Published online Dec 26, 2022. doi: 10.12998/wjcc.v10.i36.13179
Peer-review started: September 12, 2022
First decision: October 28, 2022
Revised: November 5, 2022
Accepted: November 28, 2022
Article in press: November 28, 2022
Published online: December 26, 2022
Processing time: 105 Days and 5.4 Hours
Lumbar degenerative disc disease (DDD) in the elderly population remains a global health problem, especially in patients with osteoporosis. Osteoporosis in the elderly can cause failure of internal fixation. Cortical bone trajectory (CBT) is an effective, safe and minimally invasive technique for the treatment of lumbar DDD in patients with osteoporosis. In this review, we analyzed the anatomy, biomechanics, and advantages of the CBT technique in lumbar DDD and revision surgery. Additionally, the clinical trials and case reports, indications, advance
Core Tip: Some reviews in the literature have provided information that contributes to the anatomy, surgical technique, and biomechanics of cortical bone trajectory screws. However, the aim of this review is to report the recent clinical trials and case reports, indications, advancements and limitations of this technique. We concluded that the cortical bone trajectory technique can be a practical, effective and safe alternative to traditional pedicle screw fixation, especially in degenerative disc diseases patients with osteoporosis.
- Citation: Guo S, Zhu K, Yan MJ, Li XH, Tan J. Cortical bone trajectory screws in the treatment of lumbar degenerative disc disease in patients with osteoporosis. World J Clin Cases 2022; 10(36): 13179-13188
- URL: https://www.wjgnet.com/2307-8960/full/v10/i36/13179.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i36.13179
The incidence of lumbar degenerative disc diseases (DDDs) in the elderly has increased in recent years. The anatomy and curvature of the spine changes significantly with age. Hegazy and Hegazy[1] confirmed the change in morphology and dimensions of lumbar lordosis in aging adults, which suggested that the anatomy and curvature need to be given more attention during surgery[1]. Additionally, osteoporosis is quite common among elderly individuals. Therefore, another key treatment strategy for lumbar DDD in the elderly is the management of osteoporosis. Osteoporosis in the elderly can cause the loosening of internal fixation. A study showed that the rate of pedicle screw loosening in patients with osteoporosis was 12.8% to 25%. Additionally, the risks of proximal and distal junctional kyphosis also increase accordingly[2]. Therefore, the stability of internal fixation in osteoporosis patients should be enhanced during the operation by employing expansive pedicle screws, bone cement screws, or cortical bone trajectory (CBT) screws. Although expansive pedicle screws can increase the intensity of internal fixation, there are clear shortcomings, such as complicated placement, a high screw breakage rate, and limited clinical application. Bone cement screws have also been gradually applied in the treatment of DDD patients with osteoporosis. Zhang et al[3] showed that the loosening rate of bone cement screws is less than 4.3%, but intraoperative perfusion of bone cement increased the operation time and radiation exposure. Moreover, bone cement may leak into the spinal canal and blood vessels, leading to serious complications, such as neurological dysfunction and pulmonary embolism[3]. The CBT technique was proposed by Santoni et al[4] in 2009. Compared with the traditional technique, the CBT technique increases the contact surface between screws and cortical bone, and all screws used in the CBT technique are surrounded by the cortical bone. Therefore, this technique is more suitable for the treatment of lumbar DDD patients with osteoporosis[4]. Furthermore, in 2014, Mizuno et al[5] proposed the combination of this technique with lumbar posterior midline fixation and fusion in midline lumbar fusion (MIDLF) surgery. The CBT technique in MIDLF surgery has been widely used in lumbar DDD, adjacent vertebral diseases and postoperative revision due to its low invasiveness and high safety advantages[6].
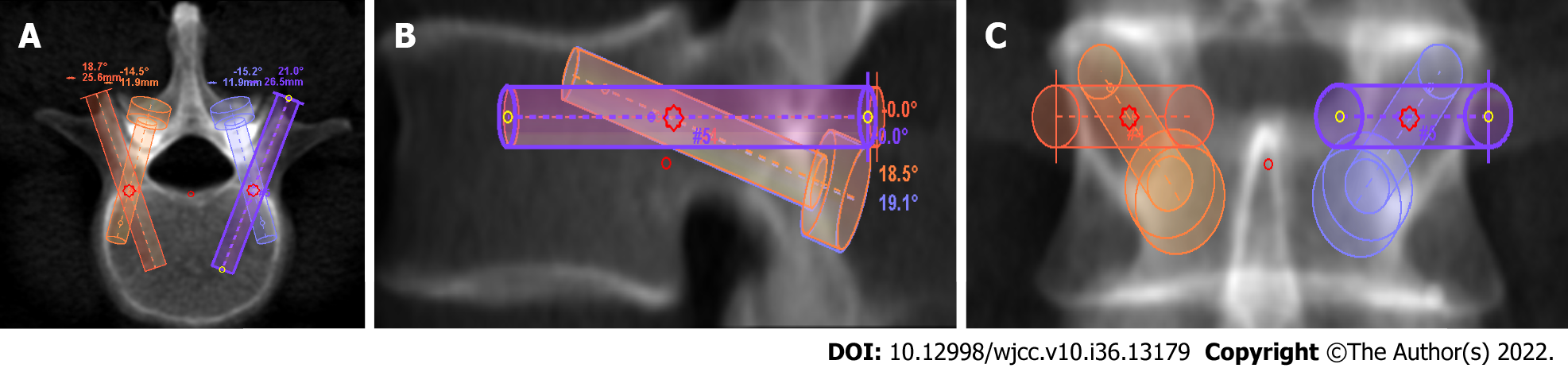
The CBT technique is performed at the intersection of the lateral isthmus of the pedicle and the lower edge of the transverse process. The entry point is at 5 o'clock on the left pedicle and 7 o'clock on the right pedicle. The ideal trajectory of placement is along the lower edge of the pedicle with a cranial incline of 25° to 30° and an external incline of 10° to ensure the maximum contact between the screw and cortical bone (Figure 1). Although the shape of the lumbar pedicles varies in different segments, the trajectory of placement remains unchanged. Four cortical bone surfaces are contacted using the standard CBT technique in the lumbar spine, namely, the isthmus, medial wall, lateral wall of the pedicle and anterior lateral wall of the vertebral body[7]. However, CBT screws are usually shorter and thinner than conventional pedicle screws. Matsukawa et al[8] measured the diameter and length of CBT in the adult lumbar spine using computed tomography (CT) and concluded that the diameter of the trajectory ranged from 6.2 ± 1.1 mm (L1) to 8.4 ± 1.4 mm (L5). The length of the trajectory at each vertebra was 36.8 ± 3.2 mm (L1), 38.2 ± 3.0 mm (L2), 39.3 ± 3.3 mm (L3), 39.8 ± 3.5 mm (L4), and 38.3 ± 3.9 mm (L5)[8]. Therefore, the biomechanical stability of the CBT technique has become a popular topic in research. Kojima et al[7] found that the bone CT value around CBT screws was four times higher than that around traditional pedicle screws, which indicated that the bone-screw interface strength of the CBT technique was greater[9]. Li et al[10] also showed that the CBT technique had better fatigue resistance stability, especially in osteoporotic vertebrae[10]. However, the CBT technique is less effective against lateral bending and rotation than the conventional pedicle screw technique, which may result in a lower interbody fusion rate using CBT screw fixation than that using traditional pedicle screw fixation[11,12]. Therefore, a transverse connection could be used to improve the anti-lateral bending and anti-rotational stability during CBT screw placement.
As the CBT technique is applied closer to the posterior midline than the traditional pedicle screw technique, vertebral muscles and adjacent segment joints are less harassed; therefore, the CBT technique has many advantages, including less blood loss and fatty infiltration, a shorter hospital stay and a lower incidence of adjacent segment degeneration (ASD). Additionally, the trajectory of the CBT technique is away from important nerve and vascular tissues, which further decreases the risk of injury. The CBT technique combined with MIDLF surgery is minimally invasive and safer and has been widely used in the treatment of lumbar diseases. Studies have shown that the CBT technique combined with MIDLF in the treatment of DDD patients with osteoporosis can achieve similar clinical decompression effects to those of the traditional pedicle screw technique combined with transforaminal lumbar interbody fusion (TLIF) technology[13]. Mizuno et al[5] proposed that CBT screws combined with MIDLF in the treatment of patients with single-level lumbar spondylolisthesis achieved good clinical outcomes. Lumbar decompression, fixation and fusion can be completed by the CBT technique at the same time, which is in line with the concept of minimally invasive surgery. Takenaka et al[14] compared the CBT technique and the traditional pedicle screw technique combined with lumbar posterior interbody fusion (PLIF) in the treatment of lumbar DDD. They concluded that the operation time, intraoperative blood loss, postoperative drainage volume, bed rest time and postoperative hospital stay time in the CBT technique group were significantly lower than those in the traditional pedicle screw technique group. CBT screws combined with PLIF surgery can achieve a more minimally invasive treatment effect for DDD patients with osteoporosis[14]. Kasukawa et al[15] compared the clinical efficacy of CBT and conventional pedicle screw internal fixation in TLIF. They concluded that the CBT technique can achieve better clinical results, smaller incisions and faster postoperative recovery than the conventional pedicle screw technique.
Recently, the incidence of failed back surgery syndrome and ASD has increased with the extensive application of spinal internal fixation, leading to a high proportion of lumbar revision surgeries[16]. In revision surgery, the exposure risk of the nerve structure and blood vessels is significantly increased due to hypertrophic scar tissue and unclear spinal anatomy. Another advantage of the CBT technique is the reduction in exposure risk in revision surgery. During revision surgery, the internal fixation of the original operation usually needs to be replaced when the adjacent segment is decompressed and fixed. However, the replacement of internal fixation can not only increase the operation time and surgery risk but also result in more blood loss. Therefore, decompression, fixation and fusion on the adjacent segments without removing the internal fixation of the original surgery has become a key technique for the treatment of ASD. The CBT technique, which has a unique entry point and trajectory, can complete screw placement, decompression and fusion of adjacent segments through a small incision while retaining the original internal fixation, thereby avoiding extensive dissection and reducing the operation time and risk. In addition, the CBT technique can be used to place two groups of screws in the same vertebral body[17]. A study by Takata et al[18] showed that the CBT technique combined with MIDLF in lumbar revision surgery has the advantages of less soft tissue injury, fewer postoperative complications and better stability of internal fixation compared with traditional revision surgery[18].
We performed an online database search on PubMed using the terms “cortical bone trajectory”, “clinical trials”, and “case reports”. Only papers published in English until June 10, 2022 were reviewed. Finally, seventeen articles were identified and included in Table 1[3,9,18-32]. There were thirteen retrospective cohort studies, two retrospective cohort comparative studies, and two prospective cohort studies. Most studies in this table indicated that the CBT technique offered good clinical outcomes with shorter incision length.
| Ref. | Country/region | Study design | Number of cases | Indication | Technique | Revision surgery | Accuracy | Outcomes | Fluoroscopy X-ray dose | Complications | Incision length |
| Crawford CH 3rd et al[19], 2019 | United States | RCCS | 56 | Spondylolisthesis and foraminal stenosis | Navigated CBT-pedicle screw (29) traditional open TLIF (27) | NA | NA | Lower ODI and less back pain in navigated CBT group | NA | Late reoperations for adjacent segment disease were significantly greater in the traditional open TLIF group | NA |
| Hsu et al[20], 2020 | Taiwan | ROS | 12 | Thoracolumbar osteoporotic compression fracture | Short-segment CBT instrumentation with vertebroplasty | None | NA | The average blood loss and VAS scores were significantly improved; the average sagittal Cobb angle significantly increased from 15.4° preoperatively to 18.8° postoperatively | NA | None | NA |
| Noh et al[21], 2021 | South Korea | ROS | 200 | Spinal stenosis, spondylolisthesis, degenerative disc diseases | Open surgery with CBT screw instrumentation | 5 cases with adjacent segment disease | NA | Symptom and quality of life significantly improved after surgery | NA | 5 cases with ASD, 1 case with screw loosening, 8 cases with dura tear | NA |
| Takata et al[18], 2014 | Japan | ROS | 6 | Degenerative spondylolisthesis | Hybrid CBT-pedicle screw | NA | NA | Mean operative time 175.8 min. Blood loss 70–200 mL | NA | One had a mild infection after surgery | Around5-6 cm, shorter than that of the conventional PS |
| Zheng et al[22], 2022 | China | RCCS | 48 | Traumatic thoracolumbar fractures without neurologic defects (type A) | Percutaneous CBT (PCBT 24) OPPS 24 | No | NA | VAS scores improved after operation. Blood loss and hospital stay were better in PCBT group | NA | No complications in PCBT group, four cases with complications in OPPS group | PCBT group was better than OPPS group |
| Petrone et al[23], 2020 | Italy | ROS | 238 | Degenerative lumbosacral disease | First group: 43 cases without CT planningSecond group: 158 cases with CT planning. Third group: 37 cases with 3D printed guide | NA | Screws entirely within the cortex of the pedicle were 78.9%, 90.5% and 93.9% in the three groups | All patients’ symptoms improved after surgery mean operation time was 187, 142 and 124 min in the three subgroups | NA | The total amount of complications were 4.2% (16.3%, 3.8%, 0.0% respectively) | NA |
| Dayani et al[24], 2019 | United States | POS | 22 | Lumbar degenerative disease and spinal instability | Early experience (first 11 patients) late experience (last 11 patients) | NA | Early experience phase: 66.7% (4/6) of medial pedicle breaches; 100% of lateral vertebral body breach | Late phase: greater efficiency | NA | Incidence of complications decreased in the late phase | NA |
| Marengo et al[25], 2018 | GER | ROS | 101 | Degenerative lumbo-sacral disease | CT planning | 32 patients (31.6%) | NA | Symptom and quality of life improved after surgery; mean procedural time 187 min; mean hospital stay 3.47 days; mean blood loss 383 mL | 1.60 mg cm2 | 4 screws misplaced; 1 wound infection; 1 pseudmeningocele | NA |
| Chen et al[26], 2018 | Taiwan | ROS | 6 | Lumbar adjacent segment disease | C-arm guidance | Revision surgery:6 cases | NA | Symptom and quality of life improved after surgery | NA | No post-operative complication | NA |
| Orita et al[27], 2016 | Japan | POS | 40 | Degenerative spondylolisthesis or lateral lumbar disc herniation; stenosis | Percutaneous CBT (pCBT 20); traditional PPS arms (20); C-arm fluoroscope guidance | NA | NA | Clinical outcome regarding LBP and lower limb pain improved with no significant difference between the two groups | Shorter duration of fluoroscopy in PCBT group | No complications | Shorter incision length in PCBT group |
| Snyder et al[28], 2016 | United States | ROS | 79 | Degenerative lumbosacral disease | Navigation guide | Revision surgery: 20 cases (25.3%) | NA | Mean length of stay was 3.5 days; mean operative blood loss was 306.3 mL | NA | 9 complications (8.9%) including hardware failure, pseudarthrosis, DVT, pulmonary embolism, epidural hematoma, wound infection. No complications by misplaced screws | NA |
| Mai et al[9], 2016 | United States | ROS | 22 | Lumbar spine disease | NA | NA | NA | NA | NA | Screw loosening: 2 intra-operative dural tear: 1. Both a pedicle fracture and screw loosening: 1 | NA |
| Ninomiya et al[29], 2016 | Japan | ROS | 21 | Degenerative spondylolisthesis | Conventional PS (10) CBT (11). C-arm fluoroscope guidance | NA | NA | Symptom and quality of life improved after surgeryboth techniques showed good slip reduction | NA | NA | NA |
| Elmekaty et al[30], 2018 | Sweden | ROS | 59 | Lumbar spondylolisthesis | MIS-PLF: 22; MIS-TLIF: 15; MIDLF: 22 | NA | NA | MIDLF: shorter operation time, less bleeding amount, lower values of CRP and CK than the other two techniques; symptom and quality of life of all the patients improved after surgery | NA | Screw loosening. MIS-PLF: 10%. MIS-TLIF: 7.14%. MIDLF: 4.76% | MIDLF with a small, single posterior midline incision (3.5 cm) |
| Zhang et al[3], 2021 | China | ROS | 52 | Lumbar tuberculosis | CBT group: 27. PS group: 25 | NA | NA | All patients achieved good clinical outcomes; incision pain in CBT group is better than PS group on the 1st day and 3rd day after surgery | NA | All patients have no intraoperative complications | NA |
| Wochna et al[31], 2018 | United States | ROS | 71 | Traumatic thoracolumbar fractures | ORIF PS: 39; MIS PS: 20; CBT: 12 | NA | NA | EBL was 337.50 mL for CBT, 184.33 mL for MIS, and 503.33 mL for ORIF; LOS was 4.06 days fewer for CBT compared to ORIF | NA | 1 case of construct failure; 1 case of incisional site infection in the PS group; but none were found in the CBT group | NA |
| Laratta et al[32], 2019 | United States | ROS | 134 | Degenerative spondylolisthesis mechanical collapse with foraminal stenosisdegenerative scoliosis adjacent segment disease | Navigation with intraoperative CT | Revision surgery: 26.9% | Accuracy rate was 98.3%. The accuracy within 1 mm of error was 99.2% | NA | NA | Lateral breaches: 3 (0.5%); medial breaches: 7 (1.1%) | NA |
CBT screw fixation not only provides more stable internal fixation strength for patients with osteoporosis but can also be combined with a variety of minimally invasive procedures to reduce the risk of injury and intraoperative exposure. Especially for patients with obesity or diabetes, the application of CBT screw fixation can significantly reduce the incidence of postoperative complications. The following indications for CBT screw fixation were determined by comprehensive analysis of the anatomical characteristics, biomechanical characteristics and technical advantages of the CBT technique: (1) Lumbar disc degenerative diseases, especially combined with osteoporosis; (2) Obesity and high iliac crest; (3) ASD after traditional pedicle screw placement; (4) Salvage screw placement after failure of traditional pedicle screws; (5) Diseases mainly characterized by the destruction of the anterior and middle columns of the vertebral body, such as lumbar tuberculosis and intervertebral space infection; (6) Thoracolumbar fracture; and (7) Lumbar scoliosis correction and internal fixation with osteoporosis. However, CBT screw fixation is not suitable for bone destructive diseases with the absence of isthmus or spinal deformity characterized by rotation.
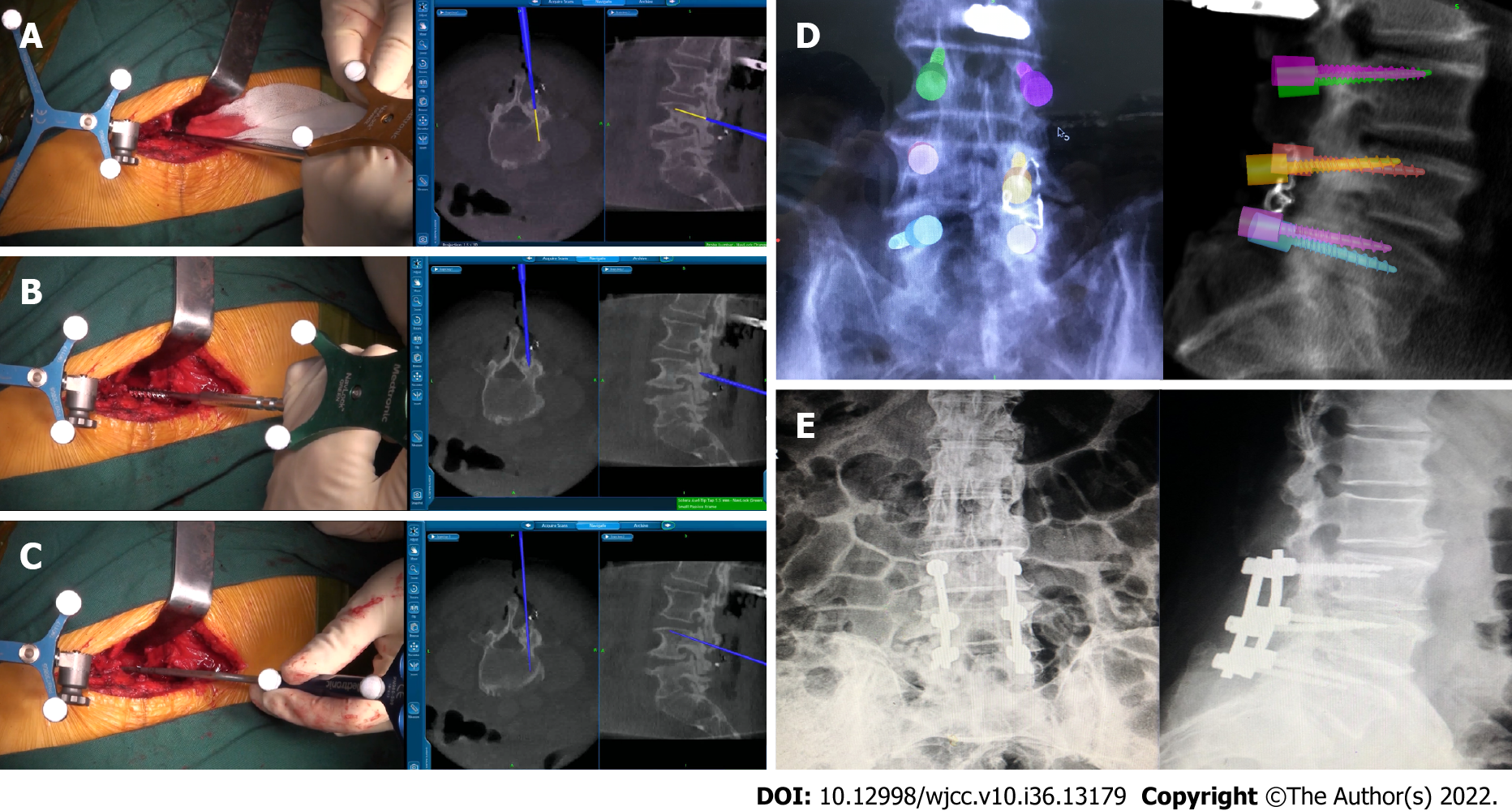
Although CBT screws are widely used in a variety of lumbar diseases, placing CBT screws is extremely demanding. Freehand techniques have a risk of exiting nerve root injury and lead to a high failure rate during screw placement. Because the anatomical entry point is hard and not evident, the placing instruments can easily slip and cause pedicle, isthmus and upper endplate injuries during surgery. The failure rate of the freehand placement technique is as high as 33.1%[33]. Second, the entry point and trajectory of the CBT technique are different from those of traditional screw placement. Surgeons cannot rely on tactile feedback to place screws, which will inevitably increase the amount of intraoperative X-ray exposure and operation time. To reduce complications and ensure screw placement safety and accuracy, researchers have begun to use 3D-printed guide plates, navigation, and robots to assist in CBT screw placement. The 3D-printed guide plate, navigation and robot-assisted placement of CBT screws successfully compensated for the disadvantages of freehand screw placement and improved the safety and accuracy of CBT screw placement for internal fixation. Marengo et al[34] used a 3D-printed guide plate to assist in the placement of CBT screws, and they concluded that 85.2% of the screw entry points were within 2 mm of the planned entry points. Buza et al[35] compared the surgical effects of MIDLF assisted by the Mazor spinal robot and free-hand MIDLF and found that the Mazor spinal robot improved the accuracy of CBT screw placement with less intraoperative blood loss and shorter hospital stays and operation times. Le et al[36] compared the free-hand CBT screw technique with the CBT screw technique assisted by the Tianji orthopedic surgery robot and found that the robot-assisted CBT screw technique reduced the incidence of adjacent segment facet joint injury. The accuracy of robot-assisted CBT screw placement was higher than that of the freehand group, and the acceptable screw placement in the robot-assisted group was 98.3%, which was significantly higher than that in the freehand group (84.5%). Additionally, the blood loss, operation time and radiation exposure dose of the robot-assisted group were significantly lower than those of the freehand group. Three-dimensional navigation technology is used to assist and monitor the trajectory of CBT screws in real time, which maximizes the contact between screws and the cortical bone interface and reduces the risks of screw placement (Figure 2). Navigation-assisted CBT screw placement can reduce the incidence of superior facet joint injury[17]. Khan et al[37] compared the accuracy of CBT screw internal fixation in the treatment of lumbar DDD with osteoporosis using a 3D guide plate, navigation and freehand[37], and they concluded that the accuracy rate of screw placement in the 3D-printed guide group and the navigation group was 100%. The accuracy rate of screw placement in the freehand group was only 87.5%. Although the application of spinal robotic and three-dimensional navigation technology has significantly improved the accuracy of CBT screw placement, there are still some shortcomings in this technology. Systematic errors are related to the patient's position change, image registration errors and screw skidding. Additionally, the angle and position of the screw may be shifted during implantation due to differences in surgeons' experience and learning curves. Therefore, it is necessary to probe the trajectory and perform intraoperative fluoroscopy to confirm the accuracy and safety of CBT screws as in the conventional pedicle screw placement technique.
Although CBT screws combined with the MIDLF technique have been widely used in clinical practice, relevant studies are still lacking. (1) The screws used in various biomechanical studies have different specifications, so the results have not been uniformly concluded; (2) Most clinical studies are retrospective case studies with small sample sizes and short follow-up times. Therefore, long-term, large-sample and prospective studies are still needed to further reveal the long-term complications and long-term fusion rate; (3) CBT screws are mostly used in patients with short-segment lumbar DDD. For patients with long segments, lumbar DDD and thoracic disease are rarely reported and need further research; and (4) To date, research on the corresponding relationship between the degree of osteoporosis and the choice of internal fixation methods is limited. The focus of further studies should be the correlation between the degree of osteoporosis and various internal fixation enhancement techniques to ensure the best selection of the internal fixation under different degrees of osteoporosis.
CBT can be used as a practical and effective alternative to traditional pedicle screw fixation. It has obvious advantages in the treatment of lumbar DDD, especially in patients with osteoporosis under strict mastery of the indications and contraindications.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Grawish ME, Egypt; Hegazy AA, Egypt S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Hegazy AA, Hegazy RA. Midsagittal anatomy of lumbar lordosis in adult egyptians: MRI study. Anat Res Int. 2014;2014:370852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Hirsch BP, Unnanuntana A, Cunningham ME, Lane JM. The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J. 2013;13:190-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Zhang J, Wang G, Zhang N. A meta-analysis of complications associated with the use of cement-augmented pedicle screws in osteoporosis of spine. Orthop Traumatol Surg Res. 2021;107:102791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA, Womack WJ, Puttlitz CM. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9:366-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 400] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 5. | Mizuno M, Kuraishi K, Umeda Y, Sano T, Tsuji M, Suzuki H. Midline lumbar fusion with cortical bone trajectory screw. Neurol Med Chir (Tokyo). 2014;54:716-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Momin AA, Steinmetz MP. Evolution of Minimally Invasive Lumbar Spine Surgery. World Neurosurg. 2020;140:622-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 7. | Kojima K, Asamoto S, Kobayashi Y, Ishikawa M, Fukui Y. Cortical bone trajectory and traditional trajectory--a radiological evaluation of screw-bone contact. Acta Neurochir (Wien). 2015;157:1173-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Matsukawa K, Yato Y, Nemoto O, Imabayashi H, Asazuma T, Nemoto K. Morphometric measurement of cortical bone trajectory for lumbar pedicle screw insertion using computed tomography. J Spinal Disord Tech. 2013;26:E248-E253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 9. | Mai HT, Mitchell SM, Hashmi SZ, Jenkins TJ, Patel AA, Hsu WK. Differences in bone mineral density of fixation points between lumbar cortical and traditional pedicle screws. Spine J. 2016;16:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Li HM, Zhang RJ, Gao H, Jia CY, Xing T, Zhang JX, Dong FL, Shen CL. Biomechanical Fixation Properties of the Cortical Bone Trajectory in the Osteoporotic Lumbar Spine. World Neurosurg. 2018;119:e717-e727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Perez-Orribo L, Kalb S, Reyes PM, Chang SW, Crawford NR. Biomechanics of lumbar cortical screw-rod fixation versus pedicle screw-rod fixation with and without interbody support. Spine (Phila Pa 1976). 2013;38:635-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 143] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 12. | Sakaura H, Miwa T, Yamashita T, Kuroda Y, Ohwada T. Posterior lumbar interbody fusion with cortical bone trajectory screw fixation versus posterior lumbar interbody fusion using traditional pedicle screw fixation for degenerative lumbar spondylolisthesis: a comparative study. J Neurosurg Spine. 2016;25:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 13. | Silva F, Silva PS, Vaz R, Pereira P. Midline lumbar interbody fusion (MIDLIF) with cortical screws: initial experience and learning curve. Acta Neurochir (Wien). 2019;161:2415-2420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Takenaka S, Mukai Y, Tateishi K, Hosono N, Fuji T, Kaito T. Clinical Outcomes After Posterior Lumbar Interbody Fusion: Comparison of Cortical Bone Trajectory and Conventional Pedicle Screw Insertion. Clin Spine Surg. 2017;30:E1411-E1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Kudo D, Shimada Y. Short-Term Results of Transforaminal Lumbar Interbody Fusion Using Pedicle Screw with Cortical Bone Trajectory Compared with Conventional Trajectory. Asian Spine J. 2015;9:440-448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 16. | Sebaaly A, Lahoud MJ, Rizkallah M, Kreichati G, Kharrat K. Etiology, Evaluation, and Treatment of Failed Back Surgery Syndrome. Asian Spine J. 2018;12:574-585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Rodriguez A, Neal MT, Liu A, Somasundaram A, Hsu W, Branch CL Jr. Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurg Focus. 2014;36:E9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Takata Y, Matsuura T, Higashino K, Sakai T, Mishiro T, Suzue N, Kosaka H, Hamada D, Goto T, Nishisho T, Goda Y, Sato R, Tsutsui T, Tonogai I, Tezuka F, Mineta K, Kimura T, Nitta A, Higuchi T, Hama S, Sairyo K. Hybrid technique of cortical bone trajectory and pedicle screwing for minimally invasive spine reconstruction surgery: a technical note. J Med Invest. 2014;61:388-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Crawford CH 3rd, Owens RK 2nd, Djurasovic M, Gum JL, Dimar JR 2nd, Carreon LY. Minimally-Invasive midline posterior interbody fusion with cortical bone trajectory screws compares favorably to traditional open transforaminal interbody fusion. Heliyon. 2019;5:e02423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Hsu WL, Lin YH, Chuang HY, Lee HC, Chen DC, Chu YT, Cho DY, Chen CH. Cortical Bone Trajectory Instrumentation with Vertebroplasty for Osteoporotic Thoracolumbar Compression Fracture. Medicina (Kaunas). 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Noh SH, Zhang HY. Minimally Invasive Spine Surgery With Midline Cortical Bone Trajectory Screw Fixation for Lumbar Degenerative Disease in a Retrospective Study of 200 Patients. Neurospine. 2021;18:355-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 22. | Zheng Z, Zhang L, Zhu Y, Chen J, Zhang X, Xia T, Wu T, Quan L, Zhao G, Ji X, Gui Z, Xue S, Yin Z. Percutaneous cortical bone trajectory screw fixation versus traditional open pedicle screw fixation for type A thoracolumbar fractures without neurological deficit. J Robot Surg. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Petrone S, Marengo N, Ajello M, Lavorato A, Penner F, Cofano F, Zenga F, Garbossa D. Cortical bone trajectory technique's outcomes and procedures for posterior lumbar fusion: A retrospective study. J Clin Neurosci. 2020;76:25-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Dayani F, Chen YR, Johnson E, Deb S, Wu Y, Pham L, Singh H. Minimally invasive lumbar pedicle screw fixation using cortical bone trajectory - Screw accuracy, complications, and learning curve in 100 screw placements. J Clin Neurosci. 2019;61:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Marengo N, Berjano P, Cofano F, Ajello M, Zenga F, Pilloni G, Penner F, Petrone S, Vay L, Ducati A, Garbossa D. Cortical bone trajectory screws for circumferential arthrodesis in lumbar degenerative spine: clinical and radiological outcomes of 101 cases. Eur Spine J. 2018;27:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 26. | Chen CH, Huang HM, Chen DC, Wu CY, Lee HC, Cho DY. Cortical bone trajectory screws fixation in lumbar adjacent segment disease: A technique note with case series. J Clin Neurosci. 2018;48:224-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Orita S, Inage K, Kubota G, Sainoh T, Sato J, Fujimoto K, Shiga Y, Nakamura J, Matsuura Y, Eguchi Y, Aoki Y, Toyone T, Yamauchi K, Sakuma Y, Oikawa Y, Suzuki T, Takahashi K, Hynes RA, Ohtori S. One-Year Prospective Evaluation of the Technique of Percutaneous Cortical Bone Trajectory Spondylodesis in Comparison with Percutaneous Pedicle Screw Fixation: A Preliminary Report with Technical Note. J Neurol Surg A Cent Eur Neurosurg. 2016;77:531-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Snyder LA, Martinez-Del-Campo E, Neal MT, Zaidi HA, Awad AW, Bina R, Ponce FA, Kaibara T, Chang SW. Lumbar Spinal Fixation with Cortical Bone Trajectory Pedicle Screws in 79 Patients with Degenerative Disease: Perioperative Outcomes and Complications. World Neurosurg. 2016;88:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Ninomiya K, Iwatsuki K, Ohnishi Y, Yoshimine T. Radiological Evaluation of the Initial Fixation between Cortical Bone Trajectory and Conventional Pedicle Screw Technique for Lumbar Degenerative Spondylolisthesis. Asian Spine J. 2016;10:251-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Elmekaty M, Kotani Y, Mehy EE, Robinson Y, Tantawy AE, Sekiguchi I, Fujita R. Clinical and Radiological Comparison between Three Different Minimally Invasive Surgical Fusion Techniques for Single-Level Lumbar Isthmic and Degenerative Spondylolisthesis: Minimally Invasive Surgical Posterolateral Fusion versus Minimally Invasive Surgical Transforaminal Lumbar Interbody Fusion versus Midline Lumbar Fusion. Asian Spine J. 2018;12:870-879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 31. | Wochna JC, Marciano R, Catanescu I, Katz J, Spalding MC, Narayan K. Cortical Trajectory Pedicle Screws for the Fixation of Traumatic Thoracolumbar Fractures. Cureus. 2018;10:e2891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Laratta JL, Shillingford JN, Pugely AJ, Gupta K, Gum JL, Djurasovic M, Crawford CH. Accuracy of cortical bone trajectory screw placement in midline lumbar fusion (MIDLF) with intraoperative cone beam navigation. J Spine Surg. 2019;5:443-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Phan K, Hogan J, Maharaj M, Mobbs RJ. Cortical Bone Trajectory for Lumbar Pedicle Screw Placement: A Review of Published Reports. Orthop Surg. 2015;7:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 34. | Marengo N, Matsukawa K, Monticelli M, Ajello M, Pacca P, Cofano F, Penner F, Zenga F, Ducati A, Garbossa D. Cortical Bone Trajectory Screw Placement Accuracy with a Patient-Matched 3-Dimensional Printed Guide in Lumbar Spinal Surgery: A Clinical Study. World Neurosurg. 2019;130:e98-e104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 35. | Buza JA 3rd, Good CR, Lehman RA Jr, Pollina J, Chua RV, Buchholz AL, Gum JL. Robotic-assisted cortical bone trajectory (CBT) screws using the Mazor X Stealth Edition (MXSE) system: workflow and technical tips for safe and efficient use. J Robot Surg. 2021;15:13-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 36. | Le X, Tian W, Shi Z, Han X, Liu Y, Liu B, He D, Yuan Q, Sun Y, Xu Y. Robot-Assisted Versus Fluoroscopy-Assisted Cortical Bone Trajectory Screw Instrumentation in Lumbar Spinal Surgery: A Matched-Cohort Comparison. World Neurosurg. 2018;120:e745-e751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 92] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 37. | Khan A, Rho K, Mao JZ, O'Connor TE, Agyei JO, Meyers JE, Mullin JP, Pollina J. Comparing Cortical Bone Trajectories for Pedicle Screw Insertion using Robotic Guidance and Three-Dimensional Computed Tomography Navigation. World Neurosurg. 2020;141:e625-e632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |