Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5869
Peer-review started: December 26, 2021
First decision: January 25, 2022
Revised: February 6, 2022
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: June 16, 2022
Lung cancer is often metastasized to the brain, liver, kidneys, bone, bone marrow, and adrenal glands; however, metastasis of primary lung cancer to the paranasal sinuses is extremely rare.
In this paper, we present a case of metastatic tumors of the sinus secondary to lung adenocarcinoma. The patient was a 46-year-old woman who underwent surgical removal of lung carcinoma. Four months after the surgical removal of the lung tumor, the patient presented with epistaxis, and on investigation, the diagnosis was confirmed to be nasal sinus tumors due to metastasis of lung adenocarcinoma.
Thorough investigation of patients with epistaxis and a history of lung cancer is necessary to diagnose metastatic sinus tumors. We reviewed relevant literature and found that there are no characteristic clinical or radiologic features for metastatic sinus tumors; however, the diagnosis can be confirmed by histopathological examination of biopsied tumor sample.
Core Tip: Lung adenocarcinoma metastasis restricted to the paranasal sinus is a rare phenomenon. In this report, we present a rare case of metastatic tumors of the sinus secondary to lung adenocarcinoma. After lung cancer surgery, the patient had no postoperative complications and was completely asymptomatic at the second-year postoperative follow-up. We reviewed relevant literature in order to identify the characteristic features observed in cases of sinus metastasis of lung adenocarcinoma.
- Citation: Li WJ, Xue HX, You JQ, Chao CJ. Lung adenocarcinoma metastasis to paranasal sinus: A case report . World J Clin Cases 2022; 10(17): 5869-5876
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5869.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5869
Advanced lung cancer is associated with a high incidence of distant metastasis[1,2], and metastasis to distant vital organs is an important factor contributing to the high mortality rate associated with lung cancer[3-5]. Metastasis of lung cancer occurs most commonly to the bones, liver, and brain and only rarely to the pericardial, adrenal, or subcutaneous tissues, spinal cord, kidney, and other organs[6]. Occasionally, lung cancer may metastasize to the external auditory canal, orbital ball, nasal cavity, or jejunum[7]. Other very rare sites of lung cancer metastases have also been reported in the literature. With respect to pathological type, studies have also shown that the most common type of metastasizing lung cancer is the adenocarcinoma[8]. Furthermore, reports have also indicated that lung cancer with nasal and sinus metastasis is associated with a short survival period and poor prognosis[1].
In this paper, we present a rare case of metastatic sinus tumor arising from adenocarcinoma of the lungs. In addition, we review literature on metastatic tumors of the nasal cavity and paranasal sinuses secondary to primary lung carcinoma.
The patient was a 45-year-old woman who was diagnosed with lung adenocarcinoma and underwent surgical resection of the tumor. Four months after the tumor removal, she presented with epistaxis and left-sided headache. however, the symptoms were considered insignificant and were not investigated further. Five months after the lung surgery, the patient developed a swelling around the left eye socket, which increased progressively and was accompanied by purulent nasal discharge, nasal obstruction, decreased sense of smell, or decreased vision.
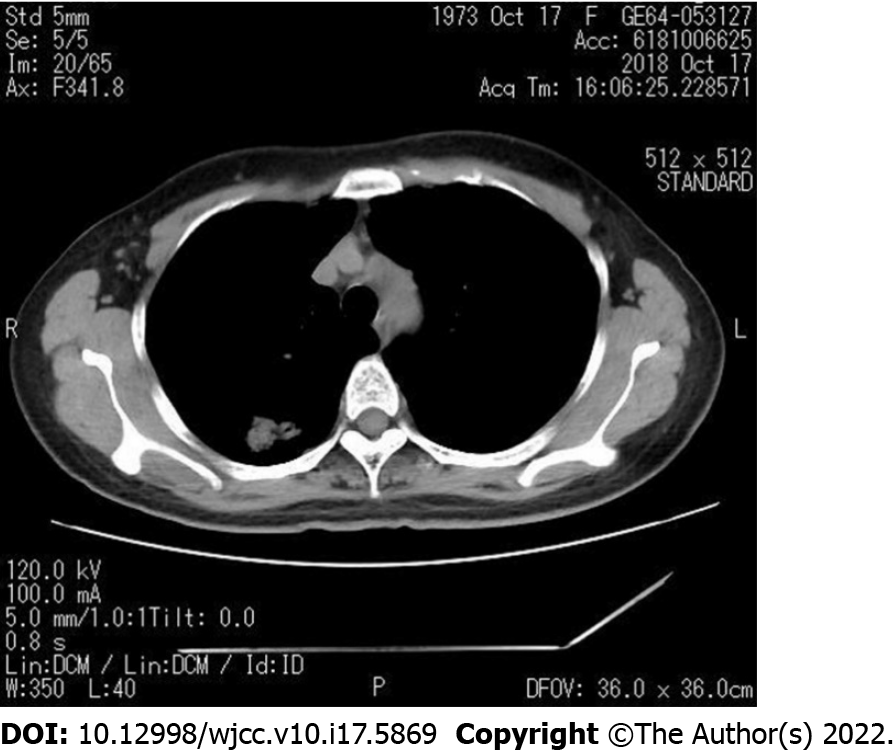
Previously, the patient was found to have a right upper pulmonary mass during a routine physical examination (Figure 1). To rule out malignancy, thoracoscopy was performed, which revealed a mass (diameter approximately 3 cm) located in the posterior segment of the right upper lobe of the lung. Surgical removal of the tumor was successful, with resection of the right upper lobe and adjacent lymph nodes. The tumor was firm in consistency and oval, with an intact capsule. Postoperative pathological examination revealed that the lesion was a moderately differentiated lung adenocarcinoma, with no involvement of the incision margin of the bronchus and no metastasis to the lymph nodes.
The patient had no previous medical history.
History taking also revealed that the patient had no other relevant medical history or family history.
On physical examination at presentation, the external nose was found to be normal in shape. No obstruction of the nasal passages was observed on either side, and no abnormal secretion or colonization was detected. There was no obvious tenderness over the areas of the sinuses.
Results of serum tests for tumor markers were all negative. No abnormalities were noted in the coagulation indices or in the results of routine blood tests, tests for immunoglobulin light chains, thyroid hormone levels, and tests for autoimmune antibodies.
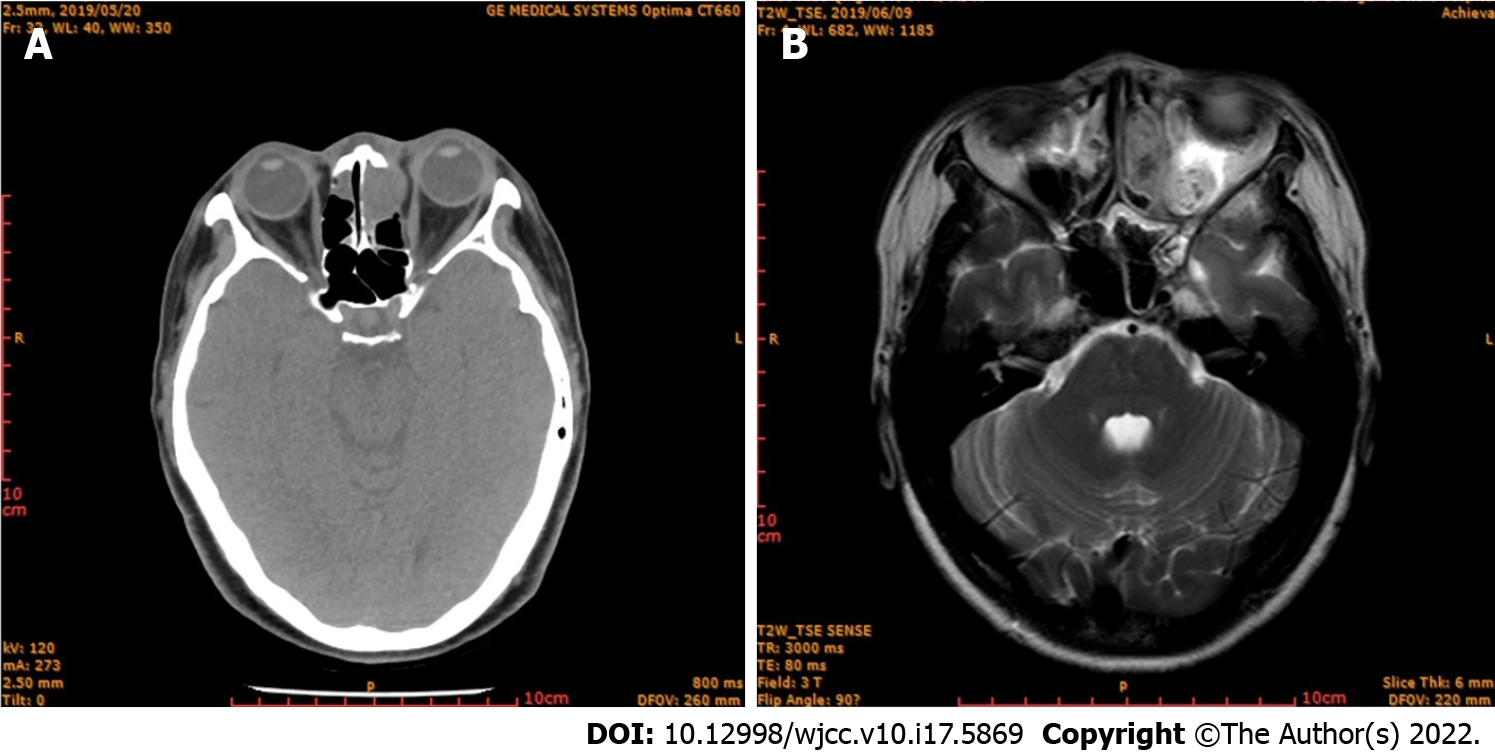
Computed tomography (CT) and magnetic resonance imaging (MRI) examination of the sinus was performed, the findings revealed left maxillary sinusitis, bilateral ethmoid sinusitis, and septal deviation, with bone destruction of the left ethmoid sinus. (Figure 2A and B).
On the basis of the clinical and imaging findings, the diagnosis was established as lung cancer metastasis to the nasal cavity. The tumor in the paranasal sinus was removed and subjected to pathological examination.
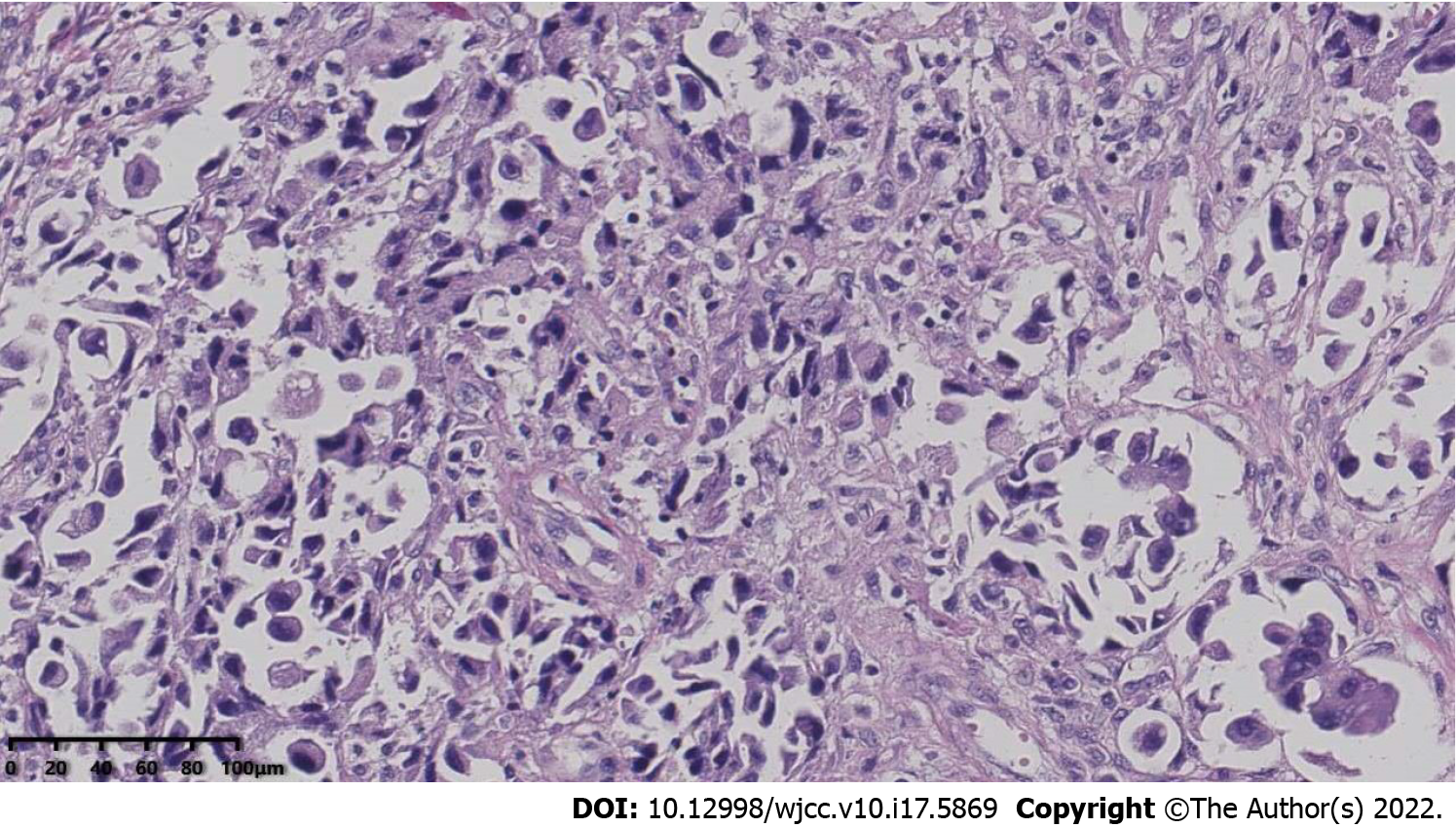
The patient underwent surgical treatment for the removal of the sinus tumors at our hospital. During the operation, a large number of lesions with fish-meat-like appearance of the tissue were found in the ethmoid sinus; the lesions were fragile and easily bleeding. Destruction of the cribriform plate was observed, as well as tumor pressure on the orbit through the orbital fascia. Pathological examination of the biopsied tumor tissue sample revealed that the tumor was malignant. The anterior and middle groups of the ethmoidal sinuses were debrided until the cribriform roof; the frontal sinus was then opened, and a large number of lesions with fish-meat-like appearance of tissue were found in the frontal recess and frontal sinus. An incision was made on the eyebrow arch, and the subcutaneous tissue and muscle tissue were separated. Bone destruction was also observed in the anterior frontal sinus wall, along with the presence of lesions with fish-meat-like appearance, which were removed. The frontal sinus cavity was opened, and the necrotic bone tissue was removed. Finally, the eyebrow arch incision was sutured. Postoperative pathological examination revealed the presence of adenocarcinoma infiltrate between fibrous connective tissues. The results of immunohistochemical examination were as follows: CK7(+), CK20(-), Villin(-), Syn(-), CgA(-), TTF-1(+), Napsin A(+), CDX-2(-), S100(-), CK5/6(-), and P63(-). Figure 3 shows the results of the immunohistochemical examination of tissue sample obtained from the metastatic tumors of the sinus.
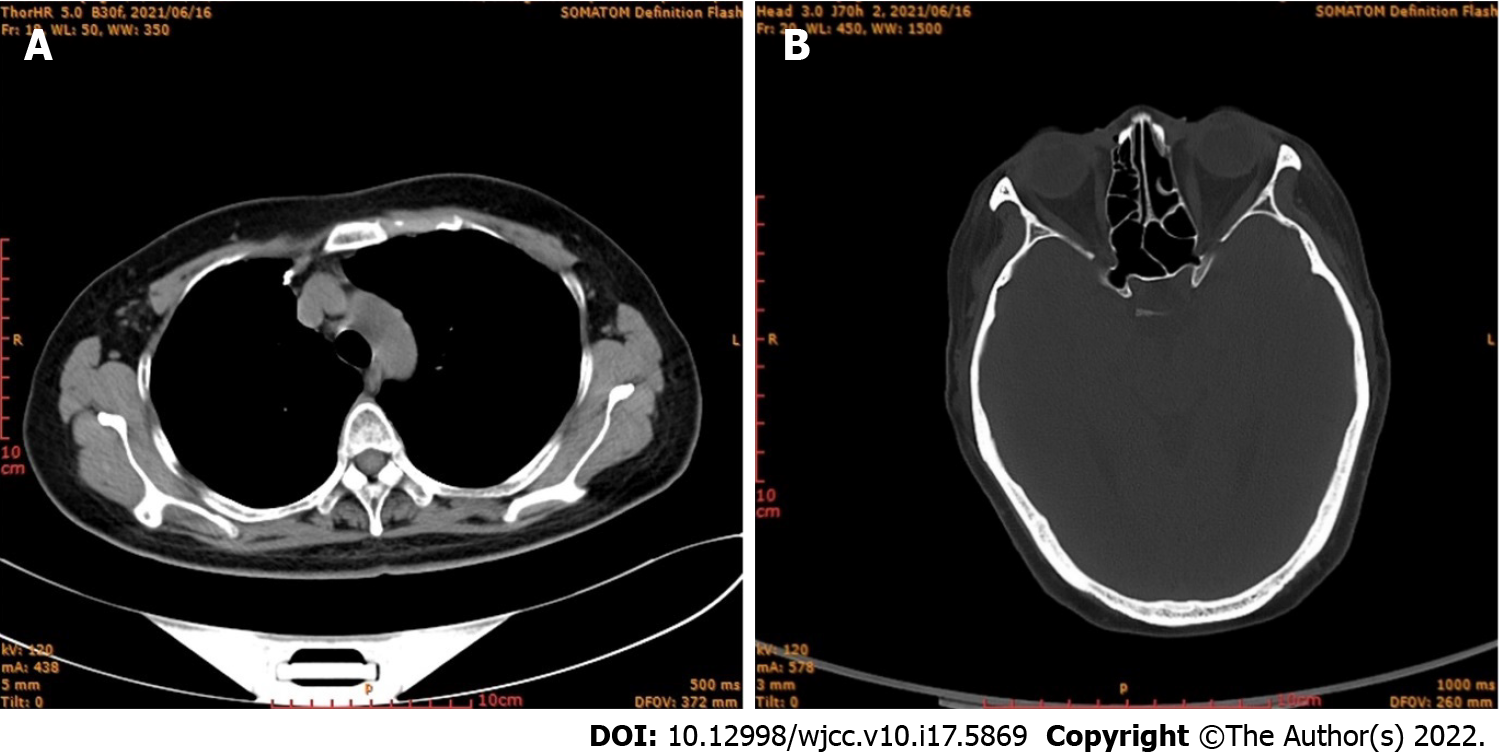
The patient had no postoperative complications and was discharged safely after 7 days. The patient did not receive further radiotherapy or chemotherapy. Follow-up was continued for 2 years, and during this period, she remained completely asymptomatic; CT scans of the lung and sinus were also normal (Figure 4A and B).
Malignant sinus tumors are mostly primary tumors, and only in rare cases are they caused by metastatic tumors originating elsewhere. Metastatic sinus tumors arising from primary tumors of the kidney, lungs, and liver have rarely been reported[9].
The most likely route by which the metastasis occurs to the sinuses may be hematogenous spread of tumor cells. Since the lungs have a rich blood supply, cells of lung adenocarcinoma may easily enter venous circulation. Intrapleural pressure and abdominal pressure may cause detachment of a tumor plug, whereby tumor cells enter blood circulation. The tumor plug may traverse to the large veins of the head, such as the wing plexus and cavernous sinus, eventually reaching the paranasal sinuses through retrograde movement. Since blood flow at the sinuses is sluggish, the tumor plug may easily fall off the circulation and plant itself, leading to the growth of metastatic tumors.
Distant metastasis of primary lung cancer generally occurs to the liver, adrenal glands, brain, or bone, and only rarely to the nasal cavity and paranasal sinuses. Four cases of lung cancer metastasizing to the nasal cavity and sinuses have been reported since 2001; in all of cases, the tumors were squamous-cell carcinoma and epistaxis was the initial clinical presentation. The distant metastasis of lung cancer is a complex process involving the detachment, transport, and growth of tumor cells[10]. Tumor cells break away from the primary tumor, adhere, and invade the basement membrane; thus, they come into close contact with local capillary or lymphatic capillary endothelial cells. The tumor cells pass through the walls of the blood or lymph vessels and are transported via the blood or lymphatic circulation; platelet agglutination may then occur, leading to the formation of a tumor thromboembolus, which reaches the target tissue to give rise to the metastatic tumor[11]. Lung cancer may metastasize though hematogenous spread, lymphatic spread, or direct invasion[12]. Adenocarcinoma and squamous-cell carcinoma of lung are mainly metastasized via blood circulation and lymphatic circulation, respectively; additionally, in lung cancer, metastasis to lymph nodes generally occurs earlier than other metastases[13].
We conducted a literature search of relevant literature with “lung cancer” and “metastasis” as search terms. The PubMed, Scopus, CNKI, and WANFANG MED ONLINE databases were searched for entries published since 2001, and case reports were screened out. One hundred and thirty-eight cases of lung cancer with distant metastasis were identified. The case reports included 100 males and 38 females, and the youngest patient was 17 years old, while the oldest was 97 years old. In all, 123 cases with confirmed pathological results and metastatic sites were identified; among these cases, adenocarcinoma (Table 1) was the most common pathological type and the sites of metastatic tumors were diverse (Table 2).
| Pathological type | No. of cases |
| Adenocarcinoma | 46 |
| Squamous-cell carcinoma | 39 |
| Small-cell carcinoma | 23 |
| Adenosquamous carcinoma | 3 |
| Carcinoma gigantocellulare | 2 |
| Non-small-cell lung cancer | 2 |
| Large-cell lung cancer | 2 |
| Small-round-cell malignant tumors | 1 |
| Sarcomatoid carcinoma | 1 |
| Papillocarcinoma | 1 |
| Mucoepidermoid carcinoma | 1 |
| Neuroendocrine carcinoma | 1 |
| Germ-cell tumor | 1 |
| Metastatic site | No. of cases | Metastatic site | No. of cases |
| Eyeball | 12 | Cerebrum | 16 |
| Choroid | 11 | Peripheral nerve | 3 |
| Iris | 5 | Bone | 15 |
| Eyelid | 2 | Skin | 8 |
| Retina | 1 | Cardioid | 8 |
| Colon | 4 | Marrow | 6 |
| Jejunum | 3 | Nasal cavity | 4 |
| Pancreas | 3 | Oral cavity | 3 |
| Spleen | 2 | Mammary gland | 3 |
| Intestine | 2 | Tonsil | 2 |
| Rectal | 2 | Inguinal glands | 2 |
| Stomach | 1 | Thyroid | 2 |
| Liver | 1 | Kidney | 2 |
| Appendix | 1 | Pituitary | 2 |
| Cervix | 3 | Greater omentum | 1 |
| Ovary | 2 | Abdominal wall | 1 |
| Penis | 1 | Abdominal cavity | 1 |
| Prostate | 1 | Thyroid cartilage | 1 |
| Testis | 1 |
Metastasis of lung cancer to the sinus is rare and its presentation nonspecific. No characteristic clinical or radiologic features have been described to differentiate metastatic tumors from primary malignancy of the sinus[3]. However, nasal and sinus tumors commonly present with epistaxis, and the diagnosis can be confirmed by histopathologic examination of biopsy tissue[4].
Distant metastasis of lung cancer generally occurs in the middle and late stages of cancer, and the survival period for patients is less than 1 year, with poor prognosis[14]. No effective treatments have been identified thus far. The survival of the patients may be improved by surgical resection of the primary and metastatic lesions and subsequent radiotherapy and chemotherapy[4]. Currently, targeted therapy combined with radiotherapy and chemotherapy are mostly used for brain metastasis of lung cancer, while chemotherapy is mainly used for bone metastasis of lung cancer[15]. Surgery combined with radiotherapy is mostly used for eyeball metastasis of lung cancer[16,17], and there is no standard treatment plan for choroidal metastasis of lung cancer[18]. In this case report, the patient received no other treatment except surgical resection of the lesion, and no recurrence was observed during follow-up for two years. Complete spontaneous remission of metastatic non-small-cell carcinoma has also been reported, which may be related to the differentiation of malignant cells into normal phenotype and/or cell death caused by apoptosis or inflammatory necrosis[19]. However, data on the efficacy of treatment are still limited, and further investigation, including large-scale clinical trials, are warranted.
To summarize, we presented a rare case of metastatic sinus tumor secondary to primary lung adenocarcinoma. We also reviewed relevant literature and found that the findings of metastatic sinus tumors were nonspecific. Therefore, physicians should be aware of the possibility of metastatic sinus lesions in patients with a history of primary lung cancer presenting with epistaxis; investigating such patients for sinus metastasis would help early diagnosis and timely initiation of appropriate treatment measures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nepal SP, Japan; Sezer HF, Turkey S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Katz TS, Mendenhall WM, Morris CG, Amdur RJ, Hinerman RW, Villaret DB. Malignant tumors of the nasal cavity and paranasal sinuses. Head Neck. 2002;24:821-829. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 183] [Cited by in F6Publishing: 162] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Clarkson JH, Kirkland PM, Mady S. Bronchogenic metastasis involving the frontal sinus and masquerading as a Pott's puffy tumour: a diagnostic pitfall. Br J Oral Maxillofac Surg. 2002;40:440-441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | King AD, Tse GM, Ahuja AT, Yuen EH, Vlantis AC, To EW, van Hasselt AC. Necrosis in metastatic neck nodes: diagnostic accuracy of CT, MR imaging, and US. Radiology. 2004;230:720-726. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 185] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 4. | Huang CT, Hong RL. Nasion swelling as the presenting symptom of lung adenocarcinoma. J Thorac Oncol. 2009;4:555-558. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Porceddu S, Martin J, Shanker G, Weih L, Russell C, Rischin D, Corry J, Peters L. Paranasal sinus tumors: Peter MacCallum Cancer Institute experience. Head Neck. 2004;26:322-330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Chhiber SS, Nizami FA, R. KA. Renal cell carcinoma presenting as metastasis to frontal sinus in a young male: a case report. Neurosurg Q. 2011;21:288-291. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Orvidas LJ, Lewis JE, Weaver AL, Bagniewski SM, Olsen KD. Adenocarcinoma of the nose and paranasal sinuses: a retrospective study of diagnosis, histologic characteristics, and outcomes in 24 patients. Head Neck. 2005;27:370-375. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Rombaux P, Hamoir M, Liistro G, Bertrand B. Frontal sinus tumor as the first sign of adenocarcinoma of the lung. Otolaryngol Head Neck Surg. 2005;132:816-817. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Koktekir E, Koktekir BE, Recber F, Akdemir G. Lung adenocarcinoma metastasis to frontal sinus mimicking Pott's puffy tumor. J Craniofac Surg. 2013;24:e538-e539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Lachhab L, Fikri M, Aitbenhaddou EH, Arkha Y, Regragui W, Jiddane M, Benomar A, Yahyaoui M. [Atypical metastatic sites for adenocarcinoma of the lung]. J Fr Ophtalmol. 2013;36:e23-e26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Nagano H, Yoshifuku K, Deguchi K, Kurono Y. Adenocarcinoma of the paranasal sinuses and nasal cavity with lung metastasis showing complete response to combination chemotherapy with docetaxel, cisplatin and 5-fluorouracil (TPF): a case report. Auris Nasus Larynx. 2010;37:238-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Agrawal S, Jayant K, Agarwal RK, Dayama KG, Arora S. An unusual case of metastatic male breast cancer to the nasopharynx-review of literature. Ann Palliat Med. 2015;4:233-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 13. | Tang WF, Wu M, Bao H, Xu Y, Lin JS, Liang Y, Zhang Y, Chu XP, Qiu ZB, Su J, Zhang JT, Zhang C, Xu FP, Chen JH, Fu R, Chen Y, Yang T, Chen QK, Wu TT, Wu X, Shao Y, Zheng JT, Xie Z, Lv ZY, Dong S, Wu YL, Zhong WZ. Timing and Origins of Local and Distant Metastases in Lung Cancer. J Thorac Oncol. 2021;16:1136-1148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 14. | Ates I, Yazici O, Ates H, Ozdemir N, Zengin N. Unusual metastases of lung cancer: bulbus oculi and maxillary sinus. Exp Oncol. 2015;37:231-232. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | D'Antonio C, Passaro A, Gori B, Del Signore E, Migliorino MR, Ricciardi S, Fulvi A, de Marinis F. Bone and brain metastasis in lung cancer: recent advances in therapeutic strategies. Ther Adv Med Oncol. 2014;6:101-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | De Potter P. Ocular manifestations of cancer. Curr Opin Ophthalmol. 1998;9:100-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Chen HF, Wang WX, Li XF, Wu LX, Zhu YC, Du KQ, Xu CW. Eye metastasis in lung adenocarcinoma mimicking anterior scleritis: A case report. World J Clin Cases. 2020;8:410-414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Arepalli S, Kaliki S, Shields CL. Choroidal metastases: origin, features, and therapy. Indian J Ophthalmol. 2015;63:122-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 19. | Kappauf H, Gallmeier WM, Wünsch PH, Mittelmeier HO, Birkmann J, Büschel G, Kaiser G, Kraus J. Complete spontaneous remission in a patient with metastatic non-small-cell lung cancer. Case report, review of the literature, and discussion of possible biological pathways involved. Ann Oncol. 1997;8:1031-1039. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 62] [Article Influence: 2.3] [Reference Citation Analysis (1)] |