Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5776
Peer-review started: November 11, 2021
First decision: December 10, 2021
Revised: December 22, 2021
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: June 16, 2022
Processing time: 210 Days and 0.9 Hours
Hemothorax is a rare but life-threatening complication of central venous catheterization. Recent reports suggest that ultrasound guidance may reduce complications however, it does not guarantee safety
A 75-year-old male patient was admitted for laparoscopic radical nephrectomy. Under ultrasound guidance, right internal jugular vein catheterization was successfully achieved after failure to aspirate blood from the catheter in the first attempt. Sudden hypotension developed after surgical positioning and persisted until the end of the operation, lasting for about 4 h. In the recovery room, a massive hemothorax was identified on chest radiography and computed tomography. The patient recovered following chest tube drainage of 1.6 L blood.
Hemothorax must be suspected when unexplained hemodynamic instability develops after central venous catheterization despite ultrasound guidance. So the proper use of ultrasound is important
Core Tip: During central venous catheterization via internal jugular vein, physicians should be aware of the possibility of hemothorax, even during ultrasound-guided procedures due to difficulty achieving real-time visualization of the dilator or catheter tip into the thorax. Confirmation of the guidewire within the brachiocephalic vein is recommended to prevent guidewire malposition, one of the reasons for dilator-induced hemothorax. In hemothorax caused by intrathoracic venous injury, the development of hemodynamic compromise can be delayed and managed with supportive care, obscuring prompt diagnosis during anesthesia. Clinical suspicion and timely diagnostic evaluations are needed for early diagnosis and treatment.
- Citation: Kang H, Cho SY, Suk EH, Ju W, Choi JY. Massive hemothorax following internal jugular vein catheterization under ultrasound guidance: A case report. World J Clin Cases 2022; 10(17): 5776-5782
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5776.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5776
Central venous catheterization (CVC) is a basic invasive procedure in anesthetic and critically ill patients management; however, it may be associated with various complications, vascular injury being the most common. Extrathoracic vascular injuries, such as common carotid artery puncture, can be easily detected and managed with manual compression. However, intrathoracic vascular injuries may be challenging to diagnose because of its invisibility, and external compression is impossible, which can lead serious results.
Ultrasound (US) guidance has markedly improved success rates, with fewer complications than the anatomic landmark method in CVC[1]. Nevertheless, it does not guarantee safety because real-time observations of the guidewire, dilator, and catheter tips are difficult. Hemothorax is a rare complication of CVC but potentially fatal if not promptly managed. The mortality rate is reported up to 93% in a closed claims analysis for hemothorax after CVC[2].
We present a case of massive hemothorax after right internal jugular vein (IJV) catheterization under US guidance and describe proper methods of US guidance and matters that require attention for the prevention of intrathoracic vascular injury causing hemothorax.
A 75-year-old male (ASA class II: weight, 57 kg; height, 160 cm) patient presented massive hemothorax after IJV catheterization under US guidance.
The patient was diagnosed with left renal cell carcinoma on computed tomography (CT) scan performed one month ago.
The patient was on 5 mg of amlodipine (calcium channel blocker) for hypertension for about 10 years.
The patient had a free personal and family history.
Upon arrival in the operating room, his vital signs were as follows: Blood pressure (BP), 155/92 mmHg; heart rate (HR), 61 beats/min; SpO2, 99%. There was no problem with the auscultation of both lungs.
Preoperative examination showed that blood test was normal.
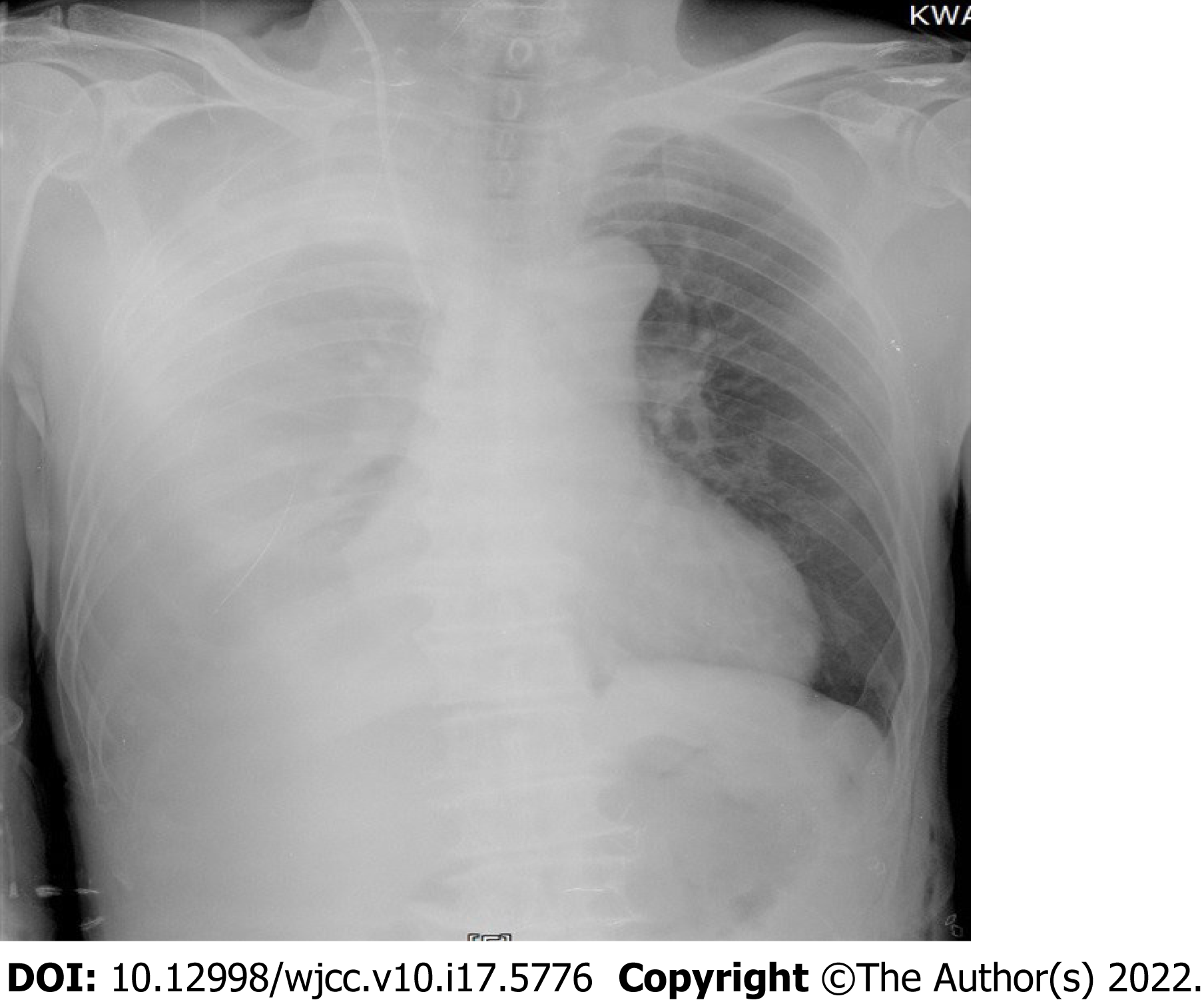
In the recovery room, portable chest radiography showed increased opacity of the right whole lung (Figure 1). Immediately performed chest CT showed a large amount of hemothorax in the right hemithorax. However, extravasation of contrast media was not observed, and the tip of the catheter was well-placed in the superior vena cava (SVC), not in the pleural space (Figure 2).
Preoperative examination showed that the chest radiography, electrocardiogram, and vital signs were normal. A pulmonary function test showed mild obstructive pulmonary disease, and echocardiography showed normal cardiac function. The patient was premedicated with intramuscular glycopyrrolate 0.2 mg.
General anesthesia was induced with 40 mg lidocaine, 120 mg propofol, 50 mcg fentanyl, and 50 mg rocuronium. After tracheal intubation, anesthesia was maintained with oxygen-air-sevoflurane-remifentanil. For continuous arterial pressure measurement, a 20G catheter was placed in the left radial artery. CVC was performed on the right IJV for fluid management and central venous pressure measurement.
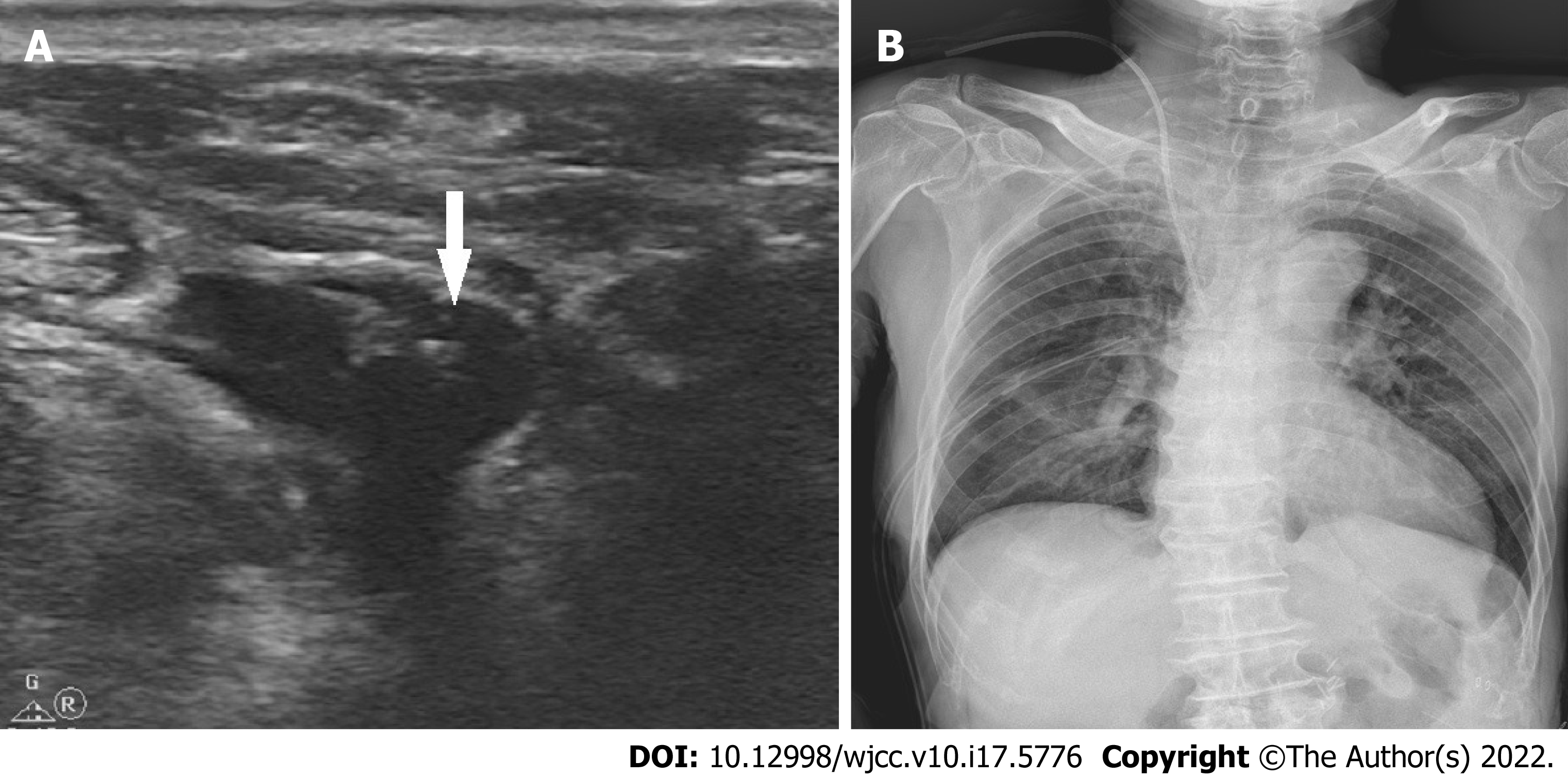
For CVC, the patient was placed in the Trendelenburg position, and we found that he had a relatively short neck. Right IJV catheterization was performed under US guidance. The L12-3 transducer (Philips Electronics, Tokyo, Japan) of the Philips HD15 US machine was used for confirming the right IJV in the short-axis view using the out-of-plane technique. An 18G introducer needle was inserted at the angle formed by the sternal head and the clavicular head of the sternocleidomastoid muscle under real-time US guidance, and dark nonpulsatile blood was aspirated. The J-tip guidewire was inserted through the needle smoothly and positioned in the IJV in the short-axis view of the US (Figure 3A). A dilator was advanced over the guidewire, and an 8.5 F catheter (Edwards Lifesciences, Edwards Oximetry Central Venous Catheter, triple lumen, 20 cm) was inserted over the guidewire without difficulty. However, no blood was aspirated from all three catheter lumens. The catheter was removed immediately, and the same procedure was performed again with the same technique. Before the second attempt, we examined the IJV and surrounding structures above the clavicle using US but did not detect any problems, such as hematoma. The second attempt was successful in aspiration from all three catheter lumens, and the catheter was fixed at a depth of 15 cm. There were no features of arterial puncture or air aspiration during the two attempts.
After surgical positioning to the right lateral decubitus, the BP suddenly dropped to 75/50 mmHg and SpO2 88%. It was considered a temporary hemodynamic reaction due to hypovolemia, and 300 mL of crystalloid was rapidly injected through the central venous catheter. Subsequently, the BP and SpO2 recovered to 110/75 mmHg and 99%. On auscultation of the right lung, there was no apparent reduction in lung sound. At that time, the arterial blood gas analysis (ABGA) results at FiO2 0.4 were pH 7.396, PCO2 33.6 mmHg, PO2 148 mmHg, HCO3- 21.0 mEq/L, BE –2.1 mmol/L/L, SaO2 99%, and Hb 10.6 g/dL. The central venous pressure waveform was adequate, and the patient's vital signs were stable; hence, we proceeded with the surgery.
After the initiation of surgery, the BP dropped to 90/55 mmHg again. The BP remained unstable despite sufficient fluid supply and several intravenous administrations of 0.1 mg of phenylephrine. The BP deteriorated to 80/45 mmHg 1 h later. Norepinephrine infusion was started at 0.03 to 0.06 mcg/kg/min to maintain the BP at 100–110/60–65 mmHg and SpO2 95%-98% until the end of surgery. The total anesthetic time was 4 h and 15 minutes, and the operation time was 3 h. A total of 3500 mL fluid with 2900 mL of crystalloid and 600 mL of colloid was administered. Estimated blood loss was 500 mL, and total urine output was 400 mL. After extubation, the patient was transferred to the recovery room with norepinephrine infusion.
In the recovery room, his vital signs were as follows: BP, 105/70 mmHg; HR, 82 beats/min; SpO2, 89%. He complained of slight difficulty in breathing. On auscultation of the lung, the right lung sound was significantly reduced.
CT revealed a massive hemothorax in the right hemithorax.
The thoracic surgeon inserted a chest tube and drained 1.6 L of dark reddish blood. Following stabilization of vital signs with fluid replacement, he was transferred to the intensive care unit after stopping norepinephrine infusion.
On the next day, the chest radiography showed no more hemothorax findings (Figure 3B). About 50 mL of blood drained through the chest tube on postoperative day (POD) 1, and no blood drained on POD 2. The central venous catheter and chest tube were removed safely on POD 3, and the patient was discharged on POD 7 without any problems.
Hemothorax occurs when an intrathoracic artery or vein is perforated by the dilator or catheter during CVC insertion. Anatomically, the neck and the thoracic inlet consist of a complex network of major vessels, and prompt identification of bleeding vessels causing hemothorax can be challenging.
During CVC, the operator predicts the proper entry of the needle and catheter into the central vein by slightly pulling on the syringe and the catheter and checking for aspiration of venous blood. However, aspiration of blood does not always guarantee proper catheter positioning, and some ports of the catheter might fail to function even when the catheter is well-positioned, depending on the location of the catheter tip. When all ports do not function and blood cannot be aspirated, it is reasonable to assume that the catheter is placed outside the central vein[3]. In this patient, blood could not be aspirated from any port of the catheter after the first attempt of CVC, suggestive of inappropriate catheter location.
The first and most important sign of hemothorax is sudden unexpected hypotension. Close observation is required while performing CVC under general anesthesia, as hypotension can be caused by multiple reasons during anesthesia and may result in delayed diagnosis of hemothorax. In this case, the diagnosis of hemothorax was not prompt. One of the several reasons for this diagnostic delay was the timing of hypotension, as the hemodynamic instability did not occur immediately after IJV catheterization. The first hypotension developed when the patient was positioned in the right lateral decubitus position for surgery and briefly treated with fluid replacement. At that time, there was no obvious abnormality in ABGA and chest auscultation enough to consider hemothorax. Accordingly, we proceeded with surgery without the impression of hemothorax because various factors can cause transient hypotension during anesthesia. The second hypotension event developed and sustained after the start of surgery. During the operation, the patient was in the right lateral decubitus position and covered with surgical drapes and laparoscopic instruments, creating difficulties in right lung examination with ultrasound or chest radiography. Fortunately, we maintained hemodynamic stability with fluid and norepinephrine infusion and planned to evaluate the patient after surgery to identify the cause. Early diagnosis of hemothorax requires frequent checking of lung sound and aggressive imaging modalities when hemothorax is suspected. We should have performed portable chest radiography or lung US scan before starting surgery because there was negative blood aspiration from the first inserted catheter. Recent studies show that using bedside lung US enables a faster diagnosis of hemothorax than chest radiography. Pleural effusions that suggest hemothorax on US are seen as hypoechoic areas between the parietal pleura and visceral pleura at the posterior axillary line in the 8th to 11th intercostal space level[4].
During CVC via IJV, US guidance can adjust the insertion point and depth to avoid vessel injury to a certain degree, but it is less helpful in preventing intrathoracic vessel injury due to dilator or catheter insertion into the thorax. A study involving 450 patients showed that the incidence of hemothorax was 0% under US guidance compared with 1.7% with the landmark technique [1]. However, there have been reports of hemothorax shortly after catheter insertion despite US guidance with CVC via IJV, with reported injured vessels being the right subclavian artery and the right and left brachiocephalic vein (BCV)[5-7]. It is known that when a dilator or catheter with a diameter greater than 7Fr is inserted into an artery, bleeding control through compression is rarely successful. When a hemothorax is caused by arterial damage during CVC, rapid deterioration of vital signs can cause sudden death of the patient, and the hemothorax is only manageable through urgent surgical or interventional repair[5,8,9]. However, most vein injuries that cause hemothorax can be managed with direct compression or venous wall reconstruction by surgical approach, balloon catheter placement, or endovascular repair using endoprosthesis, with some reports even suggesting spontaneous coagulation[6,7]. Kainuma et al[6] reported a case of massive hemothorax due to a perforated right BCV during CVC via right IJV. Thoracoscopic surgery was performed to remove the intrathoracic hematoma. Videothoracoscopic image revealed that the perforation on the right BCV was no longer bleeding. Wetzel et al[7] reported a case of massive hemothorax due to left BCV perforation during left IJV catheterization; a series of contrast venograms revealed a gradual decrease in extravasating contrast media from the BCV to the left pleural cavity. These reports suggest that bleeding from vein injury can be controlled spontaneously, probably by compression from adjacent tissues and positive pressure ventilation during general anesthesia.
In our patient, we could not determine the exact location of the intrathoracic vessel injury, but some of our findings suggest that the hemothorax could result from vein injury. First, although our patient showed a decrease in BP for about 4 h during surgery, this change was not rapid and vital signs were sustained with fluid replacement and vasopressors. If the hemothorax occurred due to an arterial injury, the patient’s vital signs would have shown rapid deterioration and not stabilized during surgery. Second, the blood from thoracentesis was a dark red color, and a postoperative chest CT showed no leakage of contrast media, suggesting spontaneous control of vein injury bleeding. The methods to identify an injured vein when a vein perforation-induced hemothorax is suspected include direct observation through videothoracoscopy, chest CT with contrast leakage, or findings of contrast extension into the pleural cavity during venogram[6,7,10]. In most cases, the site of venous injury leading to immediate hemothorax during CVC through the right IJV is the right BCV[6,11].
Right BCV injury can cause hemothorax through two possible mechanisms. First, despite proper positioning of the guidewire in the right BCV, a strong and deep insertion of the dilator can cause direct injury to the BCV[11]. Therefore, the dilator should not be advanced further than the subcutaneous tissue and should not cross the clavicle. In this case, the patient had a short neck and was positioned in the Trendelenburg position during the CVC procedure, increasing the risk of deeper dilator insertion and direct BCV injury. Another mechanism of injury is that the guidewire from the right IJV can advance into the wrong vessels, such as the right SCV, left BCV, or the azygos vein, leading to injury to the right BCV during dilator insertion[6]. Therefore, it is crucial to ensure proper positioning of the guidewire to prevent dilator-induced vein injury. In the present case, we used US just for directing the introducer needle and identify the guidewire in the IJV. Although the proximal part of the guidewire is located within the IJV, it does not ensure that the distal portion is in the proper position in the thorax. Tampo[12] suggested a three-step procedure for a safe CVC via IJV using US guidance. The first and second steps are the real-time guidance of puncture needle insertion into the IJV in the short-axis and the long-axis views to prevent injury to surrounding structures and avoid penetration into the posterior wall of the IJV. The next step is to verify the guidewire in the BCV using a short-axis and coronal image. This image can be obtained using the following technique: After locating the guidewire in the IJV with a short-axis view, slide the probe down towards the supraclavicular fossa following the guidewire. Once the probe reaches the superior margin of the clavicle, it is angled caudally to obtain the images of the BCV and the subclavian vein on one screen. Fortunately, US facilitates successful visualization of the BCV in 99% of patients, and no sign of guidewire in the BCV suggests malposition of the guidewire in the intrathoracic region[13]. This last view-imaging BCV would help detect guidewire malposition in the thorax. Other options include confirming guidewire or catheter placement with transesophageal echocardiogram or transthoracic echocardiogram, if available[14]. Weekes et al[15] revealed that bedside transthoracic echocardiography using saline flush could predict optimal catheter tip position after CVC.
During IJV catheterization, the possibility of hemothorax persists even in US-guided procedures, especially in the event of negative blood aspiration from the inserted catheter. Proper US use is important in real-time guidance and requires adequate knowledge of technique. In addition to guidewire identification in the IJV, confirmation of the guidewire within the BCV using US is recommended to avoid guidewire malposition, one of the reasons for dilator-induced hemothorax. The physicians should also be aware that hemothorax caused by intrathoracic venous injury cannot be associated with immediate hemodynamic instability. Hypotension induced by venous bleeding can develop after a time lag and be managed with fluid and vasopressor therapy. During anesthesia and surgery, many factors causing hemodynamic compromise can obscure the prompt diagnosis of hemothorax. Therefore, clinical suspicion and timely diagnostic evaluations are necessary for early diagnosis and treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Sparchez Z, Romania; Tokumine J, Japan S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Karakitsos D, Labropoulos N, De Groot E, Patrianakos AP, Kouraklis G, Poularas J, Samonis G, Tsoutsos DA, Konstadoulakis MM, Karabinis A. Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10:R162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 439] [Cited by in RCA: 407] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 2. | Domino KB, Bowdle TA, Posner KL, Spitellie PH, Lee LA, Cheney FW. Injuries and liability related to central vascular catheters: a closed claims analysis. Anesthesiology. 2004;100:1411-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 154] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Ki S, Kim M-h, Lee W, Cho H. Tension hydrothorax induced by malposition of central venous catheter: A case report. Anesth Pain Med. 2017;12(2):151-4 DOI:10.17085/apm.2017.12.2.151. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Kim YI, Ryu JH, Min MK, Park MR, Park SC, Yeom SR, Han SK, Park SW, Lee SH. Usefulness of ultrasonography for the evaluation of catheter misplacement and complications after central venous catheterization. Clin Exp Emerg Med. 2018;5:71-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Kim JH, Kim YJ, Jang JS, Hwang SM. [Endovascular repair of subclavian artery injury secondary to internal jugular vein catheterization: case report]. Braz J Anesthesiol. 2019;69:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Kainuma A, Oshima K, Ota C, Okubo Y, Fukunaga N, Suh SH. Brachiocephalic Vein Perforation During Cannulation of Internal Jugular Vein: A Case Report. A A Case Rep. 2017;9:258-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Wetzel LR, Patel PR, Pesa NL. Central Venous Catheter Placement in the Left Internal Jugular Vein Complicated by Perforation of the Left Brachiocephalic Vein and Massive Hemothorax: A Case Report. A A Case Rep. 2017;9:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Tam JK, Atasha A, Tan AK. Video-assisted thoracic surgery repair of subclavian artery injury following central venous catheterization: a new approach. Interact Cardiovasc Thorac Surg. 2013;17:13-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Lee DJ, Yun JC, Choi HR, Im UJ, Woo SH. Subclavian artery perforation and hemothorax after right internal jugular vein catheterization. Korean J Anesthesiol. 2013;64:558-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Park JH, Song J, Oh PW. Massive hemothorax after central venous catheter insertion in a patient with multiple trauma. J Dent Anesth Pain Med. 2021;21:81-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Innami Y, Oyaizu T, Ouchi T, Umemura N, Koitabashi T. Life-threatening hemothorax resulting from right brachiocephalic vein perforation during right internal jugular vein catheterization. J Anesth. 2009;23:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 12. | Tampo A. Three-step procedure for safe internal jugular vein catheterization under ultrasound guidance. J Med Ultrason (2001). 2018;45:671-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Bowdle A, Jelacic S, Togashi K, Ferreira R. Ultrasound Identification of the Guidewire in the Brachiocephalic Vein for the Prevention of Inadvertent Arterial Catheterization During Internal Jugular Central Venous Catheter Placement. Anesth Analg. 2016;123:896-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Smit JM, Raadsen R, Blans MJ, Petjak M, Van de Ven PM, Tuinman PR. Bedside ultrasound to detect central venous catheter misplacement and associated iatrogenic complications: a systematic review and meta-analysis. Crit Care. 2018;22:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 15. | Weekes AJ, Johnson DA, Keller SM, Efune B, Carey C, Rozario NL, Norton HJ. Central vascular catheter placement evaluation using saline flush and bedside echocardiography. Acad Emerg Med. 2014;21:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |