Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12261
Peer-review started: June 4, 2022
First decision: August 4, 2022
Revised: August 6, 2022
Accepted: October 26, 2022
Article in press: October 26, 2022
Published online: November 26, 2022
Processing time: 165 Days and 0.7 Hours
The common area of breast cancer metastases are bone, lung and liver. Brachial plexus metastasis from breast cancer is extremely rare. We report a case of subclavian brachial plexus metastasis from breast cancer 6 years postoperative, which were detected by ultrasound, magnetic resonance imaging (MRI) and 18F-fluorodeoxyglucose positron emission tomography and computed tomography (FDG-PET/CT).
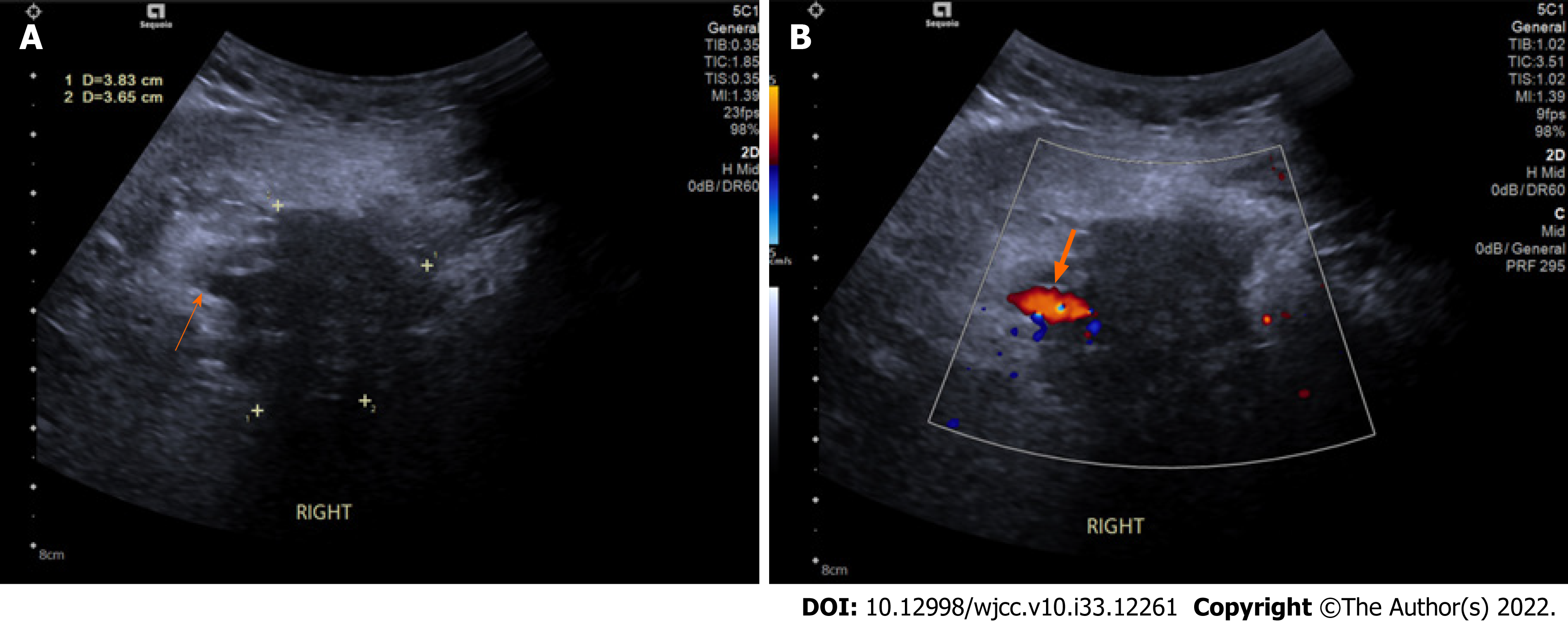
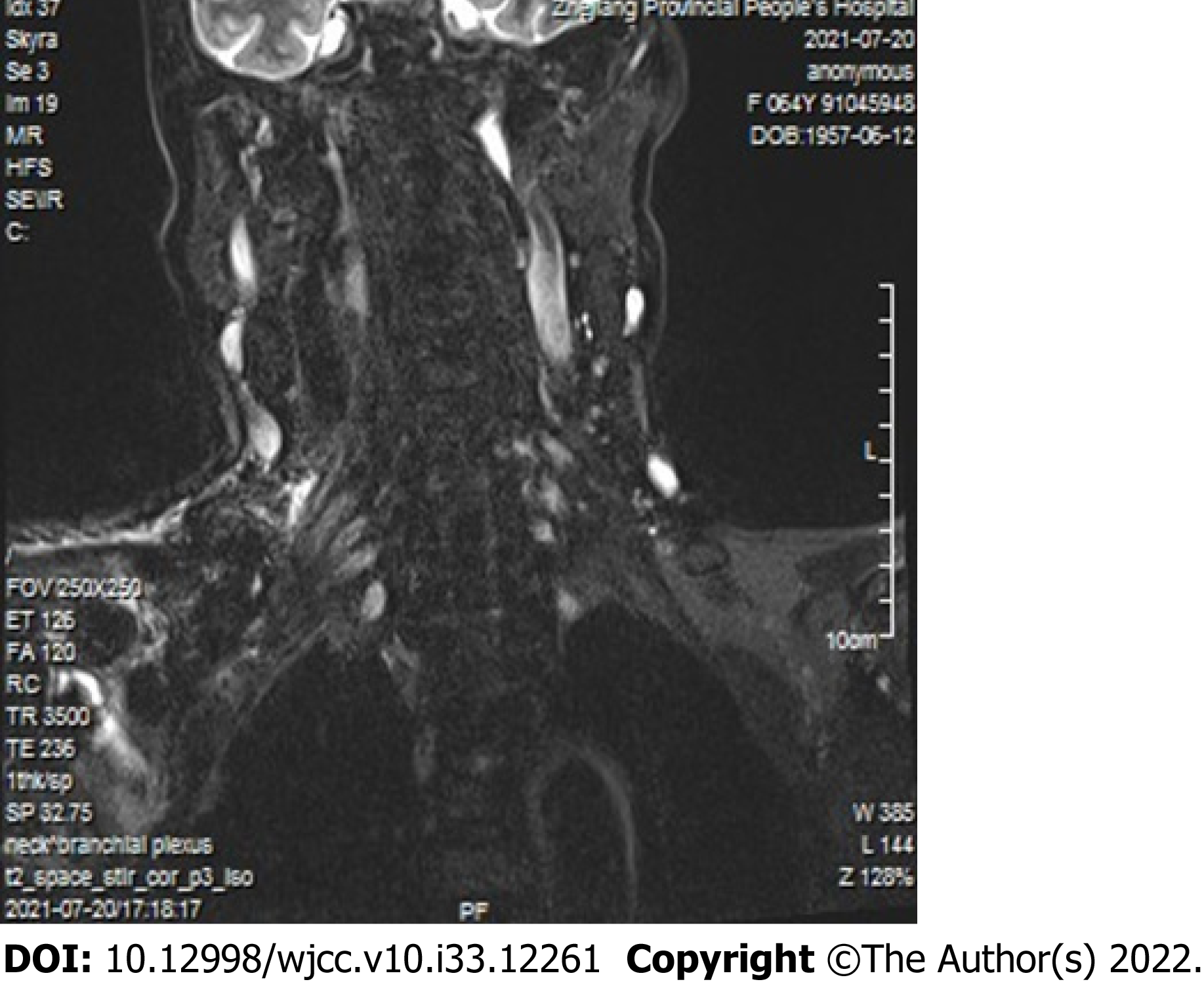
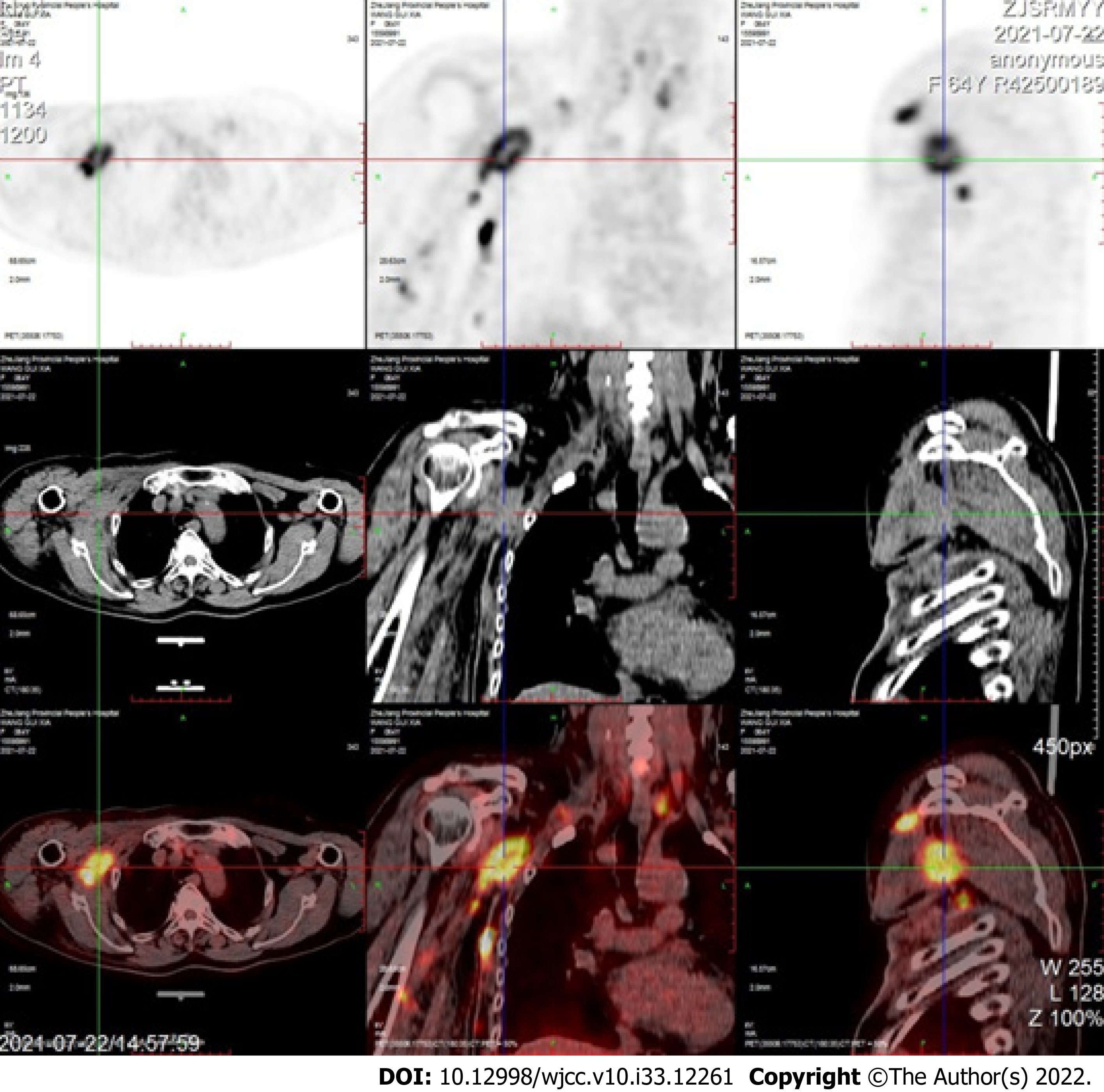
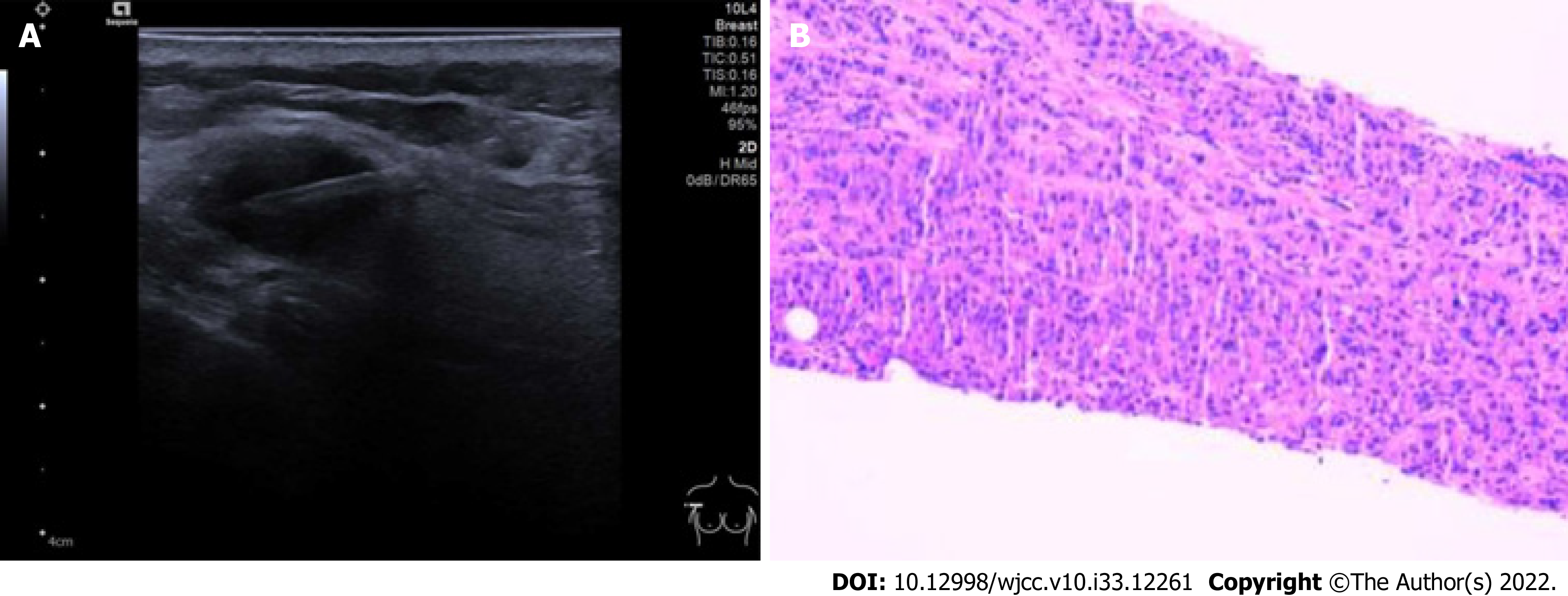
Our study reports a 64-year-old woman who had right breast cancer and underwent radical mastectomy 6 years before. Ultrasound first revealed a soft lesion measuring 38 mm × 37 mm which located on the right side of the clavicle to the armpit subcutaneously. The right subclavian brachial plexus (beam level) was significantly thickened, wrapped around by a hypoechoic lesion, the surrounded axillary artery and vein were pressed. MRI brachial plexus scan showed that the right side of brachial plexus was enlarged compared with the left side and brachial plexus bundle in the distance showed a flake shadow. FDG-PET/CT revealed that the right side of brachial plexus nodular appearance with increased FDG metabolism. These results supported brachial plexus metastasis from breast cancer. Ultrasound exam also found many lesions between pectoralis major, deltoid muscle and inner upper arm. The lesion puncture was performed under ultrasound guidance and the tissue was sent for pathology. Pathology showed large areas of tumor cells in fibroblast tissue. Immunohistochemistry showed the following results: A2-1: GATA3 (+), ER (+, strong, 90%), PR (+, moderate, 10%), HER-2 (3+), Ki67 (+15%), P120 (membrane+), P63 (-), E-cadherin (+), CK5/6 (-). These results were consistent with the primary right breast cancer characteristics, thus supporting lesion metastasis from breast cancer.
The brachial plexus metastasis from breast cancer is uncommon. Ultrasound has great value in detecting brachial plexus metastasis of breast cancer. It is an easy, non-invasive and affordable method. Close attention should be paid to new grown out lesions in those patients who had a history of breast cancer when doing ultrasound review.
Core Tip: Breast cancer metastases are commonly found in bone, lung and liver. Brachial plexus metastasis from breast cancer is extremely rare. We here report a 64-year-old woman who had brachial plexus metastasis from breast cancer. Ultrasound is an easy, non-invasive and affordable method for the detection of brachial plexus metastasis from breast cancer. Attention should be paid to new lesions in patients with a history of breast cancer when performing ultrasound review.
- Citation: Zeng Z, Lin N, Sun LT, Chen CX. Subclavian brachial plexus metastasis from breast cancer: A case report. World J Clin Cases 2022; 10(33): 12261-12267
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12261.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12261
Breast cancer is the most threatening cancer in women worldwide[1]. Bones, lungs, liver and lymph nodes are common predilection sites of breast cancer metastasis[2]. Brachial plexus metastasis from breast cancer is extremely rare. So diagnosing this metastasis shows great challenging. We report a case of a 64-year-old woman who had subclavian brachial plexus metastasis 6 years after radical mastectomy. Ultrasound was the first exam to find the metastasis lesion both at brachial plexus and muscles. Magnetic resonance imaging (MRI) and 18F-fluorodeoxyglucose positron emission tomography and computed tomography (FDG-PET/CT) gave further identification of brachial plexus metastasis. Pathology and immunohistochemistry results indicated lesions between pectoralis major and deltoid muscle as metastasis from breast cancer. The diagnosis has clinical importance for the next step of treatment whether by radiotherapy, chemotherapy or hormonal therapy.
A 64-year-old woman went to our ultrasound department with a lesion on the right side of the clavicle to the armpit subcutaneously. Her right upper arm was edema and accompanied by pain, numbness and discomfort in the right finger.
The patient was diagnosed with right breast cancer 6 years before. Her primary lesion was invasive breast cancer (T2N1M0), immunohistochemistry showed ER (+), PR (+), HER-2 (+++). At that time she had right radical mastectomy and accepted both chemotherapy and radiotherapy.
There is no history of past illness.
There is no personal and family history.
Scars were seen in the right chest area. The arm circumference was significantly widened. The upper part of the right forearm near to the proximal elbow was edema, with greater tension, accompanied by pain, numbness and discomfort at the end of the fingers. There was no difference in the remaining limbs, and the pathological signs were not elicited.
Blood test showed an elevated tumor marker-cytokeratin (CK) (195.1 ng/mL).
Ultrasound found a soft lesion measuring 38 mm × 37 mm which located on the right side of the clavicle to the armpit subcutaneously (Figure 1). Then series of other imaging and blood tests were done. MRI brachial plexus scan showed that the right side of brachial plexus was enlarged compared with the left side and brachial plexus bundle in the distance showed a flake shadow (Figure 2). FDG-PET/CT revealed that the right side of brachial plexus nodular appearance with increased FDG metabolism, an SUVmax of 13.7 (Figure 3). Ultrasound exam also found many lesions between pectoralis major, deltoid muscle and inner upper arm.
All imaging examinations suggested brachial plexus metastasis from breast cancer. Pathology showed large areas of tumor cells in fibroblast tissue. Immunohistochemistry showed the following results: A2-1: GATA3 (+), ER (+, strong, 90%), PR (+, moderate, 10%), HER-2 (3+), Ki67 (+15%), P120 (membrane+), P63 (-), E-cadherin (+), CK5/6 (-) (Figure 4).
The patient underwent lesion punctuation and the lesion was sent for pathology.
The patient abandoned treatment.
Breast cancer had the highest incidence rate of cancers in women worldwide[1]. The common area of breast cancer metastases are bone, brain, lung and liver. Brachial plexus metastasis from breast cancer is extremely rare. In this case report, we described a patient of subclavian brachial plexus metastasis after breast cancer. Our patient had a soft lesion located on the right side of the clavicle to the armpit on the chest wall subcutaneously. Ultrasound with high frequency probe (> 10 MHz) is vital in detecting subcutaneous lesions. It can reveal the lesion’s size, shape, depth of tissue and the blood supply and give out a tendency diagnosis[3]. In our department, assessment of breast and axilla is a routine for the breast cancer patients both pre-operation and post-operation in order to find and review breast lesions and metastasis lesions. In retrospect of this patient’s ultrasound images, many sonographic features suggested that the soft lesion which located on the right side of the clavicle to the armpit subcu
FDG-PET/CT revealed that the right side of brachial plexus nodular appearance with increased FDG metabolism, a SUVmax of 13.7. FDG-PET/CT is a noninvasive techniques which play a vital role in cancer with the aspects of staging, restaging and treatment monitoring[5]. It is also a sensitive way to help with identifying the nature of lesions. In this case, we found brachial plexus metastasis after radical mastectomy of a breast cancer patient. This patient had right breast cancer 6 years before and also diagnosed brachial plexus metastasis on the right side this time. Increased uptake was found in right brachial plexus with an SUVmax of 13.7. The radioactivity uptake also increased in many lesions between pectoralis major and deltoid muscle, with an SUVmax of 16.8. Thus FDG-PET/CT confirming brachial plexus and chest wall metastases.
We reviewed the literature on some novel location metastases from breast cancer. We summarized many case reports of rare metastasis of breast cancer (Table 1)[6]. It includes patients’ basic characterisitcs, tumors’ size and location. Liu et al[7] reported a soft tissue nodule which was located on the top left side of the scalp subcutaneously in a woman who underwent a mastectomy after diagnosed as right breast cancer. They concluded that soft tissue lesions should be given special attention in those patients with malignant cancer history. KANEKO et al[8] described a female patient of right invasive lobular breast carcinoma. This patient had a rare isolated gastric metastasis 7 years after right mastectomy and axillary lymph node dissection. Apodaca-Rueda et al[9] reported a 64-year-old female who had pancreatic metastasis 2 years after neoadjuvant therapy, mastectomy and adjuvant radiation therapy. They concluded that although pancreatic metastasis from breast cancer was rare, when the patient was detected a pancreatic lesion with breast cancer history should be considered carefully. Bakraoui et al[10] presented a rare case of a triple-negative breast cancer patient who was found orbital metastasis 2 mo after the end of adjuvant therapy. A case of bladder metastasis during treatment for recurrent breast cancer was reported by Yoneyama et al[11]. Bladder metastasis usually originates from peripheral organs such as the colon and rectum, cervix and prostate. Cancer metastasis from distant organ such as breast to bladder is really rare[11]. In these patients, early detect metastasis and treatment can help the clinical management thus influencing the prognosis and increasing patients survival. So we strongly recommend that women with breast cancer history should have a thorough examination of many organs not only breast but also armpits, subclavian area, abdomen, urinary system and so on once a year or more frequently.
Brachial plexus is the plexus of nerves which can supply the upper limb. It is made by the union of ventral rami of C5, C6, C7, C8 and T1 spinal nerves. Brachial plexus has roots, trunks, cords, divisions and branches. The roots and trunks variation of brachial plexus are rare, however, the origin and distribution of the branches of brachial plexus are very common[12,13]. More attention should be paid to these variations which can mislead to the assessment of the metastasis. Another import thing we should pay attention is that in the absence of breast lesions, diagnosis of metastatic cancer will be challenging and even delayed. When we diagnose a disease, we need to think logically, including understanding the patient’s past and current disease history, because these are important basis for diagnosis. Physical examination and extensive investigations are needed when diagnosing metastatic carcinoma[14]. Multidisciplinary team also shows great value in diagnosing.
Brachial plexus metastasis from breast cancer is extremely rare. When a healthy appearance patient who had breast cancer history complains about newly grown out lesion, ultrasound and further imaging tests such as MRI or FDG-PET/CT should be carefully applied. Ultrasound is an easy, non-invasive and affordable method in detecting metastasis lesions. FDG-PET/CT is an expensive method which can help to identify the nature of the lesion. Pathology is the golden standard to identify the metastasis lesion.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hasan A, Egypt; Nayak S, India S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global Cancer in Women: Burden and Trends. Cancer Epidemiol Biomarkers Prev. 2017;26:444-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 804] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 2. | Siegel RL, Fedewa SA, Miller KD, Goding-Sauer A, Pinheiro PS, Martinez-Tyson D, Jemal A. Cancer statistics for Hispanics/Latinos, 2015. CA Cancer J Clin. 2015;65:457-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 351] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 3. | Klimonda Z, Karwat P, Dobruch-Sobczak K, Piotrzkowska-Wróblewska H, Litniewski J. Breast-lesions characterization using Quantitative Ultrasound features of peritumoral tissue. Sci Rep. 2019;9:7963. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Kim J, Jeon JY, Choi YJ, Choi JK, Kim SB, Jung KH, Ahn JH, Kim JE, Seo S. Characteristics of metastatic brachial plexopathy in patients with breast cancer. Support Care Cancer. 2020;28:1913-1918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Tasdemir B, Dostbil Z, Inal A, Unal K, Yildirim S, Simsek FS. Evaluation of clinical contributions provided by addition of the brain, calvarium, and scalp to the limited whole body imaging area in FDG-PET/CT tumor imaging. Biomed Res Int. 2014;2014:129683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Fu JX, Zou YN, Long-Li, Wang XJ. Widespread Metastasis to the Stomach 10 Years After Primary Breast Cancer: A case report and review of the literature. Medicine (Baltimore). 2020;99:e22527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Liu YF, Liu LY, Xia SL, Li T, Li J. An Unusual Case of Scalp Metastasis from Breast Cancer. World Neurosurg. 2020;137:261-265. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kaneko Y, Koi Y, Kajitani K, Ohara M, Daimaru Y. Asymptomatic solitary metastasis to the stomach from breast cancer: A case report. Mol Clin Oncol. 2020;13:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Apodaca-Rueda M, Chaim FHM, Garcia MDS, Saito HPA, Gestic MA, Utrini MP, Callejas-Neto F, Chaim EA, Cazzo E. Solitary pancreatic metastasis from breast cancer: case report and review of literature. Sao Paulo Med J. 2019;137:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | El Bakraoui K, El Morabit B. Orbital Metastasis from Triple-Negative Breast Cancer: Case Report and Literature Review. Case Rep Oncol. 2020;13:1042-1046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Yoneyama K, Nakagawa M, Hara A. Bladder metastasis from primary breast cancer: a case report. Surg Case Rep. 2018;4:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Satheesha NAYAK, Nagabhooshana SOMAYAJI, Venkata Ramana VOLLALA. A rare variation in the formation of the upper trunk of the brachial plexus-A case report. Neuroanatomy. 2005;4:37-38. |
| 13. | Shetty SD, Nayak BS, Madahv V. A study on the variations in the formation of the trunks of brachial plexus. Int J Morphol. 2011;29:555-558. |
| 14. | Alfian Sulai DD, Krishnasamy T, Nik Mahmood NRK. Diagnostic challenge in silent metastatic invasive breast carcinoma: dysphagia as the only symptom. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |