Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.13022
Peer-review started: August 8, 2022
First decision: October 12, 2022
Revised: October 24, 2022
Accepted: November 17, 2022
Article in press: November 17, 2022
Published online: December 16, 2022
Processing time: 128 Days and 3 Hours
Accessory soleus muscle (ASM) is a rare congenital variation that is almost asymptomatic, but several papers have recently described symptomatic ASM. The clinical features of this condition are similar to tarsal tunnel syndrome (TTS) and include pain and numbness around the medial side of the ankle. ASM commonly originates from the fibula or soleus muscle and inserts into the Achilles tendon or calcaneus. Usually, it is identified as posteromedial swelling and definitely diagnosed by magnetic resonance imaging. In most cases, treatment is observation, but surgical excision can be considered if symptoms are severe.
A 23-year-old male Korean soldier presented with complaints of bilateral foot and ankle pain and a swelling medial to the Achilles tendon that was more pronounced on the right side. Symptoms first occurred after playing soccer 10 mo before this presentation, worsened after physical exertion, and were relieved by rest. He had no medical history, and no one in his family had the condition. Laboratory results were non-specific. Several tests were performed to exclude common diseases such as tumors or TTS. However, MRI revealed a bulky accessory soleus muscle in both feet, though the patient complained of more severe pain on the right side during physical activity. Accordingly, surgical resection was adopted. At surgery, a large accessory soleus muscle was noted anterior to the Achilles tendon with distinctive insertion from a normal soleus muscle. At 12 mo after surgery, there was no pain, numbness, or swelling of the right foot or ankle, no evidence of recurrence, and the patient could do all sports activities.
Accessory soleus muscle should be added to the list of differential diagnosis if a patient has pain, sole numbness or swelling of the posteromedial ankle.
Core Tip: The Accessory soleus muscle (ASM) is considered a rare congenital variation, and is usually asymptomatic. However, patients can present with sole numbness, posteromedial ankle pain, and, in rare cases, exertional compartment syndrome. In the majority of cases, diagnosis can be confirmed by magnetic resonance imaging. Observation is commonly recommended but surgical resection can be considered if symptoms are severe. ASM should be added to the list of differential diagnosis if a patient has pain, sole numbness, or swelling of the posteromedial ankle.
- Citation: Woo I, Park CH, Yan H, Park JJ. Symptomatic accessory soleus muscle: A cause for exertional compartment syndrome in a young soldier: A case report. World J Clin Cases 2022; 10(35): 13022-13027
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/13022.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.13022
Accessory soleus muscle (ASM) is a rare congenital variation that presents as a posteromedial ankle swelling that tends to worsen during physical activity. Its clinical features are similar to tarsal tunnel syndrome (TTS) and include pain and numbness around the medial side of the ankle. However, because of its tumor-like appearance, ASM must be distinguished from tumors, ganglion cyst, hemangioma, and lipoma. ASM commonly originates from the fibula or soleus muscle and inserts into the Achilles tendon or calcaneus[1-4]. According to autopsy studies, the prevalence of ASM is 0.5%-6% and is almost twice as common in males[5].
Cruveilhier first described ASM in 1843, but it was not until 1965 that the first clinical case was reported in the English literature[6]. Most reports issued on the topic are cadaveric studies or incidental clinical reports, and somewhat surprisingly the symptoms of ASM have not been fully established. The majority of reported cases were asymptomatic, although some presented with symptoms. ASM is mainly located in the posteromedial region of the ankle, in front of the Achilles tendon, and behind the deep posterior compartment of the lower leg. Many have reported compression of the neurovascular bundle leading to exertional compartment syndrome caused by the proximities of the tibial nerve and posterior tibial vessels. Treatment of choice is either surgical excision or fasciotomy for the symptomatic patients[7,8].
ASM characteristically occupies the posterior compartment of the lower leg, and thus may cause exertional compartment syndrome. Here we introduce a patient who had clinical exertional compartment syndrome with ASM and describe its treatment and prognosis.
A 23-year-old male Korean soldier presented with complaints of bilateral foot and ankle pain and a swelling medial to the Achilles tendon that was more pronounced on the right side.
Symptoms occurred after playing soccer 10 mo before presentation, worsened after physical exertion, and were relieved by rest.
The patient had no specific underlying disease.
Before joining the army, the patient had not exercised heavily and had never had foot or ankle pain. There was no relevant family history.
Physical examination demonstrated mass like lesion and mild tenderness around the posteromedial side of the ankle, in front of the Achilles tendon. No pain was reported at the Achilles tendon insertion, and motions of ankle and subtalar joints were normal. Mild numbness was observed on the soles of both feet, and Tinel’s sign was positive bilaterally along the tibial nerve posterior to the medial malleolar.
Routine blood and urine tests, blood biochemistry, and immune and infection indices were normal, and an electrophysiological study produced no definite evidence of tibial nerve compression in the tarsal tunnel.
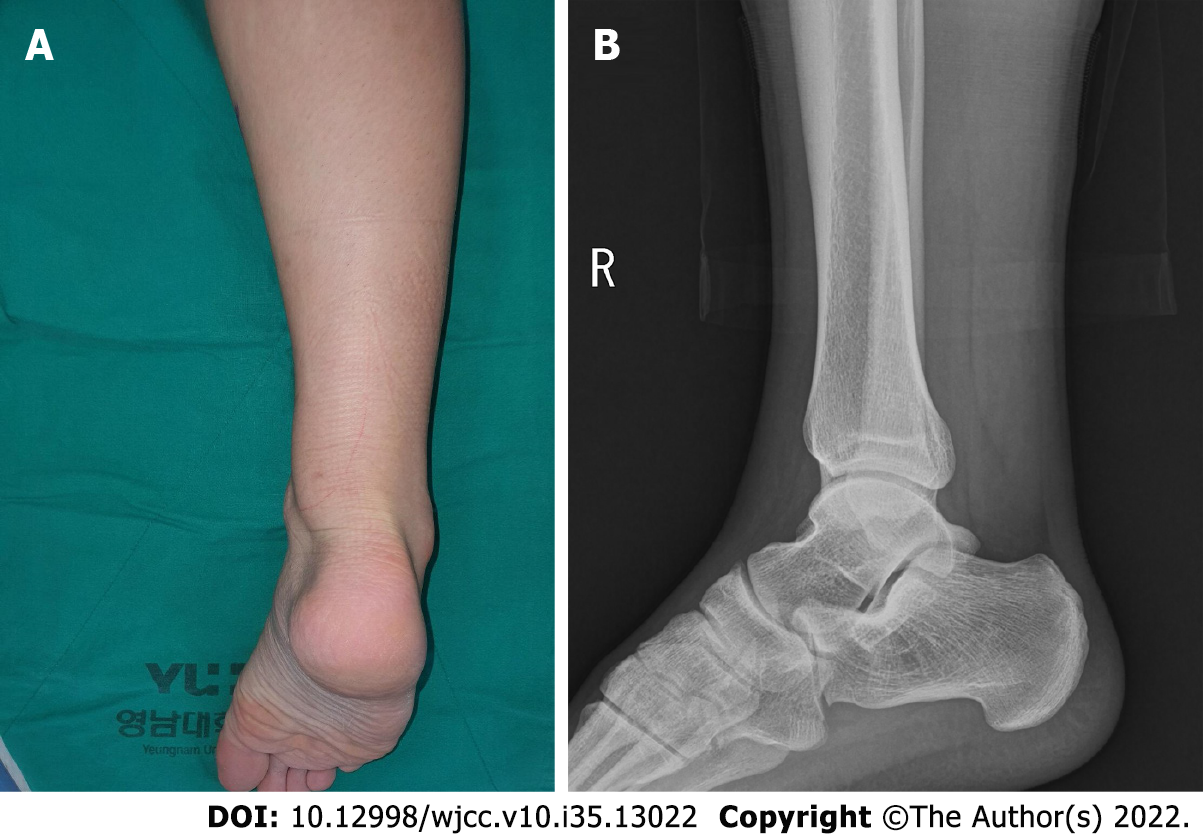
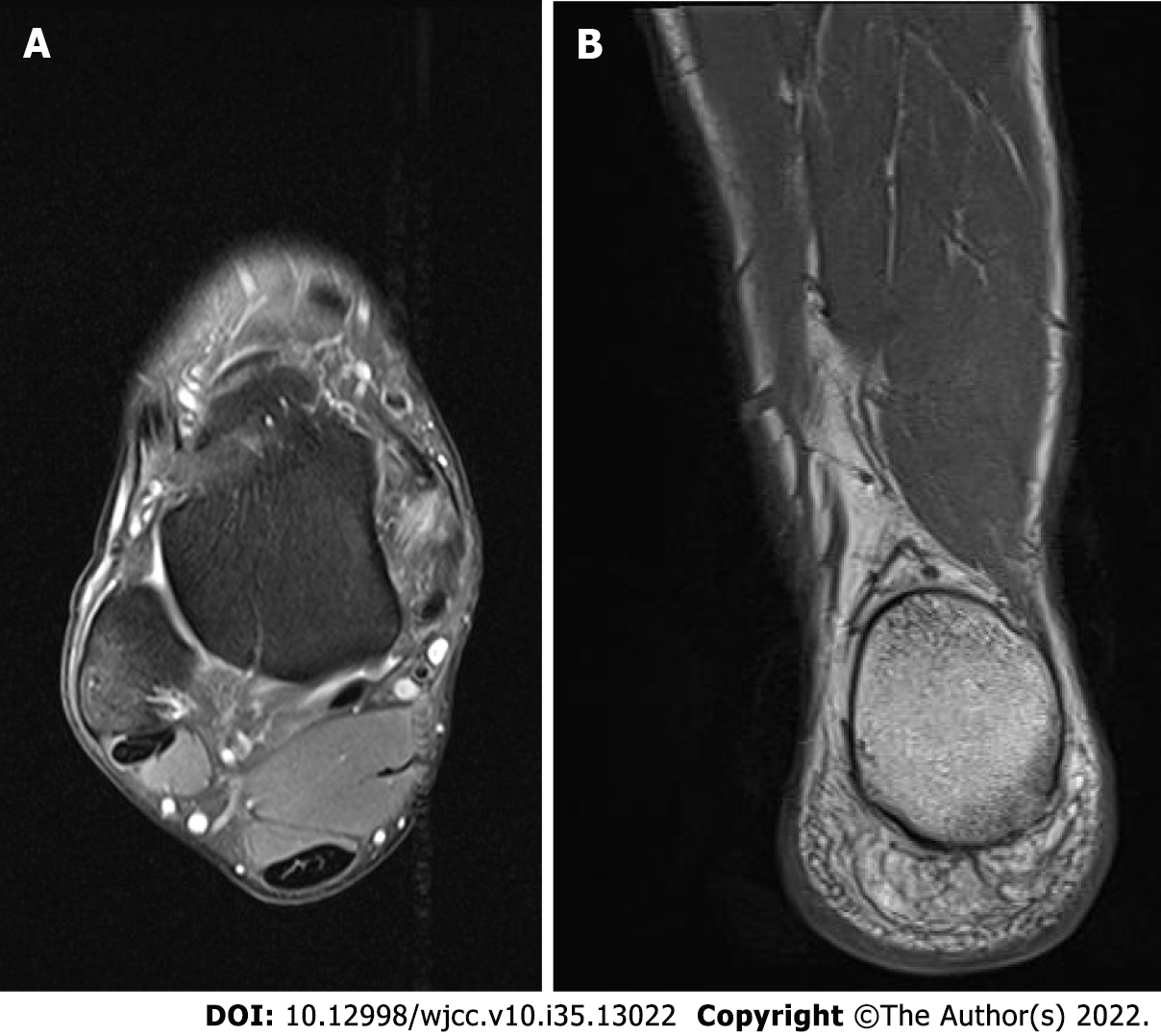
Plain radiographs revealed no bony abnormality, but a soft tissue mass obliterated Kager’s triangle on both sides. 3.0 Tesla magnetic resonance imaging (MRI) performed on the more symptomatic right side, depicted an isolated accessory muscle belly of soleus muscle within the superficial, deep compartment lying posterior to the neurovascular bundle inserting directly at the medial aspect of the calcaneus (Figures 1 and 2).
Based on these findings, we diagnosed bilateral exertional compartment syndrome caused by an ASM. In addition, based on consideration of his symptoms, this was diagnosed to be associated with intermittent tarsal tunnel syndrome due to exertional compartment syndrome despite a lack of abnormal electrophysiological findings.
The treatment method was discussed with the patient, who stressed he wanted to participate in sports activities without pain. Thus, it was decided to adopt a surgical course and excise the more symptomatic right-side ASM.
At surgery, a straight 15-cm incision was made along the posteromedial side of the tibia above the enlarged palpable muscle. The ASM was noted just anterior to the Achilles tendon and inserted into the medial aspect of the calcaneus by a separate tendon just in front of the Achilles tendon. Most of the muscle mass was readily isolated from soleus muscle, but the origin of the ASM was not clearly distinguished. After detaching the ASM from its insertion, blunt dissection was performed bluntly from the soleus origin. A tourniquet was used for bleeding control. Because of the large defect formed, a silastic drain was inserted into the surgical wound before skin closure (Figure 3).
A short leg splint was applied, and weight bearing was prohibited for two weeks after surgery, when partial weight bearing was allowed. At 12, and 24 mo after surgery, he visited the outpatient clinic for regular follow-up. No pain, numbness, or swelling of the right foot or ankle was evident at these follow-up visits, and the patient was able to perform all sports activities without pain. There was no evidence suspicious of recurrence. He reported slight, similar discomfort in both feet during daily life.
ASM is a rare congenital variation of lower extremity muscles. The muscle originates from its own fascia, is isolated from normal soleus muscle, and supplied by posterior tibial artery like normal soleus muscle[8]. ASM generally originates from the posteromedial aspect of the tibia, at the anterior aspect of the Achilles tendon[9]. Regarding insertion sites, Lorentzon et al[10] described four anatomic variations: (1) Insertion along the Achilles tendon; (2) Fleshy insertion to the upper calcaneal surface; (3) Tendinous insertion to the upper calcaneal surface; and (4) Fleshy insertion to the medial calcaneal surface. Yu et al[11] later added tendinous insertion to the medial calcaneal surface.
Although the number of case reports issued on ASM is increasing, presumably due to increased use of MRI, few reports have been published on symptomatic accessory soleus muscle, and cases comparable to exertional compartment syndrome have rarely been reported. From this point of view, the described case is meaningful as it details a condition that orthopedic surgeons can differentiate. We suppose that reduced blood stream to muscle compartment, physical activity-related compartment syndrome, or compressive neuropathy such as the tibial nerve are responsible for painful swelling of the ASM after physical activity that subsides with rest. Although the ASM is located outside the tarsal tunnel, it can cause TTS by extrinsic compression. In our case, the patient also complained of mild sole numbness and painful swelling aggravated by sports activities, although electrophysiological study produced no findings suggesting TTS. As mentioned previously[12], ASM sometimes involves both sides, as was suspected in our patient. However due to the cost involved, MRI was only performed on the more severe right side. Fortunately, both sides were improved after taking a break after he had taken a break after surgery, which prevented our confirming bilaterally.
Typically, ASM can be diagnosed based on the history, and physical and imaging findings. Patients generally present with a mass like lesion medially palpable Kager’s triangle. Plain radiographs suggest obliteration of Kager’s triangle with soft tissue swelling between deep and superficial posterior compartments in lateral ankle view[12]. MRI seems to be the diagnosis of choice for achieving a definitive diagnosis and distinguishing ASM, which is isointense with normal muscles, and soft tissue tumors in the posteromedial aspect of the ankle[13].
No treatment is required for asymptomatic patients[14], but surgical treatment can be considered if pain is provoked by exertion. When exertional compartment syndrome is suspected, fasciotomy and excision can be considered after excluding other diseases. Our patient had entrapment symptoms similar to TTS, and thus TTS was excluded by performing a nerve conduction test. Surgical treatment was performed after confirming results. Recently, botulinum injections have been used to treat ASM. However, in our case, the muscle was large, and thus excision was adopted[15].
This study has a notable limitation. By allowing rest after surgery, it was difficult to determine whether the observed improvement was due to resection or taking enough rest. In particular, our patient complained of bilateral foot pain at presentation but reported no foot pain on either side one year after surgery.
Symptomatic ASM is rare and can cause foot or ankle pain and discomfort in active young adults. ASM should be added to the list of differential diagnosis if a patient has pain, sole numbness, or swelling of the posteromedial ankle.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dang SS, China; Doski JO, Iraq; Singh M, United States S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Plečko M, Knežević I, Dimnjaković D, Josipović M, Bojanić I. Accessory Soleus Muscle: Two Case Reports with a Completely Different Presentation Caused by the Same Entity. Case Rep Orthop. 2020;2020:8851920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Romanus B, Lindahl S, Stener B. Accessory soleus muscle. A clinical and radiographic presentation of eleven cases. J Bone Joint Surg Am. 1986;68:731-734. [PubMed] |
| 3. | Cho BW, Choi JH, Han HS, Choi WY, Lee KM. Age, Body Mass Index, and Spur Size Associated with Patients' Symptoms in Plantar Fasciitis. Clin Orthop Surg. 2022;14:458-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 4. | Park HG, Youn D, Baik JM, Hwang JH. Epidemiology of Achilles Tendon Rupture in South Korea: Claims Data of the National Health Insurance Service from 2009 to 2017. Clin Orthop Surg. 2021;13:539-548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Randell M, Marsland D, Jenkins O, Forster B. Minimally Invasive Tendon Release for Symptomatic Accessory Soleus Muscle in an Athlete: A Case Report. J Foot Ankle Surg. 2019;58:644-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Dunn AW. Anomalous muscles simulating soft-tissue tumors in the lower extremities. Report of three cases. J Bone Joint Surg Am. 1965;47:1397-1400. [PubMed] |
| 7. | Mayer WP, Baptista JDS, Azeredo RA, Musso F. Accessory soleus muscle: a case report and clinical applicability. Autops Case Rep. 2013;3:5-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Carrington SC, Stone P, Kruse D. Accessory Soleus: A Case Report of Exertional Compartment and Tarsal Tunnel Syndrome Associated With an Accessory Soleus Muscle. J Foot Ankle Surg. 2016;55:1076-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Brodie JT, Dormans JP, Gregg JR, Davidson RS. Accessory soleus muscle. A report of 4 cases and review of literature. Clin Orthop Relat Res. 1997;180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Lorentzon R, Wirell S. Anatomic variations of the accessory soleus muscle. Acta Radiol. 1987;28:627-629. [PubMed] |
| 11. | Yu JS, Resnick D. MR imaging of the accessory soleus muscle appearance in six patients and a review of the literature. Skeletal Radiol. 1994;23:525-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Chotigavanichaya C, Scaduto AA, Jadhav A, Otsuka NY. Accessory soleus muscle as a cause of resistance to correction in congenital club foot: a case report. Foot Ankle Int. 2000;21:948-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Doda N, Peh WC, Chawla A. Symptomatic accessory soleus muscle: diagnosis and follow-up on magnetic resonance imaging. Br J Radiol. 2006;79:e129-e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | John MM, Borrelli AH. Asymptomatic accessory soleus muscle. J Foot Ankle Surg. 1999;38:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Isner-Horobeti ME, Muff G, Lonsdorfer-Wolf E, Deffinis C, Masat J, Favret F, Dufour SP, Lecocq J. Use of botulinum toxin type A in symptomatic accessory soleus muscle: first five cases. Scand J Med Sci Sports. 2016;26:1373-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |