Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7495
Peer-review started: December 30, 2021
First decision: February 8, 2022
Revised: February 24, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: July 26, 2022
Processing time: 192 Days and 16.4 Hours
Antipsychotics are associated with abnormalities in glucose metabolism in patients with schizophrenia. Liraglutide, a GLP-1 receptor agonist, is Food and Drug Administration approved for the treatment of type 2 diabetes mellitus. However, ways to maintain the long-term stability of psychotic symptoms and balance the disadvantages of obesity, diabetes, and other metabolic disorders caused by antipsychotic medications remain unclear. In this study, we present a case of weight gain and hyperglycemia in a schizophrenia patient who received antipsychotic polypharmacy for 6 years.
A 27-year-old man with olanzapine and sodium valproate-treated disorganized schizophrenia was admitted to a diabetes outpatient clinic. He was diagnosed with type 2 diabetes (fasting blood glucose, 20 mmol/L) and obesity (body mass index, 38.58 kg/m2). The patient had been treated with glargine (40 IU/d) and metformin (1.5 g/d) and showed a poor response for 2 mo. Two years of liraglutide treatment resulted in stable blood glucose levels and weight loss in addition to a maintained stable mental status for a long time. The biological activities of GLP-1 significantly improved glucose levels and body weight in the schizophrenia patient treated with antipsychotic medications.
Liraglutide administration can be considered an effective alternative treatment for abnormalities in glucose metabolism in schizophrenia patients receiving antipsychotics.
Core Tip: This report describes the effects of GLP-1 receptor agonist treatment in a young schizophrenia patient with long-term use of antipsychotics, which induced type 2 diabetes. It presents the success of blood glucose control with the GLP-1 receptor agonist in a short period of time during his hospitalization and helped him to control his blood glucose and lose weight while maintaining a stable mental status in the long-term.
- Citation: Zhang L, Yu WJ, Zhu H, Li HF, Qiao J. Successful treatment of hyperglycemia with liraglutide in a hospitalized 27-year-old patient with schizophrenia: A case report. World J Clin Cases 2022; 10(21): 7495-7501
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7495.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7495
The use of antipsychotics has been associated with abnormalities in glucose metabolism in patients with schizophrenia[1-3]. A high prevalence of metabolic disturbances and type 2 diabetes among patients with schizophrenia was found to increase the risk of cardiovascular morbidity and mortality[4,5]. Current intervention strategies against antipsychotic-induced weight gain and diabetes mellitus include switching to other antipsychotics, adding glucose-lowering drugs (e.g., metformin), or initiating insulin therapy. However, ways to maintain the long-term stability of psychotic symptoms and balance the disadvantages of obesity, diabetes, and other metabolic disorders caused by antipsychotic medications remain unclear.
Liraglutide is a GLP-1 receptor agonist (Victoza, Novonordisk) that was approved for the treatment of type 2 diabetes in 2009[6]. As this medicine induces weight loss, the Food and Drug Administration FDA expanded its indications for obesity treatment in 2015[6,7].
Herein, we present the case of a young man with schizophrenia who had markedly increased weight gain and hyperglycemia after 6 years of combined antipsychotic therapy. After attempting to control hyperglycemia with insulin and metformin with a poor response, we successfully attained satisfactory blood glucose control with liraglutide in a short period during hospitalization. Furthermore, liraglutide helped the patient to lose weight while maintaining a stable mental status.
Exceedingly thirsty, polydipsia, and polyuria for 2 mo.
A 27-year-old, unemployed man with schizophrenia was previously prescribed olanzapine (10 mg/d) and sodium valproate (1 g/d). Six years ago, the patient was diagnosed with schizophrenia, and since then he had been taking many antipsychotics, such as risperidone, aripiprazole, and ziprasidone, with poor responsiveness. However, the patient had gained almost 50 kg in the past 2 years, and on admission, he weighed 106.3 kg (body mass index, 38.58 kg/m2). Two months ago, he began to feel exceedingly thirsty. Polydipsia and polyuria were established at the time of the checkup. His fasting blood glucose (FBG) level was 20 mmol/L, and glycated hemoglobin A1c (HbA1c) was 12.3%. The patient was treated with glargine (40 IU/d) and metformin (1.5 g/d) in a local hospital, but his FBG and postprandial blood glucose (PBG) levels fluctuated within the range of 10-20 mmol/L and 13-24 mmol/L, respectively.
The patient was diagnosed with schizophrenia 6 years ago.
The patient denied any other specific personal or family history of other diseases.
The physical examination and diabetes complications-related examinations including fundus examination, electromyography (EMG), and renal function showed no obvious abnormalities.
After admission, we conducted many related examinations, such as urine free cortisol and blood cortisol, blood potassium, blood pressure, thyroid function, hormone, etc. The physical examination and diabetes complications-related examinations including fundus examination, EMG, and renal function showed no obvious abnormalities. The specific results are shown in Table 1.
| Hospital admission1 | Hospital discharge2 | Follow-up3 | |
| Height (cm) | 166 | 166 | 166 |
| Weight (kg) | 106.3 | 104 | 98.4 |
| BMI (kg/m2) | 38.58 | 37.74 | 35.71 |
| Blood pressure (mmHg) | 130/80 | 122/78 | 120/80 |
| Pulse rate (times/min) | 80 | 78 | 78 |
| Blood glucose (mmol/L) | 15.0 | 4.9 | 5.07 |
| HbA1c (%) | 12.3 | NA | 6.0 |
| Insulin (pmol/L) | 733.10 | NA | NA |
| Total bilirubin (μmol/L) | 12.11 | NA | 4.93 |
| Albumin (g/L) | 45.1 | NA | 47.5 |
| ALT (IU/L) | 22 | NA | 26 |
| AST (IU/L) | 27 | NA | 26 |
| Total cholesterol (mmol/L) | 6.02 | NA | 5.00 |
| Triglyceride (mmol/L) | 1.81 | 1.7 | 1.62 |
| Uric acid (μmol/L) | 484 | 366 | 382 |
| Creatinine (μmol/L) | 70 | NA | 72 |
| HDL (mmol/L) | 1.20 | NA | 1.39 |
| LDL (mmol/L) | 3.48 | 3.21 | 2.29 |
| Testosterone (nmol/L) | 14.940 | NA | NA |
| TSH (mIU/L) | 1.770 | NA | 3.500 |
| Serum potassium (mmol/L) | 4.26 | 4.25 | 4.51 |
| Urine free cortisol (nmol/24 h) | 168.3 | NA | NA |
| Fasting plasma cortisol (nmol/L) | 254 | NA | NA |
He was then transferred to the Department of Endocrinology of Shanghai Ninth Hospital with a diagnosis of diabetes, obesity, and schizophrenia (DSM-5 criteria) after psychiatric consultation at Shanghai Mental Health Center (Shanghai, China).
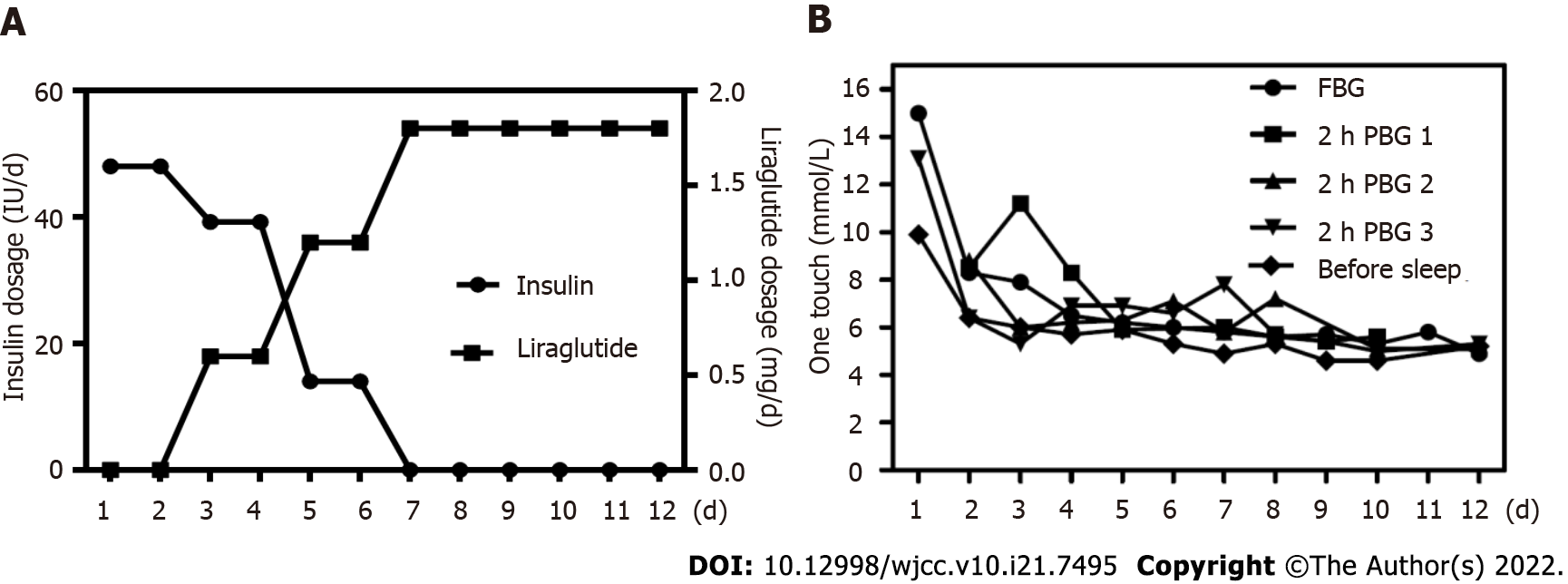
When the diagnosis was confirmed, metformin was discontinued, and the patient was treated with an insulin pump (Medtronic, MMT-712EWS). After treatment with continuous subcutaneous insulin infusion (CSII, dose 48 U/d) for 3 d, we administered an add-on treatment with liraglutide (Victoza 0.6 mg/d, subcutaneous injection). Three days later, the dosage of liraglutide was increased to 1.2 mg/d, whereas that of insulin (NovoMix 30) was decreased to 14 U/d. Two days later, the liraglutide dosage was increased to 1.8 mg/d; insulin administration was stopped without changing the prior to admission therapy regimen of olanzapine and sodium valproate (Figure 1A). The diet during hospitalization was a diabetic diet pattern. Although daily exercise was recommended, it seemed difficult, and the patient only seemed to be able to walk for 10 min after meals. Blood glucose levels were measured five times per day, including the determination of FBG and PBG levels after three meals and before bedtime (Figure 1B). FBG dropped from 15.0 mmol/L at admission to 4.9 mmol/L at discharge, and PBG from 13.1 mmol/L to 5.1 mmol/L. Blood glucose before bedtime dropped from 9.9 mmol/L to 5.2 mmol/L. Meanwhile, his weight dropped from 106.3 kg to 104 kg in one week. When he was found to be medically stabilized, he was discharged from the hospital and advised to attend a psychiatric unit for further treatment.
The patient was followed up by telephone. After 2 years of treatment, his blood glucose levels were well controlled within the normal range, and his total weight loss was almost 8 kg (a 7.5% body weight reduction) when treated with liraglutide (Victoza 0.6 mg/day, subcutaneous injection). His laboratory examinations are shown in Table 1. Meanwhile, his psychiatric status was stable during the previous 2-year period, without hospital admissions. The initiation of liraglutide treatment led to significant clinical improvement, as evidenced by decreased blood glucose levels and reduced weight.
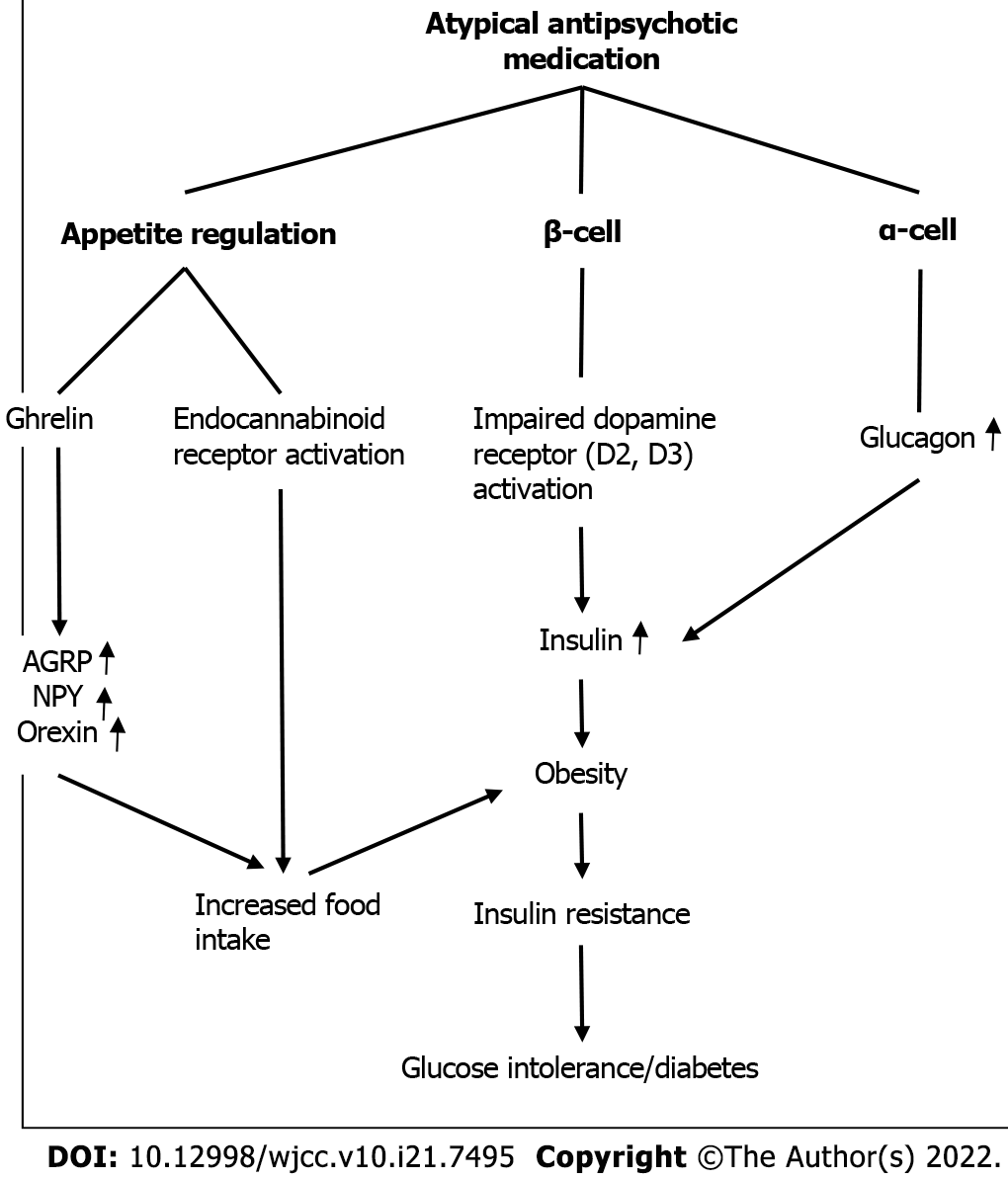
The postulated underlying mechanisms for the development of diabetes in patients treated with antipsychotics, particularly with the drugs olanzapine and clozapine, involve carbohydrate intolerance. This is associated with increased insulin resistance[1]. These medicines cause abnormalities in glucose tolerance by perturbing appetite regulation, insulin secretion and action, and release of insulin counter-regulatory hormones[8] (Figure 2).
GLP-1 is an incretin hormone secreted by L cells in the intestinal mucosa in response to nutrients. The biological activities of GLP-1 include stimulation of insulin biosynthesis and glucose-dependent insulin secretion by pancreatic beta cells, inhibition of glucagon secretion, delay in gastric emptying, and inhibition of food intake[9]. The time course of reduction in HbA1c showed full effects of liraglutide after 12 wk of treatment by liraglutide monotherapy[10]. Liraglutide reduces appetite and food intake, thereby ensuring that body weight is kept low[11,12]. The results of an animal study confirmed that olanzapine-induced weight gain and metabolic derangements were found to be reversed after treatment with the GLP-1 analog liraglutide[13]. FBG generally represents the sugar output of the liver in the body, which is a basic state. PBG generally reflects the influence of diet on blood glucose, and to some extent represents the response of the body's own islets to diet[14]. In this case, the patient's FBG and PBG were both high at admission but returned to normal after 12 days of liraglutide treatment.
To the best of our knowledge, few relevant research has reported findings that are applicable to the current clinical practice regarding the treatment of schizophrenia with glucose and lipid metabolic disturbance in China. Therefore, the potential metabolic improvement effects of GLP-1 receptor agonists in antipsychotic-treated patients require further investigation. Randomized, double-blind, controlled trials need to be conducted in the future to document the efficacy and safety of Victoza in the treatment of acute hyperglycemia and/or obesity.
Empiric treatment of hyperglycemia in patients with schizophrenia involves reducing the dosage of antipsychotics or choosing to switch to antipsychotics. In the absence of drug-specific evidence, the treatment of drug-induced hyperglycemia and diabetes is similar to the full range of standard diabetes care, including lifestyle changes, oral/injectable antidiabetic drugs, and insulin[15]. The concomitant use of metformin has been used as the first choice in the treatment of schizophrenia patients with antipsychotic-induced obesity and type 2 diabetes to counteract antipsychotic-induced weight gain and other metabolic adversities in schizophrenia[16]. However, in most patients, good blood glucose control could not be achieved by the administration of metformin only, and the addition of an insulin secretagogue or insulin is always required, which, in turn, hampers effective weight control, especially at a larger dosage. In a previous study, switching the antipsychotic medication led to a reduction in weight and contributed to achieving broader health benefits, such as decreased FBG levels[17]. But reducing antipsychotic dosage or choosing to switch to antipsychotic medications may lead to relapse. Important clinical considerations for patients with schizophrenia taking antipsychotic medications is monitoring metabolic markers such as glucose before and during treatment. Changing unhealthy lifestyles is considered essential in preventive measures. Long-term outcomes of the patient included stabilization of psychiatric symptoms and improvement of metabolic disorders. Although we could only follow up by telephone, which was a shortcoming of this study, we also obtained the patient's review indicators during this period. For patients with chronic diseases, it is very important to maintain a good lifestyle, which also requires patients to pay more perseverance. Future research is needed to elucidate pathophysiology and optimal targeted treatment for antipsychotics-induced diabetes and obesity. In the present case, the use of liraglutide achieved satisfactory short- and long-term glucose control and mild weight loss without any recurrent schizophrenia attack. Moreover, the large dose of insulin was gradually reduced until final cessation. The implementation of liraglutide treatment for 16 wk as an adjunctive therapy along with clozapine or olanzapine resulted in stabilization in overweight or obese patients with schizophrenia spectrum disorders and prediabetes and significantly improved glucose tolerance and glycemic control[11].
When monopharmacological strategies alone are insufficient and switching from antipsychotics to relatively weight-neutral agents is not feasible, Victoza can be considered an effective alternative treatment for schizophrenia patients with hyperglycemia and obesity. Large-scale longitudinal blinded studies should be adopted to obtain more objective and effective results in future.
We thank the participants in the study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Liao Z, Singapore; Nishihama K, Japan; Timsina LR, United States A-Editor: Ahmed S, Pakistan S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Lindenmayer JP, Nathan AM, Smith RC. Hyperglycemia associated with the use of atypical antipsychotics. J Clin Psychiatry. 2001;62 Suppl 23:30-38. [PubMed] [DOI] [Full Text] |
| 2. | Buse JB. Metabolic side effects of antipsychotics: focus on hyperglycemia and diabetes. J Clin Psychiatry. 2002;63 Suppl 4:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Sernyak MJ, Gulanski B, Rosenheck R. Undiagnosed hyperglycemia in patients treated with atypical antipsychotics. J Clin Psychiatry. 2005;66:1463-1467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry. 2012;25:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 369] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 5. | Soleimani M. Insulin resistance and hypertension: new insights. Kidney Int. 2015;87:497-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 110] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 6. | Davies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjøth TV, Andreasen AH, Jensen CB, DeFronzo RA; NN8022-1922 Study Group. Efficacy of Liraglutide for Weight Loss Among Patients With Type 2 Diabetes: The SCALE Diabetes Randomized Clinical Trial. JAMA. 2015;314:687-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 707] [Article Influence: 70.7] [Reference Citation Analysis (0)] |
| 7. | Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, Lau DC, le Roux CW, Violante Ortiz R, Jensen CB, Wilding JP; SCALE Obesity and Prediabetes NN8022-1839 Study Group. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N Engl J Med. 2015;373:11-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1103] [Cited by in RCA: 1566] [Article Influence: 156.6] [Reference Citation Analysis (0)] |
| 8. | Elias AN, Hofflich H. Abnormalities in glucose metabolism in patients with schizophrenia treated with atypical antipsychotic medications. Am J Med. 2008;121:98-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2055] [Cited by in RCA: 2340] [Article Influence: 130.0] [Reference Citation Analysis (1)] |
| 10. | Garber A, Henry R, Ratner R, Garcia-Hernandez PA, Rodriguez-Pattzi H, Olvera-Alvarez I, Hale PM, Zdravkovic M, Bode B; LEAD-3 (Mono) Study Group. Liraglutide versus glimepiride monotherapy for type 2 diabetes (LEAD-3 Mono): a randomised, 52-week, phase III, double-blind, parallel-treatment trial. Lancet. 2009;373:473-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 752] [Cited by in RCA: 791] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 11. | Larsen JR, Vedtofte L, Jakobsen MSL, Jespersen HR, Jakobsen MI, Svensson CK, Koyuncu K, Schjerning O, Oturai PS, Kjaer A, Nielsen J, Holst JJ, Ekstrøm CT, Correll CU, Vilsbøll T, Fink-Jensen A. Effect of Liraglutide Treatment on Prediabetes and Overweight or Obesity in Clozapine- or Olanzapine-Treated Patients With Schizophrenia Spectrum Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2017;74:719-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 133] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 12. | Vilsbøll T, Christensen M, Junker AE, Knop FK, Gluud LL. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ. 2012;344:d7771. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 737] [Cited by in RCA: 655] [Article Influence: 50.4] [Reference Citation Analysis (0)] |
| 13. | Lykkegaard K, Larsen PJ, Vrang N, Bock C, Bock T, Knudsen LB. The once-daily human GLP-1 analog, liraglutide, reduces olanzapine-induced weight gain and glucose intolerance. Schizophr Res. 2008;103:94-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Penninx BWJH, Lange SMM. Metabolic syndrome in psychiatric patients: overview, mechanisms, and implications. Dialogues Clin Neurosci. 2018;20:63-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 345] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 15. | Jain V, Patel RK, Kapadia Z, Galiveeti S, Banerji M, Hope L. Drugs and hyperglycemia: A practical guide. Maturitas. 2017;104:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Mizuno Y, Suzuki T, Nakagawa A, Yoshida K, Mimura M, Fleischhacker WW, Uchida H. Pharmacological strategies to counteract antipsychotic-induced weight gain and metabolic adverse effects in schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2014;40:1385-1403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 17. | Mukundan A, Faulkner G, Cohn T, Remington G. Antipsychotic switching for people with schizophrenia who have neuroleptic-induced weight or metabolic problems. Cochrane Database Syst Rev. 2010;CD006629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |