Published online Sep 16, 2022. doi: 10.12998/wjcc.v10.i26.9310
Peer-review started: August 6, 2021
First decision: November 6, 2021
Revised: November 10, 2021
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: September 16, 2022
Processing time: 391 Days and 6.5 Hours
Acute carotid stent thrombosis (ACST) is a rare but devastating complication in the carotid artery stenting (CAS) procedure. The aim of this article is to report a case and review cases of ACST reported in the literature, and investigate risk factors and management strategies for ACST.
We reviewed the treatment process of a patient with ACST after CAS. Then multiple databases were systematically searched to identify studies reporting ACST from 2005 to 2020. The demographic data, risk factors, treatment strategies, and prognosis were extracted and analyzed.
The reason for ACST is multifactorial. Proper patient selection, normative anti-platelet treatment, and perfect technical detail may decrease the incidence of ACST. Several treatment strategies such as thrombolysis, mechanical throm
Core Tip: The reason for acute carotid stent thrombosis (ACST) is multifactorial. Proper patient selection, normative anti-platelet treatment, and perfect technical detail may decrease the incidence of ACST. Several treatment strategies such as thrombolysis, mechanical thrombectomy, and open surgery may be options for the treatment of ACST. Limited data have shown carotid endarterectomy is effective with favorable results.
- Citation: Zhang JB, Fan XQ, Chen J, Liu P, Ye ZD. Acute carotid stent thrombosis: A case report and literature review . World J Clin Cases 2022; 10(26): 9310-9317
- URL: https://www.wjgnet.com/2307-8960/full/v10/i26/9310.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i26.9310
Carotid artery stenting (CAS) has emerged as an alternative to carotid endarterectomy (CEA) in treating carotid artery stenosis[1]. With the development of instruments and techniques, CAS has become increasingly used. The most common complications for CAS are thromboembolic events. Acute carotid stent thrombosis (ACST) refers to thrombus formation in the carotid artery during or after the CAS procedure, which is rare but can be devastating[2]. The etiology, treatment strategy, and prognosis are not well reported in the past.
In the current study, we reported the treatment process of a case with ACST caused by a stent cutting plaque. The patient gave consent to use his medical record for educational and publication purposes. Then we reviewed the current published literature reporting cases of ACST to investigate the etiologies, management strategies, and prognosis for ACST.
A 65-year-old man visited the cardiovascular surgery department of our hospital for dizziness and transient left limb weakness for 2 mo. The patient was also diagnosed with abdominal aortic aneurysm (AAA) for 1 mo.
Two months prior, the patient began to experience dizziness and transient left limb weakness without obvious inducement, which subsided within hours. The patient went to the local hospital to seek medical advice. The doctors found that the patient had right carotid artery stenosis and AAA.
The patient denied any history of hypertension, diabetes mellitus, or coronary atherosclerotic disease but had a history of smoking for more than 40 years (20 cigarettes/d).
The patient denied any history of genetic disease and familial aggregation disease history.
Abdominal palpation showed the presence of pulsatile mass, and auscultation showed murmur in the right carotid artery.
The blood routine test, liver function, renal function, coagulation function, and myocardial infarction index were all in normal range.
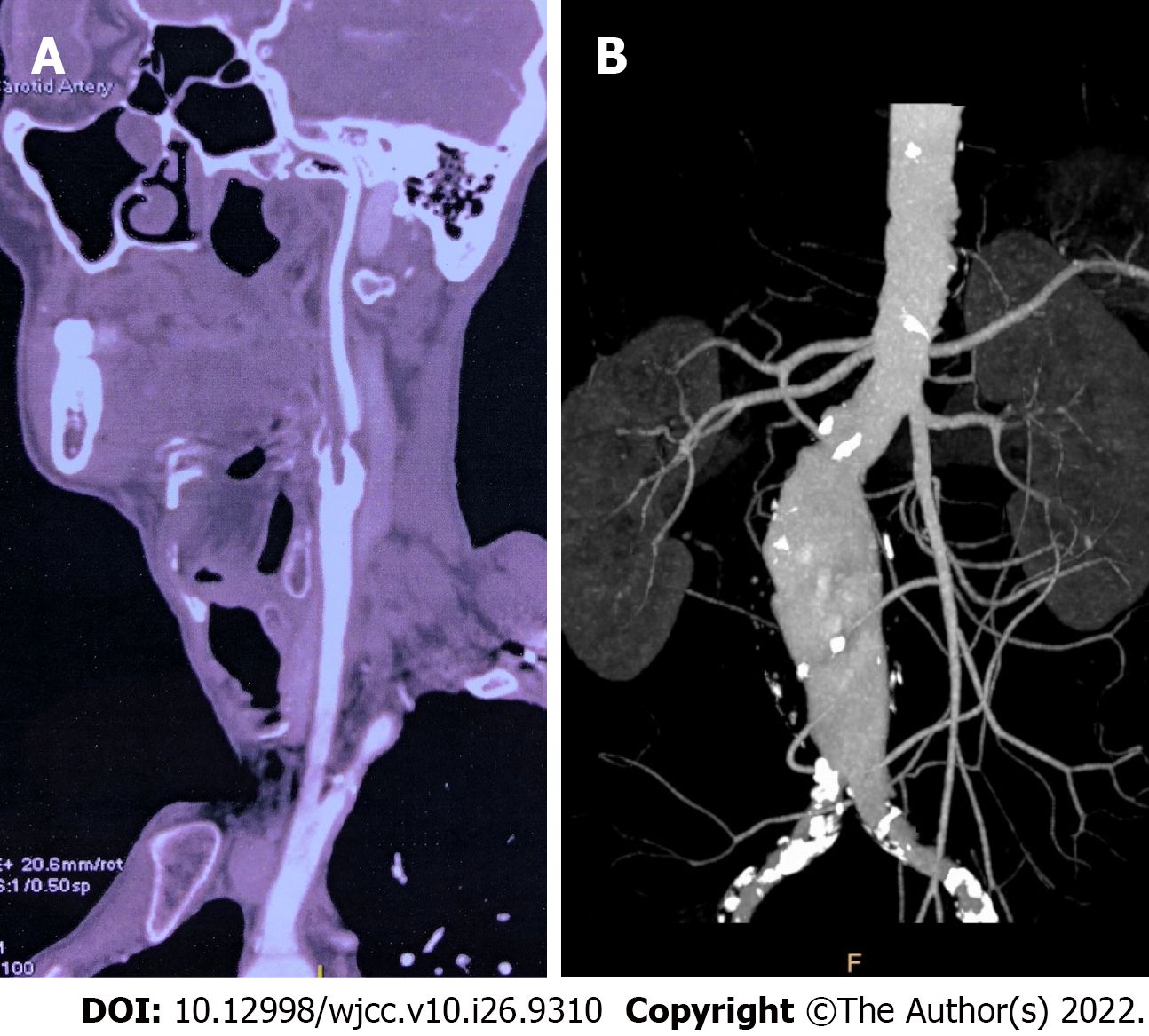
Carotid ultrasonography and computed tomography angiography (CTA) showed 95% stenosis of the right internal carotid artery (ICA). Aortic CTA showed infrarenal AAA with a maximum diameter of 53 mm and mural thrombus formation (Figure 1).
The patient was diagnosed with combined symptomatic ICA stenosis and infrarenal AAA.
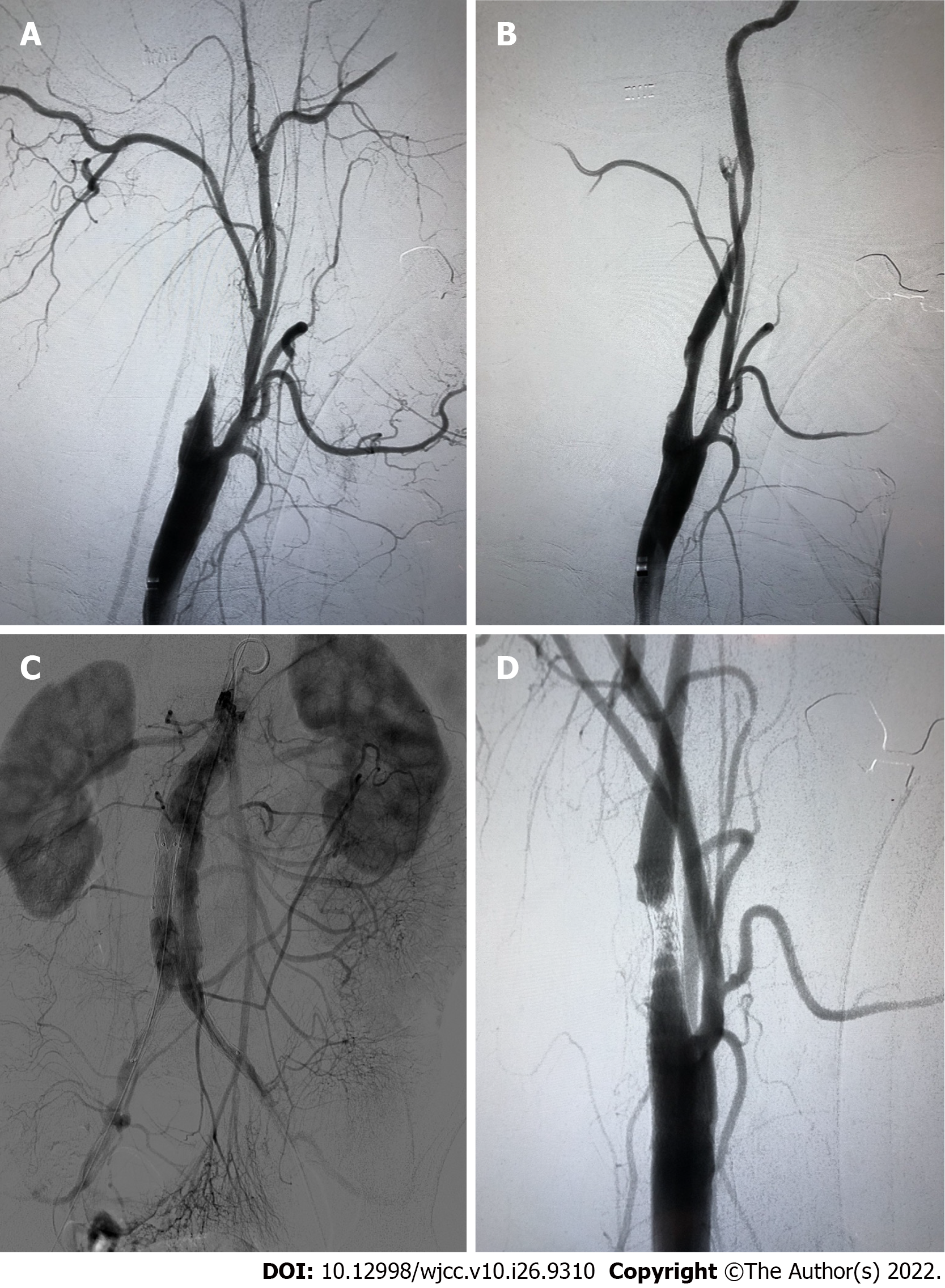
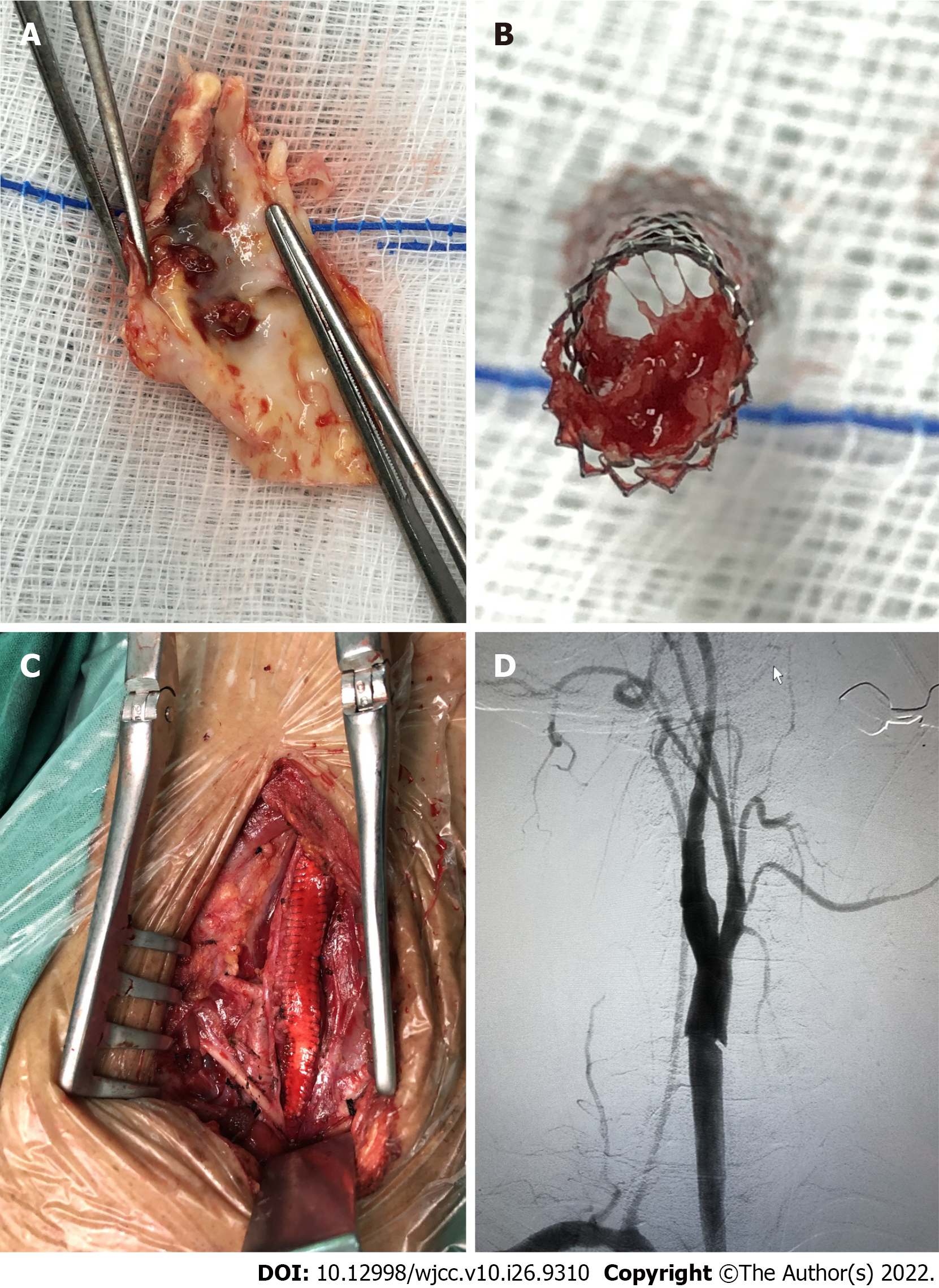
For ICA stenosis, pre-operative CTA showed that the plaque was relatively soft with less calcification. According to plaque morphology (the PLAC Scale) on CTA[3,4], soft plaque and lower grade of calcification were associated with a better stenting outcome. Due to transient ischemia attack (TIA) 2 mo prior, we preferred to carry out CAS in the patient. For the combined infrarenal AAA, it is uncomplicated with enough landing zone. The estimated time for endovascular aneurysm repair (EVAR) procedure is not long. So we planned to perform right CAS and standard EVAR simultaneously. Before the procedure, 100 mg aspirin and 75 mg clopidogrel daily were given for 5 d. The procedure was performed under general anesthesia. During the procedure, the activated clotting time was 302 s after administration of 6000 IU unfractionated heparin. CTA showed 95% stenosis at the proximal part of the right ICA. Then pre-dilatation with 4.0-20 mm and 5.0-20 mm balloons (AVIATOR; Abbott Laboratories, Chicago, IL, United States) was performed sequentially, under the protection of an embolism protection device (EPD, Emboshield NAV6; Abbott). A taper stent (9-7 mm 40 mm, XACT Carotid Stent System; Abbott) was implanted. Post-procedure angiography showed contrast agent retention in the stent, and the distal of ICA was obliterated. ICA spasm and plaque debris-occluded EPD were suspected. Then we gave the patient 30 mg papaverine and retrieved the EPD. Subsequent angiography showed the ICA was patent with 40% residual stenosis because of the spasm. After another 3000 IU unfractionated heparin was administered, standard EVAR was performed with a stent graft system (2316170, Endurant AAA Stent Graft System; Medtronic, Minneapolis, MN, United States) that was implanted smoothly. After EVAR, we performed another carotid angiography to evaluate whether the ICA spasm was alleviated. However, we found acute thrombus formation in the stent (Figure 2). Due to concerns about thrombus migration and distal embolization, we did not try to aspirate the thrombus through the catheter. Instead, we performed CEA immediately to remove the carotid stent and thrombus. Then we carried out the standard CEA procedure with a shunt (Braun; Aesculap, Inc., Kelaryes, PA, United States) implantation and patch (Edwards Lifesciences, Irvine, CA, United states) angioplasty. During the CEA procedure, we found that the stent was occluded by the plaque debris (Figure 3).
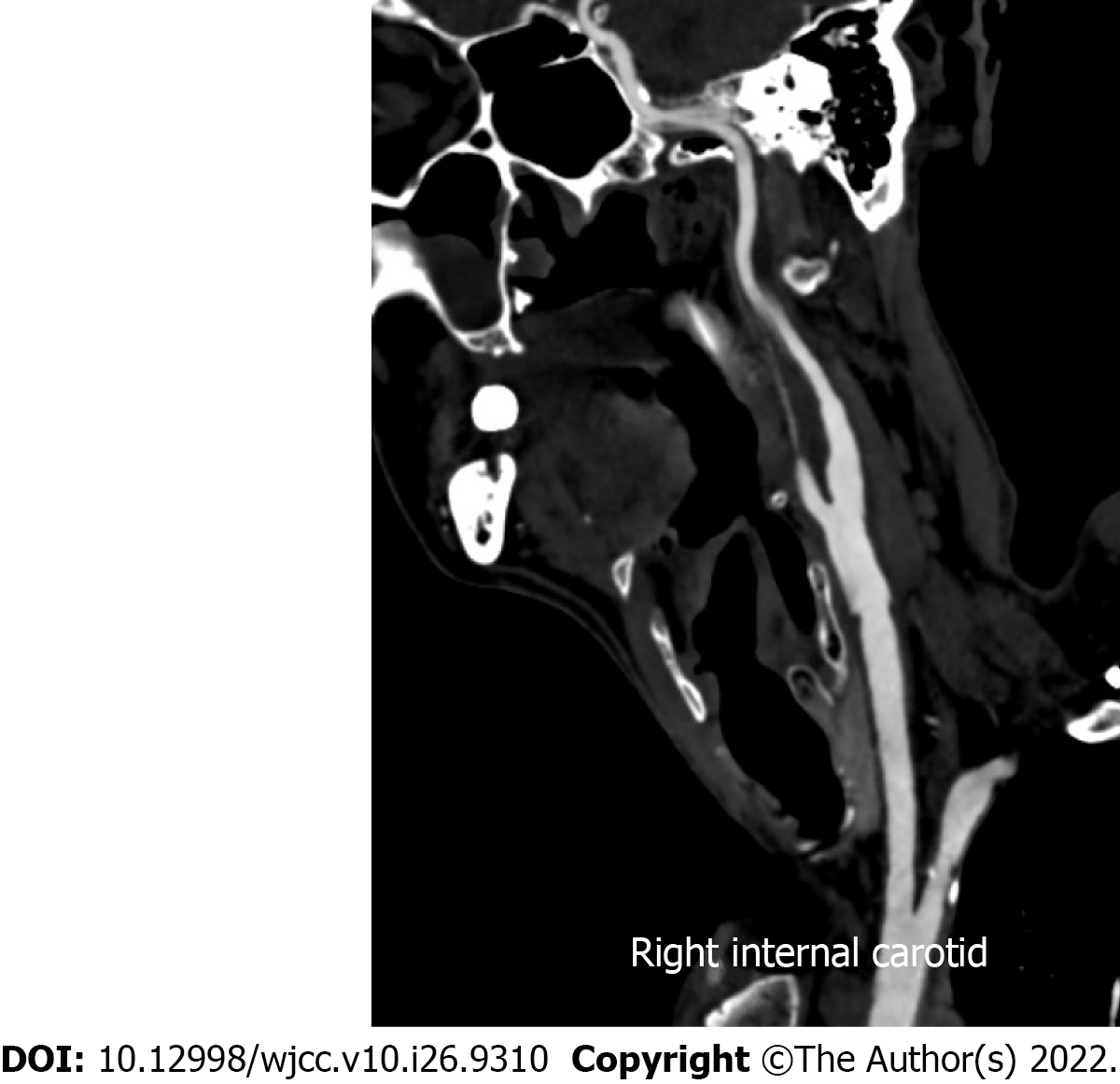
The patient was conscious and his limbs moved freely after awaking from general anesthesia after CEA. The patient also had no neurological deficit at the 1-year follow-up (Figure 4).
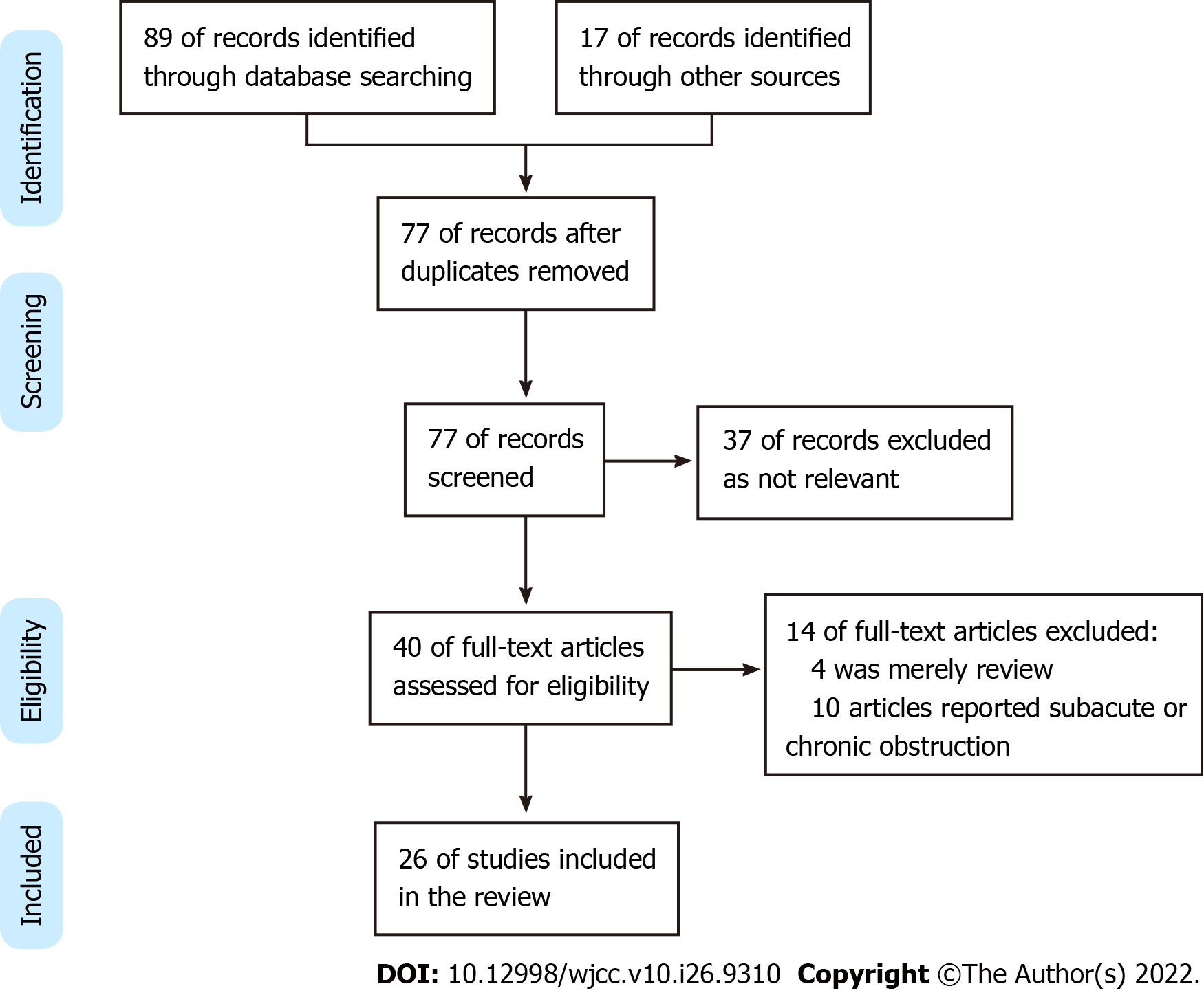
A systematic literature search using PubMed, MEDLINE, EMBASE, CNKI, Google Scholar, and Cochrane databases was conducted for all relevant published papers reporting cases of ACST. Finally, 26 articles with 43 ACST met the inclusion criteria (Figure 5)[5-30].
CAS has become an alternative treatment to CEA for carotid artery stenosis. The most common complication for CAS is peri-procedure stroke[31]. The incidence of ACST is rare, which is reportedly 0.5%-2%[21]. Though rare, delayed recanalization of ICA or inappropriate management may lead to devastating consequences.
The etiology of ACST is multifactorial. Inadequate, ceasation, or resistance of anti-platelet agent is an important reason. The incidence of acetylsalicylic acid resistance is 5.5%-45% and the incidence of clopidogrel resistance is 4%-44%[12]. Pre-operative evaluation of sensitivity to anti-platelet agent is helpful. Light transmittance aggregometry is the golden standard to measure platelet aggregation.
Hypercoagulable state including cancer history, protein C deficiency, taking oral contraceptives, heparin-induced thrombocytopenia, and thalassemia are also common. For these patients, additional anti-coagulative agent may be necessary. Local factors such as plaque protrusion in stent and debris occluding the EPD occur occasionally. Embolic events occurring in atrial fibrillation patients accidently after CAS is rare[5]. Iatrogenic injury, such as balloon burst during the procedure, should be avoided[22].
In our patient, no evidence of a hypercoagulable state was discovered. Pre-operative dual anti-platelet agent was given for 5 d. During the CAS and EVAR procedure, we gave the patient sufficient unfractionated heparin and the activated clotting time was suitable for interventional therapy. Stent cutting plaque could be found during CEA. We believe the initiating factor of platelet aggregation was the exposure of thrombogenic material after plaque rupture[13] in our case. The presence of TIA indicated that the plaque was not stable, but we did not attach enough importance to it and underestimated the risk of CAS. From our present case, we want to emphasize again that pre-operative plaque evaluation is very important for decrease the rate of plaque rupture and subsequent ACST. Vulnerable or ulcerated plaque is more suitable for CEA instead of CAS. We did not evaluate whether the patient was resistant to aspirin or clopidogrel.
The present procedure was performed under general anesthesia for possible breath control during EVAR. This may decrease the patient’s blood pressure and prolong operation time, which is another hidden reason for ACST. General anesthesia also made it impossible to perceive the patient’s neurological deficit in time. For CAS procedure, local anesthesia with close intra-operative neurologic status monitoring is more suitable.
The best treatment strategy for ACST is controversial. Multiple methods have been reported, all without large series experience. Catheter-directed thrombolysis with alteplase, urokinase, and tenecteplase is mostly used. Most of the patients achieved successful complete or partial recanalization. Administration of abciximab intravenously or intra-arterially is also reportedly effective[18,28]. ‘Facilitated thrombolysis’ consisting of reduced dosage of de-thrombosis (abciximab) and fibrinolysis (alteplase) may be beneficial with respect to both arterial recanalization and suppression of recurrent thrombosis[29].
Other endovascular management strategies include catheter thrombo-aspiration, balloon angioplasty, and subsequent stent implantation[5,10,13,16]. These methods are helpful for carotid revascularization, but balloon angioplasty and subsequent stent implantation may cause extra intima injury or damage stent structure.
The reported open surgical treatments include superficial temporal artery to middle cerebral artery (STA-MCA) bypass and CEA. STA-MCA bypass is considered second-line treatment, which may be beneficial to patients with ACST for whom intra-arterial thrombolysis is not available[14]. CEA with thorough stent removal and thrombus have shown favorable results[24]. We believe that urgent stent and thrombus removal should be performed for patients with plaque rupture and ACST to prevent thrombus extension and subsequent cerebral infarction. Unlike traditional CEA, extended exposure of carotid artery is required both proximally and distally in these situations. The ICA should be clamped first to prevent thrombosis dislocation when dissected the carotid artery. Fogarty catheter may be necessary to pull out the thrombus in distal ICA. Another reason that we chose CEA is that we did not have enough experience in endovascular treatment for ACST.
Mechanical thrombectomy using the Penumbra 4Max aspiration catheter and rheolytic thrombectomy system is also reportedly effective. Limited experience has shown that mechanical thrombectomy can effectively recanalize ICA with ACST, without the irritation of balloon angioplasty or stent deployment. The hemorrhagic risk is lower than thrombolysis. One advantage is that the patient can easily be switched to other treatment methods if necessary[21,28,30].
The reason for ACST is multifactorial. Proper patient selection, normative anti-platelet treatment, and perfect technical detail may decrease the incidence of ACST. Several treatment strategies such as thrombolysis, mechanical thrombectomy, and open surgery may be treatment options for ACST. Limited data have shown that carotid endarterectomy is effective with favorable results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozdemir HI, Turkey S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Brott TG, Howard G, Roubin GS, Meschia JF, Mackey A, Brooks W, Moore WS, Hill MD, Mantese VA, Clark WM, Timaran CH, Heck D, Leimgruber PP, Sheffet AJ, Howard VJ, Chaturvedi S, Lal BK, Voeks JH, Hobson RW 2nd; CREST Investigators. Long-Term Results of Stenting versus Endarterectomy for Carotid-Artery Stenosis. N Engl J Med. 2016;374:1021-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 515] [Article Influence: 57.2] [Reference Citation Analysis (0)] |
| 2. | Nicosia A, Nikas D, Castriota F, Biamino G, Cao P, Cremonesi A, Mathias K, Moussa I, Hopkins LN, Setacci C, Sievert H, Reimers B. Classification for carotid artery stenting complications: manifestation, management, and prevention. J Endovasc Ther. 2010;17:275-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Pelz DM, Lownie SP, Lee DH, Boulton MR. Plaque morphology (the PLAC Scale) on CT angiography: predicting long-term anatomical success of primary carotid stenting. J Neurosurg. 2015;123:856-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Scullen T, Mathkour M, Carr C, Wang A, Amenta PS, Nerva JD, Dumont AS. Anatomical Considerations for Endovascular Intervention for Extracranial Carotid Disease: A Review of the Literature and Recommended Guidelines. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Moulakakis KG, Kakisis J, Tsivgoulis G, Zymvragoudakis V, Spiliopoulos S, Lazaris A, Sfyroeras GS, Mylonas SN, Vasdekis SN, Geroulakos G, Brountzos EN. Acute Early Carotid Stent Thrombosis: A Case Series. Ann Vasc Surg. 2017;45:69-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Sorkin GC, Dumont TM, Mokin M, Eller JL, Natarajan SK, Levy EI, Siddiqui AH. Hyperacute Carotid Stent Thrombosis During Emergent Revascularization Treated with Intraarterial Eptifibatide After Systemic Administration of Recombinant Tissue Plasminogen Activator. J Vasc Interv Neurol. 2015;8:50-55. [PubMed] |
| 7. | Setacci C, de Donato G, Setacci F, Chisci E, Cappelli A, Pieraccini M, Castriota F, Cremonesi A. Surgical management of acute carotid thrombosis after carotid stenting: a report of three cases. J Vasc Surg. 2005;42:993-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Hamann GF, Liebetrau M, Pfefferkorn T, Heiss MM. Successful systemic thrombolysis for carotid stent thrombosis. Eur Neurol. 2002;48:37-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Chaturvedi S, Sohrab S, Tselis A. Carotid stent thrombosis: report of 2 fatal cases. Stroke. 2001;32:2700-2702. [PubMed] |
| 10. | Murray NM, Wolman DN, Marks M, Dodd R, Do HM, Lee JT, Heit JJ. Endovascular Treatment of Acute Carotid Stent Occlusion: Aspiration Thrombectomy and Angioplasty. Cureus. 2020;12:e7997. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Toljan K, Jovanović I, Starčević K, Ljevak J, Blažević N, Radoš M, Poljaković Z. Acute Carotid Stent Thrombosis in an Ultrarapid Clopidogrel Metabolizer: Case Report and Literature Review. Vasc Endovascular Surg. 2019;53:602-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Köklü E, Yüksel İÖ, Bayar N, Arslan Ş. Is Acute Carotid Artery Stent Thrombosis an Avoidable Complication? J Stroke Cerebrovasc Dis. 2015;24:2219-2222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Köklü E, Arslan Ş, Yüksel İÖ, Bayar N, Koç P. Acute Carotid Artery Stent Thrombosis Due to Dual Antiplatelet Resistance. Cardiovasc Intervent Radiol. 2015;38:1011-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Choi HJ, Kim ST, Jeong YG, Jeong HW. Superficial temporal artery-middle cerebral artery anastomosis for internal carotid artery occlusion by subacute in-stent thrombosis after carotid artery stenting. J Korean Neurosurg Soc. 2012;52:551-554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Hu W, Wang L, Wang G. Acute In-Stent Thrombosis after Carotid Angioplasty and Stenting: A Case Report and Literature Review. Interv Neurol. 2018;7:265-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Iwamoto Y, Kitano T, Matsubara S, Uno M, Yagita Y. In-stent thrombosis after carotid artery stenting in a patient with protein C deficiency. Neurol Sci. 2018;39:2229-2230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Kanemaru K, Nishiyama Y, Yoshioka H, Satoh K, Hashimoto K, Hanihara M, Horikoshi T, Ozaki Y, Kinouchi H. In-stent thrombosis after carotid artery stenting despite sufficient antiplatelet therapy in a bladder cancer patient. J Stroke Cerebrovasc Dis. 2013;22:1196-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Stotts G, Skinner C, Code C, Lawrie G, Lesiuk H, Lum C. Acute stent occlusion due to heparin induced thrombocytopenia and thrombosis during carotid artery stenting. J Neurointerv Surg. 2012;4:e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Moulakakis KG, Lazaris AM. Emergent Carotid Stent Removal after Carotid Stent Thrombosis. Ann Vasc Surg. 2018;46:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Masuo O, Terada T, Matsuda Y, Ogura M, Tsumoto T, Yamaga H, Itakura T. Successful recanalization by in-stent percutaneous transluminal angioplasty with distal protection for acute carotid stent thrombosis. Neurol Med Chir (Tokyo). 2006;46:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Kim YW, Kang DH, Hwang JH, Park J, Hwang YH, Kim YS. Rescue strategy for acute carotid stent thrombosis during carotid stenting with distal filter protection using forced arterial suction thrombectomy with a reperfusion catheter of the Penumbra System: a technical note. Acta Neurochir (Wien). 2013;155:1583-1588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Iancu A, Grosz C, Lazar A. Acute carotid stent thrombosis: review of the literature and long-term follow-up. Cardiovasc Revasc Med. 2010;11:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Tong FC, Cloft HJ, Joseph GJ, Samuels OB, Dion JE. Abciximab rescue in acute carotid stent thrombosis. AJNR Am J Neuroradiol. 2000;21:1750-1752. [PubMed] |
| 24. | Staudt MD, Mayich MS, Lownie SP. Emergent Carotid Endarterectomy with Open Thrombectomy for Acute Carotid Stent Occlusion. World Neurosurg. 2020;138:52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 25. | Cvjetko I, Đaković Bacalja I, Cvjetko T. Acute Carotid Artery Stent Thrombosis. Cardiovasc Intervent Radiol. 2018;41:355-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Markatis F, Petrosyan A, Abdulamit T, Bergeron P. Acute carotid stent thrombosis: a case of surgical revascularization and review of treatment options. Vascular. 2012;20:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Seo KD, Lee KO, Kim DJ, Lee KY. Rescue use of tirofiban for acute carotid in-stent thrombosis. Yonsei Med J. 2008;49:163-166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Munich S, Moftakhar R, Lopes D. Recanalization of acute carotid stent occlusion using Penumbra 4Max aspiration catheter: technical report and review of rescue strategies for acute carotid stent occlusion. J Neurointerv Surg. 2014;6:e42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Steiner-Böker S, Cejna M, Nasel C, Minar E, Kopp CW. Successful revascularization of acute carotid stent thrombosis by facilitated thrombolysis. AJNR Am J Neuroradiol. 2004;25:1411-1413. [PubMed] |
| 30. | Bush RL, Bhama JK, Lin PH, Lumsden AB. Transient ischemic attack due to early carotid stent thrombosis: successful rescue with rheolytic thrombectomy and systemic abciximab. J Endovasc Ther. 2003;10:870-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Lamanna A, Maingard J, Barras CD, Kok HK, Handelman G, Chandra RV, Thijs V, Brooks DM, Asadi H. Carotid artery stenting: Current state of evidence and future directions. Acta Neurol Scand. 2019;139:318-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |