementally based on the RPE as scored on the Borg scale. If patients recorded an RPE score < 5 after a training session, they were instructed to increase the inspiratory load of the threshold device by 5% before the next training session. The threshold load was unchanged for RPE scores ≥ 5 |
| 5 | Chen et al[19], 2019 | 5 d preoperatively | Twice a day | 20 min | Each session was under the supervision of a physical therapist | 30% of MIP. Increased incrementally, based on the RPE scored on the Borg18 scale. If the RPE was less than 5, the resistance of the inspiratory threshold trainer was then increased incrementally by 5%. Training loads were adjusted to maintain 30% of the maximal inspiratory pressure every day |
| 6 | Weber et al[20], 2021 | ≥ 2 wk preoperatively | Once a day | 20 min | Not mentioned | Not mentioned |
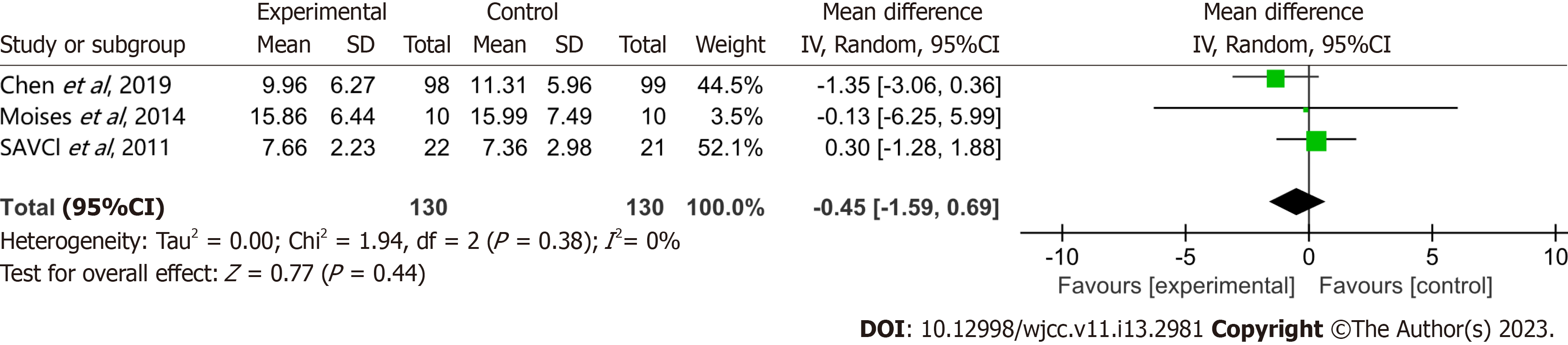
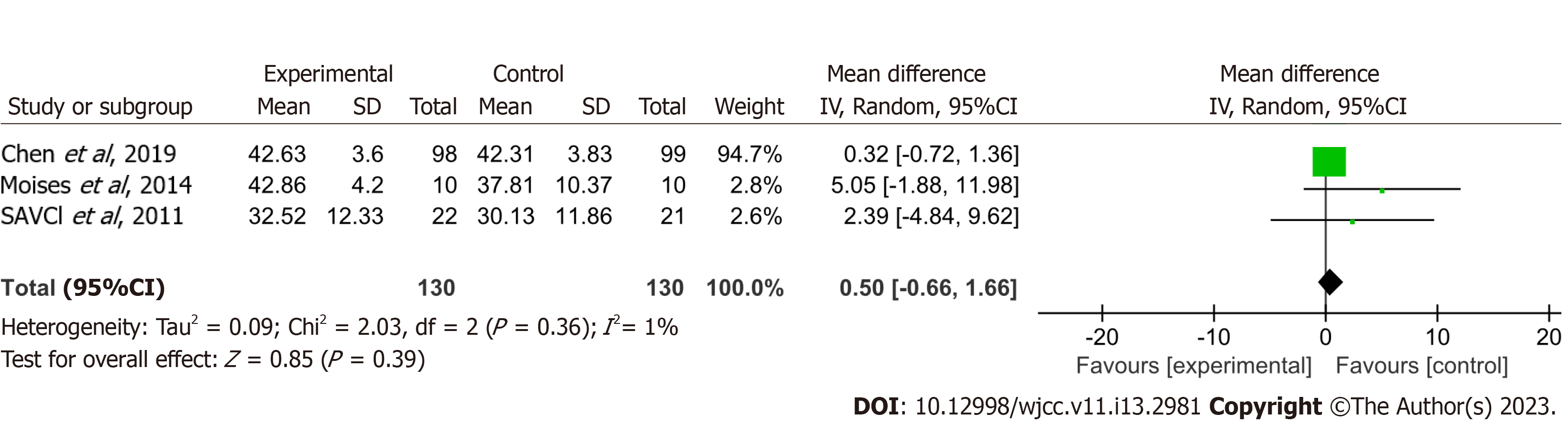
Mechanical ventilation time: Three studies[17-19] reported on the duration of mechanical ventilation. The pooled mean difference of -0.45 h (95%CI: -1.59-0.69) and low heterogeneity (I² =0) showed no statistically significant effect on mechanical ventilation time (Figure 3).
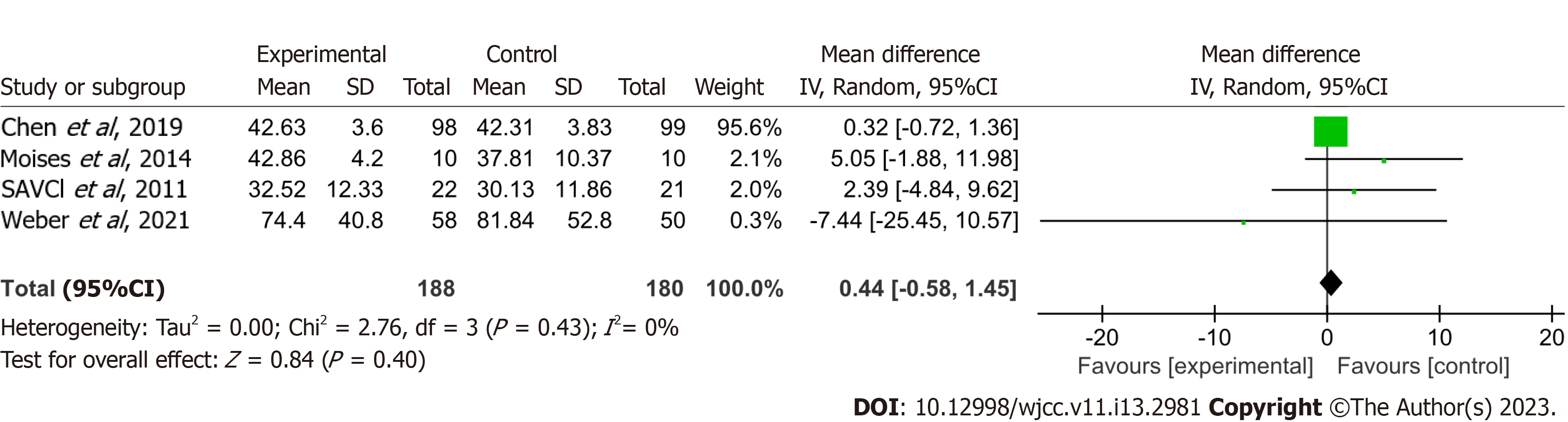
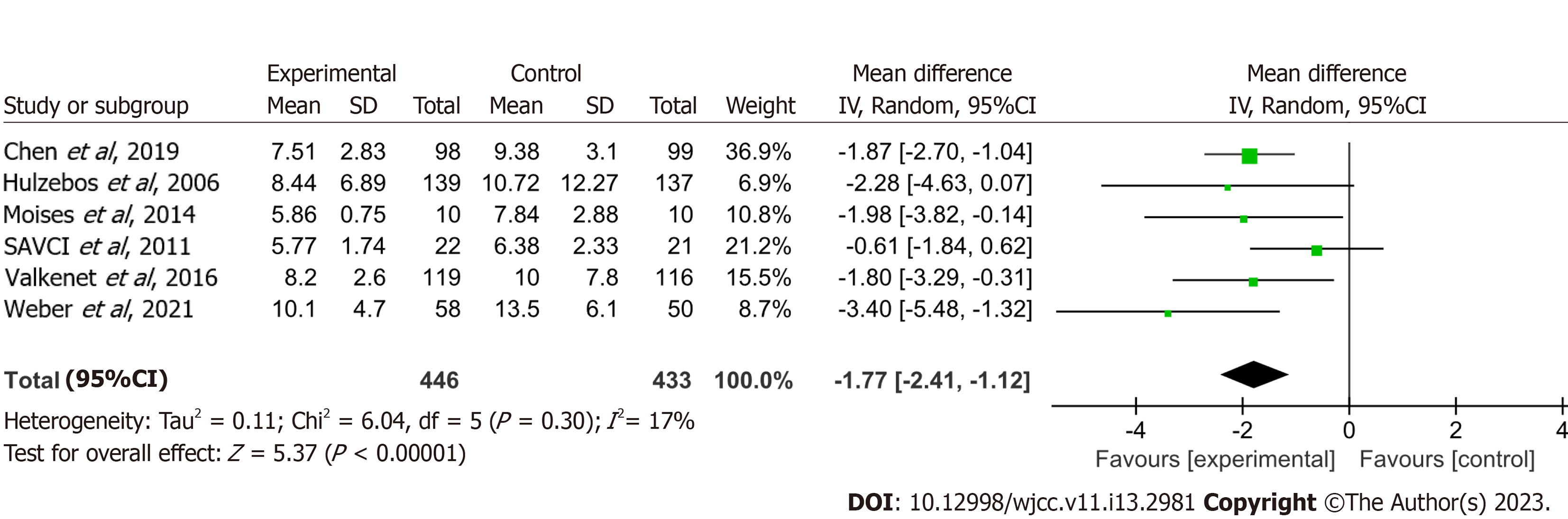
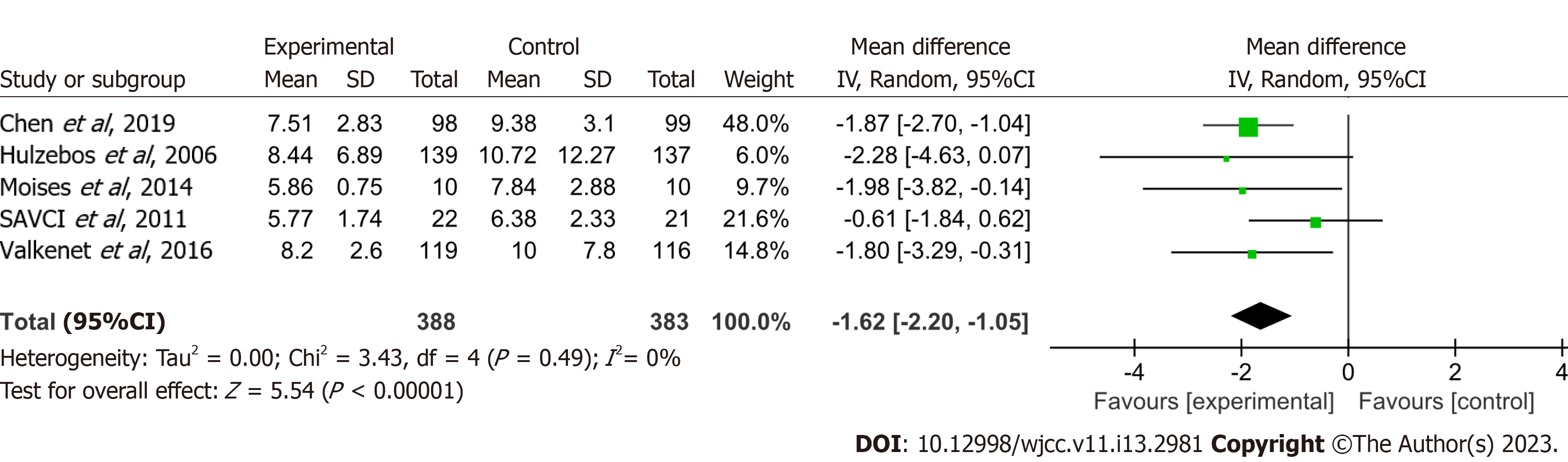
Length of ICU stay: Data from four studies[17-20] indicated a nonsignificant effect on the length of ICU stay with a pooled mean difference of 0.44 h (95%CI: -0.58-1.45) and low heterogeneity (I² = 0) (Figure 4). Excluding patients who received TAVR did not affect the results (Figure 5).
Duration of postoperative hospitalization: A meta-analysis of six trials[6,12,17-20] reporting the length of postoperative hospitalization yielded a pooled mean difference of -1.77 d [95%CI: -2.41-(-1.12)] for the intervention group vs the control group. This difference was statistically significant (Figure 6). Excluding patients who received TAVR did not affect the results (Figure 7).
This is the first systematic review and meta-analysis to explore the effect of preoperative IMT on mechanical ventilation time, length of ICU stay, and duration of postoperative hospitalization after cardiac surgery.
A summary of IMT in each study is presented in Table 2. All studies used threshold IMT. Patients received training greater than or equal to 2 wk, once a day, and lasting 20 min in the study of Hulzebos et al[12] and that of Weber et al[20]. Meanwhile, 5 d of preoperative training, twice a day, and lasting 30 min or 20 min was used in the study of Savci et al[17] and that of Chen et al[19], respectively. All patients were under supervision of a physical therapist in the studies. Studies by Hulzebos et al[12], Valkenet et al[6], and Chen et al[19] started the training with 30% of the maximum inspiratory pressure. Savci et al[17] started training with 15% of maximum inspiratory pressure, and Moises et al[18] with 40% of maximum inspiratory pressure. Weber et al[20] did not mention the starting intensity. We found no effect of preoperative IMT on mechanical ventilation time or length of ICU stay in cardiac surgery patients. Snowdon et al[21] concluded in their systematic review that preoperative intervention shortened the time to extubate from mechanical ventilation by a pooled mean difference of 0.14 d (95%CI: 0.01-0.26), which was different from our result. Interventions in their included studies were diversified and included anesthesia clinics or preadmission clinics, IMT, education booklets, etc. This likely explains the differences between our study and theirs. Because of the few studies reporting on these two outcomes, any conclusions should be made with caution.
Our study found that preoperative IMT did have a statistically significant effect on the duration of postoperative hospitalization. Katsura et al[13] reported that preoperative IMT could reduce the duration of hospitalization in patients receiving cardiac and major abdominal surgery. However, they included mostly abdominal surgery, which was different from our study. Snowdon et al[21] reported that preoperative intervention reduced hospitalization for elderly patients (> 63 years), with a pooled mean difference of -1.32 d [95%CI: -2.36-(-0.28)], similar to our study. Cook et al[22] reported that preoperative threshold IMT had the potential to reduce postoperative hospitalization and pulmonary complications after cardiac surgery, which was the same as our study. However, their study did not include the studies of Valkenet et al[6] and Weber et al[20]. Reducing the duration of hospitalization may reduce hospitalization expenses for patients. It has been hypothesized that preoperative IMT would increase the muscle strength of the patients and lead to less PPCs. Several studies (summarized in the Introduction section) have confirmed this hypothesis. We hypothesized that less postoperative complications and decreased hospitalization would in turn decrease hospitalization expenses. With the shorter postoperative stay in the hospital, patients may pay less for medicines, nursing, room and board, etc. Further cost analysis studies should be conducted to confirm our hypothesis.
With the popularity of the use of diagnosis-related groups, medical costs have caught the increasing attention of doctors and patients. In a health economic analysis of a randomized trial implemented by Boden et al[23] in Australia, participants were randomly divided into two groups (intervention group and control group). The intervention involved respiratory education and breathing exercise training with a physiotherapist. The control group received the information booklet only. They found that the mean estimate of net savings provided a return on investment of approximately 800% ($8 saved by the hospital for every $1 spent on physiotherapy to provide education and breathing exercise training to patients before surgery). This means that from the hospital’s perspective, preoperative physiotherapy was cost-effective. A meta-analysis by Takura et al[24] found that cardiac rehabilitation (CR) significantly improved cost/quality-adjusted life-years in the CR arm compared with the usual care arm [standardized mean difference: -0.31, 95%CI: -0.53-(-0.09)], which means that CR is cheaper and more effective than usual care. Preoperative IMT is one method of CR, and we can speculate that it could also decrease hospital expenses.
The most important limitation of our study was that few studies met our inclusion criteria. This led to a small sample size, which may influence the precision and accuracy of our study. At the same time, we did not obtain the patient level data from the studies. The second limitation was the heterogeneity. There were some differences among the interventions in these included studies. The length, frequency, duration, intensity, and supervision of IMT were different in each study. The details of each intervention are shown in Table 2. These differences could lead to heterogeneity of our results, and we cannot determine which training method is the best. In addition, the standards for extubating and hospital discharge are different in each country, hospital, and even doctor. These factors would lead to heterogeneity. The third limitation was that the type of operation in the included studies was mostly CABG, which did not include other cardiac surgeries (e.g., valve replacement and aortic dissection). Thus, we cannot claim the positive effect of preoperative IMT on the above outcomes in patients with all types of cardiac surgery.
The fourth limitation is the data obtained. Data about mechanical ventilation time were expressed as ranges or interquartile ranges in the studies by Hulzebos et al[12], Sobrinho et al[18], and Chen et al[19]. Data on the length of ICU stay were expressed as ranges or interquartile ranges in the studies of Sobrinho et al[18] and Chen et al[19]. Data on the duration of hospitalization were also expressed as ranges or interquartile ranges in the studies by Hulzebos et al[12] and Sobrinho et al[18]. We used the tool on the website (http://www.math.hkbu.edu.hk/~tongt/papers/median2mean.html) to estimate the sample mean and standard deviation from the sample size, median, range, and/or interquartile range for the above studies. This conversion decreases the precision and accuracy of data and can lead to statistical error. More high-quality studies are needed to explore the effect of preoperative IMT on mechanical ventilation time, length of ICU stay, and duration of postoperative hospitalization after cardiac surgery.
As we have found, preoperative IMT may decrease the length of postoperative hospitalization and potentially lessen expenses in the hospital to save money for patients. Thus, we recommend that preoperative IMT be implemented in hospitals or at home for patients who are waiting for cardiac surgery. However, we cannot determine the best length, frequency, duration, intensity, and supervision of IMT for patients. More studies are needed to find the best way to carry out IMT in hospitals or at home.
Preoperative IMT, as an important part of physical therapy, may decrease the duration of postoperative hospitalization and may decrease hospital costs for patients undergoing cardiac surgery. Meanwhile, IMT does not appear to lessen the time to extubate from mechanical ventilation or the duration of ICU stay.
The effect of preoperative inspiratory muscle training (IMT) on mechanical ventilation time, length of intensive care unit stay, and duration of postoperative hospitalization after cardiac surgery are unknown.
Decreasing pulmonary complications can lead to shorter hospital stays. This in turn could decrease costs for the patient and the hospital.
To evaluate whether preoperative IMT is effective in improving postoperative outcomes such as the mechanical ventilation time, length of intensive care unit stay, and duration of postoperative hospitalization in patients receiving cardiac surgery.
Several databases were searched to obtain eligible randomized controlled trials. Outcomes were mechanical ventilation time, length of intensive care unit stay, and duration of postoperative hospitalization.
The pooled mean difference of -0.45 h [(95%CI): -1.59-0.69] showed no statistically significant effect on mechanical ventilation time. The pooled mean difference 0.44 h (95%CI: -0.58-1.45) showed no statistically significant effect on length of intensive care unit stay. The pooled mean difference showed -1.77 d [95%CI: -2.41-(-1.12)] for postoperative hospitalization.
Preoperative IMT may decrease the duration of postoperative hospitalization for patients undergoing cardiac surgery.
More high-quality studies are needed to confirm our conclusion.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rehabilitation
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Awad AK, Egypt; Grigoriev E; Ong H, Malaysia S-Editor: Xing YX L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67-e492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4163] [Cited by in RCA: 4810] [Article Influence: 687.1] [Reference Citation Analysis (1)] |
| 2. | Dunbar SB, Khavjou OA, Bakas T, Hunt G, Kirch RA, Leib AR, Morrison RS, Poehler DC, Roger VL, Whitsel LP; American Heart Association. Projected Costs of Informal Caregiving for Cardiovascular Disease: 2015 to 2035: A Policy Statement From the American Heart Association. Circulation. 2018;137:e558-e577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 165] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 3. | Bloom DE, Cafiero ET, Mcgovern ME. The Economic Impact of Non-communicable Disease in China and India: Estimates, Projections, and Comparisons. IZA Discussion Papers. 2013;. [DOI] [Full Text] |
| 4. | Apostolakis E, Filos KS, Koletsis E, Dougenis D. Lung dysfunction following cardiopulmonary bypass. J Card Surg. 2010;25:47-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 203] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Jensen L, Yang L. Risk factors for postoperative pulmonary complications in coronary artery bypass graft surgery patients. Eur J Cardiovasc Nurs. 2007;6:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Valkenet K, Trappenburg JCA, Hulzebos EH, van Meeteren NLU, Backx FJG. Effects of a pre-operative home-based inspiratory muscle training programme on perceived health-related quality of life in patients undergoing coronary artery bypass graft surgery. Physiotherapy. 2017;103:276-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, Hauri D, Graf R, Clavien PA. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254:907-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 385] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 8. | Thompson DA, Makary MA, Dorman T, Pronovost PJ. Clinical and economic outcomes of hospital acquired pneumonia in intra-abdominal surgery patients. Ann Surg. 2006;243:547-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 119] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Hemmila MR, Jakubus JL, Maggio PM, Wahl WL, Dimick JB, Campbell DA Jr, Taheri PA. Real money: complications and hospital costs in trauma patients. Surgery. 2008;144:307-316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 670] [Cited by in RCA: 694] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 11. | Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Hulzebos EH, Helders PJ, Favié NJ, De Bie RA, Brutel de la Riviere A, Van Meeteren NL. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA. 2006;296:1851-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 421] [Article Influence: 22.2] [Reference Citation Analysis (1)] |
| 13. | Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa TA. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst Rev. 2015;2015:CD010356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 14. | Fagevik Olsén M, Hahn I, Nordgren S, Lönroth H, Lundholm K. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg. 1997;84:1535-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Boden I, Skinner EH, Browning L, Reeve J, Anderson L, Hill C, Robertson IK, Story D, Denehy L. Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ. 2018;360:j5916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 179] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 16. | Higgins JPT TJ, Chandler J, Cumpston M. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). [RCA] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 2926] [Article Influence: 487.7] [Reference Citation Analysis (0)] |
| 17. | Savci S, Degirmenci B, Saglam M, Arikan H, Inal-Ince D, Turan HN, Demircin M. Short-term effects of inspiratory muscle training in coronary artery bypass graft surgery: a randomized controlled trial. Scand Cardiovasc J. 2011;45:286-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Sobrinho MT, Guirado GN, Silva MA. Preoperative therapy restores ventilatory parameters and reduces length of stay in patients undergoing myocardial revascularization. Rev Bras Cir Cardiovasc. 2014;29:221-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Chen X, Hou L, Zhang Y, Liu X, Shao B, Yuan B, Li J, Li M, Cheng H, Teng L, Guo M, Wang Z, Chen T, Liu J, Liu Y, Liu Z, Guo Q. The effects of five days of intensive preoperative inspiratory muscle training on postoperative complications and outcome in patients having cardiac surgery: a randomized controlled trial. Clin Rehabil. 2019;33:913-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (2)] |
| 20. | Weber M, Klein U, Weigert A, Schiller W, Bayley-Ezziddin V, Wirtz DC, Welz A, Werner N, Grube E, Nickenig G, Sinning JM, Ghanem A. Use of Pre- and Intensified Postprocedural Physiotherapy in Patients with Symptomatic Aortic Stenosis Undergoing Transcatheter Aortic Valve Replacement Study (the 4P-TAVR Study). J Interv Cardiol. 2021;2021:8894223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Snowdon D, Haines TP, Skinner EH. Preoperative intervention reduces postoperative pulmonary complications but not length of stay in cardiac surgical patients: a systematic review. J Physiother. 2014;60:66-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 22. | Cook A, Smith L, Anderson C, Ewing N, Gammack A, Pecover M, Sime N, Galley HF. The effect of Preoperative threshold inspiratory muscle training in adults undergoing cardiac surgery on postoperative hospital stay: a systematic review. Physiother Theory Pract. 2022;1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 23. | Boden I, Robertson IK, Neil A, Reeve J, Palmer AJ, Skinner EH, Browning L, Anderson L, Hill C, Story D, Denehy L. Preoperative physiotherapy is cost-effective for preventing pulmonary complications after major abdominal surgery: a health economic analysis of a multicentre randomised trial. J Physiother. 2020;66:180-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Takura T, Ebata-Kogure N, Goto Y, Kohzuki M, Nagayama M, Oikawa K, Koyama T, Itoh H. Cost-Effectiveness of Cardiac Rehabilitation in Patients with Coronary Artery Disease: A Meta-Analysis. Cardiol Res Pract. 2019;2019:1840894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |