Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.11882
Peer-review started: May 24, 2022
First decision: August 21, 2022
Revised: August 29, 2022
Accepted: October 9, 2022
Article in press: October 9, 2022
Published online: November 16, 2022
Processing time: 168 Days and 0.8 Hours
Pancreatitis is a severe inflammatory pancreatic disease commonly due to bile duct stones or excessive alcohol usage, with clinical manifestations of abdominal pain, nausea, fever, and fluid collections. Healthy persons with less symptomatic pancreatitis are quite rare. Herein, we report a case of a patient with an unde
A 50-year-old woman visited our hospital for tenderness in the left arm over several recent days. She was diagnosed with cellulitis on the left arm due to left elbow tenderness. Intravenous antibiotics administration did not improve symptoms and laboratory data worsened; thus, chest and abdominal computed tomography (CT) was performed. CT demonstrated pancreatitis with pseudocyst around the pancreas extending to the mediastinum. Thrombotic vasculitis of the brachiocephalic to left brachial vein was observed, which could be the cause of left elbow pain. A pancreatic fistula was found in the head of the pancreas by endoscopic retrograde cholangiopancreatography, so a pancreatic cyst drainage tube via the duodenum was placed in the pseudocyst. Cyst content culture was positive for Escherichia coli infection. Clinical symptoms, imaging findings, and inflammatory reactions resolved gradually after starting therapeutic intervention. The mediastinal pancreatic pseudocysts shrunk, and the venous thrombi remained but shrunk.
The case of a patient with pancreatitis with an undetermined onset that mimics left arm cellulitis is reported. Deep vein thrombosis should be kept in mind when treating patients with severe inflammatory disease.
Core Tip: Pancreatitis is a severe inflammatory disease commonly caused by bile duct stones or alcohol usage, with clinical manifestations of abdominal pain, nausea, fever, fluid collections, etc. Because of its severity, it is rare to experience patients with less symptomatic pancreatitis. Herein, a 50-year-old Japanese woman was referred to our hospital due to a history of cough and fatigue for 2 mo and recent left elbow tenderness. Computed tomography showed pancreatic pseudocysts in adjacent tissues and mediastinum, with thrombotic vasculitis in the brachiocephalic to left brachial vein. A history of pancreatitis might cause systemic coagulopathy, which may result in brachiocephalic vein thrombosis.
- Citation: Kokubo R, Yunaiyama D, Tajima Y, Kugai N, Okubo M, Saito K, Tsuchiya T, Itoi T. Brachiocephalic to left brachial vein thrombotic vasculitis accompanying mediastinal pancreatic fistula: A case report. World J Clin Cases 2022; 10(32): 11882-11888
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/11882.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.11882
Pancreatitis is a severe inflammatory pancreatic disease commonly due to bile duct stones or alcohol usage, with clinical manifestations of abdominal pain, nausea, fever, fluid collections, etc[1]. Acute or chronic pancreatitis is at risk of pancreatic fistula to adjacent tissues, and it might extend to the mediastinum through the esophageal hiatus or aortic hiatus, which is called mediastinal pancreatic pseudocyst (MPP)[2,3]. The notifying signs of MPP include chest pain, dyspnea, and systemic inflammatory changes, and diagnostic imaging modalities like computed tomography (CT) or magnetic resonance imaging (MRI) have an enormous role for its definitive diagnosis[4,5]. Rare types of signs of MPP-like pancreatic panniculitis[6], multiple ascending aortic mural thrombi[7], or symmetrical peripheral gangrene[8] were also reported; however, no case of MPP accompanying brachiocephalic thrombotic vasculitis has been reported. Herein, we present of a case of a patient with an undetermined onset of pancreatitis that resulted in MPP with brachiocephalic vein thrombotic vasculitis mimicking left arm cellulitis.
A 50-year-old Japanese woman with left elbow tenderness for several days was referred to the department of dermatology of our hospital.
She suffered from cough at night and exertional dyspnea for more than six months, bilateral lower extremity edema for two months, and fatigue, which worsened in recent months. Left elbow tenderness was also noted, so she was referred to the department of dermatology of our hospital.
The patient’s medical history included epilepsy.
The patient had no family history of similar illnesses.
Her body temperature was 38.9 °C, with a heart rate of 150/min, blood pressure of 120/85 mmHg, respiratory rate of 20/min, and SpO2 of 98% at room air. Tender, erythematous, and edematous left arm was observed (Figure 1).
The following results were observed at the initial examination: White blood cell count, 14600/μL (segmented, 84.9%); red blood cell count, 322 × 104/μL; hemoglobin level, 10.6 g/dL; platelet count, 53.1 × 104/uL; total protein level, 4.7 g/dL; albumin level, 1.8 g/dL; total bilirubin level, 0.35 mg/dL; aspartate aminotransferase, 16 U/L; alanine aminotransferase, 10 U/L; γ-glutamyl transpeptidase, 52 IU/L; lactate dehydrogenase, 269 IU/L; alkaline phosphatase, 352 IU/L; urea nitrogen, 8.8 mg/dL; creatinine, 0.49 mg/dL; creatine kinase, 26 U/L; uremic acid, 4.2 mg/dL; Na, 133 mmol/L; K, 3.6 mmol/L; Cl, 102 mmol/L; c-reaction protein, 22.0 mg/dL; and D-dimer, 12.7 μg/mL.
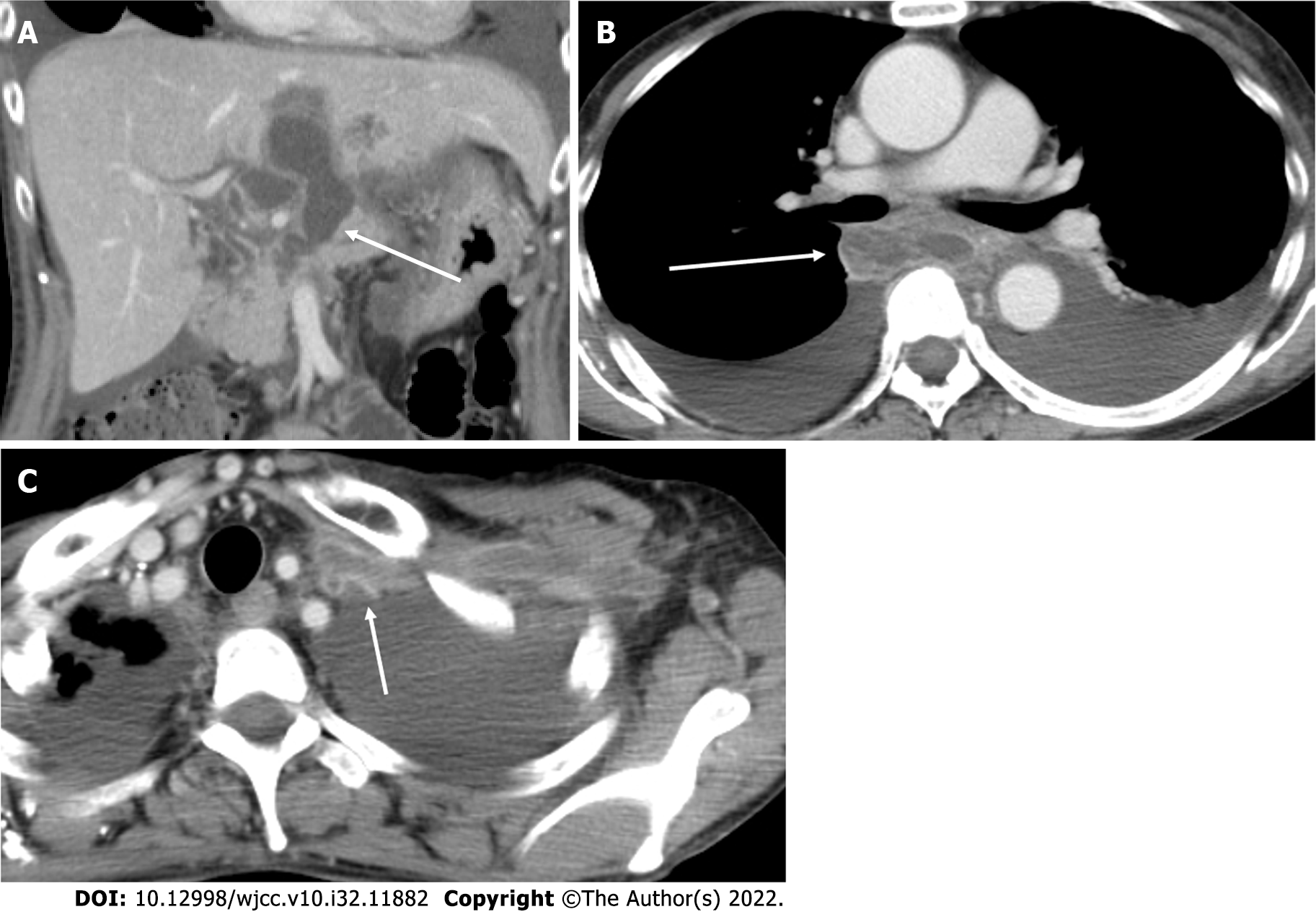
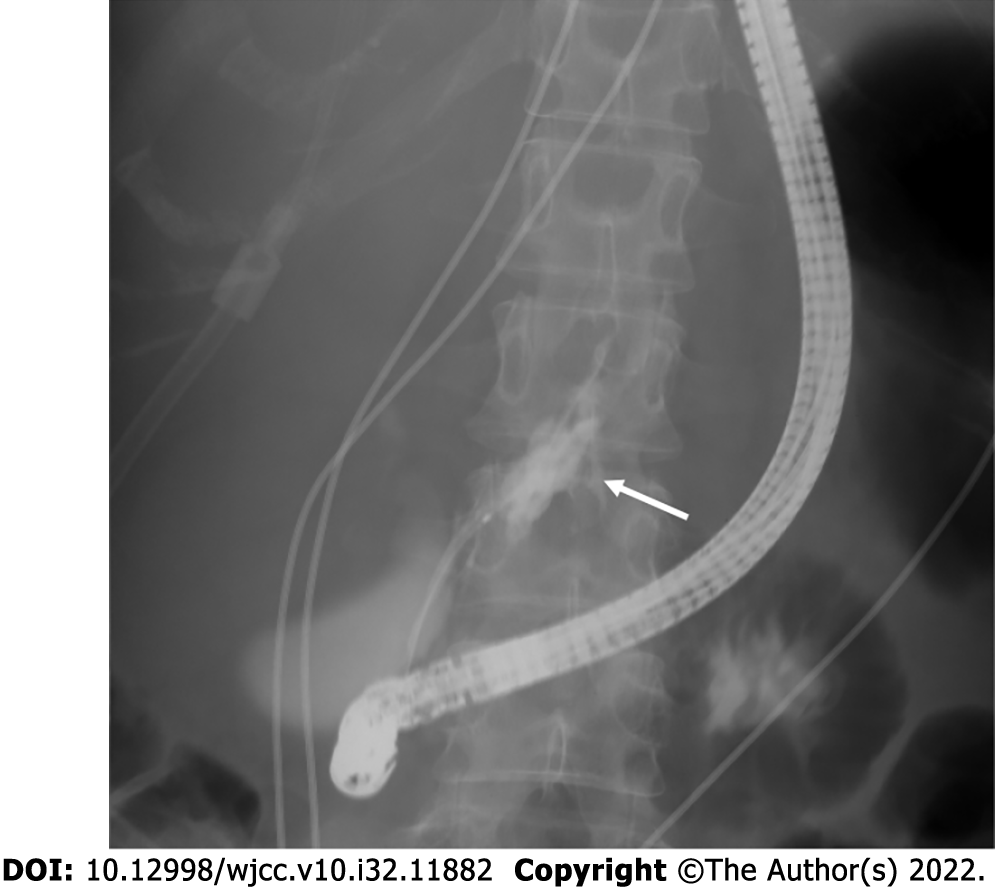
The CT demonstrated pancreatitis with pseudocysts around the pancreas (Figure 2A) extending to the mediastinum (Figure 2B). Thrombotic vasculitis of the brachiocephalic to left brachial vein was also observed (Figure 2C), which was considered to be the cause of elbow pain. MPP was not seen around the brachiocephalic vein; however, it was compressed between the sternal bone and brachial artery (Figure 3). A pancreatic fistula was found in the head of the pancreas by endoscopic retrograde cholangiopancreatography (ERCP), so a pancreatic cyst drainage tube via the duodenum was placed in the pseudocyst (Figure 4).
During the next CT scan, the amylase concentration was 1108 U/L; therefore, a final diagnosis of brachiocephalic to left brachial vein thrombotic vasculitis with pancreatic pseudocysts in adjacent tissues of the pancreas and mediastinum was made.
The pseudocyst around the head of the pancreas was drained with the tube inserted by ERCP. The culture of the cyst contents was positive for E. coli infection. MRI of MPP did not show any infection; thus, the patient was followed up with conservative treatment with antibiotics. MPP was followed up with conservative treatment with antibiotics for 32 d along with intravenous administration of heparin with 12000 U/day for 25 d and octreotide acetate for 24 d. The activated partial thromboplastin time was maintained at 38–42 s.
The clinical symptoms, imaging findings, and inflammatory reactions of acute pancreatitis were resolved, the MPPs shrunk, and the venous thrombi remained but shrunk. Table 1 summarizes the clinical course of the patient.
| Time point | Remarks |
| July 24, 2017 | Redness of the bilateral auricles |
| July 27, 2017 | Antibiotics administration at a clinician |
| August 10, 2017 | Referred to our hospital |
| August 18, 2017 | Non–contrast-enhanced chest to abdominal CT withoutsignificant findings |
| August 20, 2017 | Biopsy for auricular cartilage |
| August 21, 2017 | Contrast-enhanced head and neck MRI with presenting figures |
| Prednisolone administration was started | |
| September 1, 2017 | Symptoms and laboratory abnormality improved remarkably |
This is the first case report presenting a patient with brachiocephalic vein accompanying MPPs. MPPs are rarely found as a complication of acute pancreatitis, as first described by Clauss et al[9]. Case reports about MPPs have been accumulated in recent years; however, to the best of our knowledge, there was no report on patients with a chief complaint of left arm tenderness derived from brachiocephalic to brachial vein thrombotic vasculitis. We could find a case report of a patient with multiple ascending aortic mural thrombi and acute necrotizing mediastinitis secondary to acute pancreatitis[7]. The patient had acute pancreatitis with extended inflammation to the mediastinum, resulting in aortitis with thrombi. In contrast, in our case, the MPPs did not reach the brachiocephalic vein, so a direct inflammatory infiltration from the MPPs cannot be assumed.
There were case series reports of patients with splanchnic vein thrombosis and acute pancreatitis[10-12]. It was reported that the coagulopathy might have an effect on forming thrombi. In addition, the compression by MPPs to adjacent veins resulted in flow deficiency and coagulation[13,14]. The possible causes of thrombosis in the brachiocephalic vein, in this case, were as follows: Brachiocephalic vein stenosis due to compression of the brachiocephalic vein between the sternal body and aortic branches, resulting in systemic coagulopathy due to MPPs for an undetermined period, and edematous changes in the mediastinal tissues. Because the onset of pancreatitis in this patient is unknown, it is not clear whether systemic inflammation affected coagulopathy. Based on the presence of coagulopathy due to systemic inflammation, anatomical stenosis would be an additional cause of thrombotic vasculitis.
Panniculitis is a presenting type of pancreatic lesions derived from pancreatic enzyme migration into the systemic circulation that occur in systemic cutaneous inflammation[15]. In patients with subcutaneous inflammatory changes and pancreatitis, panniculitis should be considered; however, because panniculitis usually occurs systemically, our case was suspected to have cellulitis on the left upper arm. The original symptoms of our case were associated with brachiocephalic to left brachial vein thrombosis, so the diagnosis of our case cannot be panniculitis derived from pancreatic enzyme leakage. The D-dimer level of the patient was elevated to 12.7 µg/mL. Thus, an evaluation for deep vein thrombosis might be considered, as the patient suffered from severe inflammatory disease with elevated D-dimer count.
In this case, the MPP was detected because the dermatologist who examined the patient considered the inflammatory change to be relatively worse than the severity of the left arm cellulitis. This is an instructive case demonstrating that it is essential to perform a workup study in patients with suspicious or undetermined unexplainable data.
Herein, we report a case of a patient with pancreatitis with an undetermined onset, respiratory syndrome for a few months, and thrombotic vasculitis in the brachiocephalic vein mimicking left arm cellulitis. Long-term pancreatitis might cause systemic coagulopathy that resulted in brachiocephalic vein thrombosis. Deep vein thrombosis should be kept in mind when treating patients with severe inflammatory disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: The Japanese Society of Radiology.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Reviewer: Li G, China; Sade R, Turkey S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Rose EA, Haider M, Yang SK, Telmos AJ. Mediastinal extension of a pancreatic pseudocyst. Am J Gastroenterol. 2000;95:3638-3639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Cameron JR. Parental treatment, children's temperament, and the risk of childhood behavioral problems: 2. Initial temperament, parental attitudes, and the incidence and form of behavioral problems. Am J Orthopsychiatry. 1978;48:140-147. [PubMed] [DOI] [Full Text] |
| 3. | Gupta R, Munoz JC, Garg P, Masri G, Nahman NS Jr, Lambiase LR. Mediastinal pancreatic pseudocyst--a case report and review of the literature. MedGenMed. 2007;9:8. [PubMed] |
| 4. | Andrén-Sandberg A, Dervenis C. Pancreatic pseudocysts in the 21st century. Part I: classification, pathophysiology, anatomic considerations and treatment. JOP. 2004;5:8-24. [PubMed] |
| 5. | Tajima Y, Fukuda K, Tsuneoka N, Tsutsumi R, Kuroki T, Onizuka S, Furui J, Yamanaka S, Makimoto Y, Tsuchiya R, Kanematsu T. Demonstration of a pancreaticopleural fistula with magnetic resonance cholangiopancreatography. Am J Surg. 2004;187:741-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Laureano A, Mestre T, Ricardo L, Rodrigues AM, Cardoso J. Pancreatic panniculitis - a cutaneous manifestation of acute pancreatitis. J Dermatol Case Rep. 2014;8:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Chong BK, Yun JK, Kim JB, Park DH. Multiple Ascending Aortic Mural Thrombi and Acute Necrotizing Mediastinitis Secondary to Acute Pancreatitis. Korean J Thorac Cardiovasc Surg. 2016;49:401-404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Liao CY, Huang SC, Lin CH, Wang CC, Liu MY, Ben RJ, Kuo WH, Lee CC. Successful resolution of symmetrical peripheral gangrene after severe acute pancreatitis: a case report. J Med Case Rep. 2015;9:213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Clauss RH, Wilson DW. Pancreatic pseudocyst of the mediastinum. J Thorac Surg. 1958;35:795-801. [PubMed] |
| 10. | Nawacki Ł, Matykiewicz J, Stochmal E, Głuszek S. Splanchnic Vein Thrombosis in Acute Pancreatitis and Its Consequences. Clin Appl Thromb Hemost. 2021;27:10760296211010260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Pancreas Study Group; Chinese Society of Gastroenterology; Chinese Medical Association. Practice guidance for diagnosis and treatment of pancreatitis-related splanchnic vein thrombosis (Shenyang, 2020). J Dig Dis. 2021;22:2-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | Primignani M. Pancreatitis-related splanchnic vein thrombosis: What role, what warnings for anticoagulation therapy? J Dig Dis. 2021;22:122-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Ahmed SU, Rana SS, Ahluwalia J, Varma N, Sharma R, Gupta R, Kang M. Role of thrombophilia in splanchnic venous thrombosis in acute pancreatitis. Ann Gastroenterol. 2018;31:371-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Rebours V, Boudaoud L, Vullierme MP, Vidaud D, Condat B, Hentic O, Maire F, Hammel P, Ruszniewski P, Lévy P. Extrahepatic portal venous system thrombosis in recurrent acute and chronic alcoholic pancreatitis is caused by local inflammation and not thrombophilia. Am J Gastroenterol. 2012;107:1579-1585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Poelman SM, Nguyen K. Pancreatic panniculitis associated with acinar cell pancreatic carcinoma. J Cutan Med Surg. 2008;12:38-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |