Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8474
Peer-review started: March 23, 2022
First decision: May 30, 2022
Revised: June 8, 2022
Accepted: July 20, 2022
Article in press: July 20, 2022
Published online: August 26, 2022
Processing time: 145 Days and 23.9 Hours
In the last few years, much more information on the anterolateral complex of the knee has become available. It has now been demonstrated how it works in conjunction with the anterior cruciate ligament (ACL) controlling anterolateral rotatory laxity. Biomechanical studies have shown that the anterolateral complex (ALC) has a role as a secondary stabilizer to the ACL in opposing anterior tibial translation and internal tibial rotation. It is of utmost importance that surgeons comprehend the intricate anatomy of the entire anterolateral aspect of the knee. Although most studies have only focused on the anterolateral ligament (ALL), the ALC of the knee consists of a functional unit formed by the layers of the iliotibial band combined with the anterolateral joint capsule. Considerable interest has also been given to imaging evaluation using magnetic resonance and several studies have targeted the evaluation of the ALC in the setting of ACL injury. Results are inconsistent with a lack of association between magnetic resonance imaging evidence of injury and clinical findings. Isolated ACL reconstruction may not always reestablish knee rotatory stability in patients with associated ALC injury. In such cases, additional procedures, such as anterolateral reconstruction or lateral tenodesis, may be indicated. There are several techniques available for ALL reconstruction. Graft options include the iliotibial band, gracilis or semi
Core Tip: Although research on anterolateral ligament (ALL) has increased considerably in recent years, some debate remains regarding its anatomy and further refinement is still ongoing. Biomechanical studies have revealed that anterolateral structures contribute significantly to rotational stability of the knee and should be accounted for in the setting of an anterior cruciate ligament (ACL) injury. Surgical indications for ALL reconstruction are not currently evidence-based and the ideal graft type and fixation have not yet been determined. Further clinical research remains to be conducted to determine the most appropriate scenarios for augmentation of a primary ACL reconstruction with an anterolateral procedure to enhance patient outcomes.
- Citation: Garcia-Mansilla I, Zicaro JP, Martinez EF, Astoul J, Yacuzzi C, Costa-Paz M. Overview of the anterolateral complex of the knee. World J Clin Cases 2022; 10(24): 8474-8481
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8474.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8474
The initial description of the anterolateral complex of the knee is attributed to various authors, and the anatomical details of the so-called anterolateral ligament of the knee have changed according to the historical context of each century. In 1752, Weitbrecht was the first to refer to a series of fibers that reinforced the lateral joint capsule of the knee and that, according to his observation, gave support to the external meniscus. One hundred years later, Henle described a group of fibers anterior to the external collateral ligament that inserted into the edge of the external meniscus, and that reinforced the joint capsule. The first anatomo-clinical approach was advanced by Paul Segond who described an avulsion fracture of the anterolateral portion of the proximal tibia associated with this ligament. Through a series of cadaveric dissections, he characterized the fibers of the ligament as a stringy, beaded, tough band that, according to his observation, tightened upon excessive internal rotation of the knee. Since then, the ligament has taken different names in the literature and numerous and non-specific descriptions have been made of the ligamentous capsule structures of the anterolateral region of the knee[1,2].
More than a century had to pass until the landmark works of Claes et al[3], Vincent et al[4] and Helito et al[5] when the term anterolateral ligament of the knee began to spread. From that time on, there has been a great deal of dispute surrounding the presence of the LLA and its possible role in the control of anterolateral rotational instability (ALRI) following anterior cruciate ligament (ACL) injury. Great emphasis has been given to a better understanding of these structures, including their anatomy, biomechanics, injury patterns, and the optimal strategies to treat any rotational laxity of the knee resulting from damage to these structures[6]. Lateral extra-articular tenodesis has re-emerged in popularity and several ALL reconstruction techniques have been developed in the attempt to lower the failure rate following ACL reconstruction[7-9]. The aim of this review is to outline the latest literature findings on the anatomy of the anterolateral complex, biomechanical findings, treatment of anterolateral lesions, and ALL reconstruction techniques. It is intended to provide information to readers on the most current approaches to help enhance patient outcomes following an ACL injury and subsequent reconstruction.
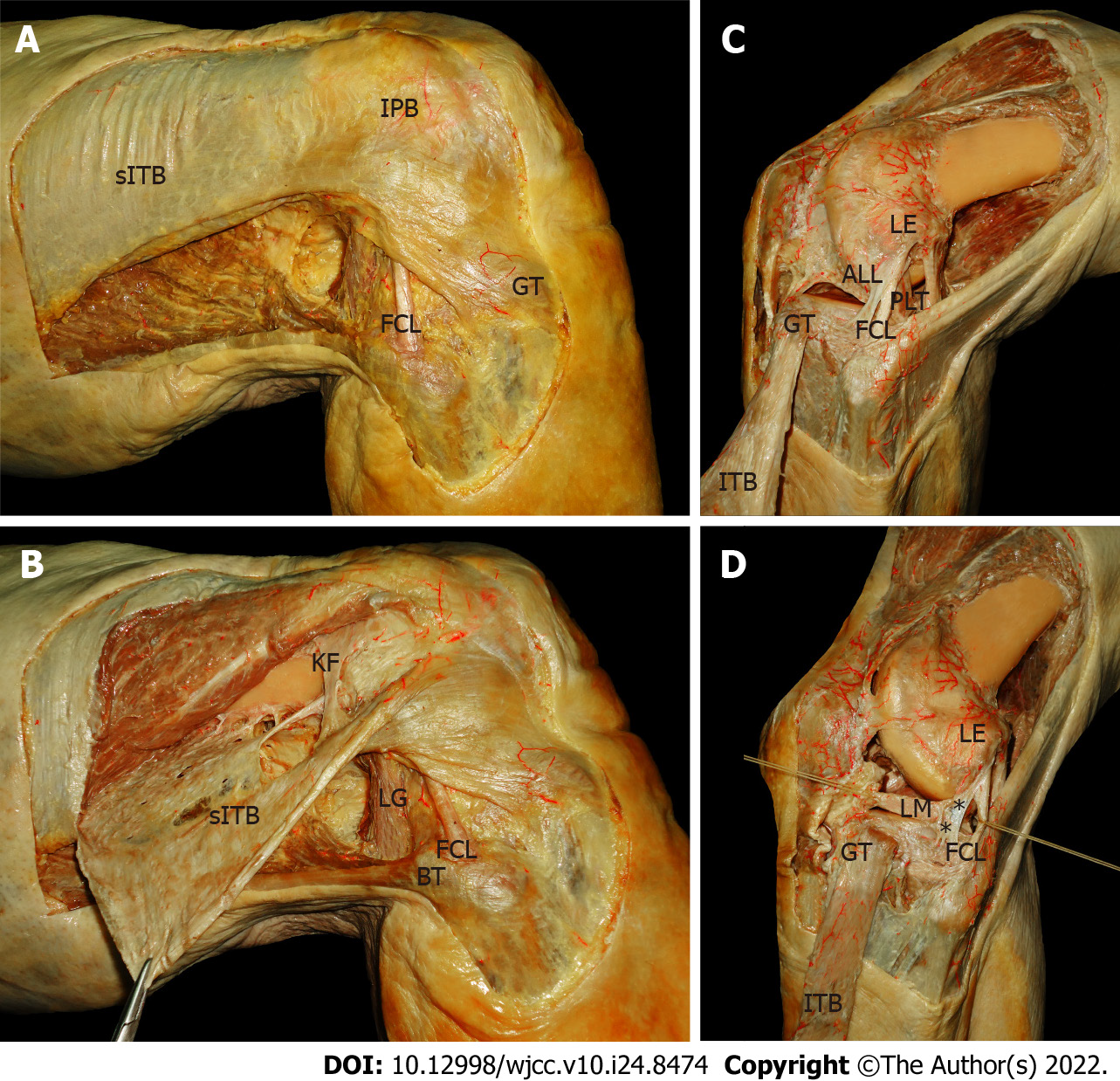
The complex ligamentous capsule anatomy of the anterolateral region of the knee is given by the relative and multiplanar position adopted by its bony parts. To distinguish the anatomy of the anterolateral ligament, it is necessary to understand the three-dimensional arrangement of the iliotibial band. In this anatomical complex, which has been widely described, the following layers can be recognized: Superficial layer of the reflected iliotibial band (sITB) (Figure 1A): It is found immediately deep to the subcutaneous cellular tissue and superficial to the vastus lateralis, easily identifiable by its pearly white color. Its main insertion on Gerdy's tubercle is distinguished distally. Its most anterior fibers are curved distally and insert on the lateral surface of the patella and the patellar tendon (iliopatellar band). Middle layer of the ITB (mITB): Made up of the patellofemoral ligament and the fascia of the quadriceps femoris. Its fibers, contrary to the vertical arrangement of the first layer, run obliquely from proximal and lateral to distal and medial. Deep layer of the ITB (dITB) (Figure 1B): It is localized posterior to the superficial layer. It is inserted into the distal femur, from its metaphyseal portion to the supracondylar area through the so-called Kaplan fibers. These fibers arrange transversely to the femur, which form the deep layer of the iliotibial band and, together with the superficial portion, have an important role in knee stability.
The Capsulo-osseous Layer of the ITB and the anterolateral capsule. There is still considerable controversy surrounding the terminology of the joint capsule that underlies the deepest layer of the ITB. Some authors proposed a capsular-osseous layer and described it as a medial retaining wall of the deepest layer of the ITB. Distally, the fibers run just proximal to Gerdy's tubercle, inserting posterior to the convergence between the superficial and deep layers of the iliotibial band[10]. The lateral joint capsule comprises a superficial layer and a deep layer, based on their relation with respect to the lateral collateral ligament (LCL). These layers converge anterior to the LCL. Hughston et al[1] divided the deep capsule into three parts: an anterior layer (of minor importance due to its thickness and negligible insertions), a posterior layer (made up of the posterolateral arcuate complex) and an intermediate layer called the “mid-third lateral capsular ligament” (a capsular thickening with distinct femoral and tibial bony insertions). The latter also has a firm attachment to the lateral meniscus. These fibers form the meniscofemoral and meniscotibial ligaments, also known as the coronary ligament[11].
All these descriptions overlap with those of the anterolateral ligament of the knee, and can be understood as the same structure[11-13]. In relation to its arrangement, its direction is from proximal and posterior to distal and anterior, inserted at the lateral epicondyle of the femur and the lateral articular margin of the external tibial condyle (Figure 1C). It is related to the lateral meniscus through the coronary ligament (Figure 1D). The proximal attachment is subject to debate, although most authors agree that it is located proximal and posterior to the center of the lateral femoral epicondyle[14].
During the pivot shift phenomenon, internal rotation and anterior translation are responsible for the rupture of the ACL and for the load on other soft tissue structures attached to the lateral tibia, which will eventually could tear or avulse the lateral margin of the tibia (Segond fracture)[15]. There have been several studies that pointed out that the Segond fracture is caused by some capsule-ligamentous structure throughout the lateral aspect of the knee connecting the distal femur to the tibia[12,14,16,17].
Visualization of the ALL on ultrasonography is challenging. Some studies showed that this structure could be identified at least partially on ultrasound. The sensibility of this method varied, among different authors, between 60% to 100%[18,19]. However, it was not easy to isolate the ALL from the adjacent structures like the anterolateral capsule and the iliotibial band (ITB). Performing the ultrasound examination with the knee in internal rotation and flexion may improve the visualization of this ligament structure[20]. Even though anterolateral ligament injuries can be diagnosed with ultrasound, this imaging method is not routinely utilized in the diagnostic algorithm of these patients.
Many authors studied how to identify the ALL by magnetic resonance imaging (MRI), most of them agreed that this structure is difficult to analyze along its entire length and that is best identified in the coronal plane[21]. Clear identification of the ligament is described in more than half of the cases, varying between 51% and 100% in most studies. However, other authors visualized the ligament in only 11% of the cases[22-24]. The femoral origin is difficult to visualize because it is not clearly distinguishable from the LCL and ITB[25]. In injured knees, soft tissue swelling and joint effusion can provide signal intensification that may allow enhanced visualization of the ALL[21,23]. The true utility of MRI is its capacity to identify involvement of the ALL following knee injuries to potentially guide in deciding ligament reconstruction alternatives. Abnormal ALL includes one or the combination of the following features: complete disruption, irregular contour and ligamentous edema. This findings can correlate with an increase in pivot shift test[26].
A developing body of literature has examined the role of anterolateral structures in rotatory knee stability. Given the high complexity of this region of the knee, with its varying anatomical structures, biomechanical studies have shown uncertain results. In a controlled laboratory study, Zens et al[27] described the biomechanical properties of the ALL and found that the LLA becomes longer under flexion and internal rotation, while it becomes shorter under external rotation. The mean length change during internal rotation was also higher when the knee was flexed[27]. According to different studies, mean ultimate failure load ranged between 50 and 205 N, mean stiffness 20 to 42 N/mm, and mean ultimate strain 36%[27-29]. Sectioning of the ALL resulted in a statistically significant increase in anterior translation and internal knee rotation after ACL section[30-32]. However, a number of authors suggested that the ALL or anterolateral capsule plays just a minor role at physiologic ranges of tibial translation acting as a secondary stabilizer to anterolateral translation only after loss of the ACL[33-35]. Most biomechanical studies evaluated the anterolateral structures with preserved ITB. On the contrary, Kittl et al[26] showed that when Kaplan's fibers and the capsulo-osseous layer are disrupted, thus interrupting the functional unity of the ITB between the distal femur and the proximal tibia, the internal rotation of the tibia is substantially increased throughout range of motion[36]. Demonstrating a crucial contribution of the ITB to rotatory knee stability. In another study, Noyes et al[35] observed that sectioning of the ALL and the ITB in ACL-deficient knees converted 71% of the specimens to a grade 3 pivot shift as measured by composite tibiofemoral translations and rotations. These results emphasize the importance of approaching the anterolateral complex of the knee as a unit rather than the anterolateral ligament in isolation.
There is no agreement on the optimal treatment management strategy for anterolateral knee injuries and the possible long-term clinical impact of ALL insufficiency is currently unknown. As noted above, anterolateral structures contribute significantly to rotational knee stability and should be acknowledged in the setting of ACL reconstruction or revision surgery. Concomitant ACLR and ALL reconstruction (ALLR) significantly decreased internal rotation and tibial translation in the axial plane with respect to isolated ACLR in the presence of ALL deficiency[32]. The indication for lateral tenodesis or re
| Major Criteria | Minor Criteria |
| ACL revision; pivot shift grade IIIpivot sports; competitive athlete or “elite”; age: ≤ 25 yr old | Hyperlaxity/recurvatum ≥ 10°; KT-1000 ≥ 8 mm side-side difference; instability ≥ 6 mo; medial meniscectomy and/or lateral meniscus root lesion; contralateral knee instability; Bmi ≥ 30; tibial plateau slope ≥ 10°; severe anterior tibial translation; presence of a ‘‘lateral femoral notch sign’’ or an impaction of the lateral femoral condyle[39]; segond fracture |
Several techniques have been described to perform an ALLR. The main goal is to control internal rotation and restore the normal knee kinematics. From a technical point of view, there are two surgical alternatives: a lateral extra-articular tenodesis (LET) or an "anatomical" reconstruction of the ALL. Different fixation sites, grafts, and fixation angles have been described (Table 2). Available evidence is based on mixed clinical and in vitro studies 9. No study has demonstrated improvement in objective or subjective outcomes of one procedure over the others[38]. Three recent systematic reviews with meta-analyses including only comparative studies have shown that the addition of a lateral extra-articular tenodesis procedure to an ACL reconstruction has been found to reduce rotational laxity control, but has no effect on anterior translation or patient-reported outcomes[9,39,40]. For the LET the most frequently used graft is the ITB and for the anatomical reconstruction the gracilis tendon or allograft. The most frequent femoral insertion site is posterior and proximal to the lateral epicondyle. The ITB can be passed under or over the LCL. It can also be fixed anterior and distal to the epicondyle. Suture anchors, interference screws or cortical buttons can be used for graft fixation. Whichever technique is used, the most important consideration is to avoid the confluence of the tunnels with the ACL. This can usually be avoided easily by aiming the drill 30° proximal and 30° anterior. It is recommended to perform this step while directly visualizing the intra-articular femoral tunnel; positioning the arthroscope in the tunnel to confirm if necessary. Other techniques describe a mixture of intra-articular and extra-articular ACL reconstruction utilizing a unique graft through a single femoral tunnel as described by Sonnery-Cottet et al[41] or passing the graft over-the-top as described by Dejour et al[42], Grassi et al[43], Sarraj et al[44], Placella et al[45].
| Ref. | Graft | Direction | Fixation site | Fixation angle | Graft fixation |
| Grassi et al[43] | ITB | Deep to the LCL | Proximal and posterior to the lateral femoral epicondyle | Neutral rotation/0°-90° | Interference screw |
| Mahmoud et al[47] | ITB | Deep to the LCL and then passed through the lateral distal intermuscular septum from posterior to anterior and adjacent to the femur | - | Neutral rotation/around 50° flexion | ITB is sutured to itself at physiological tension |
| Arnold et al[48] | ITB | Under the LCL and the Popliteus tendon | - | External rotation/90°-100° | Sutured with periosteal stitches to GT |
| Porter et al[49] | ITB | Around the proximal LCL | Posterior to the Gerdy tubercle | Neutral rotation/35° | Interference screw |
| Losee et al[50] | ITB | Deep to the LCL | The femoral tunnel originated at the attachment point of the lateral gastrocnemius and ended antero-distal to the LCL femoral insertion site | External rotation/30° | Sutured at the Gerdy tubercle |
| Dejour et al[42] | ITB | Over the LCL | Anterior to the junction of the femoral shaft and lateral femoral condyle | External rotation/30° | 1 Cancellous screws |
| Ellison et al[51] | ITB | Deep to the LCL | Slightly anterior to its original harvest site at the Gerdy tubercle | External rotation/90° | Interference screw |
| Lee et al[52] | Allograft | Over the LCL | Femur: Proximal and posterior to the lateral femoral epicondyle/Tibia: Between the fibular head and Gerdy tubercle at approximately 10 mm below the joint line | Neutral rotation/30° | 2 Interferences screws1 |
| Sonnery-Cottet et al[41] | Gracillis (ACL and ALL) | Single femoral tunnel/graft is routed deep to the iliotibial band from the femur to the tibia, shuttled through a tibial bony tunnel and back proximally to the femur | Proximal and posterior to the lateral femoral epicondyle | Neutral rotation/extension | Fixed to the ACL graft |
| Dejour et al[42] | Double hamstrings (ACL and ALL) | Over-the-top | Proximal and posterior to the lateral femoral epicondyle | 90 | Stapples |
The findings outlined in the present mini-review contribute to the comprehension of the role of the anterolateral complex of the knee. Although research on ALL has increased considerably in recent years, some debate remains regarding its anatomy and further refinement is still ongoing. Biomechanical studies have revealed that anterolateral structures contribute significantly to rotational stability of the knee and should be accounted for in the setting of an ACL injury, especially in cases with a high degree of pivot shift or revision surgery. Surgical indications for ALL reconstruction are not currently evidence-based and the ideal graft type, fixation location and fixation angle have not yet been determined. Further clinical research remains to be conducted to identify the most appropriate situations for augmentation of a primary ACL reconstruction with an anterolateral procedure to enhance patient outcomes.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Argentina
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pace V, Italy; Santoso A, Indonesia S-Editor: Wang DM L-Editor: A P-Editor: Wang DM
| 1. | Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am. 1976;58:173-179. [PubMed] |
| 2. | Johnson LL. Lateral capsualr ligament complex: anatomical and surgical considerations. Am J Sports Med. 1979;7:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 90] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 545] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 4. | Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyret P. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 319] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 5. | Helito CP, Demange MK, Bonadio MB, Tírico LE, Gobbi RG, Pécora JR, Camanho GL. Anatomy and Histology of the Knee Anterolateral Ligament. Orthop J Sports Med. 2013;1:2325967113513546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 209] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 6. | Santoso A, Anwar IB, Sibarani T, Soetjahjo B, Utomo DN, Mustamsir E, Budhiparama NC. Research on the Anterolateral Ligament of the Knee: An Evaluation of PubMed Articles From 2010 to 2019. Orthop J Sports Med. 2020;8:2325967120973645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Feng J, Cao Y, Tan L, Liang J, He C, He J, Wu S. Anterior cruciate ligament reconstruction with lateral extra-articular tenodesis reduces knee rotation laxity and graft failure rate: A systematic review and meta-analysis. J Orthop Surg (Hong Kong). 2022;30:10225536221095969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Lanzetti RM, Pace V, Ciompi A, Perugia D, Spoliti M, Falez F, Auro C. Over the top anterior cruciate ligament reconstruction in patients with open physes: a long-term follow-up study. Int Orthop. 2020;44:771-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM. Lateral Extra-articular Tenodesis Reduces Rotational Laxity When Combined With Anterior Cruciate Ligament Reconstruction: A Systematic Review of the Literature. Arthroscopy. 2015;31:2022-2034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 184] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 10. | Terry GC, Hughston JC, Norwood LA. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14:39-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 245] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Herbst E, Albers M, Burnham JM, Shaikh HS, Naendrup JH, Fu FH, Musahl V. The anterolateral complex of the knee: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2017;25:1009-1014. [PubMed] |
| 12. | Vieira EL, Vieira EA, da Silva RT, Berlfein PA, Abdalla RJ, Cohen M. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23:269-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 200] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 13. | Getgood A, Brown C, Lording T, Amis A, Claes S, Geeslin A, Musahl V; ALC Consensus Group. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc. 2019;27:166-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 257] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 14. | Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96-B:325-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 310] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 15. | Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40:1808-1813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 132] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 16. | Helito CP, do Amaral C Jr, Nakamichi YD, Gobbi RG, Bonadio MB, Natalino RJ, Pécora JR, Cardoso TP, Camanho GL, Demange MK. Why Do Authors Differ With Regard to the Femoral and Meniscal Anatomic Parameters of the Knee Anterolateral Ligament? Orthop J Sports Med. 2016;4:2325967116675604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Daggett M, Ockuly AC, Cullen M, Busch K, Lutz C, Imbert P, Sonnery-Cottet B. Femoral Origin of the Anterolateral Ligament: An Anatomic Analysis. Arthroscopy. 2016;32:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 18. | Cavaignac E, Wytrykowski K, Reina N, Pailhé R, Murgier J, Faruch M, Chiron P. Ultrasonographic Identification of the Anterolateral Ligament of the Knee. Arthroscopy. 2016;32:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 19. | Capo J, Kaplan DJ, Fralinger DJ, Adler RS, Campbell KA, Jazrawi LM, Alaia MJ. Ultrasonographic visualization and assessment of the anterolateral ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25:3134-3139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Cianca J, John J, Pandit S, Chiou-Tan FY. Musculoskeletal ultrasound imaging of the recently described anterolateral ligament of the knee. Am J Phys Med Rehabil. 2014;93:186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Helito CP, Helito PV, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL, Demange MK. MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skeletal Radiol. 2014;43:1421-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 22. | Hartigan DE, Carroll KW, Kosarek FJ, Piasecki DP, Fleischli JF, D'Alessandro DF. Visibility of Anterolateral Ligament Tears in Anterior Cruciate Ligament-Deficient Knees With Standard 1.5-Tesla Magnetic Resonance Imaging. Arthroscopy. 2016;32:2061-2065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 23. | Taneja AK, Miranda FC, Braga CA, Gill CM, Hartmann LG, Santos DC, Rosemberg LA. MRI features of the anterolateral ligament of the knee. Skeletal Radiol. 2015;44:403-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 24. | Kosy JD, Mandalia VI, Anaspure R. Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skeletal Radiol. 2015;44:1647-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 25. | Porrino J Jr, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS. The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. AJR Am J Roentgenol. 2015;204:367-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 26. | Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, Lopomo N, Samuelsson K, Irrgang JJ. The Influence of Meniscal and Anterolateral Capsular Injury on Knee Laxity in Patients With Anterior Cruciate Ligament Injuries. Am J Sports Med. 2016;44:3126-3131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 134] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 27. | Zens M, Niemeyer P, Ruhhammer J, Bernstein A, Woias P, Mayr HO, Südkamp NP, Feucht MJ. Length Changes of the Anterolateral Ligament During Passive Knee Motion: A Human Cadaveric Study. Am J Sports Med. 2015;43:2545-2552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 28. | Helito CP, Bonadio MB, Rozas JS, Wey JM, Pereira CA, Cardoso TP, Pécora JR, Camanho GL, Demange MK. Biomechanical study of strength and stiffness of the knee anterolateral ligament. BMC Musculoskelet Disord. 2016;17:193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 29. | Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF. The Anterolateral Ligament: An Anatomic, Radiographic, and Biomechanical Analysis. Am J Sports Med. 2015;43:1606-1615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 274] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 30. | Spencer L, Burkhart TA, Tran MN, Rezansoff AJ, Deo S, Caterine S, Getgood AM. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:2189-2197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 187] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 31. | Rasmussen MT, Nitri M, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 1: Secondary Role of the Anterolateral Ligament in the Setting of an Anterior Cruciate Ligament Injury. Am J Sports Med. 2016;44:585-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 205] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 32. | Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 2: Anterolateral Ligament Reconstruction Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44:593-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 33. | Thein R, Boorman-Padgett J, Stone K, Wickiewicz TL, Imhauser CW, Pearle AD. Biomechanical Assessment of the Anterolateral Ligament of the Knee: A Secondary Restraint in Simulated Tests of the Pivot Shift and of Anterior Stability. J Bone Joint Surg Am. 2016;98:937-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 109] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 34. | Huser LE, Noyes FR, Jurgensmeier D, Levy MS. Anterolateral Ligament and Iliotibial Band Control of Rotational Stability in the Anterior Cruciate Ligament-Intact Knee: Defined by Tibiofemoral Compartment Translations and Rotations. Arthroscopy. 2017;33:595-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Noyes FR, Huser LE, Levy MS. Rotational Knee Instability in ACL-Deficient Knees: Role of the Anterolateral Ligament and Iliotibial Band as Defined by Tibiofemoral Compartment Translations and Rotations. J Bone Joint Surg Am. 2017;99:305-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 36. | Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA. The Role of the Anterolateral Structures and the ACL in Controlling Laxity of the Intact and ACL-Deficient Knee. Am J Sports Med. 2016;44:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 239] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 37. | Musahl V, Getgood A, Neyret P, Claes S, Burnham JM, Batailler C, Sonnery-Cottet B, Williams A, Amis A, Zaffagnini S, Karlsson J. Contributions of the anterolateral complex and the anterolateral ligament to rotatory knee stability in the setting of ACL Injury: a roundtable discussion. Knee Surg Sports Traumatol Arthrosc. 2017;25:997-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 38. | Ferretti A, Monaco E, Ponzo A, Basiglini L, Iorio R, Caperna L, Conteduca F. Combined Intra-articular and Extra-articular Reconstruction in Anterior Cruciate Ligament-Deficient Knee: 25 Years Later. Arthroscopy. 2016;32:2039-2047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 106] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 39. | Devitt BM, Bell SW, Ardern CL, Hartwig T, Porter TJ, Feller JA, Webster KE. The Role of Lateral Extra-articular Tenodesis in Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review With Meta-analysis and Best-Evidence Synthesis. Orthop J Sports Med. 2017;5:2325967117731767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 40. | Song GY, Hong L, Zhang H, Zhang J, Li Y, Feng H. Clinical Outcomes of Combined Lateral Extra-articular Tenodesis and Intra-articular Anterior Cruciate Ligament Reconstruction in Addressing High-Grade Pivot-Shift Phenomenon. Arthroscopy. 2016;32:898-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 41. | Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral Ligament Reconstruction Is Associated With Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients From the SANTI Study Group. Am J Sports Med. 2017;45:1547-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 361] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 42. | Dejour D, Zaffagnini S, Ntagiopoulos PG, Grassi A, Muccioli GMM, Marcacci M. ACL Reconstruction with Extra-articular Plasty. In: Siebold R, Dejour D, Zaffagnini S, editors. Anterior Cruciate Ligament Reconstruction. Springer Berlin Heidelberg, 2014: 299-316. [DOI] [Full Text] |
| 43. | Grassi A, Zicaro JP, Costa-Paz M, Samuelsson K, Wilson A, Zaffagnini S, Condello V; ESSKA Arthroscopy Committee. Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg Sports Traumatol Arthrosc. 2020;28:418-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 44. | Sarraj M, de Sa D, Shanmugaraj A, Musahl V, Lesniak BP. Over-the-top ACL reconstruction yields comparable outcomes to traditional ACL reconstruction in primary and revision settings: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2019;27:427-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 45. | Placella G, Bartoli M, Peruzzi M, Speziali A, Pace V, Cerulli G. Return to sport activity after anterior cruciate ligament reconstruction in skeletally immature athletes with manual drilling original all inside reconstruction at 8 years follow-up. Acta Orthop Traumatol Turc. 2016;50:635-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Herbst E, Hoser C, Tecklenburg K, Filipovic M, Dallapozza C, Herbort M, Fink C. The lateral femoral notch sign following ACL injury: frequency, morphology and relation to meniscal injury and sports activity. Knee Surg Sports Traumatol Arthrosc. 2015;23:2250-2258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 47. | Mahmoud A, Torbey S, Honeywill C, Myers P. Lateral Extra-Articular Tenodesis Combined With Anterior Cruciate Ligament Reconstruction Is Effective in Knees With Additional Features of Lateral, Hyperextension, or Increased Rotational Laxity: A Matched Cohort Study. Arthroscopy. 2022;38:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 48. | Arnold JA, Coker TP, Heaton LM, Park JP, Harris WD. Natural history of anterior cruciate tears. Am J Sports Med. 1979;7:305-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 191] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 49. | Porter MD, Shadbolt B, Pomroy S. The Augmentation of Revision Anterior Cruciate Ligament Reconstruction With Modified Iliotibial Band Tenodesis to Correct the Pivot Shift: A Computer Navigation Study. Am J Sports Med. 2018;46:839-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 50. | Losee RE, Johnson TR, Southwick WO. Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am. 1978;60:1015-1030. [PubMed] |
| 51. | Ellison AE. Distal iliotibial-band transfer for anterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1979;61:330-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 178] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 52. | Lee DW, Kim JG, Cho SI, Kim DH. Clinical Outcomes of Isolated Revision Anterior Cruciate Ligament Reconstruction or in Combination With Anatomic Anterolateral Ligament Reconstruction. Am J Sports Med. 2019;47:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 112] [Article Influence: 18.7] [Reference Citation Analysis (0)] |