Published online May 6, 2022. doi: 10.12998/wjcc.v10.i13.4177
Peer-review started: September 10, 2021
First decision: October 22, 2021
Revised: November 2, 2021
Accepted: March 16, 2022
Article in press: March 16, 2022
Published online: May 6, 2022
Processing time: 231 Days and 20.6 Hours
Augmentation cystoplasty, first described by Mikulicz in 1899 involves segments of bowel, stomach or mega-ureter to increase bladder capacity in those with inadequate bladder function or lack of detrusor compliance. The most widely used bowel segment is a detubularised patch of ileum. When ileum is not suitable for augmentation, sigmoid colon is the alternative. However, only eight pregnancies after sigmoidocystoplasty have been reported without detail and clinicians may be uncertain about the effects of sigmoidocystoplasty on reproductive health and pregnancy.
We followed the patient from gestational week 32+3 until 6 wk after delivery. During pregnancy, our patient suffered urinary tract infection twice and had to undergo percutaneous nephrostomy drainage due to progressive hydronephrosis. Despite a dense adhesion between the uterus and neobladder, we were able to deliver a healthy baby by cesarian section in the presence of the attending urologist.
Augmentation cystoplasty-afflicted women can have a healthy reproductive life. Certain perioperative measures may be advisable to avoid serious surgical complications.
Core Tip: Pregnancy following augmentation cystoplasty is relatively rare. Here, we report on a 30-year-old woman who underwent augmentation cystoplasty. We followed the patient from gestational week 32+3 until 6 wk after delivery. Our case, together with a relatively small amount of literature, suggests that women who undergo augmentation cystoplasty can have a healthy reproductive life.
- Citation: Ruan J, Zhang L, Duan MF, Luo DY. Pregnancy and delivery after augmentation cystoplasty: A case report and review of literature. World J Clin Cases 2022; 10(13): 4177-4184
- URL: https://www.wjgnet.com/2307-8960/full/v10/i13/4177.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i13.4177
Augmentation cystoplasty was first described by Mikulicz in 1899[1], and involves segments of bowel, stomach or mega-ureter to increase bladder capacity in those with inadequate bladder function or lack of detrusor compliance. The procedure became widespread in the 1970s after the invention of clean intermittent self-catheterization. The most widely used bowel segment for augmentation cystoplasty is a detubularised patch of ileum or ileocecum while sigmoid colon is the less common alternative.
Pregnancy following augmentation cystoplasty is relatively rare. Clinicians may be uncertain about the effects of augmentation cystoplasty on reproductive health and pregnancy. Here we describe successful pregnancy outcomes in a woman with a history of myelomeningocele and sigmoidocolocystoplasty. As we know, this is the first detailed case report of pregnancy after sigmoidocystoplasty. We also place this case in the context of 24 related studies and 106 reports of 120 pregnancies by women with augmentation cystoplasty.
A 30-year-old pregnant woman with a history of augmentation cystoplasty.
A 30-year-old woman (G2P0A1, one spontaneous miscarriage in first trimester) came to us at gestational week 32+3 for obstetric care. She had a history of congenital myelomeningocele, which was repaired at a local hospital as an infant. At age 13, she underwent nephrectomy of the left kidney at a local hospital to treat severe hydronephrosis. Until 18-years-old, she suffered from urinary incontinence and nocturnal enuresis which gradually resolved after age 18. However, she continued to experience mental distress due to dysuria as well as high urinary frequency and urgency. At age 21, these symptoms worsened and she visited the urology department of our hospital. Color Doppler ultrasonography revealed hydronephrosis of the right kidney as well as stones in the bilateral lower ureter and trabecular bladder. Urodynamics testing indicated low bladder compliance leading to a diagnosis of neurogenic bladder. The patient underwent augmentation sigmoidocolocystoplasty, during which the bladder was observed to have a pear shape with thick walls. A sigmoid colon segment 15 cm long was selected and clam-anastomosed to the bi-valved bladder, while taking care to preserve the mesentery vascular supply. A suprapubic tube was secured in the bladder and the patient self-catheterized until regaining continence at 4 mo after surgery.
At the age of 22, the woman came to the gynecology department of our hospital with a complaint of excessive menses volume. Examinations indicated large intramural myoma and severe anemia. She was given a transfusion of 3 units of erythrocyte suspension, after which abdominal myomectomy was performed. During the procedure, the intestine, left side of the uterus, left adnexa, omentum and mesentery were discovered to be extensively adhered to one another. A myoma of diameter 6 cm with a clear border was observed on the right side of the uterus deep inside the uterine cavity.
When the woman returned to us at the age of 30-years-old and in gestational week 32+3 she reported becoming incontinent starting in the second trimester and experiencing urinary incontinence when standing, dysuria when squatting and incomplete bladder emptying. Previous prenatal examinations and obstetric assessments at a local hospital revealed no fetal congenital anomalies. At 26 wk of gestation, she developed acute pyelonephritis in the right kidney and progressive hydronephrosis; the renal pelvis dilated to a thickness of 4.6 cm with parenchymal thickness 2.0 cm and the diameter of the upper right ureter increased to 1 cm. Because bladder deformity and the trabecula made it difficult to find the ureteric orifice, we failed to place a double pigtail ureteral stent under cystoscopy and instead performed percutaneous nephrostomy drainage. There was no change in creatinine clearance in the serial examinations and serial urine dipsticks for protein and occult blood were negative. In the third trimester, the patient showed elevated liver enzymes and itching over the entire body. After testing negative for hepatitis virus infection, she was given oral transmetil and liver function gradually returned to normal. During the entire pregnancy, she suffered two urinary tract infections which were treated promptly with cefoxitin and ceftriaxone.
The patient had no family history of similar illnesses.
Abdominal enlargement, other signs were negative.
There was no change in creatinine clearance in the serial examinations and serial urine dipsticks for protein and occult blood were negative.
The patient was admitted at gestational week 39+3 to the obstetrics department. Ultrasonography and magnetic resonance imaging showed that the bladder was vertically stretched by the pregnant uterus to a level approximately 3.1 cm above the umbilical level and 2.9 cm below the fundus (Figure 1). This implied a severe adhesion between her uterus and the neobladder.
Pregnant woman with a history of augmentation cystoplasty and isolated kidney.
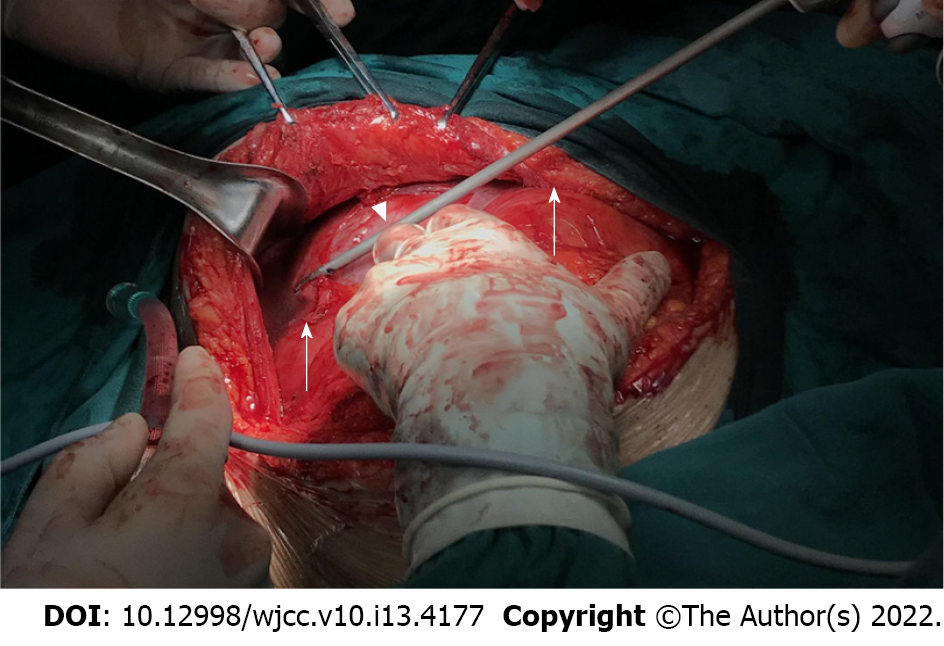
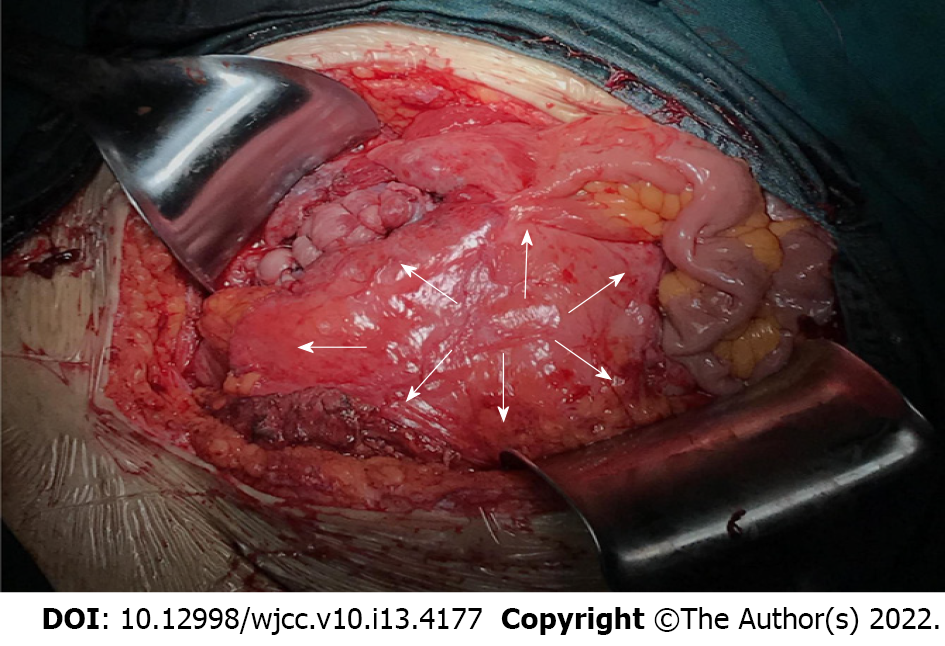
Given the patient’s history of myomectomy deep inside the uterine cavity, we performed a cesarian section under general anesthesia in the presence of an experienced obstetrician and reconstructive urological surgeon at gestational week 40+2. During the procedure, which took 167 min, dense adhesions between the omentum and the parietal peritoneum were observed. The bowel loop, which was used for augmentation, was draped over the entire anterior surface of the uterus. The mesentery of the neobladder went across the uterus from the left side. Saline solution was injected to expand the bladder and neobladder until their interface with surrounding structures was obvious. The adhesion between the uterus and neobladder was dissected with an ultrasonic scalpel. Left lateral traction was applied to the neobladder and finally a right lateral longitudinal incision was made (Figures 2 and 3). A live female newborn weighing 2790 g was delivered. Apgar scores were 9.9 at 1.5 min and 10 at 10 min. No sign of injury to the vascular pedicle of the neobladder was found. Mother and child recovered normally and were discharged 1 wk after delivery.
Telephone follow-up with the patient at 42 d after delivery revealed that she had suffered another urinary tract infection which was treated with ceftazidime. The nephrostomy tube was removed at 5 wk after delivery, after which the patient intermittently self-catheterized to maintain urinary continence. No significant problems were observed in the newborn.
As augmentation cystoplasty becomes more common, clinicians and patients may wish to understand in detail whether it influences pregnancy outcomes. The present case highlights that the procedure need not have negative impacts on such outcomes, even when the patient has a history of myelomeningocele surgical repair, left nephrectomy and repeated urinary tract infections.
To put the present case in perspective with other clinical experiences, we reviewed the literature on outcomes of pregnancies involving women with augmentation cystoplasty (Table 1)[2-25]. The main indication for reconstruction in published cases is myelodysplasia which is also normally an indication for invasive prenatal diagnosis using, for example, amniocentesis. However, amniocentesis may not be appropriate if the patient shows adhesions due to previous extensive abdominopelvic surgeries and if the mesenteric blood supply may be damaged by the procedure. While one report of patients with ileocecal cystoplasty indicated that amniocentesis was not performed because of the risk of injury to the bladder vasculature[3], other reports of patients with augmentation cystoplasty showed that it can be performed without complications[4,5]. We recommend adequate doctor-patient communication of the potential risks of different methods of prenatal screening. Our patient refused amniocentesis after prolonged consideration so instead we performed color Doppler ultrasonography.
| Ref. | Year | Patients (n) | Neobladder | Pregnancies (n) | Time of delivery | Urinary complications during pregnancy | Mode of delivery |
| This case | 2021 | 1 | Sigmoidocystoplasty | 1 | 40+2 GW | UTI, hydronephrosis | CS |
| Yamazaki et al[7] | 1997 | 1 | Ileocystoplasty | 1 | 32 GW | UTI, hydronephrosis | CS |
| Yamamoto et al[8] | 1997 | 1 | N/A | 1 | N/A | UTI, hydronephrosis | CS |
| Shaikh et al[12] | 2006 | 1 | Ileocystoplasty | 1 | 38 GW | UTI | CS |
| Sagili et al[13] | 2013 | 1 | N/A | 1 | 40 GW | None | VD |
| Kapoor et al[14] | 2014 | 1 | N/A | 1 | Full term | UTI | CS (unsuccessful induction of labor) |
| Correia et al[15] | 2015 | 1 | Ileocystoplasty | 1 | 38 GW | UTI, hydronephrosis | CS (orthopedic limitations to vaginal delivery) |
| Kameda et al[16] | 2017 | 1 | Ileocystoplasty | 1 | 38 GW | N/A | VD |
| Goodwin et al[19] | 1962 | 1 | Ileocystoplasty | 1 | Full term | UTI | VD |
| Kirkeby et al[20] | 1992 | 1 | Ileocystoplasty | 1 | Full term | None | VD |
| Muthulakshmi et al[21] | 2010 | 1 | Ileocystoplasty | 1 | 37+4 GW | None | VD |
| Henry et al[22] | 2002 | 1 | Ileocystoplasty | 1 | Full term | UTI | VD |
| Natarajan et al[23] | 2002 | 1 | Ileocystoplasty | 1 | 37 GW | UTI | CS |
| Smith et al[2] | 1973 | 2 | Ileocystoplasty, colocystoplasty | 3 | 39, 35, 30 GW (baby died from atelectasis) | UTI, incontinence, deterioration of renal insufficiency | 2VD, 1CS (placenta previa) |
| Doyle et al[3] | 1988 | 2 | Ileocecocystoplasty | 2 | 41, 37 GW | UTI, bladder calculi, incontinence | 2 VD |
| Taniguchi et al[9] | 2002 | 2 | Sigmoidocystoplasty, ileocecocystoplasty | 2 | 36, 36 GW | UTI, hydronephrosis | 2VD |
| Hayashi et al[18] | 2017 | 2 | Sigmoidocystoplasty | 2 | N/A | N/A | N/A |
| Quenneville et al[10] | 2003 | 3 | Ileocystoplasty | 3 | All full term | UTI | 3VD |
| Dap et al[17] | 2017 | 3 | N/A | 6 | 1 premature labor | UTI, Artificial sphincter Infection, hydronephrosis, incontinence | 6CS (3 breech) |
| Le Liepvre et al[24] | 2017 | 3 | N/A | 5 | 1 miscarriage | UTI, 2 hydronephrosis | N/A |
| Hensle et al[25] | 2004 | 4 | N/A | 4 | 1 premature labor | UTI, 1 incontinence | 1VD, 3CS |
| Greenwell et al[11] | 2003 | 13 | N/A | 13 | 35-40 GW | 13 UTI, 3 hydronephrosis | Majority CS |
| Hill et al[4] | 1990 | 15 | 6 ileocystoplasty, 4 ileocecocystoplasty, 5 sigmoidocystoplasty | 15 | 4 premature labor | 9 UTI, 5 incontinence, 1 bilateral ureteral obstruction+anemia+renal function deteriorated | 10VD, 5CS |
| Fenn et al[5] | 1995 | 18 | N/A | 19 | 1 premature labor | 14 UTI, 1 AUS dysfunction | 18VD, 1CS (transverse lie) |
| Creagh et al[6] | 1995 | 27 | N/A | 34 | All full term | All UTI, 6 postpartum incontinence | 28VD, 6CS (4 obstetrical indications, 2 AUS) |
Our patient suffered repeated urinary tract infections and had a history of pyelonephritis and hydronephrosis. These features appear to affect 60%-100% of pregnant women with a history of augmentation cystoplasty[4-6]. Most studies recommend monthly culture tests of midstream urine to detect and treat infections early and completely. Recurrent urinary tract infections have been associated with premature labor[4,5,7,9,17,26], but our review of 104 pregnancies involving women with a history of augmentation cystoplasty, including the present case, showed that only 11 (10.6%) ended in preterm births. Our analysis of the literature suggests that most reports of premature labor in women with augmentation cystoplasty and recurrent urinary tract infections were published before 2002. This suggests that clinical management of such women has improved.
Our patient had a history of hydronephrosis during pregnancy, and we identified nine patients who had suffered this condition[4,7-9,11,15,17]. Seven of those cases were treated with ureteral stent or, as in the present case, nephrostomy. Both procedures can relieve obstructions and thereby protect renal function[27]. One study recommended assaying serum creatine monthly and if it increases, performing renal ultrasonography of the upper tract to detect progressive hydronephrosis[4]. Although our patient had only one functioning kidney and experienced two urinary tract infections, pyelonephritis and progressive hydronephrosis during pregnancy, her renal function remained normal. This was likely because she was treated promptly with antibiotics and nephrostomy. Similarly, renal function remained stable throughout pregnancy in all but two of the pregnancies involving women with an augmentation cystoplasty that we identified in the literature. Those two patients suffered complications of hyperchloremic acidosis and hypokalemia[2], or anemia and anuria secondary to bilateral ureteral obstruction[4].
Our review of the literature indicates no consensus on a particular mode of delivery as the best for women with augmentation cystoplasty. Of 101 pregnancies for which the mode of delivery was described (including the present case), 72 were vaginal deliveries, with or without instrumental extraction, while the remaining 29 were by cesarean section, 13 of which were conducted because of obstetric indications.
It is recommended that all patients who have undergone augmentation cystoplasty alone can deliver vaginally in the absence of any obstetric indications[4,5]. For women with a history of enterocystoplasty who had undergone insertion of an artificial urinary sphincter (AUS) together, vaginal delivery may not be indicated because pressure on the AUS may cause ischemic damage to the urinary continence mechanism. Indeed, some studies have suggested that vaginal delivery may increase risk of postpartum incontinence in women who have undergone augmentation cystoplasty combined with bladder neck reconstruction[5]. Other studies, however, have shown that the presence of a reconstructed lower urinary tract, with or without an artificial urinary sphincter, does not preclude normal pregnancy and vaginal delivery[6] and need not affect postpartum continence[10].
On the other hand, Cesarean section can damage the neobladder and vascular pedicle[6] leading some to suggest that it should be avoided unless there is a positive obstetric indication[28]. Most reports of cesarean sections performed on pregnant women with a history of augmentation cystoplasty have involved a classical incision rather than a low-segment uterine incision. In fact, some advocate making the incision in an upper rather than lower segment in order to avoid adhesions between the neobladder and surrounding tissues[4,15]. In our case, we made a right lateral longitudinal incision of the corpus uteri, based on the position of the mesentery. Injury of mesentery to the neobladder can occur whether the incision is made higher or lower since the augmentation cystoplasty may be draped over the uterus[12,14]. We suggest that the choice of uterine incision should be individualized. We also recommend two measures that may have contributed to the good outcomes of cesarean section for our patient: (1) Preoperative imaging, especially magnetic resonance imaging, should be performed to gain thorough insight into the patient`s anatomy; and (2) The cesarean section should be performed in the presence of a urologist with knowledge of the cystoplasty, as emphasized in several previous studies[7,10,28,29]. Vesical injection of saline or methylene blue solution may facilitate dissection in patients with marked adhesion, as in the present case. If perforation of the neobladder is suspected, the potential leak should be inspected[4].
Ensuring good pain control during delivery can be challenging in patients with myelodysplasia, such as the present case. Epidural anesthesia is generally not possible in these patients so general anesthesia may be required during cesarean section[11], as we performed in our patient. It may be possible to achieve painless vaginal delivery by inducing extradural anesthesia above the point of myelomeningocele repair[16].
The present case, together with a relatively small amount of literature, suggests that women who undergo augmentation cystoplasty can have a healthy reproductive life. The most common complications are urinary tract infections and hydronephrosis. During pregnancy, clinicians should closely monitor urine and renal function. Ureteral stent or nephrostomy may be necessary to relieve obstructions and preserve renal function. Augmentation cystoplasty by itself is not a contraindication for vaginal delivery, though it may not be optimal for women who undergo bladder neck surgery. Research is needed to identify the optimal delivery method for such women. When performing cesarean sections on such women, attention should be paid to exploratory preoperative imaging and to consultation with the urologist familiar with the patient`s cystoplasty.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Chinese Society of Perinatal Medicine.
Specialty type: Obstetrics and gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Issack FHH, Ethiopia; Tajiri K, Japan S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Vordermark JS, Deshon GE, Agee RE. Management of pregnancy after major urinary reconstruction. Obstet Gynecol. 1990;75:564-567. [PubMed] |
| 2. | Smith AM. Enterocystoplasty and pregnancy. Am J Obstet Gynecol. 1973;117:527-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Doyle BA, Smith SP, Stempel LE. Urinary undiversion and pregnancy. Am J Obstet Gynecol. 1988;158:1131-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Hill DE, Kramer SA. Management of pregnancy after augmentation cystoplasty. J Urol. 1990;144:457-9; discussion 460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Fenn N, Barrington JW, Stephenson TP. Clam enterocystoplasty and pregnancy. Br J Urol. 1995;75:85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Creagh TA, McInerney PD, Thomas PJ, Mundy AR. Pregnancy after lower urinary tract reconstruction in women. J Urol. 1995;154:1323-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Yamazaki Y, Yago R, Toma H, Onodera J, Nakabayashi M. [Pregnancy after augmentation cystoplasty. A case report]. Nihon Hinyokika Gakkai Zasshi. 1997;88:632-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Yamamoto M, Yamada K, Hirata N, Kawata Y, Hirayama A, Kashiwai H, Momose H, Shiomi T, Suemori T, Natsume O, Hirao Y. [Pregnancy and delivery in the patients with spina bifida--report of 5 cases]. Nihon Hinyokika Gakkai Zasshi. 1997;88:1005-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Taniguchi A, Kakizaki H, Murakumo M, Nonomura K, Koyanagi T. [Management of pregnancy and delivery after augmentation cystoplasty]. Nihon Hinyokika Gakkai Zasshi. 2002;93:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Quenneville V, Beurton D, Thomas L, Fontaine E. Pregnancy and vaginal delivery after augmentation cystoplasty. BJU Int. 2003;91:893-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Greenwell TJ, Venn SN, Creighton S, Leaver RB, Woodhouse CR. Pregnancy after lower urinary tract reconstruction for congenital abnormalities. BJU Int. 2003;92:773-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 47] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Shaikh A, Ahsan S, Zaidi Z. Pregnancy after augmentation cystoplasty. J Pak Med Assoc. 2006;56:465-467. [PubMed] |
| 13. | Sagili H, Singh P, Manikandan K, Dasari P. Vaginal delivery after augmentation cystoplasty and Mitrofanoff's procedure for incontinence following traumatic bladder neck transection. J Obstet Gynaecol. 2013;33:740-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Kapoor D, Chipde SS, Agrawal S, Chipde S, Kapoor R. Delivery after augmentation cystoplasty: Implications and precautions. J Nat Sci Biol Med. 2014;5:206-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Correia C, Pardal C, Igreja J. Management of pregnancy after augmentation cystoplasty. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Kameda M, Takahara E, Kobayashi M, Sasaki K, Morihara R, Date I. Pregnancy and delivery after myelomeningocele repair, ventriculoperitoneal shunt implantation, and augmentation cystoplasty. Childs Nerv Syst. 2017;33:1015-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Dap M, Larmure O, Morel O, Lemelle JL. Pregnancy outcomes among patients with prior bladder exstrophy. Int J Gynaecol Obstet. 2017;139:368-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Hayashi Y, Nishimura E, Shimizu S, Miyano G, Okawada M, Nagae I, Lane GJ, Katsumata K, Yamataka A, Tsuchida A. Sigmoidocolocystoplasty for neurogenic bladder reviewed after 20 years. J Pediatr Surg. 2017;52:2070-2073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | GOODWIN WE, BETENBAUGH HS, HAYNES VE, ROSS SC. Full-term pregnancy and spontaneous delivery after ileocystoplasty. JAMA. 1962;181:906-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Kirkeby LT, Beier-Holgersen R, Nordling J. Successful pregnancy after ileocystoplasty. Case report. Scand J Urol Nephrol. 1992;26:195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 21. | Muthulakshmi B, Allahdin S. Pregnancy with clam ileocystoplasty and appendix Mitrofanoff procedure: vaginal delivery can be considered. Int Urogynecol J. 2010;21:893-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Henry L, Cormier L, Fontaine B, Mangin P. [Vaginal delivery in a patient with an artificial urinary sphincter and augmentation enterocystoplasty]. Prog Urol. 2002;12:303-305. [PubMed] |
| 23. | Natarajan V, Kapur D, Sharma S, Singh G. Pregnancy in patients with spina bifida and urinary diversion. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:383-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Le Liepvre H, Dinh A, Idiard-Chamois B, Chartier-Kastler E, Phé V, Even A, Robain G, Denys P. Pregnancy in spinal cord-injured women, a cohort study of 37 pregnancies in 25 women. Spinal Cord. 2017;55:167-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Hensle TW, Bingham JB, Reiley EA, Cleary-Goldman JE, Malone FD, Robinson JN. The urological care and outcome of pregnancy after urinary tract reconstruction. BJU Int. 2004;93:588-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Bey E, Perrouin-Verbe B, Reiss B, Lefort M, Le Normand L, Perrouin-Verbe MA. Outcomes of pregnancy and delivery in women with continent lower urinary tract reconstruction: systematic review of the literature. Int Urogynecol J. 2021;32:1707-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Voges GE, Orestano L, Schumacher S, Hohenfellner R. [Continent urinary diversion and pregnancy]. Geburtshilfe Frauenheilkd. 1995;55:711-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Greenwell TJ, Venn SN, Mundy AR. Augmentation cystoplasty. BJU Int. 2001;88:511-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 130] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | Niknejad KG, Atala A. Bladder augmentation techniques in women. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11:156-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |